Abstract
Thrombosis is one of the most common causes of mortality in Paroxysmal nocturnal hemoglobinuria (PNH), but the predisposing factors for thrombosis are yet to be defined. In this study, we outline the clinical characters and the susceptible genes which lead to thrombotic formation in 104 patients with PNH. The results displayed that the genotypes with minor alleles of rs495828 or rs2519093 in the ABO gene were associated with high risk to thrombus formation (OR 5.95, 95% CI 1.90-18.65 and OR 6.3, 95% CI 2.01-19.79, respectively). Further, the TT haplotype was associated with a significant increased risk of thrombosis (OR=3.25, 95%CI 1.42-7.39). Multivariate regression analysis showed larger PNH clone and genotypes with rs495828/rs2519093 minor allele as independent risk factors for thrombosis in PNH. Some patients who came back for follow-up were tested for the plasma levels of vWF and factor VIII. Patients carrying the rs495828/rs2519093 minor allele had a significant higher level of vWF and factor VIII compared with those carrying the major allele. Therefore, we found for the first time that the rs495828/rs2519093 polymorphism represent an independent prognostic factor in PNH patients for thrombus formation, probably by increasing the vWF and factor VIII.
Keywords: polymorphism, gene, thrombosis risk, paroxysmal nocturnal hemoglobinuria
INTRODUCTION
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare disease caused by an acquired mutation of the X-linked PIG-A (phosphatidylinositol glycan class A) gene on the hematopoietic stem cell. The PIG-A mutation disturbs the biosynthesis of glycosylphosphatidylinositol (GPI) anchor, which is necessary to attach dozens of membrane proteins to the cell surface [1]. Deficiency of the GPI-anchored complement regulatory proteins CD55 and CD59 on blood cells (CD55 inhibits the C3 and C5 convertases, CD59 blocks the assembly of the membrane attack complex), results in more vulnerable to the action of complement, and therefore leading to complement-mediated lysis [2, 3].
The main clinical manifestations of PNH include hemolytic anemia, thrombosis and bone marrow failure. However, Thromboembolism is one of the most common causes of mortality in PNH and accounts for approximately 40% to 67% of deaths [4, 5]. The incidence of thrombotic in PNH patients is various among different ethnic groups, 29%-44% in Caucasians [6, 7],18% in Korean [8], whereas 11.5% in Chinese [9]. According to the data from the international PNH registry, the incidence is 15.5% [10]. However, Thrombosis in PNH frequently occurs in vital site, either in western or eastern countries, which cause severe complications or even death [11, 12].
Multiple mechanisms including platelet activation, free hemoglobin release, nitric oxide depletion, urokinase type plasminogen activator receptor absence and endothelial dysfunction contribute to thrombosis in PNH, nevertheless, the predisposing factors and mechanisms for thrombosis are yet to be clearly elucidated [13–15].
To further identify intrinsic risk factors which lead to thrombotic formation, twenty-six SNPs in 17 genes which had been reported as high risk factors for venous thromboembolism (VTE) were detected [16–18]. Subsequently the correlation between clinical factors and thrombotic events was analyzed. The results showed the genotypes in the ABO gene were associated with high risk to thrombus formation,ABO gene is located at chromosome 9p 34.1-34.2, determines not only the biosynthesis of blood group antigen, but also encodes glycosyltransferases responses for post translational glycosylation of vWF, which protect vWF from proteolysis [19, 20]. As the carrier molecule of factor VIII, the vWF level further affect the level of factor VIII [21]. Therefore, patients who came back for follow-up were tested for the plasma levels of vWF and factor VIII, the risk factors associated with thromboembolism and the possible underlying mechanism was also investigated in this study.
RESULTS
Clinical characteristics of patients
The basic information and clinical characteristics of patients were summarized in Table 1. The mean age of 104 PNH patients was 42.7 years, with 54% of males. 41% of patients were diagnosed as PNH/aplastic anemia (AA), these patients treated with corticosteroids, blood transfusion supportive therapy, and immunosuppressant for PNH/AA. During the median 719 days of follow-up period, twenty-one thrombotic events occurred in 17 (16.3%) of 104 PNH patients. Only 2 thrombosis occurred at arterial sites and 19 occurred at venous sites (details were shown in Supplementary Table 3). The median time from first diagnosis to thrombotic formation in these 17 patients was 264 days. There have been 4 deaths during the follow-up periods, 2 were attributable to thrombosis, another 2 patients were secondary to the infection and the colorectal carcinoma respectively. Only granulocyte PNH clone sizes was significant higher in thrombus group compared with non-thrombus group (86.24% vs. 59.03%, P<0.001), whereas no significant difference was noticed in age, gender, white blood cell and platelet counts, hemolytic parameters, thrombotic parameters (all P value>0.05) between the patients with and without thrombosis.
