Abstract
Context:
Tumors of the central nervous system (CNS) constitute the second most common pediatric cancers. Unlike leukemia, management of CNS tumors requires a good multidisciplinary team. Higher rates of treatment abandonment are documented in view of complexity of the treatment with long duration, involving neurosurgery, radiation, chemotherapy, and high cost of treatment. Morbidity associated with CNS tumors may be significant in terms of physical deficits as well as neuropsychological and neuroendocrine sequelae. Pediatric neurooncology is still at a very nascent stage in the developing countries. There are only a few reports on the multidisciplinary approach and outcomes of pediatric brain tumors in developing countries.
Aims:
The aim of this study is to identify the clinicopathological profile of Pediatric CNS tumors in a tertiary care center located in South India in comparison with reports from other low-and middle-income Countries.
Settings and Design:
A retrospective analysis of medical records of all children diagnosed with brain tumors from January 2012 to November 2016 at our institute was done.
Subjects and Methods:
A retrospective study of clinical, pathological profile, and outcomes of children <18 years diagnosed with brain tumors at our institute from January 2012 to November 2016 was done. Histopathological categorization was done as per the WHO classification 2007. The multidisciplinary treatment with respect to surgery, radiation, and chemotherapy was noted and the outcomes were recorded.
Statistical Analysis Used:
R for Statistical Computing (Version 3.0.2; 2013-09-25).
Results:
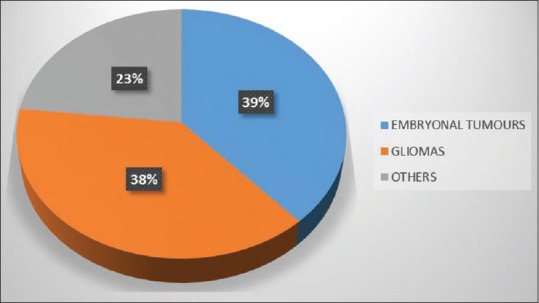
A total of 52 children were diagnosed with male preponderance of 66.6%. Highest incidence was noted in the age group of 0–4 years (50%). Majority of them were supratentorial (59.6%). CNS embryonal tumors contributed to 48% of all our brain tumors. 73% of them underwent either resection or biopsy. Eight (15.3%) of them died due to the progression of disease, but 44% abandoned treatment due to the progression/recurrence of disease. Those lost to follow-up were mostly among the high-risk groups with poor prognosis such as pontine glioma, medulloblastoma (high risk), and primitive neuroectodermal tumor.
Conclusions:
Although brain tumors constituted 30% of all our solid tumors, only 56% of them received appropriate treatment and 25% abandoned treatment. High rates of abandonment were a consequence of late diagnosis, complex multidisciplinary treatment involved, high treatment cost, lack of uniformity in management between different oncology centers and poor prognosis of the tumor subtype.
KEYWORDS: Childhood brain tumors, low- income country, outcomes
INTRODUCTION
Annual incidence of childhood brain tumors is about 3/100,000 children.[1] Pediatric brain tumors are implicated as the most common cause of cancer deaths in children.[2] Around 20% of all cancers under 15 years of age are due to central nervous system (CNS) tumors.[3] The incidence of CNS tumors in the US has shown an increase from 3.45/100,000 thousand years in 1994 to about 4.92/100,000 person-years.[4,5] Topographical variations in incidence rates have been noted with the Western population reporting a higher incidence (30 per million person-years) as compared to Africa (10 per million years) and Asia (15 per million years).[3] As per available Indian data, brain tumors constitute about 11.4%–20.1% of all childhood tumors.[6,7,8,9]
SUBJECTS AND METHODS
Ours is a 200-bed pediatric tertiary care center in South India which receives patients from all parts of the country. The Department of Pediatric Oncology at our institute was started in 2010. We see about 100–150 new patients with cancer each year. The Departments of Pediatric Surgery, Neurosurgery, Intensive care, and Endocrinology are fully functional. We also have a Radiation Oncologist as a visiting consultant, and those requiring radiation are sent to another institute close by. We have monthly tumor board meetings to discuss complex cases and get inputs from experts in different specialities and make individualized plans for each patient after consensus.
A retrospective analysis of case records and neurosurgical operative records of all patients younger than 18 years diagnosed with CNS tumors from January 2012 to November 2016 at the Department of Pediatric Haematology and Oncology was done. Details of age, gender, clinical presentation, investigations, histopathology, and treatment given including the extent of surgery, chemotherapy, and radiation along with outcomes were recorded. All patients were divided into three subgroups based on age as 0–4 years, 5–9 years, and 10–18 years. Biopsy specimens were sent to National Institute of Mental Health and Neurosciences, which is a premier multidisciplinary central government institute in the field of mental health and neurosciences for reporting. Histopathological categorization was done as per the WHO 2007 Classification of brain tumors.
