Abstract
The fornix, which connects the medial temporal lobe and the medial diencephalon, is involved in episodic memory as an important part of the Papez circuit. The mechanisms of recovery of an injured fornix revealed by diffusion tensor tractography in the five studies are summarized as follows: 1) recovery through the nerve tract from an injured fornical crus to the medial temporal lobe via the normal pathway of the fornical crus; 2) recovery through the nerve tract originating from an ipsi-lesional fornical body connected to the ipsi-lesional medial temporal lobe via the splenium of the corpus callosum; 3) recovery through the nerve tract from the ipsi-lesional fornical body extending to the contra-lesional medial temporal lobe via the splenium of the corpus callosum; 4) recovery through the nerve tract originating from the ipsi-lesional fornical column connected to the ipsi-lesional medial temporal lobe; and 5) recovery through the nerve tract originating from the contra-lesional fornical column connected to the ipsi-lesional medial temporal lobe via the contra-lesional medial temporal lobe and the splenium of the corpus callosum. These diffusion tensor tractography studies on mechanisms of recovery of injured fornical crus appeared to provide useful information for clinicians caring for patients with brain injury, however, studies on this topic are still in the beginning stages.
Keywords: nerve regeneration, fornix, diffusion tensor tractography, recovery mechanism, memory assessment scale, Papez, neural regeneration
Introduction
The fornix, which connects the medial temporal lobe and the medial diencephalon, is involved in episodic memory as an important part of the Papez circuit (Wolk and Budson, 2010; Thomas et al., 2011). Research on the mechanisms of recovery of an injured fornix is limited compared with other brain neural structures, including the corticospinal tract (Jang, 2011; Yeo and Jang, 2013; Lee and Jang, 2014; Rong et al., 2014; Jang et al., 2016; Jang and Lee, 2016; Jang and Seo, 2016). That is because accurate assessment of the fornix is difficult due to its anatomical characteristics: long and thin shape, deep location within the brain, and less discrimination from adjacent neural structures (Thomas et al., 2011). However, recently introduced diffusion tensor tractography (DTT), derived from diffusion tensor imaging (DTI), has enabled three-dimensional reconstruction and estimation of the fornix (Concha et al., 2005). Several studies using DTT have demonstrated recovery mechanisms of the injured fornix in patients with brain injury (Yeo and Jang, 2013; Lee and Jang, 2014; Jang et al., 2016; Jang and Lee, 2016; Jang and Seo, 2016).
Clarification of mechanisms of recovery following brain injury is clinically important because such information provides a scientific basis for neurorehabilitation and prediction of prognosis. The mechanisms of recovery of an injured brain are based on the following concepts: 1) Reserve axons and synapse to be revealed for particular functions following injury of the ordinarily dominant system and 2) collateral sprouting from an intact neuron to a denervated region) (Bach y Rita, 1981a, b; Jang and Kwon, 2014a). Therefore, the mechanisms for recovery of an injured fornix might be based in part on the involvement of the neural connectivity of the fornix and recent studies have suggested that the neural connectivity of the fornix is much wider and more complex than the classical concept of the fornix anatomy: in detail, the anterior fornical body has high connectivity with the anterior commissure, corpus callosum, medial temporal lobe, and brain areas relevant to cholinergic nuclei (the basal forebrain region and brainstem), while the posterior fornical body has connectivity with the cerebral cortex, corpus callosum, and brainstem (Jang and Kwon, 2013, 2014a, b).
In this article, DTT studies on the mechanisms of recovery of an injured fornix in patients with brain injury were reviewed. Relevant studies were identified using the following electronic databases (PubMed and MEDLINE) from 1966 to 2016. The following key words were used: DTI, DTT, fornix, fornical crus, memory, traumatic brain injury, brain tumor, and brain injury. This review was limited to studies of humans with brain injury. Finally, five studies were selected and reviewed (Yeo and Jang, 2013; Lee and Jang, 2014; Jang et al., 2016; Jang and Lee, 2016; Jang and Seo, 2016).
Recovery Mechanisms of Injured Fornical Crus Revealed by DTT
The mechanisms of recovery of an injured fornical crus reported in the five studies are summarized as follows: 1) mechanism 1: recovery through the nerve tract from an injured fornical crus to the medial temporal lobe via the normal pathway of the fornical crus; 2) mechanism 2: recovery through the nerve tract originating from an ipsi-lesional fornical body connected to the ipsi-lesional medial temporal lobe via the splenium of the corpus callosum; 3) mechanism 3: recovery through the nerve tract from the ipsi-lesional fornical body extending to the contra-lesional medial temporal lobe via the splenium of the corpus callosum; 4) mechanism 4: recovery through the nerve tract originating from the ipsi-lesional fornical column connected to the ipsi-lesional medial temporal lobe; and 5) mechanism 5: recovery through the nerve tract originating from the contra-lesional fornical column connected to the ipsi-lesional medial temporal lobe via the contra-lesional medial temporal lobe and the splenium of the corpus callosum (Yeo and Jang, 2013; Lee and Jang, 2014; Jang et al., 2016; Jang and Lee, 2016; Jang and Seo, 2016) (Figure 1 and Table 1).