Table 1. Clinical characteristics of 104 patients with PNH.
| Characteristic | Whole cohort | With thrombosis | Without thrombosis | P value |
|---|---|---|---|---|
| Cases, n (%) | 104 (100) | 17 (16.3) | 87 (83.7) | |
| Age (years) | 42.70±15.39 | 38.94±10.11 | 43.44±16.16 | 0.144 |
| Male gender, n (%) | 56 (54) | 9 (53) | 47 (45) | 0.935 |
| Bone marrow failure, n (%) | 43 (41) | 9 (53) | 34 (39) | 0.289 |
| PNH clone size (%) | 63.48±35.53 | 86.24±19.90 | 59.03±36.27 | <0.001 |
| Blood cells counting | ||||
| Reticulocytes (%) | 4.69±3.29 | 4.12±2.02 | 4.82±3.51 | 0.429 |
| Leukocytes (×109/L) | 4.01±1.91 | 4.31±2.28 | 3.95±1.84 | 0.49 |
| Hemoglobin (g/L) | 79.80±24.55 | 80.69±18.35 | 79.64±25.63 | 0.876 |
| Platelets (×109/L) | 109.51±85.55 | 93.94±98.41 | 112.44±83.24 | 0.43 |
| Hemolytic parameters | ||||
| Lactate dehydrogenase (U/L) | 1211.40±883.60 | 1115.31±713.73 | 1231.36±917.73 | 0.635 |
| Total bilirubin (μmol/L) | 27.54±21.73 | 27.68±19.41 | 27.52±22.27 | 0.979 |
| Conjugated bilibubin (μmol/L) | 7.43±4.23 | 8.32±3.86 | 7.25±4.30 | 0.36 |
| Unconjugated bilibubin (μmol/L) | 20.11±19.34 | 19.36±17.49 | 20.26±19.79 | 0.865 |
| Hematuria, n (%) | 44 (42) | 7 (41) | 37 (43) | 0.918 |
| Thrombotic parameters | ||||
| Protein C (%) | 111.04±21.01 | 110.63±27.01 | 111.12±19.87 | 0.932 |
| Protein S (%) | 105.96±19.91 | 101.56±25.70 | 106.80±18.69 | 0.338 |
| Fibrinogen (g/L) | 2.55±0.71 | 2.79±1.14 | 2.50±0.59 | 0.323 |
| D-dimer (mg/L) | 0.46±0.52 | 0.63±0.80 | 0.43±0.45 | 0.324 |
| Antithrombin (%) | 113.67±14.79 | 117.38±18.28 | 112.95±14.05 | 0.276 |
P value represented the significance of the data between patients with and without thrombosis.
Association between SNPs and thrombotic risk in PNH
Among the twenty-six alleles in seventeen genes sequenced, nine SNPs (rs8176750, rs146922325, rs1799963, rs1801133, rs397507444, rs199469491, rs199469495, rs121918474, rs6025) were found to have only one genotype. In addition, two SNPs (rs8176704 and rs2289252) did not conform to Hardy-Weinberg equilibrium on statistical analysis (P<0.05; shown in Supplementary Table 4). Therefore, these eleven SNPs were excluded for further analysis. Among the rest fifteen SNPs detected, the rs495828 of ABO gene was significant relevant to an increased risk of thrombosis in PNH patients, as shown by the dominant model (GT+TT vs. GG: OR 5.95, 95% CI 1.90-18.65, P=0.002) and allele model (T vs. G: OR 3.52, 95%CI 1.57-7.90, P=0.003). An increased risk of thrombosis was also observed in rs2519093 of ABO gene (dominant model: TC+TT vs. CC, OR 6.3, 95% CI 2.01-19.79, P=0.001; allele model: T vs. C, OR 3.25, 95%CI 1.43-7.39, P=0.006; Table 2). No correlation was found between any other SNPs and thrombotic risk.
Table 2. Genotype and allele frequencies of 15 SNPs in PNH patients and their associations with thrombosis.
| Gene | SNP | Genotype | With thrombosis | Without thrombosis | Dominant model | Recessive model | Allele | With thrombosis | Without thrombosis | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P value | OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | ||||||||
| ABO | rs495828 | TT | 1 | 1 | 0.003 | 5.95 (1.90-18.65) | 0.002 | 5.38(0.32-90.42) | 0.302 | T | 13 | 26 | 3.52 (1.57-7.90) | 0.003 |
| TG | 11 | 24 | G | 21 | 148 | |||||||||
| GG | 5 | 62 | ||||||||||||
| rs8176719 | CC | 6 | 15 | 0.087 | 2.24(0.47-10.63) | 0.516 | 2.62(0.84-8.19) | 0.105 | C | 21 | 82 | 1.81 (0.85-3.85) | 0.136 | |
| C -- | 9 | 52 | --. | 13 | 92 | |||||||||
| -- -- | 2 | 20 | ||||||||||||
| rs8176747 | GG | 0 | 12 | 0.242 | 0.60 (0.21-1.71) | 0.428 | 1.23(1.11-1.35) | 0.208 | G | 7 | 59 | 0.51 (0.21-1.23) | 0.160 | |
| GC | 7 | 35 | C | 27 | 115 | |||||||||
| CC | 10 | 40 | ||||||||||||
| rs2519093 | TT | 0 | 1 | 0.002 | 6.3 (2.01-19.79) | 0.001 | 1.20(1.10-1.31) | 1 | T | 12 | 25 | 3.25 (1.43-7.39) | 0.006 | |
