Abstract
Background:
The early repair of acute proximal hamstring ruptures provides better clinical results than delayed repair. However, it is unclear how nonoperative treatment compares with the operative treatment of these injuries.
Purpose:
To compare the clinical results of the nonoperative and operative treatment of acute proximal hamstring ruptures.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A total of 25 patients with complete, retracted proximal hamstring ruptures presenting to 1 institution were retrospectively reviewed. All patients were given the option of proximal hamstring repair at the time of the initial evaluation. Patients with at least 12 months of follow-up from the time of surgery or injury were included in the evaluation. Both nonoperative and operative treatment groups were evaluated using the same outcome measures. The primary outcome measure was the Lower Extremity Functional Scale (LEFS). Secondary outcome measures included the Short Form–12 (SF-12) physical and mental component summaries, strength testing, a single-leg hop test, the patient’s perception of strength, and the ability to return to activity.
Results:
There were 11 patients treated nonoperatively, with a mean follow-up of 2.48 ± 3.66 years, and 14 patients treated operatively, with a mean follow-up of 3.56 ± 2.11 years. The mean LEFS scores for the nonoperative and operative groups were 68.50 ± 7.92 and 74.71 ± 5.38, respectively (P = .07). No statistical differences were found between the groups regarding SF-12 scores and mean single-leg hop distance compared with the uninjured leg. Isometric testing of the injured hamstring in the nonoperative group demonstrated significant clinical weakness compared with the uninjured side at both 45° and 90° of flexion (57.54% ± 7.8% and 67.73% ± 18.8%, respectively). Isokinetic testing of the injured leg in the operative group demonstrated 90.87% ± 16.3% strength of the uninjured leg. All patients in the operative group were able to return to preinjury activities, whereas 3 patients in the nonoperative group were unable to return (chi-square = 4.33, P = .07).
Conclusion:
Patients with acute proximal hamstring ruptures treated surgically regained approximately 90% strength of the uninjured extremity and tended to have a greater likelihood of returning to preinjury activities than patients treated nonoperatively.
Keywords: hamstring, proximal hamstring rupture, proximal hamstring repair, outcome
Acute proximal hamstring ruptures are rare injuries that can lead to significant disability if left untreated.11,15 The injury is typically caused by a forced eccentric contraction of the hamstring when the hip is hyperflexed and the ipsilateral knee extended. Many studies have advocated for the early repair of complete proximal hamstring ruptures.7,10,16 Because of the lack of comparative studies, it is unclear if the surgical repair of acute proximal hamstring injuries provides better outcomes than nonoperative treatment.
The purpose of this study was to directly compare the nonoperative and operative treatment of complete proximal hamstring ruptures. We hypothesized that the operative treatment of these injuries would provide better functional outcomes and return to preinjury activities compared with nonoperative treatment.
Methods
A retrospective study of patients with an acute, complete, retracted proximal hamstring rupture treated by a single sports medicine fellowship-trained orthopaedic surgeon (S.L.M.) was performed from 2007 to 2013. The study was approved by an institutional review board, and all patients gave informed consent to participate in the investigation. Noncontrast magnetic resonance imagining (MRI) was used to confirm the injury. An acute injury was defined as ≤6 weeks to the time of the initial evaluation by the senior surgeon. A retracted injury was defined as greater than 2 cm of retraction on MRI.6 After a thorough discussion of the nonsurgical and surgical options at the time of the initial evaluation, it was recommended that patients with acute, complete proximal hamstring ruptures undergo proximal hamstring repair. Patients at least 12 months from injury or surgery were included in this study. Exclusion criteria included patients aged <18 years or >75 years and those with partial proximal hamstring injuries, chronic proximal hamstring injuries, and other musculoskeletal injuries or diseases that precluded physical testing for strength.
Nonsurgical care consisted of rest, ice, physical therapy, selective corticosteroid injections, and gradual return to activities in about 4 months. All patients in the nonoperative group followed the same rehabilitation protocol with formal physical therapy. This consisted of early mobilization, gentle range of motion, and flexibility exercises with progression to strengthening and return to sport within 6 to 12 weeks. Patients were seen every 6 weeks to monitor their rehabilitiation and recovery status. No patients from the nonoperative group crossed over into the operative group.