Literature review was done through NCBI PubMed database with the terms “Pediatric brain tumors”, “childhood brain tumors”, “developing country” “Lower Middle income countries” to find similar studies from low- and middle-income countries were done. Country income categorization was done as per the World Bank List of Economies (July 2016). Data analysis was done using R for Statistical Computing (Version 3.0.2; 2013-09-25).
RESULTS
Demographics and clinical presentation
Out of the 52 cases of pediatric brain tumors diagnosed at our institute from January 2012 to November 2016, 26 (50%) were in the age group of 0–4 years. The mean age of distribution among both sexes was 4 years. There were 37 (71%) boys and 15 (29%) girls. The overall male/female ratio was 2.5:1. Male preponderance was seen in all tumors except Ependymomas (1:1.5) as shown in Figure 1.
Figure 1.
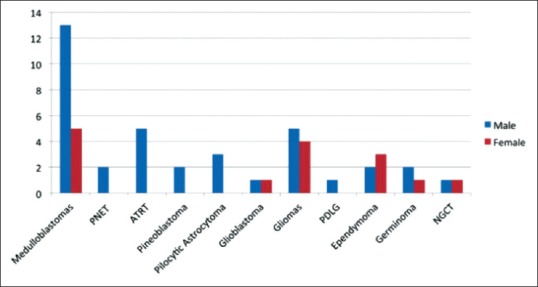
Gender-wise distribution of central nervous system tumors. PNET: Primitive neuro-ectodermal tumor, ATRT: Atypical teratoid rhabdoid tumor, PDLG: Primary diffuse leptomeningeal gliomatosis, NGCT: Nongerminomatos germ cell tumor
Clinical features
The most common clinical presentation noted in our study was vomiting (25, 62.5%) followed by headache 15 (37.5%) and impaired vision 14 (35%) as shown in Table 1. Average time from symptom onset to seeking medical attention was >3 months in about 40.3%[10] as shown in Table 2.
Table 1.
Clinical features of pediatric central nervous system tumours (n=52)
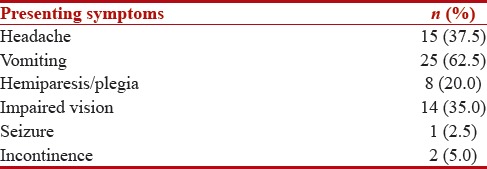
Table 2.
Time to presentation following symptoms (n=52)
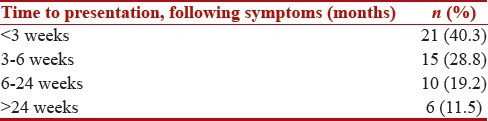
The disease frequency across different age groups is showed in Table 3. Medulloblastomas, primitive neuroectodermal tumor, atypical teratoid rhabdoid tumor (ATRT) and ependymomas were most commonly seen in of 0–4 years in the 5-9 years age group; however, the most common tumors were low-grade gliomas followed by medulloblastoma. In the 10–17 years age group, medulloblastoma was the most common tumor.
Table 3.
Distribution of central nervous system tumors
Type of tumor and location
As per the WHO 2007 Classification, in this case series, the most common tumor was Medulloblastoma 18 (34.6%) as shown in Table 3. Other common tumors were astrocytomas (15, 28.8%) followed by ependymomas (5, 9.6%). Figure 2 shows the WHO grading reported in 33 tumors out of which Grade IV were 23 (69%). Of the 52 tumors, 31 (59.6%) were supratentorial, and 21 (40.4%) were infratentorial. There were no primary CNS tumors localized to the spine in our study.
Figure 2.
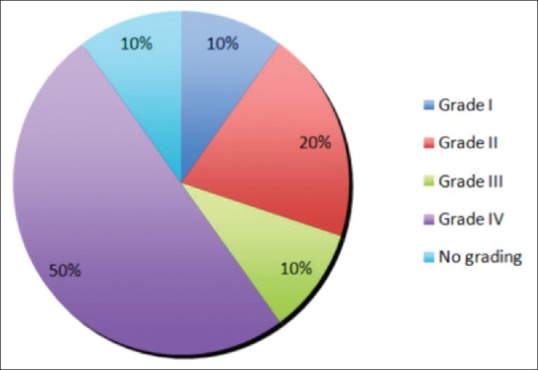
Distribution according to the WHO grading of central nervous system tumors
Medulloblastoma was the most common tumor noted in our case series with nearly 90%[11] of them belonging to the desmoplastic subtype.