| TC | 12 | 23 | C | 22 | 149 | |||||||||
| CC | 5 | 63 | ||||||||||||
| STXBP5 | rs1039084 | GG | 2 | 9 | 0.671 | 1.63 (0.56-4.60) | 0.434 | 1.16(0.23-5.89) | 1 | G | 12 | 50 | 1.35 (0.62-2.94) | 0.539 |
| GA | 8 | 32 | A | 22 | 124 | |||||||||
| AA | 7 | 46 | ||||||||||||
| vWF | rs1063856 | CC | 0 | 1 | 0.721 | 1.52 (0.29-8.06) | 0.647 | 1.20(1.10-1.31) | 1 | C | 2 | 8 | 1.30 (0.26-6.39) | 0.669 |
| CT | 2 | 6 | T | 32 | 166 | |||||||||
| TT | 15 | 80 | ||||||||||||
| GP6 | rs1613662 | GG | 0 | 0 | 0.187 | 3.73 (0.57-24.27) | 0.187 | -- | -- | G | 2 | 3 | 3.56 (0.57-22.19) | 0.189 |
| GA | 2 | 3 | A | 32 | 171 | |||||||||
| AA | 15 | 84 | ||||||||||||
| THBD | rs16984852 | AA | 0 | 0 | 1 | 0.69 (0.03-13.97) | 1 | -- | -- | A | 0 | 3 | 0.71 (0.04-14.07) | 1 |
| AC | 0 | 3 | C | 34 | 171 | |||||||||
| CC | 17 | 84 | ||||||||||||
| F11 | rs2036914 | TT | 0 | 7 | 0.364 | 0.54 (0.17-1.66) | 0.420 | 1.21(1.11-1.33) | 0.596 | T | 5 | 45 | 0.49 (0.18-1.36) | 0.193 |
| TC | 5 | 31 | C | 29 | 129 | |||||||||
| CC | 12 | 49 | ||||||||||||
| FGG | rs2066865 | GG | 2 | 24 | 0.362 | 0.91 (0.29-2.87) | 1 | 0.35(0.07-1.65) | 0.228 | G | 14 | 87 | 0.70 (0.33-1.48) | 0.357 |
| GA | 10 | 39 | A | 20 | 87 | |||||||||
| AA | 5 | 24 | ||||||||||||
| SLC44A2 | rs2288904 | AA | 1 | 10 | 0.278 | 1.95 (0.63-6.01) | 0.291 | 0.48(0.06-4.03) | 0.687 | A | 13 | 58 | 1.24 (0.58-2.65) | 0.693 |
| AG | 11 | 38 | G | 21 | 116 | |||||||||
| GG | 5 | 39 | ||||||||||||
| KNG1 | rs710446 | CC | 1 | 7 | 0.950 | 0.90 (0.31-2.59) | 1 | 0.71(0.08-6.21) | 1 | C | 8 | 45 | 0.88 (0.37-2.09) | 1 |
| CT | 6 | 31 | T | 26 | 129 | |||||||||
| TT | 10 | 49 | ||||||||||||
| TSPAN15 | rs78707713 | CC | 0 | 0 | 0.163 | 15.91 (0.62-408) | 0.163 | -- | -- | C | 1 | 0 | 15.63 (0.62-392.2) | 0.164 |
| CT | 1 | 0 | T | 33 | 174 | |||||||||
| TT | 16 | 87 | ||||||||||||
| PROCR | rs867186 | GG | 0 | 0 | 0.208 | 2.45 (0.56-10.62) | 0.208 | -- | -- | G | 3 | 7 | 2.31 (0.57-9.42) | 0.212 |
| GA | 3 | 7 | A | 31 | 167 | |||||||||
| AA | 14 | 80 | ||||||||||||
| VKORC1 | rs9923231 | CC | 0 | 0 | 0.737 | 1.37 (0.39-4.74) | 0.737 | -- | -- | C | 4 | 16 | 1.32 (0.41-4.21) | 0.750 |
| CT | 4 | 16 | T | 30 | 158 | |||||||||
| TT | 13 | 71 | ||||||||||||
OR: odds ratio; CI: confidence interval
Furthermore, the effect of rs495828/rs2519093 genotype on cumulative incidence of thrombosis was also analyzed, as shown in Figure 1. For rs495828, patients with GT+TT genotype showed significant increased incidence of thrombotic events, compared with patients with GG genotype. Similarly, for rs2519093, TC+TT genotype had higher rate of thrombosis.
Figure 1. Cumulative incidence of thrombosis in PNH patients with different ABO genotypes.
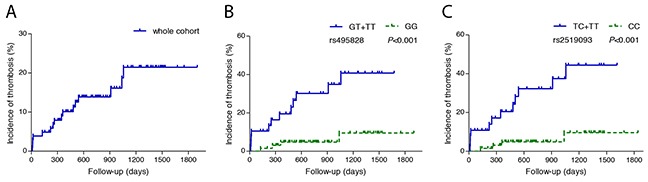
(A) whole cohort (B) thrombosis in different rs495828 genotypes, blue line represent PNH patients with genotype GT and genotype TT, green line represent PNH patients with genotype GG (C) thrombosis in different rs2519093 genotypes, blue line represent PNH patients with genotype TT and genotype TC, green line represent PNH patients with genotype CC.
Association between ABO haplotypes and thrombotic risk in PNH
In addition to single SNP analysis, haplotype analysis was also performed for the ABO gene. rs495828 and rs2519093 were in linkage disequilibrium (LD) (both D’ and r2 value ≥80), as shown in Figure 2. Thus, haplotype analysis of these two SNPs was further performed by SHEsis software. As shown in Table 3, the haplotype containing the rs495828 T and the rs2519093 T alleles displayed a significant association with increased risk of thrombosis (OR=3.25, 95%CI 1.43-7.39; P=0.004), the haplotype containing the rs495828 G and the rs2519093 C alleles associate with decreased risk of thrombosis (OR=0.28, 95%CI 0.13-0.64; P=0.002).
