Abstract
A case is described where laparoscopic principles in the management of spontaneous sigmoid diverticular perforation are applied to foreign body perforation.
Keywords: Foreign body perforation, Diverticular disease
Gastrointestinal foreign body is a common reason for acute admission with up to 6000 incidents in the UK in 2008 according to Department of Health statistics. Less than 1% result in perforation. In this case, laparoscopic principles in the management of spontaneous sigmoid diverticular perforation are applied to foreign body perforation.
Case history
The patient was a 65-year-old man who presented with a 1-day history of severe lower abdominal pain and nausea with no preceding gastrointestinal disturbance. Previous medical history included atrial fibrillation, thorocotomy and removal of a right lung cyst. Drug history was sildenafil, simvastatin, perindopril, indapamide, ibersartan and wafarin. On examination, he was febrile, tachypnoeic, tachycardic and dehydrated. Abdominal examination revealed a tender lower abdomen with guarding and minimal distension. The white blood cell count was 15.3 × 109/l and C-reactive protein 196.5 mg/l. No abnormality was found on plain abdominal radiograph or erect chest radiograph. A clinical diagnosis of acute diverticulitis was made; initial management of fluid resuscitation, intravenous antibiotics and observation was commenced.
After 24 h, he was systemically more stable but there was little improvement in abdominal findings; therefore, a computed tomography (CT) scan of his abdomen and pelvis was arranged. The images revealed focal diverticular perforation in the sigmoid colon by a linear hyperdense structure with the reactive inflammatory changes in the caecal pole and base of the appendix. Minimal improvement on antibiotics coupled with a suspected foreign body led to the decision for operative intervention. Anticoagulation was reversed with human prothrombin complex concentrate and the patient was taken to theatre for a diagnostic laparoscopy.
Figure 1.
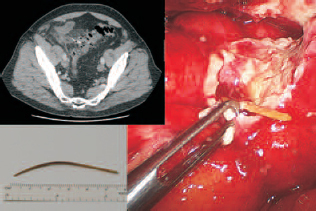
CT and laparoscopic appearance with measurement of sigmoid perforation from a bone, thought to be a chicken fibula.
Under general anaesthetic, an open technique subumbilical 10-mm port was inserted followed by left iliac fossa 10 mm and suprapubic 5 mm, carbon dioxide insufflation was to 12 mmHg. The phlegmon was opened with blunt dissection revealing a bone; there was no generalised peritonitis or faecal contamination, so, in combination with the CT findings was classified as a Hinchey Grade II. The foreign body was removed revealing a small hole in the sigmoid colon. Following washout with 2 l of 0.9% sodium chloride, an abdominal drain was left in the inflammatory cavity.
The patient was given 5 days of intravenous antibiotics on the ward postoperatively and was walking the following day. He required rate control for his atrial fibrillation and wafarin was recommenced; otherwise recovery was uncomplicated. He remained afebrile postoperatively with decreasing inflammatory markers. On discussion with the patient regarding a chicken drumstick, the conclusion was drawn that the foreign body was a chicken fibula. He did not required further admission for diverticulitis in the following 6 months.
Discussion
Most foreign body perforations of the gastrointestinal tract are discovered intra-operatively, as in this case the patient does not usually recall ingestion, the most common site for foreign body perforation being the terminal ileum.1
Previously, three cases of bowel perforation by chicken bone have been documented with the foreign body discovered during laparotomy.2 Abdominal X-ray is unlikely to detect a foreign body unless it is high bone density or metal, CT scan has a higher yield.3 CT scanning is becoming the first-line examination for acute diverticulitis and, although this case is a rare event, it further highlights the value of this imaging modality in the acute setting.
Traditionally, perforated diverticular disease is managed with laparotomy, sigmoid colectomy and end colostomy (Hartman’s procedure). Increasingly where there is no faecal contamination or purulent peritonitis (Hinchey classification I and II), operative management of diverticular perforation with laparoscopy, washout and drain is being favoured.4,5 In selected patients, this offers a less invasive acute intervention, more rapid recovery and avoids the necessity of a stoma. Should the patient have recurrent symptoms, an interval elective sigmoid colectomy can be considered.
References
- 1.Pinero Madrona A, Fernandez Hernandez JA, Carrasco Prats M, Riquelme Riquelme J, Parrila Paricio P. Intestinal perforation by foreign bodies. Eur J Surg 2000; : 307–9. [DOI] [PubMed] [Google Scholar]
- 2.Akhtar S, McElvanna N, Gardiner KR, Irwin ST. Bowel perforation caused by swallowed chicken bones – a case series. Ulster Med J 2007; : 37–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Coulier B, Tancredi MH, Ramboux A. Spiral CT and multidetector-row CT diagnosis of perforation of the small intestine caused by ingested foreign bodies. Eur Radiol 2004; : 1918–25. [DOI] [PubMed] [Google Scholar]
- 4.Mutter D, Bouras G, Forgione A, Vix M, Leroy J, Marescaux J. Two-stage totally minimally invasive approach for acute complicated diverticulitis. Colorectal Dis 2006; : 501–5. [DOI] [PubMed] [Google Scholar]
- 5.Jaffer U, Moin T. Perforated sigmoid diverticular disease: a management protocol. JSLS 2008; : 188–93. [PMC free article] [PubMed] [Google Scholar]


