Abstract
We present our experience in diagnosing and treating a case of a massive left paraduodenal fossa hernia, containing over 30% of the small bowel, presenting with a history of recurrent incomplete small bowel obstruction.
Keywords: Paraduodenal fossa, Hernia, Small bowel, Obstruction
Internal intestinal hernias are classified as congenital or acquired and cause as much as 5.8% of all small bowel obstructions.1,2 Paraduodenal fossa hernias (PDFHs) represent 53% of all congenital internal hernias and 0.2–0.9% of all small bowel obstructions.3 The left-sided one is three times as common as the right, and occurs three times more frequently in males.2,4 Patients with a PDFH have a 50% life-time risk of developing small bowel obstruction (SBO),2 with a 20–50% mortality rate for acute presentations.5 Establishing the correct diagnosis in these patients can be difficult as they often present with vague chronic abdominal symptoms. Indeed, most are discovered incidentally at laparotomy, or during autopsy.
We present our experience in diagnosing and treating a case of a massive left paraduodenal fossa hernia, containing over 30% of the small bowel, presenting with a history of recurrent incomplete small bowel obstruction.
Case history
A 20-year-old man presented with 24-h history of colicky abdominal pain localising to upper abdomen, associated with bilious vomiting, and alternating constipation and diarrhoea. He had had a number of similar episodes within the last 6 years, all of which resolved spontaneously within a few hours of onset. The patient’s past medical history was unremarkable. Physical examination revealed tenderness and guarding in upper quadrants and epigastrium with mild abdominal distension but no visible external hernia.
Plain abdominal X-ray series (Fig. 1) demonstrated no free air and presence of gas in both large and small bowel without distension, but with multiple air fluid levels. Computed tomography (CT) of the abdomen and pelvis (Fig. 2) demonstrated features of small bowel obstruction with a transition point near the terminal ileum. In addition, it demonstrated the abnormal positioning of mesenteric vessels and crossing of these in the abdomen suggesting a possible internal hernia.
Figure 1.

Plain abdominal X-ray demonstrating no free air and presence of gas in both large and small bowel without distension, but with multiple air fluid levels.
Figure 2.

CT of abdomen and pelvis demonstrating features of small bowel obstruction with a transition point (circled) near the terminal ileum.
While in the emergency department, the patient’s symptoms spontaneously resolved and he was discharged with an appointment for out-patient barium follow-up.
A barium follow through (Fig. 3) performed electively demonstrated an abnormal position of duodenum and jejunum, with the entire jejunum being on the right side of the abdomen, suggestive of a small bowel malrotation.
Figure 3.
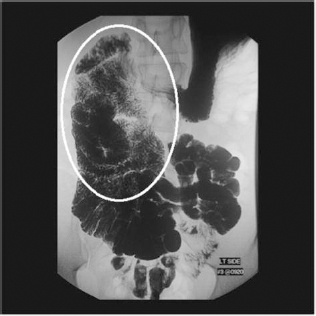
Barium follow through performed electively demonstrated an abnormal position of duodenum and jejunum (circled), with the entire jejunum being on the right side of the abdomen, suggestive of a small bowel malrotation.
The patient was admitted electively for an exploratory laparotomy and hernia repair. At operation, inspection of the small bowel revealed a transition zone at the distal jejunum that was involved in the hernia. We proceeded to reduce what was between 30–40% of the small bowel involved in a left paraduodenal hernia. Once reduced into the infracolic compartment, the bowel was examined and found to be structurally and functionally intact, with normal vascularity. The paraduodenal hernia sac was suture ligated at its neck. The abdomen was closed without difficulty or tension. The patient’s postoperative recovery was uneventful and he was discharged on postoperative day 6.
Discussion
The aetiology of left PDFHs is thought to result from failure of normal counter-clockwise rotation of the mid-gut around the superior mesenteric artery during weeks 5–11 of embryological development. In addition, failure of fusion of the mesocolon with the peritoneum of the body wall leaves a potential space – the fossa of Landzert – behind the mesocolon. This fossa is located lateral to the fourth part of the duodenum, and posterior to inferior mesenteric vein and left colic artery; the hernia results from invagination of small bowel into this unsupported area through an opening bound anteriorly by the inferior mesenteric vein.