Figure 2. Linkage disequilibrium plots of ABO polymorphisms.
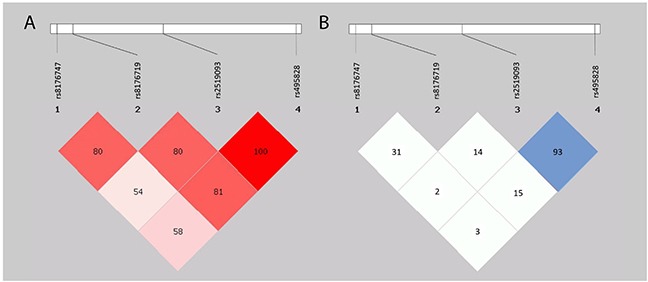
(A) Red squares indicate statistically significant associations between two SNPs which measured by D’; darker shades of red indicate higher D’. (B) Blue squares indicate statistically significant associations between two SNPs which measured by r2 value; darker shades of blue indicate higher r2 value.
Table 3. Haplotypes for the two SNPs in ABO gene and their associations with thrombosis risk in PNH patients.
| rs495828 | rs2519093 | Case (N=34), n (%) | Control (N=174), n (%) | OR (95%) | P value |
|---|---|---|---|---|---|
| G | C | 21 (62) | 148 (85) | 0.28 (0.13-0.64) | 0.002 |
| T | C | 1 (3) | 1 (1) | 5.24 (0.53-51.94) | 0.119 |
| T | T | 12 (35) | 25 (14) | 3.25 (1.43-7.39)) | 0.004 |
OR: odds ratio; CI: confidence interval.
Analysis of risk factors associated with thrombosis in PNH
In order to identify possible risk factors for thrombosis in PNH, different risk factors like age, gender, rate of bone marrow failure, PNH granulocyte clone size, LDH level, and polymorphism of ABO gene were analyzed. Only larger PNH clone and rs495828 GT/TT (or rs2519093 TC/TT) genotype was shown to be related with higher incidence of thrombosis. Multivariate regression analysis showed that larger PNH clone and rs495828 GT/TT (or rs2519093 TC/TT) genotype were independent risk factors for thrombosis in patients with PNH (Table 4).
Table 4. Univariate and multivariate regression analysis of risk factors associated with thrombosis in PNH.
| Parameters | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Age | ||||
| ≥40 years/<40 year | 0.36 (0.12-1.12) | 0.077 | ||
| Gender | ||||
| male/female | 0.96 (0.34-2.71) | 0.935 | ||
| Bone marrow failure | ||||
| with/without | 1.75 (0.62-4.99) | 0.292 | ||
| PNH granulocyte clone size | 9.29 (1.14-75.75)# | 0.037# | ||
| >50%/≤50% | 9.78 (1.24-77.19) | 0.031 | 9.60 (1.17-78.60)* | 0.035* |
| LDH | ||||
| ≥1.5 ULN/<1.5 ULN/ | 2.09 (0.43-10.11) | 0.360 | ||
| rs495828 | ||||
| GT+TT/GG | 5.63 (1.80-17.60) | 0.003 | 5.41 (1.67-17.52)# | 0.005# |
| rs2519093 | ||||
| TC+TT/CC | 5.95 (1.90-18.65) | 0.002 | 5.87 (1.81-19.10)* | 0.003* |
OR: odds ratio; CI: confidence interval, # analyzed PNH clone size and rs495828; * analyzed PNH clone size and rs2519093.
Association between ABO polymorphism and plasma levels of vWF: Ag and VIII: C
Patients carrying rs495828 GT/TT phenotype had a significant higher level of vWF:Ag and VIII: C compared with those carrying rs495828 GG phenotype (vWF:Ag:179±42 IU/dl vs.138±43 IU/dl, P=0.031; VIII: C:211±60% vs.148±36%, P=0.009, respectively; Figure 3). Similarly, Patients carrying rs2519093 TC+TT phenotype had a significant higher level of vWF:Ag and VIII: C compared with those carrying CC phenotype (vWF:Ag: 186±38 IU/dl vs. 136±42 IU/dl, P=0.014; VIII: C: 218±59% vs. 148±35%, P=0.004, respectively; Figure 3). Meanwhile, there were no significant correlation between LDH level, PNH clone, platelet counts and plasma levels of vWF:Ag and VIII:C among these patients (Supplementary Figure 1). Further, the PNH cohort had significant higher plasma levels of vWF and factor VIII compared with normal controls (vWF:Ag: 156±47 IU/dl vs. 127±45 IU/dl, P=0.039; VIII: C: 176±57% vs. 129±50%, P=0.005, respectively; Figure 3).
Figure 3. Plasma levels of vWF: Ag and VIII: C.