Among the Astrocytomas, low-grade gliomas were the most common (9, 17.3%) and pilocytic astrocytoma constituted to only about 5.7%[3] of all the CNS tumors. We had only two cases of Glioblastoma Multiforme in our study belong to the 5–9 years age group.
Among the ependymal tumors (5, 9.6%), all five were ependymomas belonging to the 0–5 years age group.
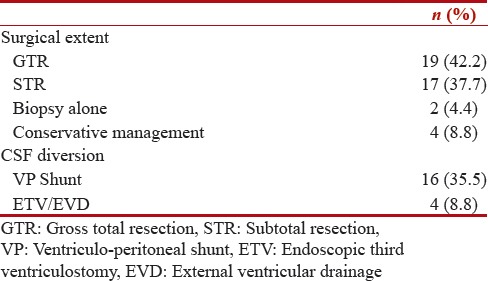
Operative characteristics
Surgical resection was done in 36 (69%) of patients as shown in Table 4. Gross total resection was reported in 52.7%, and subtotal resection was reported in 37.7% of all surgical resections. Biopsy alone was done in 5.5%, and no surgery was done in 4.1% of cases. CSF diversion procedure was done in about 20 cases out of which 16 cases required Ventriculoperitoneal shunt and 4 cases required Endoscopic Third Ventriculostomy as shown in Table 4.
Table 4.
Operative characteristics of patients with central nervous system tumors (n=45)
Out of the 52 patients, 28 (53.8%) patients received radiotherapy either IMRT or IGRT based on affordability and two patients abandoned radiotherapy midway. A total of 26 (50%) patients received chemotherapy as per Children's Oncology Group protocols. Nine (17.3%) did not require any chemotherapy after surgery and radiotherapy.
Outcomes
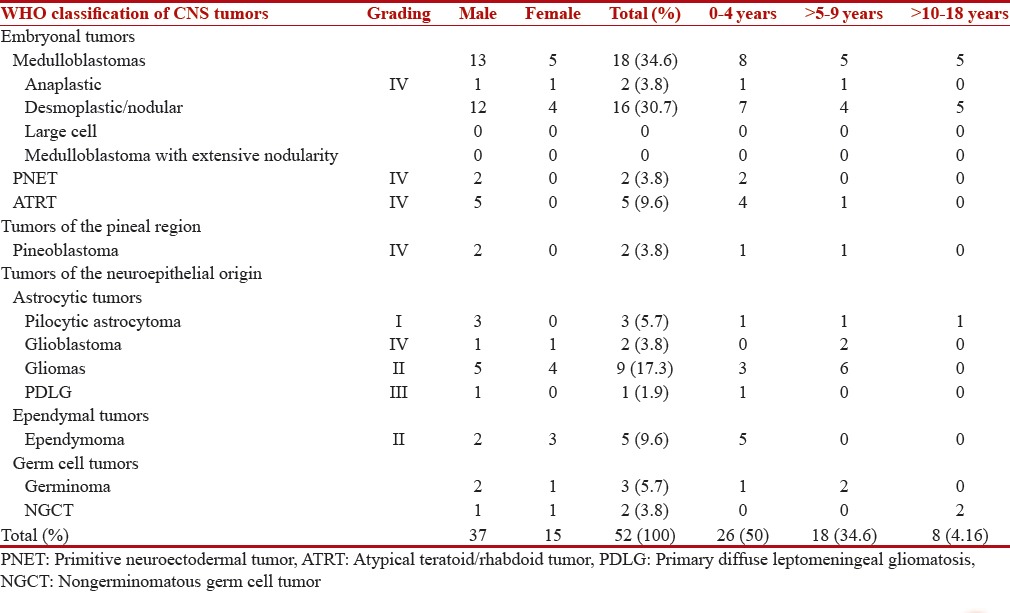
Out of 52 cases diagnosed at our institute, 9 patients were referred to other centers after the diagnosis as shown in Table 5. There were 8 deaths (15.3%) in our study with highest mortality in ATRT where 3 out of 5 children diagnosed had a fatal outcome. 13 patients (25%) were lost to follow-up. Moreover, 17 patients (32.6%) have completed treatment and are on regular follow-up, and 6 (11.53%) are currently on treatment. A total of 13 (25%) out of 52 patients abandoned treatment out of which five (9.6%) were low-grade gliomas, and three (5.7%) were medulloblastomas as shown in Figure 3. Survival is represented by Kaplan–Meier curves in Figure 4.
