Abstract
Introduction
Emergency general surgery services in England are undergoing rapid structural change with the aim of improving care. In our centre, the key issues identified were high numbers of admissions, inappropriate referrals, prolonged waiting times, delayed senior input and poor patient satisfaction. A new model was launched in January 2015 to address these issues: the surgical triage unit (STU). This study assesses the success of the new service.
Methods
All emergency general surgical admissions during a five-month period before introduction of the STU were compared with those of a comparable five-month period after its introduction. Process, clinical and patient experience outcomes were assessed to identify improvement.
Results
Attendance fell from 3,304 patients in the 2014 cohort to 2,830 in the 2015 cohort. During the 2015 study period, 279 more patients were discharged on the same day. Resource requirement fell by 2,635 bed days (23%). The number of true surgical emergencies remained consistent. Rates for reattendance (7.8% for 2014 vs 8.1% for 2015) and readmission (5.7% for 2014 vs 5.7% for 2015) showed no significant difference. Patient experience data demonstrated a significant improvement in both net promoter score (64.1 vs 82.2) and number of complaints (34 vs 5). Clinical outcomes for low risk procedures remained similar. Emergency laparotomy in-hospital mortality fell (11.4% vs 10.3%) despite preoperative risk stratification suggesting a risk burden that was significantly higher than the national average.
Conclusions
This novel model of emergency general surgery provision has improved clinical efficiency, patient satisfaction and outcomes. We encourage other units to consider similar programmes of service improvement.
Keywords: Emergency surgery, Admissions, Consultant, Improvement
The delivery of emergency general surgery in England is undergoing rapid structural change. Publications by The Royal College of Surgeons of England (RCS) have drawn attention to problems in the delivery of emergency general surgery.1,2 Service improvements are a necessary response to evidence of suboptimal outcomes2–4 but these can only be achieved with recognition and development of innovative practice, both in the UK and worldwide.
Recent studies have presented data associating relatively high mortality rates with common general surgical presentations,2–4 especially in elderly populations. The RCS has produced guidance through documents such as The Higher Risk General Surgical Patient,2 key recommendations including increasing consultant front-line presence as well as objective patient risk assessment with linked prioritisation and resource allocation.1,5
Our centre had practised the standard model of junior-to-senior sequential assessment combined with an ‘open door’ policy of unquestioned and undiscussed admission rights for patients presenting to emergency departments or general practitioners (GPs) in primary care. In common with many other units, our service faced the challenges of high numbers of daily general surgical admissions, long waiting times, insufficient ward space, inappropriate referrals and delayed senior decisions.
Evaluation of our service revealed that 40% of patients admitted had a length of stay (LOS) of 0–1 days, and that a high proportion of this cohort were diagnosed with ‘non-specific abdominal pain’, had normal physiological parameters and did not require surgical admission. In response, a new model of service provision was designed with the broad aims of ensuring that sick patients requiring surgery receive prompt effective treatment while at the same time providing a framework of resources to facilitate efficient and effective management of cases not requiring in-hospital care. In order to accomplish this, consultant front-line presence has been significantly increased and a senior decision maker is available at all times to form a definitive management decision at the earliest opportunity. Additional diagnostic services have also been made available and facilities reconfigured to support these.
After negotiations with the hospital board and regional funding organisations, full approval and funding was granted, and the Nottingham surgical triage unit (STU) opened on 2 January 2015. This study aimed to assess the impact of the service change on workload, clinical outcomes and patient experience.
Methods
All emergency general surgical patients in Nottingham are admitted to the emergency general surgical service based at Queen’s Medical Centre. Prior to 2015, patients were referred to the emergency ward (C31). GP referrals were made to an administrator with no clinical input whereas emergency department admissions were made to junior surgical trainees. All patients were admitted and then clerked by the junior surgical team prior to review by a registrar (within 6 hours) or a consultant (within 12 hours).
In January 2015 the STU was introduced. This was set up similar to an outpatient facility. The space includes a reception and waiting room where patients are seated, two offices, an ultrasonography room and six triage rooms where patients are assessed. Triage rooms contain a desk, chairs and a trolley for examination. There are no ‘beds’ on the STU.
At all times, general surgical referrals are made via the STU mobile phone. During office hours, this phone is held by a consultant surgeon (free from other activity), to offer advice, to redirect to a more appropriate service, or to review the case on the STU or in the emergency department, as necessary. Patients attending the STU are seen by the consultant first and a management decision is made. If a patient is to be admitted to a surgical ward, the surgical team will admit the patient and implement the management plan. The STU consultant then hands over the admitted patient to the appropriate emergency on-call consultant. Outside office hours, the STU continues to function in the same way but the referral phone is held by the senior surgical registrars on duty.