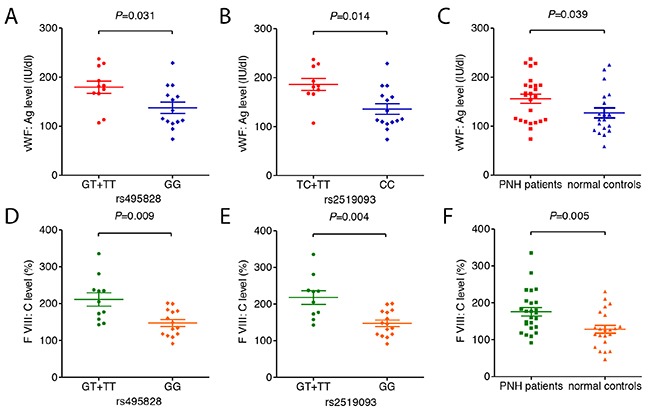
(A) vWF:Ag between PNH patients with different rs495828 genotypes. (B) vWF:Ag between PNH patients with different rs2519093 genotypes. (C) vWF:Ag level between PNH patients and normal controls. (D) VIII: C level between PNH patients with different rs495828 genotypes. (E) VIII: C level between PNH patients with different rs2519093 genotypes. (F) VIII: C level between PNH patients and normal controls. Data are presented as mean ± Standard deviation.
DISCUSSION
In our study, 17 (16.3%) of 104 patients were found to have at least one episode of thrombotic event. Although thrombotic rate is much lower in Asian people than in western people, thromboembolism is still the major cause of severe morbidities and early mortality in PNH patients. Several studies have outlined some possible mechanisms which can lead to thrombosis in patients with PNH. Hall et al. demonstrated that patients with large PNH granulocyte clone (>50%) had higher thrombotic incidence compared with those with smaller PNH clone, large PNH granulocyte clones are predictive of venous thrombosis [22]. Moyo et al. confirmed the association and indicated the risk of thromboembolic events increases by 1.64-fold for every 10% increase in clone size [7]. Lee and colleagues had shown that patients with elevated hemolysis (LDH levels large than 1.5 times the upper limit of normal) at diagnosis were at significant higher risk for thrombosis [8]. However, thrombosis can sometimes occur in patients with small PNH clone, or minor presentations of hemolysis. So there may have some other factors rather than PNH clone size which affect the thromboembolic balance in PNH patients. In some other studies, ethnicity, elevation of D-dimer, transfusion dependence, age more than 55 years were described as risk factors for thrombosis [13, 23, 24], but the results of these risk factors have not been confirmed by other investigators.
To the best of our knowledge, this is the first study to investigate the genetic risk of thromboembolism in patients with PNH. Twenty-six SNPs in 17 genes which had been identified previously to be associated with high risk of venous thromboembolism were selected in this study. These genes encode proteins affect function of coagulation factors, anticoagulation factors, endothelial cells and platelet. The results demonstrated that two SNPs in ABO gene, rs495828 and rs2519093, had strong correlation with thrombosis in PNH, the minor alleles of the two SNPs were associated with 5.95 and 6.3 fold increase risk of thrombus formation, compared with major alleles. Haplotype analysis displayed that the combination of twp SNPs could correlation with the thrombosis risk in PNH, an increased risk of thrombosis was observed for the haplotype containing the rs495828 T and the rs2519093 T alleles of the ABO gene in PNH patients. Multivariate regression analysis showed that genotype with minor allele of rs495828/rs2519093 and PNH clone size were independent risk factors for thrombosis in PNH. rs2519093, rs495828, rs8176719 in ABO gene has been demonstrated to be related with venous thromboembolism by Heit and colleagues [25, 26], but it is the first time to be shown in patients with PNH. Rs495828 locates on the ABO exon 7 region, thus affects ABO gene expression. While rs2519093 locates on the ABO intron 1 region, which does not affect RNA splicing or harbor any suppressor RNA elements, nor is it in linkage disequilibrium (LD) with or closes to known variants in ABO exon 6 and 7 according to previous studies [25, 27]. In this study, the result of haplotype analysis firstly demonstrated rs2519093 were in LD with functional variant (rs495828).
Polymorphism of ABO gene could affect the ABO-mediated glycosylation of vWF, thus impact on the plasma levels of vWF and factor VIII. Previous studies had demonstrated that some ABO polymorphism correlates with plasma levels ofvWF and factor VIII: people with rs8176719 ABO gene deletion (O blood type) have approximately 25% lower level of vWF and factor VIII than those without rs8176719 deletion (non-O blood type) [21, 28]. We then speculated the correlation between the rs495828/rs2519093 polymorphism in ABO gene and the levels ofvWF and factor VIII, and found that patients carrying the rs495828/rs2519093 minor allele had an approximately 30% higher level of vWF: Ag and 40% higher level of VIII: C compared with those carrying the major allele. It has been addressed that patients with PNH have higher level of vWF [13], as being demonstrated in our study as well, additionally the level of factor VIII also higher in PNH patients, and higher level of vWF and factor VIII is related with higher risk of thrombosis [29, 30]. Considered the level of vWF and factor VIII may be affected by the function of platelets and endothelial cells, and intravascular hemolysis is the most important factor for the activation of platelets and endothelial cells in PNH [6], we detected the correlation between the PNH clone, LDH level (correlated with intravascular hemolysis), platelet counts, and the level of vWF and factor VIII in patients with PNH, and found no significant correlations (Supplementary Figure 1). In brief, although many other reasons such as endothelial cell activation and damage from hemolysis could also contribute to higher level of vWF and factor VIII, our data strongly suggested that the polymorphism of ABO rs495828/rs2519093 probably play a key role, and thus contribute the thrombus formation.
Our findings clearly demonstrate that the rs495828/rs2519093 polymorphism in ABO gene represent an independent risk factor in PNH patients for thromboembolism, the mechanism for the associations probably involved in the regulation of plasma level of vWF and factor VIII. However, further studies with larger patient population and longer follow-up duration to verify the conclusions are needed.