Table 5.
Outcomes of central nervous system tumors
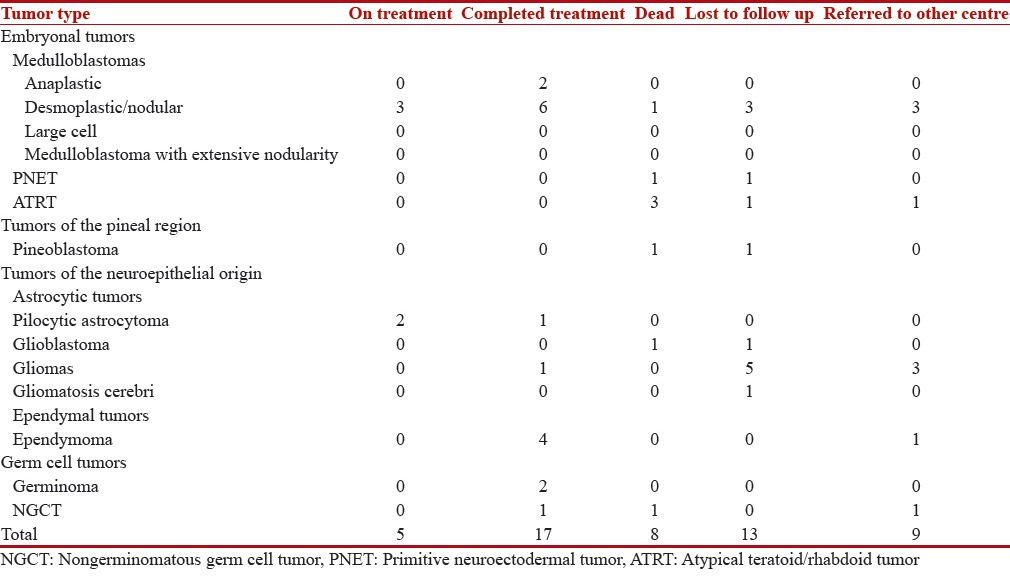
Figure 3.
Distribution according to abandonment
Figure 4.
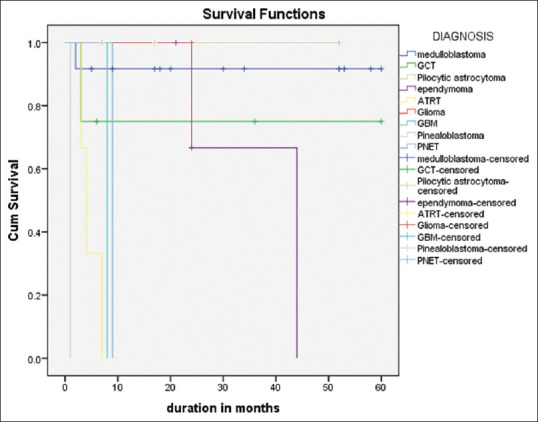
Kaplan–Meier survival curves
DISCUSSION
As per the American Cancer Society 2016 facts and figures, incidence of childhood cancer has gradually increased by 0.6% per year since 1975. Brain and other CNS tumors rank second among childhood cancers (26%) after leukemias (30%) in the 0–14 years age group. About 4,300 children are diagnosed with primary central nervous tumors annually as per the Central Brain Tumor Registry of the United States (CBTRUS).[12] In India, 55%–120% increase in incidence of childhood brain tumors has been noted in the both the sexes over the past 25 years.[6] Various explanations have been proposed for this increase in incidence, most important of which is the use of magnetic resonance imaging for the diagnosis of intracranial abnormalities.[4]
The road to diagnosis of brain tumors is often difficult as many of the clinical symptoms mimic those of common childhood ailments. Based on location, age and aggressiveness of the tumor clinical signs may vary, and it requires a high degree of suspicion, and prompt evaluation which is often not the case and the diagnosis is delayed. Correct diagnosis and staging are required for the selection of the most appropriate therapy requiring coordinated efforts of multiple pediatric specialists in the fields of neurosurgery, radiation oncology, neurooncology, endocrinology, psychology, neuroradiology, and rehabilitation.