Figure 1.
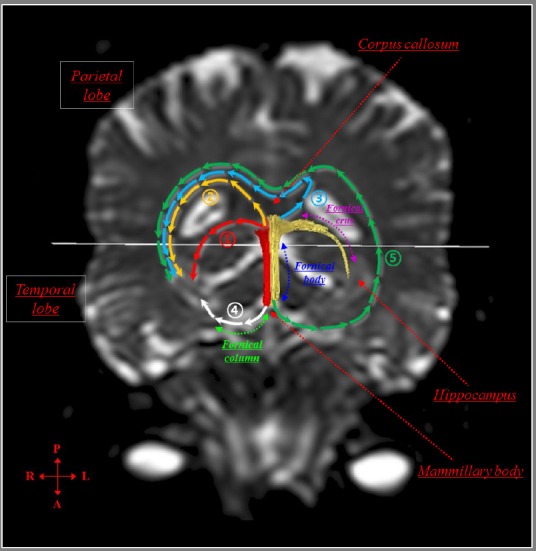
Mechanisms of recovery of injured fornical crus determined by diffusion tensor tractography.
①Mechanism 1: Recovery through the neural tract from an injured fornical crus to the medial temporal lobe via the normal pathway of the fornical crus. ② Mechanism 2: Recovery through the neural tract originating from an ipsi-lesional fornical body connected to the ipsi-lesional medial temporal lobe via the splenium of the corpus callosum. ③Mechanism 3: Recovery through the neural tract from the ipsi-lesional fornical body extending to the contra-lesional medial temporal lobe via the splenium of the corpus callosum. ④ Mechanism 4: Recovery through the neural tract originating from the ipsi-lesional fornical column connected to the ipsi-lesional medial temporal lobe. ⑤Mechanism 5: Recovery through the nerve tract originating from the contra-lesional fornical column connected to the ipsi-lesional medial temporal lobe via the contra-lesional medial temporal lobe and the splenium of the corpus callosum.
Table 1.
Previous diffusion tensor imaging studies on mechanisms of recovery of injured forni
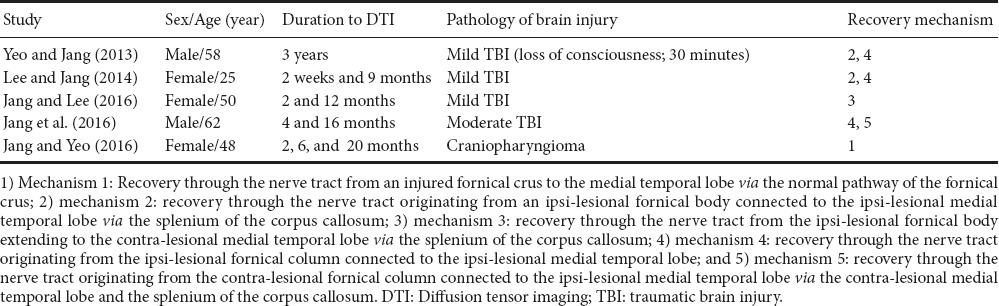
In 2003, Yeo and Jang estimated the fornix in a patient who complained of memory impairment for 3 years after direct head trauma due to an in-car accident (loss of consciousness: 30 minutes). The patient showed memory impairment on the Memory Assessment Scale (MAS, global memory: 70 [2%ile]), although total intelligence on the Wechsler Intelligence Scale (WAIS) was within the normal range (total IQ: 109) (Wechsler, 1981; Williams, 1991). On 3-year DTT, discontinuation of both fornical crus in the proximal portion was observed and a nerve tract originating from the right fornical body extended to the right temporal lobe through the splenium of the corpus callosum (mechanism 2). Another nerve tract originating from the left fornical column passed the left medial temporal lobe (mechanism 4). As a result, the authors concluded that these nerve tracts of the fornix observed in this patient were the result of nerve reorganization following bilateral injury of the fornix crus (Yeo and Jang, 2013).