MATERIALS AND METHODS
Patients
There were totally 104 PNH patients from February, 2011 to August, 2016 in Peking union medical college hospital (PUMCH) enrolled in the study. All patients were confirmed diagnosis through classical symptoms in combination with the proportion of fluorescent aerolysin (FLAER) negative granulocytes higher than 1% [31, 32]. Clinical data including age, sex, clinical symptoms including hemolysis were captured. Laboratory tests including PNH clone size by CD59 and FLAER assay, complete blood count, reticulocyte count, lactate dehydrogenase (LDH) levels, serum bilirubin levels, and thrombophilia risk factors like protein C, protein S, fibrinogen, D-Dimer and antithrombin were detected at the time of the first diagnosis. Thrombotic events were monitored form first diagnosis to December, 2016. This study was performed in accordance with relevant guidelines and was approved by the PUMCH Ethics Committee. Informed consent was obtained from each patient.
Genotyping
Whole blood samples of 104 patients were collected into tubes containing ethylene diaminetetraacetic acid. Genomic DNA from whole blood was extracted with DNA purification kits (Qiangen, Hilden, Germany). The DNA concentration was measured by spectrometry. Twenty-six SNPs in 17 genes including MTHFR, PROC, PROS, F2, F5, ABO, Prothrombin and other genes (shown in Supplementary Table 1) which had been reported as high risk factors were selected for the present study. SNPs were genotyped using the Sequenom MassARRAY system (Sequenom, Inc, San Diego, CA, USA) according to the manufactory protocol. The Primers used for SNPs in this study were listed in Supplementary Table 2.
Examination of vWF:Ag and VIII:C
Twenty-five PNH patients (11 patients with rs495828 GT/TT genotype, 14 patients with GG genotype) in this study who came back for follow-up were tested for the plasma levels of vWF:Ag and VIII:C through a one stage clotting assay and an enzyme-linked immunosorbent assay (ELISA). Equal number of age and gender matched health were recruited as normal controls and their plasma levels of vWF:Ag and VIII:C were also tested.
Statistical analysis
Statistical analysis was performed using SPSS 19.0 software. Hardy-Weinberg equilibrium (HWE) was evaluated by comparing expected and observed frequencies using Online Encyclopedia for Genetic Epidemiology HWE tool (OEGE) (http://www.oege.org/software/hwe-mr-calc.shtml) [33]. The observed genotype frequencies were compared to expected values calculated from HWE theory (p2 + 2pq + q2 = 1; where p is the frequency of the major allele and q is the frequency of the minor allele) by using the chi-squared test. Linkage disequilibrium (LD) and haplotypes analyses were carried out using SHEsis (http://analysis2.bio-x.cn/myAnalysis.php) [34]. Continuous variables were represented as mean ± Standard deviation. Pearson's chi-squared test or fisher exact test was used to determine whether there was any significant difference in allele and genotype frequencies between PNH patients with or without thrombosis. OR with 95% CI was used to assess the association between the studied SNPs and thromboembolism. Student's t-test (data were normal contributed) or Mann-Whitney U test (data were not normal contributed) and fisher exact test were used to evaluate the correlation between the thrombus formation and the clinical parameters. The influence of genotypes on cumulative incidence of thrombosis was analyzed by the Kaplan-Meier method with log-rank test. Risk factors were identified by univariate and multivariate logistic regression. For all tests, a two-sided P value less than 0.05 was considered as statistically significant.
SUPPLEMENTARY MATERIALS FIGURES AND TABLES
Acknowledgments
We thank all patients who consented to disclose their medical records and answered our review calls. Their cooperation and helpful comments throw light upon our data collection and statistical analysis. This study was supported by grants from the Chinese Academy of Medical Sciences innovation fund for medical sciences (2016-I2M-3-004).
Footnotes
Author contributions
Z.L. and B.H. designed the study and wrote the manuscript. Z.L. and Y.D. collected samples, performed genotyping and analyzed data. H.L. helped to perform genotyping. All authors reviewed the manuscript. Z.L., Y.D., H.L. and B.H. approved the final version of the manuscript.
CONFLICTS OF INTEREST
The authors declare no competing financial interests.