The service is supported by dedicated nursing and administrative staff at all times. A senior (band 7) full-time nurse supports the service on weekdays. Patients not requiring admission can be brought back to the STU for reassessment and further investigation or to a specialty clinic if indicated.
In order to measure the effect of the STU model, all emergency general surgical admissions were reviewed for two five-month periods: January to May 2014 (before introduction of the STU) and January to May 2015 (immediately after the STU was implemented). The same months of the year were chosen for both time periods to avoid seasonal bias.
The data were collected retrospectively using our code for emergency general surgical admission/attendance on our hospital electronic record. International Classification of Diseases (10th revision) codes were checked for diagnosis. Clinical outcome data were retrieved for diagnosis, procedure, LOS, morbidity, in-hospital mortality and readmission. Emergency laparotomy, abscess incision and drainage, appendicectomy and emergency laparoscopic cholecystectomy were selected for analysis as index procedures reflecting the clinical outcomes of an acute general surgical service. All reattending patients had their electronic record scrutinised to determine the reason for reattendance. During the second study period, each STU referral had a proforma completed prospectively. These are recorded on trust electronic patient information systems and contributed to the data. Patient satisfaction data relating to the study periods were retrieved from the trust intranet. From these, a net promoter score (NPS) was calculated as well as a National Health Service Friends and Family Test (FFT) recommendation score.
Statistical analysis
Statistical analysis was performed using Prism® version 4.0 (GraphPad Software, La Jolla, CA, US). Categorical data were compared using the chi-squared test. Normality of distribution was assessed using the D’Agostino and Pearson normality test, prior to unpaired t-test comparison. Non-parametric mean data were compared using the Mann–Whitney U test.
Results
Emergency general surgical attendances fell from 3,304 in the 2014 study period to 2,830 in 2015, equating to a 14.5% reduction. In 2014, 778 patients (23.8%) attending ward C31 were discharged the same day while 2,516 (76.2%) were admitted. In comparison, during the second study period, 1,057 patients (37.3%) were discharged the same day and 1,773 (62.7%) were admitted. The rise in same-day discharges achieved statistical significance (p<0.001, chi-squared test) (Fig 1).
Figure 1.
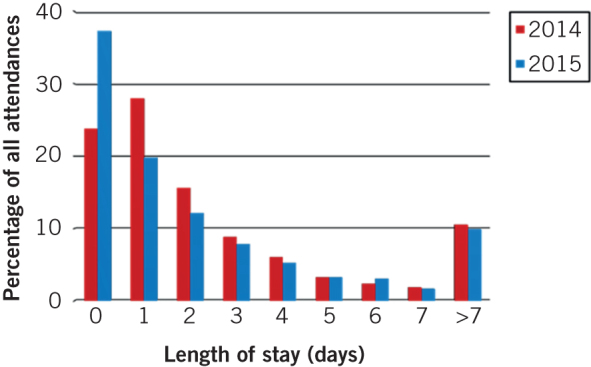
Comparison of length of stay
Following the introduction of the STU, there was a statistically significant fall (p<0.001, chi-squared test) in the number of patients being admitted for short stays (1–4 days). In 2014, 1,927 (58.3%) were admitted for short stays while in 2015, 1,273 (44.9%) had a stay of 1–4 days (Fig 1).
The median LOS was 1.0 days for both time periods. On the other hand, the mean LOS fell significantly from 3.5 days in 2014 to 3.1 days in 2015 (p<0.001, Mann–Whitney U test).
The total number of bed days for acute surgical admissions fell from 11,494 over the study period in 2014 to 8,859 over the same period in 2015. This represents a saving of 2,635 bed days, a 23% reduction.
A remarkably consistent number of true surgical emergencies (eg abscess, appendicitis, acute pancreatitis, bowel obstruction) were observed during the two time periods (Table 1). However, there was a decrease in the number of patients attending with diagnoses such as non-specific abdominal pain, constipation, urinary tract infection and gynaecological problems. There was also a significant fall in the number of patients attending with biliary colic.
Table 1.
