Prescribing benzodiazepines (BZDs) for patients receiving opioid agonist therapies is controversial (1). Little has been reported on the regional variation of this practice, a possible marker of clinical uncertainty. We examined regional variation in BZD prescribing for opioid agonist therapy patients in the Veterans Health Administration (VHA) for fiscal year 2010.
The sample included 5,409 methadone maintenance patients and 5,690 buprenorphine maintenance patients, representing all VHA patients with an opioid use disorder in maintenance therapy. Medication exposure was determined by fill dates and days’ supply, except for methadone maintenance prescriptions, which are not recorded in VHA administrative data. To be included in the sample, methadone patients had at least two visits to a VHA opioid maintenance clinic and no buprenorphine prescriptions. Concurrent BZD exposure was defined for methadone patients as a BZD prescription and a maintenance clinic visit in the same 30 days; for buprenorphine patients, it was defined as overlapping BZD and buprenorphine prescriptions. Regions were based on the Veterans Integrated Service Networks (VISNs). We excluded VISNs in which fewer than five patients were prescribed BZDs or in which the 95% confidence intervals around the proportion with concurrent BZD prescriptions were greater than ±10%. Ten of 11 VISNs with BZD prescribing of ≤15% for methadone and all 16 VISNs with ≤25% for buprenorphine patients differed significantly from the VISNs with the greatest BZD prescribing.
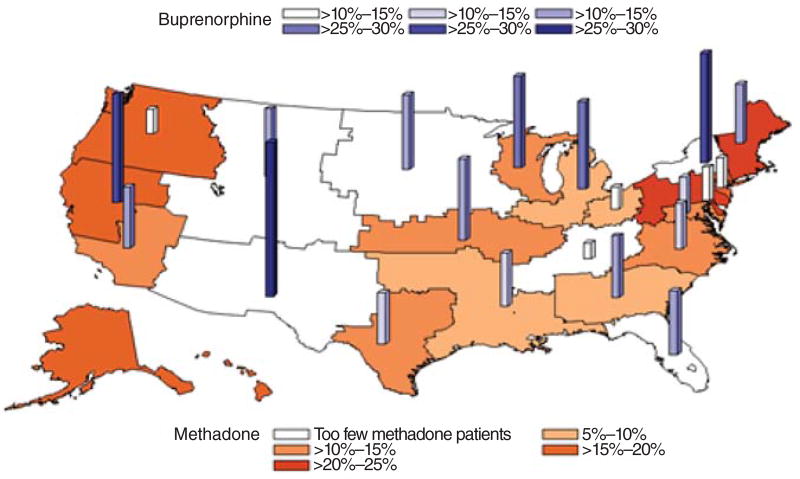
Considerable variation was found in BZD prescribing between the VISNs in the study: range for methadone patients, 6.7%–24.2%; for buprenorphine patients, 11.0%–38.5% (Figure 1). Median BZD prescribing was 13.3% for methadone patients (interquartile range [IQR]=10.0%–17.5%) and 20.2% for buprenorphine patients (IQR=15.3%–24.3%).
Figure 1.
Percentages of patients in opioid agonist therapy in the Veterans Health Administration who were prescribed benzodiazepines, fiscal year 2010
BZD prescribing for patients receiving opioid agonist therapy was not uncommon and varied regionally. This variation in practice may reflect prescriber uncertainty. However, research on the reasons behind it and whether it affects outcomes is warranted.
Footnotes
Disclosures
The authors report no competing interests.
Contributor Information
Dr. Tae Woo Park, Department of Veterans Affairs (VA) Boston Healthcare System
Dr. Amy S. Bohnert, VA Ann Arbor Healthcare System
Ms. Karen Austin, VA Ann Arbor Healthcare System
Dr. Richard Saitz, Boston University School of Medicine
Dr. Steven D. Pizer, Department of Veterans Affairs (VA) Boston Healthcare System
References
- 1.McCowan C, Kidd B, Fahey T. Factors associated with mortality in Scottish patients receiving methadone in primary care: retrospective cohort study. BMJ (Clinical Research Ed) 2009;338:b2225. doi: 10.1136/bmj.b2225. [DOI] [PMC free article] [PubMed] [Google Scholar]