Ours is an exclusive pediatric tertiary care hospital and academic center located in Chennai, South India. It is a 200-bedded hospital with a fully equipped Pediatric Neurosurgery and Pediatric Oncology Department. However, we refer the patients to other institutions for imaging and radiotherapy. We observed that limited data are available from low- and middle-income countries with regard to the incidence and outcomes of pediatric CNS tumors. We have conducted the present study to better understand the demographics, presentation and outcomes of the same in comparison with other nations as shown in Figure 5. We recorded significant differences in our experience with pediatric CNS tumors and also notable similarities as shown in Table 6.
Figure 5.
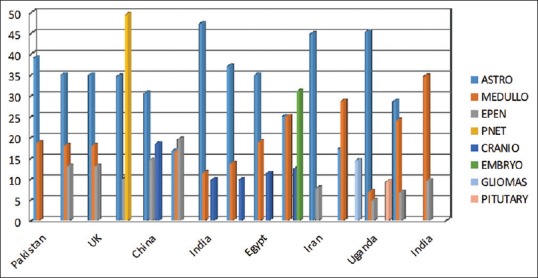
Literature review from other countries
Table 6.
Literature review from other countries
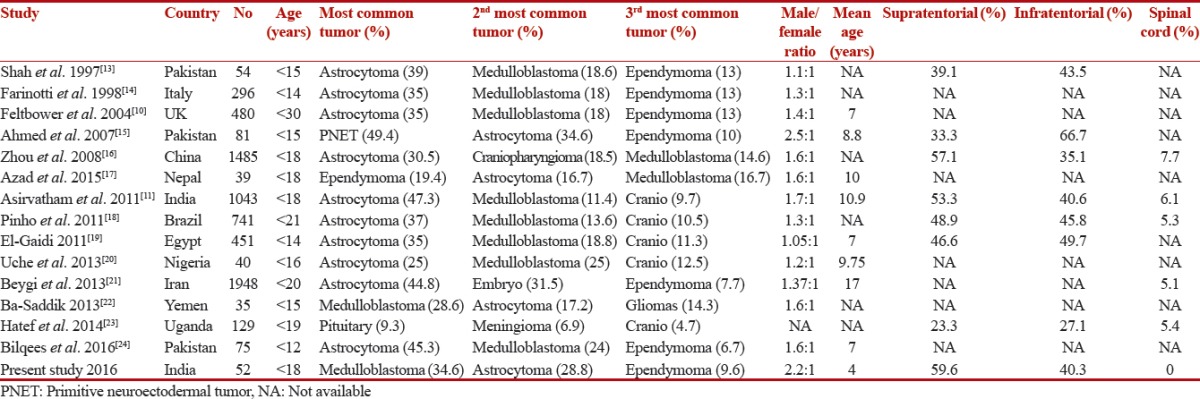
In our study of 52 cases of pediatric brain tumors from 2012 to 2016, Embryonal tumors constituted the highest proportion. 34.6% of the tumors were medulloblastomas, followed by astrocytic tumors (28.8%) and ependymomas (9.6%). Medulloblastomas were the most common tumor (28.6%) reported by a similar study from Yemen.[22] Annual incidence rate of 6.8 per million children (0–14 years) was reported from Europe for the period 2000-2007 with 15%–20% of all CNS tumors being Medulloblastomas (RARECAREnet, 2016). Incidence was higher in boys compared to girls similar to our study. In other studies from Brazil, Nigeria, Pakistan, Medulloblastomas were the second most common.[18,20,24]
More than two-third of cases were desmoplastic in our study as against only one-fourth reported by another similar study from South India.[11] We had no reported cases of Medulloblastoma Extensive Nodularity and large cell variant type of medulloblastoma.
Astrocytic tumors were the second most common in our study (28.8%) similar to studies from Nepal and Yemen.[17,22] Interestingly, nearly 17.3% of our CNS tumors were low-grade gliomas whereas pilocytic astrocytoma was the most commonly reported tumor (22.33%) from Europe.[25,26] Glioblastoma multiforme constituted to only about 3.8% of all tumors as against 17.2% reported in Korea.[27]
Ependymomas constituted only about 9.6% of all tumors in our study similar to those noted in other studies from the UK, Italy, Iran, and Pakistan.[10,14,21,24] 9.5% of the tumors were germ cell tumors similar to studies from China.[16] There were no nerve sheath tumors in our study while some studies have reported an incidence of 4.1%.[28]
Our study had a mean age of 4 years. Studies from China, Japan, and France have reported highest incidence in 1–4 years, 5–9 years, and 5–9 years, respectively.[25,29,30] Another study from India with a much larger sample size of 1043 patients reported the mean age to be around 10.9 years.[11] Such gross differences from nearly the same geographic area can be the result of small sample size in our study.
