Abstract
Retroperitoneal abscesses are rare complications of pyogenic sacroiliitis. Diagnosis is often delayed due to the initial non-specific symptoms and signs and also a low awareness of the clinical presentation and diagnostic procedures among clinicians. We describe a case of an 18-year-old man who was diagnosed with septic arthritis of his left sacro-iliac joint which was complicated by a retroperitoneal abscess. After discussion with the radiologist and orthopaedic surgeons, the abscess was successfully drained via minimally invasive surgery transperitoneally.
Keywords: Colorectal surgery, Minimally invasive surgery, Bone diseases, Surgical pathology
Retroperitoneal abscesses are uncommon and are usually caused by gastrointestinal, urinary tract and, rarely, musculoskeletal infections.1,2 The conventional treatment described is an open surgical drainage via a retroperitoneal approach with an incision on the flank. We report a case of Staphylococcus aureus infection of the sacro-iliac joint resulting in a retroperitoneal abscess which was successfully drained via a laparoscopic transabdominal approach. This case also highlights the importance of multidisciplinary input in the management of this unusual condition.
Case history
An 18-year-old man presented with a 6-day history of progressive pain in his left loin and buttock region. He was reviewed in the emergency department and was not keen to be admitted. He was, therefore, discharged with a review appointment a week after and was given crutches as he had difficulty in weight-bearing. Subsequently, he presented with fever and rigors and was admitted. He denied any urinary or abdominal symptoms or any history of trauma or intravenous drug use. There was no other significant past medical history or family history.
Examination revealed a tachycardia of 105 bpm and a temperature of 38ºC. There was tenderness over his left sacro-iliac joint and gluteal region with no visible erythema over loin or buttocks. Lumbar spine and hip joints revealed a good range of movement and did not exacerbate his symptoms. His inflammatory markers were elevated with a white cell count of 18·109 cells/l and a C-reactive protein of 300 mg/l. X-rays of his abdomen, pelvis and hip were normal and urine microscopy did not reveal any pyuria or microscopic haematuria. Blood cultures grew S. aureus and he was started on intravenous flucloxacillin based on sensitivities and advice from the microbiologist.
A computed tomography scan of his abdomen and pelvis revealed enhancement in the left sacro-iliac joint and a large retroperitoneal abscess on the left which extended from the sacro-iliac joint into the pelvis between the iliacus muscle and the bony pelvis (Fig. 1). After discussion with the radiologist and orthopaedic surgeons at our hospital, it was decided that surgical drainage was necessary and needed to be performed by the surgical team as the abscess was in close proximity to the left iliac vessels.
Figure 1.
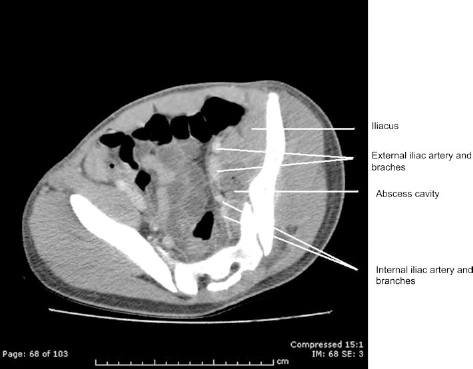
Computed tomography image (axial) confirming the abscess cavity on the left, lateral to the internal and external iliac arteries, deep to psoas muscle.
It was decided to undertake a minimally invasive procedure and a laparoscopy was carried out. There were no intra-abdominal or pelvic findings of note. The left colon was mobilised laterally, the left ureter and gonadals were identified and protected, and the common, external and internal iliac arteries were exposed. With the guidance of the radiologist, who was present in the operating theatre with access to the CT scan images, correlation was achieved between the laparoscopic view and the radiological appearances. A safe path was negotiated between the branches of the internal iliac artery to incise the iliacus muscle and enter the abscess cavity. The cavity was found to be full of thick purulent material, which was aspirated (> 200 ml) and washed out. A suction drain was left in the cavity and a tube drain was left in the pelvis for the first 24 h in case of any spillage into the peritoneal cavity.