Comparison of presentation rates for common primary diagnoses
| Before STU (2014) | n | After STU (2015) | n |
| Non-specific abdominal pain | 751 (22.7%) | Non-specific abdominal pain | 611 (21.6%) |
| Abscess | 282 (8.5%) | Abscess | 268 (9.5%) |
| Cholecystitis | 151 (4.6%) | Cholecystitis | 123 (4.3%) |
| Appendicitis | 141 (4.3%) | Appendicitis | 146 (5.2%) |
| Acute pancreatitis | 137 (4.1%) | Acute pancreatitis | 132 (4.7%) |
| Hernia | 136 (4.1%) | Hernia | 122 (4.3%) |
| Constipation | 123 (3.7%) | Constipation | 72 (2.5%) |
| Diverticulitis | 108 (3.3%) | Diverticulitis | 87 (3.1%) |
| Urinary tract infection | 104 (3.1%) | Urinary tract infection | 36 (1.3%) |
| Biliary colic | 88 (2.6%) | Biliary colic | 41 (1.4%) |
| Gynaecological causes | 87 (2.6%) | Gynaecological causes | 47 (1.7%) |
| Gastroenteritis | 80 (2.4%) | Gastroenteritis | 56 (2.0%) |
| Lower GI bleed | 76 (2.3%) | Lower GI bleed | 69 (2.4%) |
| Small bowel obstruction | 40 (1.2%) | Small bowel obstruction | 56 (2.0%) |
| Chronic pancreatitis | 34 (1.0%) | Chronic pancreatitis | 24 (0.9%) |
| Volvulus | 32 (1.0%) | Volvulus | 26 (0.9%) |
GI = gastrointestinal; STU = surgical triage unit
There was no significant difference in reattendance to the service between the two time periods studied (p=0.641, chi-squared test). In 2014, 259 patients (7.8% of all attendances) reattended within 28 days of discharge while 228 patients (8.1%) reattended in 2015. Of those reattending, 189 were readmitted in 2014 and 162 in 2015, leading to a readmission rate of 5.7% across both time periods. The underlying cause for reattendance also remained stable (Table 2). The median time to reattendance across both study periods was 5 days and the median LOS for patients reattending was 2 days.
Table 2.
Comparison of frequency of causes of reattendance and percentage of all attendances
| Cause of reattendance | Before STU (2014) | After STU (2015) |
| Separate episode of same problem | 96 (2.9%) | 111 (3.9%) |
| Failed discharge | 69 (2.1%) | 44 (1.6%) |
| Emergency surgery (postoperative problem) | 39 (1.2%) | 37 (1.3%) |
| Elective surgery (postoperative problem) | 39 (1.2%) | 25 (0.9%) |
| Missed diagnosis | 16 (0.5%) | 11 (0.4%) |
| Total | 259 (7.8%) | 228 (8.1%) |
STU = surgical triage unit
Clinical outcomes
The clinical outcome data for appendicectomy, abscess incision and drainage, and emergency laparoscopic cholecystectomy are summarised in Table 3. No significant differences were detected between the 2014 and 2015 appendicectomy cohorts for procedure number, LOS, readmission or morbidity. Similarly, for the two abscess incision and drainage groups, there were no significant differences for case number, readmission rate or morbidity. However, the STU 2015 cohort demonstrated a significantly reduced mean LOS (0.6 vs 1.3 days, p<0.005) and length of time spent on the assessment unit (3.8 vs 19.3 hours, p<0.005).
Table 3.
Clinical outcomes before and after introduction of the STU
| Before STU (2014) | After STU (2015) | |
| Appendicectomy | ||
| Cases | 146 | 141 |
| Mean LOS | 2.8 days | 3.3 days |
| Readmission rate | 8.9% | 9.9% |
| Total morbidity rate | 7.1% | 6.2% |
| Abscess incision and drainage | ||
| Cases | 282 | 268 |
| Mean LOS | 1.3 days | 0.6 days |
| Mean time at assessment unit | 19.3 hours | 3.8 hours |
| Readmission rate | 2.9% | 1.9% |
| Total morbidity rate | 2.5% | 1.1% |
| Emergency laparoscopic cholecystectomy | ||
| Cases | 54 | 40 |
| Mean LOS | 5.0 days | 4.0 days |
| Conversion rate | 3.7% | 7.5% |
| Total morbidity rate | 9.0% | 20.0% |
| Bile leak rate (Strasberg A only) | 3.7% | 12.5% |
LOS = length of stay; STU = surgical triage unit
All emergency laparoscopic cholecystectomies were performed under the auspices of hepatopancreatobiliary consultant surgeons. No significant differences were found for case number, conversion rate or LOS. A higher rate of morbidity in terms of low grade bile leak (Strasberg type A)6 was observed in the 2015 cohort (12.5% vs 3.7%) but this did not reach statistical significance. All bile leaks occurred from the cystic duct stump in the context of gangrenous cholecystitis managed by subtotal cholecystectomy. Patients experiencing bile leaks were all successfully managed conservatively. There were no instances of bile duct injury (Strasberg B–E) in either the 2014 or 2015 study periods.
