Abstract
Oesophagogastric invagination is a relatively rare disease that is primarily caused by a sliding hiatal hernia. We report a successfully treated case of oesophagogastric invagination caused by achalasia. Oesophagogastric invagination should be considered in patients complaining of upper abdominal discomfort.
Keywords: Oesophagogastric invagination, Hiatal hernia, Thoracic surgery
Oesophagogastric invagination is a rare condition that involves intussusception of a gastric section into the distal oesophagus. We report the case of a patient who had successful surgical treatment for oesophagogastric invagination.
Case history
A 22-year-old man visited the emergency department complaining of upper abdominal discomfort, followed by vomiting and abdominal cramps after lunch. An hour later, He developed haematemesis and a fever (38°C), gastrointestinal decompression and gastric acid secretion inhibition. Haemostatics, somatostatin and antibiotics were administered. Emergency endoscopy showed a spherical mass located 30cm from the incisors occupying the lumen, as well as surface erosion and bleeding (Fig 1). Chest and full abdominal computed tomography revealed an expanded oesophageal hiatus. A hiatal hernia was observed; most of the gastric tissue had herniated into the posterior mediastinum (Fig 2).
Figure 1.
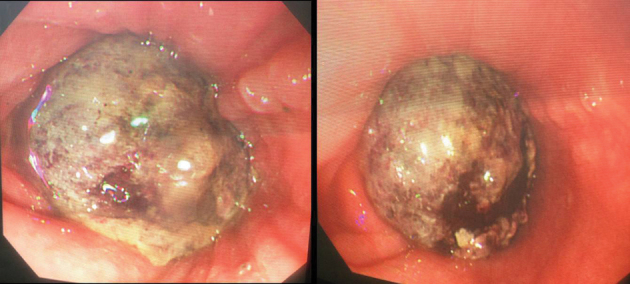
Emergency endoscopy showing a spherical mass located 30cm from the incisors occupying the lumen as well as surface erosion and bleeding
Figure 2.

Chest and full abdominal computed tomography showing an expanded oesophageal hiatus. Most of the gastric tissue has herniated into the posterior mediastinum.
The patient had a seven-year history of oesophageal achalasia and inefficient drug treatment. Consequently, he had undergone a lower oesophageal sphincterotomy (peroral endoscopic myotomy [POEM]). A preliminary clinical diagnosis was made of strangulated hiatal hernia.
An exploratory thoracotomy via a left posterolateral incision was performed. A small amount of light yellow hydrothorax was observed. The mediastinal pleura was incised and the lower segment of the oesophagus freed. The oesophagus was evidently enlarged. Incising from the diaphragm to the oesophageal hiatus, the contents of the hernial sac showed annular strangulation. Further incising the oesophagus and cardia at the point of strangulation, the hernial sac was found to contain the gastric body.
The gastric mucosa had become dark purple and was partly necrosed so we restored the gastric section that had entered the oesophagus. The seromuscular layer still had good vascular supply despite local gastric mucosal hyperaemia, oedema and necrosis. As necrosis was only suspected in the mucosa, the incision on part of the oesophagus and cardia was sutured, the muscular layer was embedded, the diaphragm was sutured and the hiatus was rebuilt. The oesophageal incision was covered with the intercostal muscles. Finally, a drainage tube was placed. The patient recovered from the surgery and was discharged successfully.
Discussion
Oesophagogastric invagination is relatively rare and only very few cases have been reported previously. These cases were caused by a sliding hiatal hernia (SHH). Consequently, it is generally believed that a SHH is the pathological basis of oesophagogastric invagination. Disordered gastrointestinal dynamics is a common reason for alimentary tract intussusception. Numerous factors have been cited and include abnormalities in neurohumoral mechanisms, rhythm disorders relating to action potential transmission, the effect of alimentary tract lesions and surrounding viscera, and a variety of endocrine anomalies. All of these conditions can cause irregular peristalsis of the alimentary tract, which may lead to invagination or its reverse.1
Radiological diagnosis of oesophagogastric invagination presents a formidable problem because the condition usually further alters the position of anatomical landmarks. (This distortion of anatomy already occurs to a certain extent in cases of SHH.) Moreover, the prolapsing mucosal folds of the gastro-oesophageal junction and intermittent invagination of the lower oesophagus into a SHH can themselves mimic the findings of certain malignancies.2–5 Distinguishing oesophagogastric invagination from a carcinoma or other lesions of the gastric cardia is therefore difficult. Numerous examples have been encountered of pseudotumours produced by mucosal prolapse and/or oesophagogastric invagination in patients who were subjected to unnecessary surgery.2,3
Our patient exhibited basic pathological changes of the oesophagus. It had evidently expanded owing to a long history of achalasia. After the POEM, lower oesophageal sphincter function was lost, presenting an anatomical risk factor for SHH or oesophagogastric invagination. Given that diagnosis using imaging and endoscopic examination is difficult, together with the signs of alimentary tract strangulation in our patient, endoscopy could not be performed. Instead, an exploratory thoracotomy was carried out, which confirmed oesophagogastric invagination as the correct diagnosis.
Conclusions
Oesophagogastric invagination should be considered in patients complaining of upper abdominal discomfort.
References
- 1.Ghahremani GG, Collins PA. Esophago-gastric invagination in patients with sliding hiatus hernia. Gastrointest Radiol 1976; : 253–261. [DOI] [PubMed] [Google Scholar]
- 2.Kaye JJ, Stassa G. Mimicry and deception in the diagnosis of tumors of the gastric cardia. Am J Roentgenol Radium Ther Nucl Med 1970; : 295–303. [DOI] [PubMed] [Google Scholar]
- 3.Rudnick JP, Ferrucci JT, Eaton SB, Dreyfuss JR. Esophageal pseudotomor: retrograde prolapse of gastric mucosa into the esophagus. Am J Roentgenol Radium Ther Nucl Med 1972; : 253–256. [DOI] [PubMed] [Google Scholar]
- 4.Walker BQ. The variable roentgenographic appearance of invagination of the esophagus. Based on thirteen cases. Cleve Clin Q 1966; : 35–37. [DOI] [PubMed] [Google Scholar]
- 5.Palmer ED. Mucosal prolapse at the esophagogastric junction. Am J Gastroenterol 1955; : 530–537. [PubMed] [Google Scholar]