Subsequently, in 2014, Lee and Jang followed up the changes of an injured fornix for 8.5 months from 2 weeks to 9 months after onset in a patient with mild traumatic brain injury (TBI) due to a pedestrian car accident. On 9-month DTT, two nerve tracts originating from each fornical column extended to each medial temporal lobe, respectively (mechanism 4) and a neural tract originating from the right fornical body and crus extended to the right medial temporal lobe (mechanism 2). The patient showed a total score of 86 for mild memory impairment on the Memo Assessment Scale at 2 weeks after onset, however, her memory had recovered to be within normal range, with a score of 105 at 9 months after onset (Williams, 1991). Therefore, the authors concluded that three neural tracts from both fornical columns and the right forncal body and crus were the apparent mechanisms of recovery of the injured fornix (Lee and Jang, 2014).
In 2016, Jang and Lee reported on the recovery process for an injured fornical crus following mild TBI due to an in-car traffic accident. The patient complained of memory impairment since the onset of head trauma and showed mild memory impairment with global memory (77[6%ile]) on the MAS at 2 months after onset (Williams, 1991). The patient underwent rehabilitation, including cognitive therapy and cholinergic drugs until 12 months after onset. She showed significant improvement of memory impairment with global memory: 90(25%ile) on the MAS at 12 months after onset. A discontinuation of the left fornical crus was observed on 2-month DTT. However, on 12-month DTT, the left discontinued fornical crus was shortened, instead, a nerve tract from the right fornical body extending to the left medial temporal lobe via the splenium of the corpus callosum and the left fornical column was elongated to the left medial temporal lobe (mechanism 3). The authors assumed that the recovery of memory impairment in this patient was attributed to the above nerve tract (mechanism 3) (Jang and Lee, 2016).
Recently, Jang et al. (2016) reported on a patient with moderate TBI resulting from a car accident, which occurred while riding a bicycle, who showed nerve tracts from the bilateral fornical columns to each medial temporal lobe following bilateral injury of the fornical crura. He showed memory impairment at 4 months after onset as the global memory: 79 (8%ile) on the MAS and his memory impairment was improved to normal range, as the global memory: 99 (47%ile) on the MAS at 16 months after onset (Williams, 1991). Discontinuations of the proximal portion of bilateral fornical crura were observed on both 4-month and 16-month DTTs. On 16-month DTT, both fornical columns were connected to each medial temporal lobe through the new nerve tracts (mechanism 4) and a new nerve tract originating from the left fornical column was connected to the right medial temporal lobe via the left medial temporal lobe and the splenium of the corpus callosum (mechanism 5).
During the same year, Jang and Yeo investigated the recovery process of injured fornical crura following a neurosurgical operation for a brain tumor (Jang and Seo, 2016). The patient showed severe memory impairment after craniotomy and navigator assisted removal of craniopharyngioma at the suprasellar space. Discontinuation of both fornical crura was observed on 2-month DTT. However, on 6-month DTT, fornical crura emerged from the end of the fornical body on both sides and were elongated to the medial temporal lobe on both sides on 20-month DTT. The authors suggested that the injured fornical crus recovered via the normal pathway of the fornical crus in this patient (mechanism 1) (Jang and Seo, 2016).
To conclude, in this article, five DTT studies (four studies: traumatic brain injury, and one study: brain tumor) on mechanisms of recovery of injured fornical crus in patients with brain injury were reviewed. The frequency of mechanisms of recovery of an injured fornix was in the following order: mechanism 4 three times, mechanism 2 twice, mechanism 1 three times, and mechanism 5 once. These DTT studies on mechanisms of recovery of injured fornical crus appeared to provide useful information for clinicians caring for patients with brain injury, however studies on this topic are still in the beginning stages. Therefore, we could not describe the factors which could affect the acting recovery mechanism among five mechanisms after injury of fornical crus. These factors might include brain pathology, severity and location of injury of fornical crus, and patient's gender or age.
In-depth DTT studies on this topic, particularly those involving large numbers of subjects and other brain pathologies, should be encouraged. In addition, the limitation of DTT should be considered: regions of fiber complexity and crossing fibers hinder full reflection of the underlying fiber architecture, resulting in possible underestimation of the nerve tracts (Parker and Alexander, 2005; Wedeen et al., 2008; Yamada et al., 2009).
Footnotes
Conflicts of interest: None declared.
Data sharing statement: Datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
Copyedited by Li CH, Song LP, Zhao M
Funding: This work was supported by the National Research Foundation (NRF) of Korea Grant funded by the Korean Government (MSIP) (2015R1A2A2A01004073).