Data presented through the UK National Emergency Laparotomy Audit show a reduction in overall in-hospital mortality at Nottingham University Hospitals NHS Trust from 11.4% in 2014 to 10.3% in 2015 (national average 11%).7 Improvements in mortality outcomes were most pronounced in the elderly population (>70 years), with a 2014 in-hospital mortality rate of 20.9% compared with 15.1% in 2015.
Patient experience
In the 2014 study period, all patients were assessed, admitted and treated via ward C31. Consequently, all data concerning patient experience in this cohort relate to that ward. In 2015 the patient experience was analysed in two groups: those attending the STU for assessment prior to diagnosis, treatment and discharge; and those assessed on the STU prior to admission to C31. Patient experience data are therefore presented for the STU (attenders not admitted) and for C31 (admitted general surgical patients).
During the 2014 study period, 384 patients responded to feedback requests (response rate 30.1%). The NPS was 64.1 (with 35 ‘detractor’ responses) and the FFT recommendation score was 88.8%. Thirty-four complaints were received. Complaint and detractor comment themes included waiting time for medical review, imaging delays, surgery delays, communication issues and noise.
In 2015, 351 patients gave feedback for ward C31 (response rate 35.1%). The NPS was 77.3 (with 8 ‘detractor’ responses) and the FFT recommendation score was 95.7%. There were four complaints. Complaint and detractor comment themes consisted of discharge delays, imaging delays, surgical error and communication issues.
There were 164 feedback responses from STU patients (response rate 39.7%). The NPS was 82.2 (with 10 ‘detractor’ responses) and the FFT recommendation score was 93.3%. One complaint was received following a medication error. Detractor comment themes included referral to other services, waiting time for blood test results and communication issues.
Discussion
The results of our study demonstrate that the service reorganisation described has led to increased clinical and organisational efficiency without compromise of patient safety and with improved patient satisfaction. The STU represents one of several projects aimed at improving all aspects of acute surgical care in our trust. Others include the introduction of a consultant anaesthetist in the theatre coordinator role and strict adherence to UK emergency laparotomy targets (rapid computed tomography, time-to-theatre targets, consultant presence in theatre, intensive care unit access). Together these service changes are associated with an improving trend in mortality outcomes from emergency laparotomy, which compare healthily with the national average.7
Other UK centres have made significant effort and progress in modernising their services. The Blackburn8 and Derby9 models both employ systems based on early registrar level assessment combined with rapid access to bloods tests and imaging investigations. Besides traditional hospital admission, alternative patient outcomes include ‘hot clinic’ review and ambulatory procedure listing.
Similar scenarios are in evidence in other developed countries including the US, the Netherlands, Australia and New Zealand.10,11 A new subspecialty of acute general surgery (AGS) operating through senior-led AGS units is fast becoming a prevalent model in many countries. Publications from such units suggest benefits in terms of appendicitis, acute biliary disease and emergency laparotomy.12–14
For many UK centres, AGS units will be an attractive proposition. For others, the necessity to employ (or retask currently employed) consultant AGS surgeons in significant numbers is prohibitive. Such factors are often in evidence in larger tertiary referral organisations such as ours. In this context, the model described represents a successful method of achieving acute service improvement without surgical workforce expansion.
A striking effect of the introduction of the STU model was a reduction in attendance of emergency general surgery patients by up to 15% and the almost complete elimination of incorrect specialty attendances. This is important as patients may be harmed by unnecessary admission or erroneous specialty referral. The most probable explanation for these improvements is the introduction of consultant referral screening; the availability of a ‘gatekeeper’ with a mobile phone is therefore possibly one of the most important factors in the new model.
Another dramatic change following the launch of the STU was the 56.7% increase in patients discharged on the same day (37.3% after STU vs 23.8% before STU). The 30.4% reduction in one-night stays from 28.0% in 2014 to 19.8% in 2015 translated into 231 fewer patients being admitted overnight. It is also interesting to note the correlation between the 13.4% reduction in patients staying 1–4 days following the introduction of the STU and the 13.5% increase in same-day discharges. This suggests that many of the patients previously needing a short admission are now being managed successfully as outpatients.
