Abstract
Rapunzel syndrome complicated with gastric perforation is a very rare presentation of trichobezoar. Trichobezoar is an uncommon condition affecting predominantly females. It has non-specific clinical presentation, a wide range of complications, and, if not treated appropriately, carries significant mortality. Traditional treatment of trichobezoar is surgical, though, attempts have been made to excise endoscopically, dissolve chemically or fragment using extracorporeal shock waves. We report a case of a very large trichobezoar occupying most of the stomach and duodenum complicated with gastric perforation, and summarise the literature regarding trichobezoar aetiology, diagnostic difficulties, and management.
Keywords: Rapunzel syndrome, Gastric perforation, Diagnosis, Management
Case history
A 23-year-old woman, 3 weeks postpartum via spontaneous vaginal delivery, presented with 2-week history of abdominal pain, vomiting, haematemesis and constipation. The only relevant past medical history was of previous oesophagogastroduodenoscopy in 2005 revealing a gastric ulcer which was treated medically. On examination, she appeared cachectic, dehydrated and pale. She was apyrexial, but tachycardic and hypotensive. Abdominal examination revealed evidence of generalised peritonitis and the blood results indicated raised inflammatory markers and renal impairment. Chest X-ray was consistent with a pneumoperitoneum and thus a provisional diagnosis of perforated gastric/duodenal ulcer was made. Subsequently, urgent laparotomy was performed with the findings of generalised peritonitis secondary to a perforated gastric ulcer. Surprisingly, hair tufts were found coming out of the gastric perforation (Fig. 1A). The stomach and duodenum were distended and fully occupied by trichobezoar. A gastrotomy was made and a large (35 cm × 16 cm) hair ball was removed cast in the shape of the stomach and duodenum (Fig. 1B). The gastric perforation was oversewn and reinforced with an omental patch. Postoperatively, she was reviewed by the psychiatrists to whom she denied hair ingestion. Thereafter, her progress was routine and she discharged herself against medical advice 2 weeks following surgery.
Figure 1.
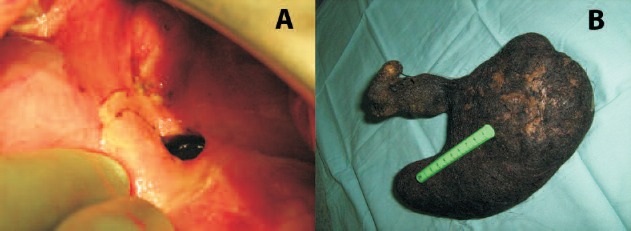
(A) Visible hair tufts are clearly seen coming out of the gastric perforation. (B) A large trichobezoar (35 cm × 16 cm) casts the shape of the stomach and duodenum.
Discussion
Bezoars are foreign bodies found in the gastrointestinal tract and formed from the conglomeration of indigestible material. The origin of the word bezoar is Arabic ‘badzehr’ or Persian ‘panzehr’, both meaning antidote. Bezoars are classified according to their content into phytobezoars (vegetable fibres), trichobezoars (hair), or lactobezoars (milk). Overall, phytobezoars are the most common, followed by the trichobezoars.
Rapunzel syndrome, first described in 1968 and named after the maiden from the eponymous Grimm Brothers’ fairy tale, is a mass of hair extending from the stomach into the bowel through the pylorus. Naik et al.1 reported a series of 24 cases of this condition and showed that various criteria have been used to diagnose the syndrome; however, the essential features are a trichobezoar, and a tail extending to the bowel or symptoms suggestive of bowel obstruction.
The prevalence of trichotillomania (hair pulling) is 0.6–1.6% and is much more common in females than males with a bimodal age of onset – early childhood and adolescence. The latter is more chronic and difficult to treat. Of those affected by trichotillomania, 30% will suffer from trichophagia (hair eating), and only 1% of those will require surgical intervention to deal with the developed trichobezoars. In an early review dating back to 1939, 80% of trichobezoars were found in patients younger than 30 years of age. Most trichobezoars are found in the stomach. Only 5% of gastric trichobezoars are multiple and 15% of trichobezoars are intestinal.2
The clinical presentation can be variable. Patients may present with abdominal pain (37%), nausea and vomiting (33%), abdominal distension, diarrhoea or constipation, anorexia, weight loss (7%), or abdominal mass. A history of trichophagia is obtained in 50%.3 Complications of trichobezoars include gastrointestinal obstruction (26%), bleeding (10%), perforation, malabsorption, and nutritional deficiencies. Rapunzel syndrome associated with gastric perforation is a very rare entity and only three cases have been reported in the literature. If bezoars are left without treatment, the mortality rate can reach 30% because of the associated complications.4
In terms of investigations, plain abdominal X-ray may show a mottled heterogeneous mass with the shape of the stomach along with signs of intestinal obstruction. Barium studies may show a freely mobile intraluminal mass. Ultrasound scans may show an echogenic arc-like surface with sharp posterior acoustic shadowing and can pick up 88% of trichobezoar in experienced hands, whereas CT scan may reveal an intraluminal mass of concentric rings and can diagnose 97% of bezoars.
Medical treatment of trichotillomania includes tricyclic antidepressant, selective serotonin re-uptake inhibitors, behaviour therapy (e.g. habit-reversal training), psychotherapy and hypnosis. Endoscopic removal is an option for small trichobezoars. Enzymatic dissolution, Nd-YaG laser and extracorporeal shock wave fragmentation are novel approaches to be further evaluated.5 Fragmentation carries the risk of small bowel obstruction.3 The standard treatment remains laparotomy, though laparoscopic attempts have been successful for bezoars smaller than 20 cm.
Conclusions
The presented case demonstrates gastric perforation which is an extremely rare complication of Rapunzel syndrome. In such an event, treatment should follow the general lines of managing a perforated viscus. At which point the trichobezoar can be removed via a gastrotomy. Nevertheless, psychiatric counselling and follow-up are important adjuncts to treatment.
References
- 1.Naik S, Gupta V, Naik S, Rangole A, Chaudhary AK, Jain P et al. Rapunzel syndrome reviewed and redefined. Dig Surg 2007; : 157–61. [DOI] [PubMed] [Google Scholar]
- 2.Malhotra A, Jones L, Drugas G. Simultaneous gastric and small intestinal trichobezoars. Pediatr Emerg Care 2008; : 774–6. [DOI] [PubMed] [Google Scholar]
- 3.Lynch KA, Feola PG, Guenther E. Gastric trichobezoar: an important cause of abdominal pain presenting to the pediatric emergency department. Pediatr Emerg Care 2003; : 343–7. [DOI] [PubMed] [Google Scholar]
- 4.Williams RS. The fascinating history of bezoars. Med J Aust 1986; : 613–4. [PubMed] [Google Scholar]
- 5.Coulter R, Antony MT, Bhuta P, Memon MA. Large gastric trichobezoar in a normal healthy woman: case report and review of pertinent literature. South Med J 2005; : 1042–4. [DOI] [PubMed] [Google Scholar]


