CREATING A STANDARD
In 2015/2016 47% of all cancer diagnoses in Leeds were first referred via the ‘2-week wait’ suspected cancer pathway. Over 25 000 2-week wait referrals were generated from primary care during this period.1 A 2016 audit of Leeds cancer referrals found only 52% to be completed in accordance with referrals guidance. During the same period, Leeds clinical commissioning groups received reports from staff expressing concerns regarding delayed referrals due to process failures. Incomplete forms and delayed referrals have profound implications for patients at a time of heightened stress, and can lead to delay in diagnosis and/or treatment.
To address these issues, a quality improvement project was initiated. The primary aim of the project was to create a standard for the 2-week wait referrals process that improves compliance with referrals guidance and reduces the risk of delayed referrals.
In order to understand referral process variation, analysis was conducted at 11 practices. A video recording was made of a designated staff member completing the entire referral process. Staff responsible for completing the referral process were informally interviewed to establish any concerns regarding the process and its impact on patient care. There was wide variation in the number of ‘clicks’ (mean 20) and ‘time’ (mean 96 seconds) to access and process forms. Eight practices reported recent delayed referrals, often through failure to specify the ‘due date’ and ‘urgency’ of electronic tasks. Clinicians felt referral forms were difficult to access and time-consuming to complete.
ENTER DART
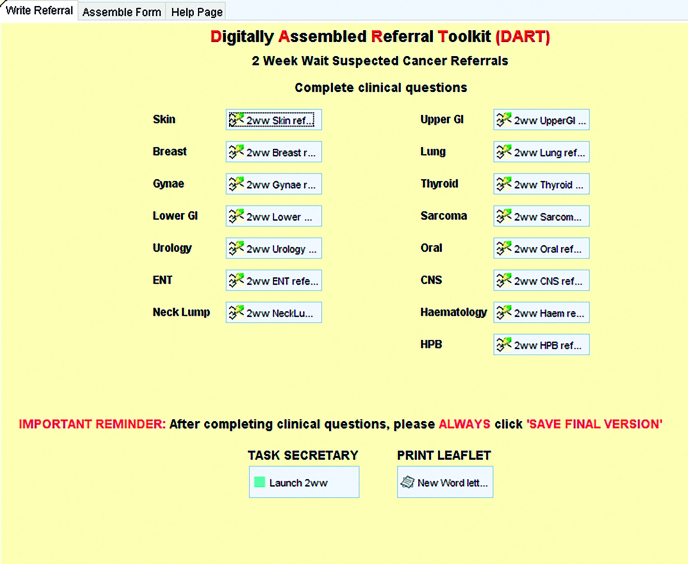
These findings led to the development of the ‘Digitally Assembled Referral Toolkit’ (DART). DART is a proposed ‘standard’ for the referral assembly process and has been created initially for SystmOne (Figure 1). The toolkit can be accessed via a cloud-based template that contains new referral forms native to GP clinical systems.
The new forms contain mandatory fields for core clinical information, thus reducing the risk of incomplete forms and, crucially, consequent delay in assessment. The forms are easy to access and quick to complete.
After completing the new forms, a button can be pressed to automatically assemble a completed MS Word referral form in the style that is expected by secondary care colleagues. The system is able to automatically populate all required information including patient demographics and blood test results. Importantly, if a clinician chooses to send an electronic task, the new process automates input of the ‘urgency’ and ‘due date’ of the task, reducing the risk of delayed referrals. The forms can be centrally updated and the process is easily scalable.
PILOT SUCCESS
A pilot of the new process demonstrated significant improvement in compliance with referrals guidance and the patient experience from initial GP contact. Form completion rates improved from a mean of 44% of forms at baseline (n = 210) to 99% post-intervention n = 236). There was a dramatic increase in the number of times clinicians discussed with patients the nature of the referral (31% pre-, 94% post-), checked their 14-day availability (28% pre-, 99% post-) and issued a safety-netting/information leaflet (2% pre-, 52% post-). Time spent processing forms also decreased from a mean of 96 seconds to 35 seconds post-introduction of the new system.
The Digitally Assembled Referral Toolkit (DART).
The new referrals process reduces risk of incomplete forms, delayed referrals, and any consequent delay in diagnosis and/or treatment. The reduction in time spent processing forms could release over 500 hours of clinical time annually city-wide. This novel use of existing technology could potentially be applied to a number of referral pathways and is easily scalable. After a successful pilot the DART process has now been rolled out city-wide and is available to all SystmOne practices. It is hoped that a similar process will be piloted shortly for the EMIS platform. Reducing delayed referrals improves patient safety and employing a more efficient, leaner process can free up much needed clinical resources.
REFERENCE
- 1.NHS England 2015/16 quarterly provider based cancer waiting times statistics. https://www.england.nhs.uk/statistics/statistical-work-areas/cancer-waiting-times/quarterly-prov-cwt/201516-quarterly-prov-cwt/ (accessed 17 Oct 2017)