Because of persistent drainage of pus from the suction drain for 10 days, our local orthopaedic surgeons suggested that the patient should be transferred to a specialist pelvic surgeon. The patient was then taken back to theatre and the abscess cavity was approached extraperitoneally via an incision over the iliac crest with drainage of less than 10 ml of pus. The patient improved and was discharged with no further problems after a 6-week course of intravenous antibiotics. A follow-up review at 3 months has shown that the patient has recovered with no evidence of residual sepsis.
Discussion
Retroperitoneal abscesses are uncommon and present with insidious symptoms and signs, often leading to a delay in diagnosis with a mean interval between admission and diagnosis of 12 days.1 Risk factors include diabetes mellitus, steroid or intravenous drug abuse, alcoholism and renal failure.1 The common offending organisms are Escherichia coli and Bacteroides spp., as most of the causes of these abscesses are related to the gastrointestinal and urinary tract1,2 and, rarely, from bone infections.3,4
Pyogenic sacroiliitis is rare and only represents 1–2% of all cases of septic arthritis.4 Elderly patients are more susceptible and females tend to have a higher incidence than male patients.5 Most cases are unilateral with a higher incidence on the left side in younger patients.5 S. aureus is the leading bacterial pathogen although some highly resistant Gram-negative strains such as Acinetobacter baumannii and Citrobacter freundii have been reported.2,5 Although scintigraphic bone scan has the highest sensitivity in the diagnosis of pyogenic sacroiliitis,4 computed tomography is the imaging modality of choice once an abscess has formed, as it delineates the exact anatomical location of the pus to plan drainage procedures.
Medical management with parenteral antibiotics in the absence of an abscess is the mainstay of treatment of pyogenic sacroiliitis. However, once an abscess has developed, surgical drainage is indicated and usually performed via a retroperitoneal approach with an incision on the flank.1 If left untreated, joint destruction would ensue leading to long-term joint pain and loss of function.4 In selected cases, radiological drainage has been successful. The open transperitoneal route has been associated with a high failure rate;1 however, as far as we are aware, a laparoscopic transabdominal approach in draining these retroperitoneal abscesses has not been described in the literature.
Conclusions
Early diagnosis and treatment of retroperitoneal abscesses complicating septic arthritis of the sacro-iliac joints is important in preventing mortality and long-term morbidity. Close collaboration between the general surgeons, radiologist, orthopaedic surgeons and micro-biologist was essential in the successful treatment of this case. Minimally invasive surgery should be considered in the treatment of these abscesses.
Acknowledgement
The authors thank Dr Rhodri Davies for providing the labelled CT image for this case report and also for his guidance in theatre.
References
- 1.Crepps JT, Welch JP, Orlando R. Management and outcome of retroperitoneal abscess. Ann Surg 1987; : 276–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siam ARM, Hammoudeh M, Uwaydah AK. Pyogenic sacroiliitis in Qatar. Br J Rheumatol 1993; : 699–701. [DOI] [PubMed] [Google Scholar]
- 3.Ford LS, Ellis AM, Allen HW, Campbell DE. Osteomyelitis and pyogenic sacroiliitis: a difficult diagnosis. J Paediatr Child Health 2004; : 317–9. [DOI] [PubMed] [Google Scholar]
- 4.O’Brien A, Roberts M, Ampat G, Bowley J. Streptococcus pneumoniae infection of the sacro iliac joint – a case report and literature review. J Orthopaedics 2008; : e9. [Google Scholar]
- 5.Wu MS, Chang SS, Lee SH, Lee CC. Pyogenic sacroiliitis –a comparison between paediatric and adult patients. Rheumatology (Oxford) 2007; : 1684–7. [DOI] [PubMed] [Google Scholar]


