Abstract
We describe the second reported case of three consecutive episodes of gallstone ileus and ask the question whether recurrent gallstone ileus justifies definitive surgery to the fistula itself or can be safely managed by repeated enterotomies.
Keywords: Fistula, Gall-stones, Recurrent, Recurrence, Ileus
Case history
An 87-year-old woman presented with a 48-h history of colicky abdominal pain and bilious vomiting. She was dehydrated and had a distended abdomen consistent with small bowel obstruction demonstrable on plain X-ray films. Computed tomography (CT) showed a thickened gallbladder containing two large stones and gas consistent with a cholecystoduodenal fistula. The small bowel was distended up to the site of an intraluminal gall stone (Fig. 1).
Figure 1.
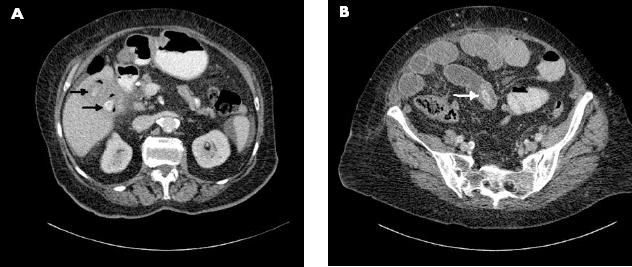
CT scan of the abdomen. (A) The gallbladder fossa is grossly inflamed and contains two gallstones (black arrows) with a large amount of gas and a fistulous tract communicating with the second part of the duodenum. (B) The small bowel is moderately distended with a calibre change in the ileum and an intraluminal gallstone (white arrow) at the point of obstruction.
Laparotomy was performed and, through an enterotomy, a large stone was delivered. There were no other stones or strictures found on palpating the rest of the small bowel. Her recovery was uneventful and she was discharged a week later.
Nine days later, she was re-admitted with small bowel obstruction. There was superficial surgical site infection. CT scan showed a recurrence of gallstone ileus with a single cuboidal stone approximately two-thirds of the way along the small bowel. On this occasion, there was one cuboidal stone seen in the gallbladder. A further mid-line laparotomy was performed and an obstructing gallstone was removed from the distal ileum through an enterotomy. The skin was left open because of the established infection of the previous operative site. She made a slow recovery and was discharged on the 23rd postoperative day.
Thirty-four days after discharge, she had a third episode of small bowel obstruction. CT scan showed a 28-mm gallstone impacted in the mid small bowel with no gallbladder stone.
As she had an open abdominal wound from her previous mid-line laparotomy, an oblique right-sided incision over the site of the gallstone, as located on the CT scan, was made. Segmental small bowel resection and end-to-end anastomosis was performed. She made an uneventful recovery.
On follow-up 12 months later, she had no recurrence of symptoms and her liver function tests were normal.
Discussion
Gall-stone ileus is a mechanical intestinal obstruction caused by impaction of a gallstone within the lumen of the bowel. It is uncommon and the diagnosis is frequently missed or delayed. It is usually associated with a cholecystoduodenal fistula.1 Gall-stone ileus complicates an estimated 0.4–1.5% of all cases of cholelithiasis,1 and accounts for 0.3–5.3% of all cases of small bowel obstruction.2 The maximal diameter of the gallstone is generally larger than 2 cm when causing small bowel obstruction.1–4 The incidence of gallstone ileus is higher in older patients and accounts for up to 25% of all cases of mechanical small bowel obstruction in patients over 65 years of age.3
Patients with gallstone ileus present with intermittent symptoms . This is due to partial, short-lived obstruction at various points as the stone moves along the bowel – the so-called ‘tumbling phenomenon’. Recurrent gallstone ileus must be considered in any patient with a history of gallstone ileus who has a second episode of small bowel obstruction. The recurrence rate of gallstone ileus is quoted as 8.2%. More than 50% of recurrences occur within the first month and the rest within 2 years.1,4 The mortality rate varies from 12–20%.3 Advanced age and presence of multiple co-morbidities in these patients contribute to the significant risk of mortality and high peri-operative morbidity.