REFERENCES
- 1.Sahin F, Ozkan MC, Mete NG, Yilmaz M, Oruc N, Gurgun A, Kayikcioglu M, Guler A, Gokcay F, Bilgir F, Ceylan C, Bilgir O, Sari IH, Saydam G. Multidisciplinary clinical management of paroxysmal nocturnal hemoglobinuria. American journal of blood research. 2015;5:1–9. [PMC free article] [PubMed] [Google Scholar]
- 2.Brodsky RA. Narrative review: paroxysmal nocturnal hemoglobinuria: the physiology of complement-related hemolytic anemia. Annals of internal medicine. 2008;148:587–595. doi: 10.7326/0003-4819-148-8-200804150-00003. [DOI] [PubMed] [Google Scholar]
- 3.Brodsky RA. Paroxysmal nocturnal hemoglobinuria. Blood. 2014;124:2804–2811. doi: 10.1182/blood-2014-02-522128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parker C, Omine M, Richards S, Nishimura J, Bessler M, Ware R, Hillmen P, Luzzatto L, Young N, Kinoshita T, Rosse W, Socie G, International PNH Interest Group Diagnosis and management of paroxysmal nocturnal hemoglobinuria. Blood. 2005;106:3699–3709. doi: 10.1182/blood-2005-04-1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hillmen P, Muus P, Duhrsen U, Risitano AM, Schubert J, Luzzatto L, Schrezenmeier H, Szer J, Brodsky RA, Hill A, Socie G, Bessler M, Rollins SA, et al. Effect of the complement inhibitor eculizumab on thromboembolism in patients with paroxysmal nocturnal hemoglobinuria. Blood. 2007;110:4123–4128. doi: 10.1182/blood-2007-06-095646. [DOI] [PubMed] [Google Scholar]
- 6.Hill A, Kelly RJ, Hillmen P. Thrombosis in paroxysmal nocturnal hemoglobinuria. Blood. 2013;121:4985–4996. doi: 10.1182/blood-2012-09-311381. quiz 5105. [DOI] [PubMed] [Google Scholar]
- 7.Moyo VM, Mukhina GL, Garrett ES, Brodsky RA. Natural history of paroxysmal nocturnal haemoglobinuria using modern diagnostic assays. Br J Haematol. 2004;126:133–138. doi: 10.1111/j.1365-2141.2004.04992.x. [DOI] [PubMed] [Google Scholar]
- 8.Lee JW, Jang JH, Kim JS, Yoon SS, Lee JH, Kim YK, Jo DY, Chung J, Sohn SK. Clinical signs and symptoms associated with increased risk for thrombosis in patients with paroxysmal nocturnal hemoglobinuria from a Korean Registry. International journal of hematology. 2013;97:749–757. doi: 10.1007/s12185-013-1346-4. [DOI] [PubMed] [Google Scholar]
- 9.Yu F, Du Y, Han B. A comparative analysis of clinical characteristics of patients with paroxysmal nocturnal hemoglobinuria between Asia and Europe/America. International journal of hematology. 2016;103:649–654. doi: 10.1007/s12185-016-1995-1. [DOI] [PubMed] [Google Scholar]
- 10.Schrezenmeier H, Muus P, Socie G, Szer J, Urbano-Ispizua A, Maciejewski JP, Brodsky RA, Bessler M, Kanakura Y, Rosse W, Khursigara G, Bedrosian C, Hillmen P. Baseline characteristics and disease burden in patients in the International Paroxysmal Nocturnal Hemoglobinuria Registry. Haematologica. 2014;99:922–929. doi: 10.3324/haematol.2013.093161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meppiel E, Crassard I, Peffault de Latour R, de Guibert S, Terriou L, Chabriat H, Socie G, Bousser MG. Cerebral venous thrombosis in paroxysmal nocturnal hemoglobinuria: a series of 15 cases and review of the literature. Medicine. 2015;94:e362. doi: 10.1097/MD.0000000000000362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ziakas PD, Poulou LS, Pomoni A. Thrombosis in paroxysmal nocturnal hemoglobinuria at a glance: a clinical review. Current vascular pharmacology. 2008;6:347–353. doi: 10.2174/157016108785909742. [DOI] [PubMed] [Google Scholar]
- 13.Helley D, de Latour RP, Porcher R, Rodrigues CA, Galy-Fauroux I, Matheron J, Duval A, Schved JF, Fischer AM, Socie G, French Society of Hematology Evaluation of hemostasis and endothelial function in patients with paroxysmal nocturnal hemoglobinuria receiving eculizumab. Haematologica. 2010;95:574–581. doi: 10.3324/haematol.2009.016121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Van Bijnen ST, Van Heerde WL, Muus P. Mechanisms and clinical implications of thrombosis in paroxysmal nocturnal hemoglobinuria. Journal of thrombosis and haemostasis. 2012;10:1–10. doi: 10.1111/j.1538-7836.2011.04562.x. [DOI] [PubMed] [Google Scholar]
- 15.Devalet B, Mullier F, Chatelain B, Dogne JM, Chatelain C. The central role of extracellular vesicles in the mechanisms of thrombosis in paroxysmal nocturnal haemoglobinuria: a review. Journal of extracellular vesicles. 2014;3 doi: 10.3402/jev.v3.23304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tang L, Hu Y. Ethnic diversity in the genetics of venous thromboembolism. Thrombosis and haemostasis. 2015;114:901–909. doi: 10.1160/TH15-04-0330. [DOI] [PubMed] [Google Scholar]
- 17.Soria JM, Morange PE, Vila J, Souto JC, Moyano M, Tregouet DA, Mateo J, Saut N, Salas E, Elosua R. Multilocus genetic risk scores for venous thromboembolism risk assessment. Journal of the American Heart Association. 2014;3:e001060. doi: 10.1161/JAHA.114.001060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morange PE, Suchon P, Tregouet DA. Genetics of Venous Thrombosis: update in 2015. Thrombosis and haemostasis. 2015;114:910–919. doi: 10.1160/TH15-05-0410. [DOI] [PubMed] [Google Scholar]