CNS tumors are more common in boys than girls as per reports worldwide.[25,27,31] Although the boys in our study were affected more frequently than girls (2.5:1), the ratio was significantly higher than most studies from the west. This might be a reflection of the prevalent gender bias in this part of the world in seeking treatment. Only ependymomas were slightly more common in girls (1:1.5) in our study while oligodendrogliomas (0.3:1), hemangioblastomas (0.3:1), pituitary adenoma (0.6:1) were tumors with girls as the majority in studies from Korea and France.[27,29] We had no cases of primary spinal cord tumors in our study as compared to 7.7% in a study from China.[16]
Treatment outcomes of CNS tumors from middle- and low-income countries are substantially lower than high-income countries as a consequence of late diagnosis and lack of integration of multidisciplinary teams.[32] Limited data on outcome of pediatric CNS tumors is available. As per the CBTRUS 2016 fact sheet, in the US, 73.8% was the 5-year relative survival rates following the diagnosis of primary malignant brain and other CNS tumors in the age group of 73.8%.[5] Even low-grade tumors can have a significant morbidity adversely affecting the quality of life. Several studies from the West have reported a ten-year overall survival rates of 90% or greater with complete resection for low-grade gliomas.[33] German studies on standard risk medulloblastoma with conventional chemotherapy and intrathecal and systemic methotrexate avoiding radiation have shown 5-year progression-free survival and overall survival rates of 82% + 9% and 93% + 6%, respectively for patients with complete resection of localized disease and 33% + 14% and 38% + 15% for disseminated disease.[34] Significant disparity between outcomes of high- and low-income countries are noted. An Indian study has reported a median overall survival of 36 months (58.1%) in age <14 years for medulloblastomas.[35]
This study has some obvious limitations. Most importantly, it is the relatively small sample size and lack of data from patients who visited only the neurosurgery department without a referral to the pediatric oncology department. Short period of analysis (<10 years) and lack of multi-institutional analysis in the geographic area are among the others.
CONCLUSIONS
We present a single-center experience of treating pediatric CNS tumors. Variations in pattern and frequency of occurrence among various subtypes were noted in our study. The question of whether the present study truly depicts the regional prevalence or just a reporting bias can only be resolved by creation of a central database from all parts of India like a National Brain Tumour Registry. However, our study does contribute to the growing literature regarding epidemiological aspects and treatment outcomes of pediatric CNS tumors in India. Abandonment rates in low- and middle-Income countries continue to be high and require addressing in the form of improved standards of care, financial, and social support. Enrolling patients in clinical trials may be of particular benefit as they have shown to improve on the best-accepted therapy available. Survivor clinics for brain tumors are essential as many adverse effects on the brain are better appreciated years after treatment completion.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Albright AL, Sposto R, Holmes E, Zeltzer PM, Finlay JL, Wisoff JH, et al. Correlation of neurosurgical subspecialization with outcomes in children with malignant brain tumors. Neurosurgery. 2000;47:879–85. doi: 10.1097/00006123-200010000-00018. [DOI] [PubMed] [Google Scholar]
- 2.Ostrom QT, de Blank PM, Kruchko C, Petersen CM, Liao P, Finlay JL, et al. Alex's lemonade stand foundation infant and childhood primary brain and central nervous system tumors diagnosed in the united states in 2007-2011. Neuro Oncol. 2015;16(Suppl 10):x1–36. doi: 10.1093/neuonc/nou327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parkin DM, Pisani P, Ferlay J. Global cancer statistics. CA Cancer J Clin. 1999;49:33–64, 1. doi: 10.3322/canjclin.49.1.33. [DOI] [PubMed] [Google Scholar]