CT scanning can demonstrate the classic triad of small bowel obstruction, pneumobilia and ectopic gallstone, analogous to that described by Rigler et al.5 on plain radiographs. CT is more sensitive than plain radiography in diagnosing each of the components of the triad. A pre-operative CT scan is helpful in locating multiple gallstones and identifying the various levels of obstruction. When the diagnosis of gallstone ileus is made at laparotomy, it is important to palpate the rest of small bowel carefully for a second stone, as many of the recurrent cases are caused by an enterolith missed during first operation. An intra-operative ultrasound scan may help in this.1 If a further stone in the small bowel is picked up at surgery, it should be removed.
Controversy remains about the most appropriate approach should a residual gallstone be identified within the gallbladder. Simple enterolithotomy to manage gallstone ileus has been the historical procedure of choice. In the past few decades, some groups have advocated concomitant definitive correction of the cholecystoenteric fistula to prevent complications such as recurrence of gallstone ileus, cholecystitis, cholangitis and malabsorption.6 However, supporters of simple enterolithotomy cite the infrequency of recurrent gallstone ileus, the rarity of complications directly related to persistent cholecystoenteric fistula, the possibility of spontaneous fistula closure when there are no distal gallstones and the high morbidity and mortality rates associated with treatment of the fistula as arguments against more aggressive surgery.1 Reisner and Cohen3 reviewed literature to collect 1001 cases of gallstone ileus. Of these, 11% underwent one-stage procedure with a mortality rate of 16.9%, versus 80% of patients who underwent enterolithotomy alone and had a mortality rate of 11.7%. This difference was not statistically significant.6 However, patients who undergo one-stage repair are usually selected for their lower operative risk, thus skewing the available data.1,6
The management of recurrent gallstone ileus is even more controversial. Vagefi et al.7 suggested recurrence of gallstone ileus as an indication for definitive management of the biliary-enteric fistula. However, patients with gallstone ileus are usually elderly, in poor general condition and have a delayed diagnosis, frequently leading to dehydration, shock, sepsis or peritonitis. The main goal of therapy must be relief of the small bowel obstruction.1,6 This can be done with simple enterolithotomy.
In our case report, this 87-year-old patient made a satisfactory recovery after each of the simple entero-lithotomy procedures she underwent. More extensive one-stage enterolithotomy, cholecystectomy and chole-cystoduodenal fistula repair may be performed in carefully selected patients.
References
- 1.Doogue MP, Choong CK, Frizelle FA. Recurrent gallstone ileus: underestimated. Aust NZ J Surg 1998; : 755–6. [DOI] [PubMed] [Google Scholar]
- 2.Day EA, Marks C. Gallstone ileus: review of the literature and presentation of thirty-four new cases. Am J Surg 1975; : 552–8. [DOI] [PubMed] [Google Scholar]
- 3.Reisner RM, Cohen JR. Gallstone ileus: a review of 1001 reported cases. Am Surg 1994; : 441–6. [PubMed] [Google Scholar]
- 4.Ulreich S, Massi J. Recurrent gallstone ileus. AJR Am J Roentgenol 1979; : 921–3. [DOI] [PubMed] [Google Scholar]
- 5.Rigler LG, Borman CN, Noble JF. Gallstone obstruction: pathogenesis and roentgen manifestations. JAMA 1941; : 1753–9. [Google Scholar]
- 6.Rodriguez-Sanjuán JC, Casado F, Fernández MJ, Morales DJ, Naranjo Cholecystectomy and fistula closure versus enterolithotomy alone in gallstone ileus. Br J Surg 2005; : 634–7. [PubMed] [Google Scholar]
- 7.Vagefi PA, Ferguson CM, Hall JF. Recurrent gallstone ileus: third time is the charm. Arch Surg 2008; : 1118–20. [DOI] [PubMed] [Google Scholar]