Although congenital, most left PDFHs are diagnosed during the 4–6th decade of life with the average age of diagnosis being 38.5 years. They are often difficult to diagnose, as the most common presentation is rather non-specific; indeed, most are discovered incidentally at laparotomy or at autopsy. The presentation ranges in severity from recurrent vague abdominal pain, tenderness, nausea, and vomiting in partial, incomplete obstruction, to acute abdomen in cases of incarceration and strangulation. The pain is typically post-prandial and relieved by turning. Therefore, high index of suspicion should be maintained in a patient with pertinent but unexplained complaints.
Imaging is often not helpful unless it is done at the time of acute obstruction. Plain abdominal X-rays may show ovoid mass of multiple jejunal loops in the left upper quadrant next to the ascending duodenum. Due to the ambiguous clinical presentation, CT may be the initial investigation of choice in many patients. CT may show focal cluster of small bowel abnormally positioned between the stomach and the pancreas.6,7 If the bowel loops are collapsed and oral contrast is not used, the hernia contents may be mistaken for a oft tissue mass which may result in a CT-guided biopsy attempt, potentially causing a disastrous bowel perforation. Small bowel follow may demonstrate small bowel herniating through the defect in the mesocolon, thus demonstrating the extent of the hernia.
Once the correct diagnosis is made, the treatment is surgical. First, the viscera are reduced manually. When difficult to reduce, because of bulky bowel or adhesion, inferiorly based incision in the avascular portion of the hernia sac is made. Care should be taken to avoid injury to inferior mesenteric vessels.8 This restores normal anatomy and is followed by closure of the hernia defect. Although most left PDFHs are repaired via the open laparotomy approach, a laparoscopic approach has also been described. The advantage of performing a diagnostic laparoscopy is the quick establishment of diagnosis, eliminating the need for further investigations, followed by immediate cure of the hernia.9–11
Conclusions
Left paraduodenal fossa hernia is a relatively uncommon cause of small bowel obstruction. It should be included in the differential diagnosis in a patient who is relatively young, experiences recurrent episodes of intermittent small bowel obstruction, and without history of previous abdominal surgery. A combination of high index of suspicion and timely diagnosis combined with surgical intervention effectively cure the patient and prevent future complications.
References
- 1.Blachar A, Federle MP. Internal hernia: an increasingly common cause of small bowel obstruction. Semin Ultrasound CT MR 2002; : 174–83. [DOI] [PubMed] [Google Scholar]
- 2.Newson BD, Kukova JS. Congenital and acquired internal hernias: unusual causes of small bowel obstruction. Am J Surg 1986; : 279–85. [DOI] [PubMed] [Google Scholar]
- 3.Yoo HY, Mergelas J, Seibert DG. Paraduodenal hernia: a treatable cause of upper gastrointestinal tract symptoms. J Clin Gastroenterol 2000; : 226–9. [DOI] [PubMed] [Google Scholar]
- 4.Rastogi A, Laplante S. Right paraduodenal hernia. Can Assoc Radiol J 1997; : 205–7. [PubMed] [Google Scholar]
- 5.Tong RSK, Sengupta S, Tjandra JJ. Left paraduodenal hernia: case report and review of the literature. Aust NZ J Surg 2002; : 69–71. [DOI] [PubMed] [Google Scholar]
- 6.Warshauer DM, Mauro MA. CT diagnosis of paraduodenal hernia. Gastrointest Radiol 1992; : 13–5. [DOI] [PubMed] [Google Scholar]
- 7.Olazabal A, Guasch I, Casas D. CT diagnosis of nonobstructive left paraduodenal hernia. Clin Radiol 1992; : 288–9. [DOI] [PubMed] [Google Scholar]
- 8.Brigham RA, Fallon WF, Saunders JR, Harmon JW, D’Avis JC. Paraduodenal hernia: diagnosis and surgical management. Surgery 1984; : 498–502. [PubMed] [Google Scholar]
- 9.Jeong GA, Cho GS, Kim HC, Shin EJ, Song OP. Laparoscopic repair of paraduodenal hernia: comparison with conventional open repair. Surg Laparosc Endosc Percutan Tech 2008; : 611–5. [DOI] [PubMed] [Google Scholar]
- 10.Moon CH, Chung MH, Lin KM. Diagnostic laparoscopy and laparoscopic repair of a left paraduodenal hernia can shorten hospital stay. J Soc Laparosc Surg 2006; : 90–3. [PMC free article] [PubMed] [Google Scholar]
- 11.Uematsu T, Kitamura H, Iwase M. Laparoscopic repair of a paraduodenal hernia. Surg Endosc 1998; : 50–2. [DOI] [PubMed] [Google Scholar]