- 4.Smith MA, Freidlin B, Ries LA, Simon R. Trends in reported incidence of primary malignant brain tumors in children in the United States. J Natl Cancer Inst. 1998;90:1269–77. doi: 10.1093/jnci/90.17.1269. [DOI] [PubMed] [Google Scholar]
- 5.Ostrom QT, Gittleman H, Xu J, Kromer C, Wolinsky Y, Kruchko C, et al. CBTRUS statistical report: Primary brain and other central nervous system tumors diagnosed in the united states in 2009-2013. Neuro Oncol. 2016;18:v1–75. doi: 10.1093/neuonc/now207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arora RS, Eden TO, Kapoor G. Epidemiology of childhood cancer in India. Indian J Cancer. 2009;46:264–73. doi: 10.4103/0019-509X.55546. [DOI] [PubMed] [Google Scholar]
- 7.Kusumakumary P, Jacob R, Jothirmayi R, Nair MK. Profile of pediatric malignancies: A ten year study. Indian Pediatr. 2000;37:1234–8. [PubMed] [Google Scholar]
- 8.Nandakumar A, Anantha N, Appaji L, Swamy K, Mukherjee G, Venugopal T, et al. Descriptive epidemiology of childhood cancers in Bangalore, India. Cancer Causes Control. 1996;7:405–10. doi: 10.1007/BF00052665. [DOI] [PubMed] [Google Scholar]
- 9.Swaminathan R, Rama R, Shanta V. Childhood cancers in Chennai, India, 1990-2001: Incidence and survival. Int J Cancer. 2008;122:2607–11. doi: 10.1002/ijc.23428. [DOI] [PubMed] [Google Scholar]
- 10.Feltbower RG, Picton S, Bridges LR, Crooks DA, Glaser AW, McKinney PA, et al. Epidemiology of central nervous system tumors in children and young adults (0-29 years), Yorkshire, United Kingdom. Pediatr Hematol Oncol. 2004;21:647–60. doi: 10.1080/08880010490501079. [DOI] [PubMed] [Google Scholar]
- 11.Asirvatham JR, Deepti AN, Chyne R, Prasad MS, Chacko AG, Rajshekhar V, et al. Pediatric tumors of the central nervous system: A retrospective study of 1,043 cases from a tertiary care center in South India. Childs Nerv Syst. 2011;27:1257–63. doi: 10.1007/s00381-011-1407-z. [DOI] [PubMed] [Google Scholar]
- 12.Ostrom QT, Gittleman H, Farah P, Ondracek A, Chen Y, Wolinsky Y, et al. CBTRUS statistical report: Primary brain and central nervous system tumors diagnosed in the united states in 2006-2010. Neuro Oncol. 2013;15(Suppl 2):ii1–56. doi: 10.1093/neuonc/not151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shah SH, Soomro IN, Hussainy AS, Hassan SH. Clinico-morphological pattern of intracranial tumors in children. J Pak Med Assoc. 1999;49:63–5. [PubMed] [Google Scholar]
- 14.Farinotti M, Ferrarini M, Solari A, Filippini G. Incidence and survival of childhood CNS tumours in the region of Lombardy, Italy. Brain. 1998;121(Pt 8):1429–36. doi: 10.1093/brain/121.8.1429. [DOI] [PubMed] [Google Scholar]
- 15.Ahmed N, Bhurgri Y, Sadiq S, Shakoor KA. Pediatric brain tumours at a tertiary care hospital in Karachi. Asian Pac J Cancer Prev. 2007;8:399–404. [PubMed] [Google Scholar]
- 16.Zhou D, Zhang Y, Liu H, Luo S, Luo L, Dai K, et al. Epidemiology of nervous system tumors in children: A survey of 1,485 cases in Beijing Tiantan hospital from 2001 to 2005. Pediatr Neurosurg. 2008;44:97–103. doi: 10.1159/000113110. [DOI] [PubMed] [Google Scholar]
- 17.Azad TD, Shrestha RK, Vaca S, Niyaf A, Pradhananga A, Sedain G, et al. Pediatric central nervous system tumors in Nepal: Retrospective analysis and literature review of low- and middle-income countries. World Neurosurg. 2015;84:1832–7. doi: 10.1016/j.wneu.2015.07.074. [DOI] [PubMed] [Google Scholar]
- 18.Pinho RS, Andreoni S, Silva NS, Cappellano AM, Masruha MR, Cavalheiro S, et al. Pediatric central nervous system tumors: A single-center experience from 1989 to 2009. J Pediatr Hematol Oncol. 2011;33:605–9. doi: 10.1097/MPH.0b013e31822031d9. [DOI] [PubMed] [Google Scholar]
- 19.El-Gaidi MA. Descriptive epidemiology of pediatric intracranial neoplasms in Egypt. Pediatr Neurosurg. 2011;47:385–95. doi: 10.1159/000337872. [DOI] [PubMed] [Google Scholar]