References
- Bach y Rita P. Central nervous system lesions: sprouting and unmasking in rehabilitation. Arch Phys Med Rehabil. 1981a;62:413–417. [PubMed] [Google Scholar]
- Bach y Rita P. Brain plasticity as a basis of the development of rehabilitation procedures for hemiplegia. Scand J Rehabil Med. 1981b;13:73–83. [PubMed] [Google Scholar]
- Concha L, Gross DW, Beaulieu C. Diffusion tensor tractography of the limbic system. AJNR Am J Neuroradiol. 2005;26:2267–2274. [PMC free article] [PubMed] [Google Scholar]
- Jang SH. A review of diffusion tensor imaging studies on motor recovery mechanisms in stroke patients. Neuro Rehabilitation. 2011;28:345–352. doi: 10.3233/NRE-2011-0662. [DOI] [PubMed] [Google Scholar]
- Jang SH, Kwon HG. Neural connectivity of the posterior body of the fornix in the human brain: diffusion tensor imaging study. Neurosci Lett. 2013;549:116–119. doi: 10.1016/j.neulet.2013.06.017. [DOI] [PubMed] [Google Scholar]
- Jang SH, Kwon HG. Perspectives on the neural connectivity of the fornix in the human brain. Neural Regen Res. 2014a;9:1434–1436. doi: 10.4103/1673-5374.139459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang SH, Kwon HG. Neural connectivity of the anterior body of the fornix in the human brain: diffusion tensor imaging study. Neurosci Lett. 2014b;559:72–75. doi: 10.1016/j.neulet.2013.11.040. [DOI] [PubMed] [Google Scholar]
- Jang SH, Lee HD. Compensatory neural tract from contralesional fornical body to ipsilesional medial temporal lobe in a patient with mild traumatic brain injury: A case report. Am J Phys Med Rehabil. 2016;95:e14–17. doi: 10.1097/PHM.0000000000000390. [DOI] [PubMed] [Google Scholar]
- Jang SH, Seo YS. Recovery of injured fornical crura following neurosurgical operation of a brain tumor: a case report. Neural Regen Res. 2016;11:854–855. doi: 10.4103/1673-5374.182714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang SH, Kim SH, Lee HD. New neural tracts from bilateral fornical columns to compensate bilateral injury of fornical crura. Am J Phys Med Rehabil. 2016;95:e75–76. doi: 10.1097/PHM.0000000000000451. [DOI] [PubMed] [Google Scholar]
- Lee HD, Jang SH. Changes of an injured fornix in a patient with mild traumatic brain injury: diffusion tensor tractography follow-up study. Brain Inj. 2014;28:1485–1488. doi: 10.3109/02699052.2014.930178. [DOI] [PubMed] [Google Scholar]
- Parker GJ, Alexander DC. Probabilistic anatomical connectivity derived from the microscopic persistent angular structure of cerebral tissue. Philos Trans R Soc Lond B Biol Sci. 2005;360:893–902. doi: 10.1098/rstb.2005.1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rong D, Zhang M, Ma Q, Lu J, Li K. Corticospinal tract change during motor recovery in patients with medulla infarct: a diffusion tensor imaging study. Biomed Res Int. 2014;2014:524096. doi: 10.1155/2014/524096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas AG, Koumellis P, Dineen RA. The fornix in health and disease: an imaging review. Radiographics. 2011;31:1107–1121. doi: 10.1148/rg.314105729. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Manual for the wechsler adult intelligence scale-revised. New York: Psychological Corporation; 1981. [Google Scholar]
- Wedeen VJ, Wang RP, Schmahmann JD, Benner T, Tseng WY, Dai G, Pandya DN, Hagmann P, D’Arceuil H, de Crespigny AJ. Diffusion spectrum magnetic resonance imaging (DSI) tractography of crossing fibers. Neuroimage. 2008;41:1267–1277. doi: 10.1016/j.neuroimage.2008.03.036. [DOI] [PubMed] [Google Scholar]
- Williams JM. MAS: Memory Assessment Scales : professional manual. Odessa, Fla: Psychological Assessment Resources; 1991. [Google Scholar]
- Wolk DA, Budson AE. Memory systems. Continuum (Minneap Minn) 2010;16:15–28. doi: 10.1212/01.CON.0000368257.30791.3a. [DOI] [PubMed] [Google Scholar]
- Yamada K, Sakai K, Akazawa K, Yuen S, Nishimura T. MR tractography: a review of its clinical applications. Magn Reson Med Sci. 2009;8:165–174. doi: 10.2463/mrms.8.165. [DOI] [PubMed] [Google Scholar]
- Yeo SS, Jang SH. Neural reorganization following bilateral injury of the fornix crus in a patient with traumatic brain injury. J Rehabil Med. 2013;45:595–598. doi: 10.2340/16501977-1145. [DOI] [PubMed] [Google Scholar]