Over the first 5 months of the new system, LOS was reduced by 2,635 bed days, equating to a 23% reduction compared with the same months in the previous year. In our institution, this achievement removed the requirement for the equivalent of 14 acute surgical beds (estimated saving £0.8 million), which represents a key opportunity for cost savings. The overall benefit to commissioners from the launch of the STU was in the region of £2.1 million for 2015.
However, the financial impact of improved efficiency is complex to calculate. While there were savings from reduced emergency bed occupancy as well as higher income through increased elective work and target achievement (facilitated by improved patient flow and bed availability), this was counteracted by the increase in staffing requirements, diagnostic resources and capital outlay associated with establishing a service such as the STU. In our trust, these increased costs were estimated to be approximately £870,000 per annum plus ten programmed activity sessions for consultants per week. This is combined with a reduction in departmental income due to the lower number of emergency attendances and admissions.
Our experience was that the clinically desirable outcomes of reduced attendance and admission resulted ultimately in a departmental income reduction from emergency work. In simple terms, fewer admissions meant less money. The local solution was to negotiate a profit sharing agreement with the local commissioning group, allowing financial protection of the service. This illustrates the importance of the imminent renegotiation of acute care tariffs in England so that acute service improvement programmes are not disincentivised.
Conclusions
This evaluation of a novel system of assessment and treatment of acute general surgical cases through the Nottingham STU has produced strong data supporting safe patient outcomes, improved clinical efficiency and outstanding levels of patient satisfaction. We would encourage other surgical units to consider similar programmes of service improvement. The long-term success of these important initiatives will ultimately be determined by support from commissioning groups through the negotiation of reasonable acute surgical care tariffs.
References
- 1.Royal College of Surgeons of England Emergency Surgery. London: RCS; 2011. [Google Scholar]
- 2.Royal College of Surgeons of England, Department of Health The Higher Risk General Surgical Patient. London: RCS; 2011. [Google Scholar]
- 3.Al-Temimi MH, Griffee M, Enniss TM et al. When is death inevitable after emergency laparotomy? Analysis of the American College of Surgeons National Surgical Quality Improvement Program database. J Am Coll Surg 2012; : 503–511. [DOI] [PubMed] [Google Scholar]
- 4.Huddart S, Quiney N, Peden C. Poor outcomes after emergency laparotomy: the United Kingdom response. J Am Coll Surg 2013; : 378–379. [DOI] [PubMed] [Google Scholar]
- 5.Royal College of Surgeons of England, Association of Surgeons of Great Britain and Ireland Commissioning Guide: Emergency General Surgery (Acute Abdominal Pain). London: RCS; 2014. [Google Scholar]
- 6.Strasberg SM, Callery MP, Soper NJ. Laparoscopic surgery of the bile ducts. Gastrointest Endosc Clin N Am 1996; : 81–105. [PubMed] [Google Scholar]
- 7.National Emergency Laparotomy Audit The Second Patient Report of the National Emergency Laparotomy Audit (NELA). London: RCoA; 2016. [Google Scholar]
- 8.Watson R. The delivery of emergency surgical care in a district general hospital. J Assoc Surg G B Irel 2012; : 8–10. [Google Scholar]
- 9.Tierney GM, Tou S, Hender J, Lund JN. Pilot study of a new paradigm in the management of surgical emergencies using emergency surgery ambulatory care. Ann R Coll Surg Engl (Suppl) 2014; : 198–201. [Google Scholar]
- 10.Nagaraja V, Eslick GD, Cox MR. The acute surgical unit model verses the traditional ‘on call’ model: a systematic review and meta-analysis. World J Surg 2014; : 1,381–1,387. [DOI] [PubMed] [Google Scholar]
- 11.Pritchard N, Newbold R, Robinson K, Ooi WM. Effect of the acute general surgical unit: a regional perspective. ANZ J Surg 2015 Dec 17. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 12.Earley AS, Pryor JP, Kim PK. et al. An acute care surgery model improves outcomes in patients with appendicitis. Ann Surg 2006; : 498–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cubas RF, Gómez NR, Rodriguez S. et al. Outcomes in the management of appendicitis and cholecystitis in the setting of a new acute care surgery service model: impact on timing and cost. J Am Coll Surg 2012; : 715–721. [DOI] [PubMed] [Google Scholar]
- 14.Shakerian R, Thomson BN, Gorelik A. et al. Outcomes in emergency general surgery following the introduction of a consultant-led unit. Br J Surg 2015; : 1,726–1,732. [DOI] [PubMed] [Google Scholar]