- 20.Uche EO, Shokunbi MT, Malomo AO, Akang EE, Lagunju I, Amanor-Boadu SD, et al. Pediatric brain tumors in Nigeria: Clinical profile, management strategies, and outcome. Childs Nerv Syst. 2013;29:1131–5. doi: 10.1007/s00381-013-2105-9. [DOI] [PubMed] [Google Scholar]
- 21.Beygi S, Saadat S, Jazayeri SB, Rahimi-Movaghar V. Epidemiology of pediatric primary malignant central nervous system tumors in Iran: A 10 year report of national cancer registry. Cancer Epidemiol. 2013;37:396–401. doi: 10.1016/j.canep.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 22.Ba-Saddik IA. Childhood cancer in Aden, Yemen. Cancer Epidemiol. 2013;37:803–6. doi: 10.1016/j.canep.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 23.Hatef J, Adamson C, Obiga O, Taremwa B, Ssenyojo H, Muhumuza M, et al. Central nervous system tumor distribution at a tertiary referral center in Uganda. World Neurosurg. 2014;82:258–65. doi: 10.1016/j.wneu.2014.06.040. [DOI] [PubMed] [Google Scholar]
- 24.Bilqees F, Samina K, Mohammad T, Khaleeq-uz-Zamaan Morphological pattern and frequency of central nervous system tumours in children. J Ayub Med Coll Abbottabad. 2016;28:44–6. [PubMed] [Google Scholar]
- 25.Peris-Bonet R, Martínez-García C, Lacour B, Petrovich S, Giner-Ripoll B, Navajas A, et al. Childhood central nervous system tumours – incidence and survival in Europe (1978-1997): Report from automated childhood cancer information system project. Eur J Cancer. 2006;42:2064–80. doi: 10.1016/j.ejca.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 26.Rosemberg S, Fujiwara D. Epidemiology of pediatric tumors of the nervous system according to the WHO 2000 classification: A report of 1,195 cases from a single institution. Childs Nerv Syst. 2005;21:940–4. doi: 10.1007/s00381-005-1181-x. [DOI] [PubMed] [Google Scholar]
- 27.Cho KT, Wang KC, Kim SK, Shin SH, Chi JG, Cho BK, et al. Pediatric brain tumors: Statistics of SNUH, Korea (1959-2000) Childs Nerv Syst. 2002;18:30–7. doi: 10.1007/s00381-001-0547-y. [DOI] [PubMed] [Google Scholar]
- 28.Wong TT, Ho DM, Chang KP, Yen SH, Guo WY, Chang FC, et al. Primary pediatric brain tumors: Statistics of Taipei VGH, Taiwan (1975-2004) Cancer. 2005;104:2156–67. doi: 10.1002/cncr.21430. [DOI] [PubMed] [Google Scholar]
- 29.Bauchet L, Rigau V, Mathieu-Daudé H, Fabbro-Peray P, Palenzuela G, Figarella-Branger D, et al. Clinical epidemiology for childhood primary central nervous system tumors. J Neurooncol. 2009;92:87–98. doi: 10.1007/s11060-008-9740-0. [DOI] [PubMed] [Google Scholar]
- 30.Makino K, Nakamura H, Yano S, Kuratsu J Kumamoto Brain Tumor Group. Population-based epidemiological study of primary intracranial tumors in childhood. Childs Nerv Syst. 2010;26:1029–34. doi: 10.1007/s00381-010-1126-x. [DOI] [PubMed] [Google Scholar]
- 31.Mehrazin M, Rahmat H, Yavari P. Epidemiology of primary intracranial tumors in Iran, 1978-2003. Asian Pac J Cancer Prev. 2006;7:283–8. [PubMed] [Google Scholar]
- 32.Wagner HP, Antic V. The problem of pediatric malignancies in the developing world. Ann N Y Acad Sci. 1997;824:193–204. doi: 10.1111/j.1749-6632.1997.tb46222.x. [DOI] [PubMed] [Google Scholar]
- 33.Gajjar A, Sanford RA, Heideman R, Jenkins JJ, Walter A, Li Y, et al. Low-grade astrocytoma: A decade of experience at St. Jude children's research hospital. J Clin Oncol. 1997;15:2792–9. doi: 10.1200/JCO.1997.15.8.2792. [DOI] [PubMed] [Google Scholar]
- 34.Rutkowski S, Bode U, Deinlein F, Ottensmeier H, Warmuth-Metz M, Soerensen N, et al. Treatment of early childhood medulloblastoma by postoperative chemotherapy alone. N Engl J Med. 2005;352:978–86. doi: 10.1056/NEJMoa042176. [DOI] [PubMed] [Google Scholar]
- 35.Kumar LP, Deepa SF, Moinca I, Suresh P, Naidu KV. Medulloblastoma: A common pediatric tumor: Prognostic factors and predictors of outcome. Asian J Neurosurg. 2015;10:50. doi: 10.4103/1793-5482.151516. [DOI] [PMC free article] [PubMed] [Google Scholar]