- 19.Yamamoto F, McNeill PD, Hakomori S. Genomic organization of human histo-blood group ABO genes. Glycobiology. 1995;5:51–58. doi: 10.1093/glycob/5.1.51. [DOI] [PubMed] [Google Scholar]
- 20.McGrath RT, McKinnon TA, Byrne B, O'Kennedy R, Terraube V, McRae E, Preston RJ, Laffan MA, O'Donnell JS. Expression of terminal alpha2-6-linked sialic acid on von Willebrand factor specifically enhances proteolysis by ADAMTS13. Blood. 2010;115:2666–2673. doi: 10.1182/blood-2009-09-241547. [DOI] [PubMed] [Google Scholar]
- 21.Souto JC, Almasy L, Muniz-Diaz E, Soria JM, Borrell M, Bayen L, Mateo J, Madoz P, Stone W, Blangero J, Fontcuberta J. Functional effects of the ABO locus polymorphism on plasma levels of von Willebrand factor, factor VIII, and activated partial thromboplastin time. Arteriosclerosis, thrombosis, and vascular biology. 2000;20:2024–2028. doi: 10.1161/01.atv.20.8.2024. [DOI] [PubMed] [Google Scholar]
- 22.Hall C, Richards S, Hillmen P. Primary prophylaxis with warfarin prevents thrombosis in paroxysmal nocturnal hemoglobinuria (PNH) Blood. 2003;102:3587–3591. doi: 10.1182/blood-2003-01-0009. [DOI] [PubMed] [Google Scholar]
- 23.de Latour RP, Mary JY, Salanoubat C, Terriou L, Etienne G, Mohty M, Roth S, de Guibert S, Maury S, Cahn JY, Socie G, French Society of Hematology, French Association of Young Hematologists Paroxysmal nocturnal hemoglobinuria: natural history of disease subcategories. Blood. 2008;112:3099–3106. doi: 10.1182/blood-2008-01-133918. [DOI] [PubMed] [Google Scholar]
- 24.Nishimura J, Kanakura Y, Ware RE, Shichishima T, Nakakuma H, Ninomiya H, Decastro CM, Hall S, Kanamaru A, Sullivan KM, Mizoguchi H, Omine M, Kinoshita T, Rosse WF. Clinical course and flow cytometric analysis of paroxysmal nocturnal hemoglobinuria in the United States and Japan. Medicine. 2004;83:193–207. doi: 10.1097/01.md.0000126763.68170.46. [DOI] [PubMed] [Google Scholar]
- 25.Heit JA, Cunningham JM, Petterson TM, Armasu SM, Rider DN, DE Andrade M. Genetic variation within the anticoagulant, procoagulant, fibrinolytic and innate immunity pathways as risk factors for venous thromboembolism. Journal of thrombosis and haemostasis. 2011;9:1133–1142. doi: 10.1111/j.1538-7836.2011.04272.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Heit JA, Armasu SM, Asmann YW, Cunningham JM, Matsumoto ME, Petterson TM, De Andrade M. A genome-wide association study of venous thromboembolism identifies risk variants in chromosomes 1q24.2 and 9q. Journal of thrombosis and haemostasis. 2012;10:1521–1531. doi: 10.1111/j.1538-7836.2012.04810.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu O, Bayoumi N, Vickers MA, Clark P. ABO(H) blood groups and vascular disease: a systematic review and meta-analysis. Journal of thrombosis and haemostasis. 2008;6:62–69. doi: 10.1111/j.1538-7836.2007.02818.x. [DOI] [PubMed] [Google Scholar]
- 28.Ohira T, Cushman M, Tsai MY, Zhang Y, Heckbert SR, Zakai NA, Rosamond WD, Folsom AR. ABO blood group, other risk factors and incidence of venous thromboembolism: the Longitudinal Investigation of Thromboembolism Etiology (LITE) Journal of thrombosis and haemostasis. 2007;5:1455–1461. doi: 10.1111/j.1538-7836.2007.02579.x. [DOI] [PubMed] [Google Scholar]
- 29.Timp JF, Lijfering WM, Flinterman LE, van Hylckama Vlieg A, le Cessie S, Rosendaal FR, Cannegieter SC. Predictive value of factor VIII levels for recurrent venous thrombosis: results from the MEGA follow-up study. Journal of thrombosis and haemostasis. 2015;13:1823–1832. doi: 10.1111/jth.13113. [DOI] [PubMed] [Google Scholar]
- 30.Shahidi M. Thrombosis and von Willebrand Factor. Advances in experimental medicine and biology. 2017;906:285–306. doi: 10.1007/5584_2016_122. [DOI] [PubMed] [Google Scholar]
- 31.Parker CJ. Update on the diagnosis and management of paroxysmal nocturnal hemoglobinuria. Hematology. American Society of Hematology. Education Program. 2016;2016:208–216. doi: 10.1182/asheducation-2016.1.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Borowitz MJ, Craig FE, Digiuseppe JA, Illingworth AJ, Rosse W, Sutherland DR, Wittwer CT, Richards SJ. Clinical Cytometry Society. Guidelines for the diagnosis and monitoring of paroxysmal nocturnal hemoglobinuria and related disorders by flow cytometry. Cytometry. Part B, Clinical cytometry. 2010;78:211–230. doi: 10.1002/cyto.b.20525. [DOI] [PubMed] [Google Scholar]
- 33.Rodriguez S, Gaunt TR, Day IN. Hardy-Weinberg equilibrium testing of biological ascertainment for Mendelian randomization studies. American journal of epidemiology. 2009;169:505–514. doi: 10.1093/aje/kwn359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li Z, Zhang Z, He Z, Tang W, Li T, Zeng Z, He L, Shi Y. A partition-ligation-combination-subdivision EM algorithm for haplotype inference with multiallelic markers: update of the SHEsis ( http://analysis.bio-x.cn) Cell research. 2009;19:519–523. doi: 10.1038/cr.2009.33. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