Surgical repair was performed with patients in the prone position. A transverse incision was made at the gluteal crease, and the caudal edge of the gluteus maximus was identified and retracted proximally. The hamstring sheath was divided longitudinally, and the hematoma was evacuated. The hamstring insertion site on the ischial tuberosity was visualized and prepared for 2 to 4 Q-Fix (Smith & Nephew) double-loaded suture anchors depending on the size of the footprint and quality of the tendon. The proximal edge of the hamstring tendon was retrieved, debrided to viable tissue, and sutured using a running locking suture (Krackow stitch) from one of the suture anchor strands and a modified Mason-Allen stitch from the second strand. The suture from the running locking stitch was used to reduce the tendon to the tuberosity, and all sutures were tied. Care was taken to identify and protect the sciatic nerve throughout the procedure. The incision was closed with a Monocryl (Ethicon) absorbable suture and covered with waterproof dressing. All patients were placed in an X-Act ROM brace (DJO Global). Patients were instructed to wear the brace full-time and maintain toe-touch weightbearing for balance only for 4 weeks. Patients were seen every 6 weeks in the office to monitor rehabilitiation progression and compliance. Full weightbearing out of the brace began in the second month with the initiation of gentle range of motion of the knee and hip. Strengthening and nonimpact aerobic activities were permitted at 8 to 10 weeks with a gradual return to full activities.
All eligible patients (N = 50) were contacted by telephone, and 25 patients agreed to participate. Questionnaires and physical testing were performed at a single visit. Participating patients completed 3 questionnaires: the Short Form–12 (SF-12) with physical and mental component summaries,19 the Lower Extremity Functional Scale (LEFS),2 and a demographic questionnaire developed by the senior author. An independent physical therapist assessed isometric hamstring strength with a handheld dynamometer (Lafayette Instrument) or assessed isokinetic strength with an isokinetic dynamometer (System 3; Biodex) in addition to a single-leg hop test.
Isometric testing was performed in the nonoperative group using a handheld dynamometer.4 The affected hamstring was tested at 45° and 90° of knee flexion with the patient in the prone position. The average of 3 peak force measurements (in kg) was analyzed and compared with the unaffected leg as described previously.11 After initial strength testing of the nonoperative group with a handheld dynamometer, the senior author gained access to a Biodex isokinetic testing device to obtain more quantitative data for strength measurements. After an amendment to the original institutional review board–approved protocol, isokinetic testing was performed in the operative group for a range of motion of 10° to 90° at 300 deg/s.8 Patients performed 3 submaximal contractions at each velocity to become familiar with the exercise. After a short rest, patients then repeated 3 maximal contractions for each velocity on each leg. Peak torque values (in N·m) were averaged and compared with the unaffected leg. The single-leg hop was measured from a starting line to the end of the toes after the completion of a hop.11 The test was demonstrated by the physical therapist, and the patients were allowed 1 trial per leg. Each limb was tested 3 times, and the values were averaged.
The primary outcome measure was the LEFS. Secondary outcome measures included the SF-12 physical and mental component summaries, isometric and isokinetic strength testing, a single-leg hop test, the patient’s perception of strength (0%-100%), and the ability to return to activity.
Descriptive statistics were calculated for continuous and categorical variables by a biomedical statistician using SAS 9.4 (SAS Institute). The normality of continuous data was verified with the Shapiro-Wilk test and 2-sample t test. The Wilcoxon and Mann-Whitney tests were used for normal and nonnormal distributions, respectively. Categorical data were analyzed with the chi-square test and Fisher exact test. The 2-tailed threshold of significance was set at P < .05. Post hoc power analysis demonstrated a power of 0.712 for the LEFS with a minimal clinically important difference of ±9. The LEFS scores were correlated, using a regression analysis, with patient age, functional testing, and perceived strength.
Results
Fourteen patients in the operative group and 11 patients in the nonoperative group participated in the study. The operative group had more female patients (chi-square = 5.31, P = .021) and was younger at the time of the injury and evaluation. The most common mechanism of injury was a slip and fall or from waterskiing. Other mechanisms included injuries sustained during ice hockey, surfing, and rugby. The nonoperative group underwent physical therapy for a mean of 4.63 ± 3.66 months. The mean time from injury to surgery in the operative group was 28.14 ± 14.06 days (range, 15-62 days). The mean follow-up time from injury to evaluation in the nonoperative group and from surgery to evaluation in the operative group was 2.48 ± 3.66 years and 3.56 ± 2.11 years (P = .36), respectively (Table 1).
TABLE 1.
Patient Demographicsa
| Nonoperative Group (n = 11) | Operative Group (n = 14) | P Value | |
|---|---|---|---|
| Male sex, % | 81 | 35 | .02 |
| Age at time of injury, y | 55.68 ± 10.45 | 46.98 ± 9.73 | .048 |
| Age at time of evaluation, y | 58.40 ± 8.32 | 50.62 ± 10.11 | .058 |
| Time from injury/surgery to evaluation, y | 2.48 ± 3.66 | 3.56 ± 2.11 | .36 |
aValues are shown as mean ± SD unless otherwise indicated.
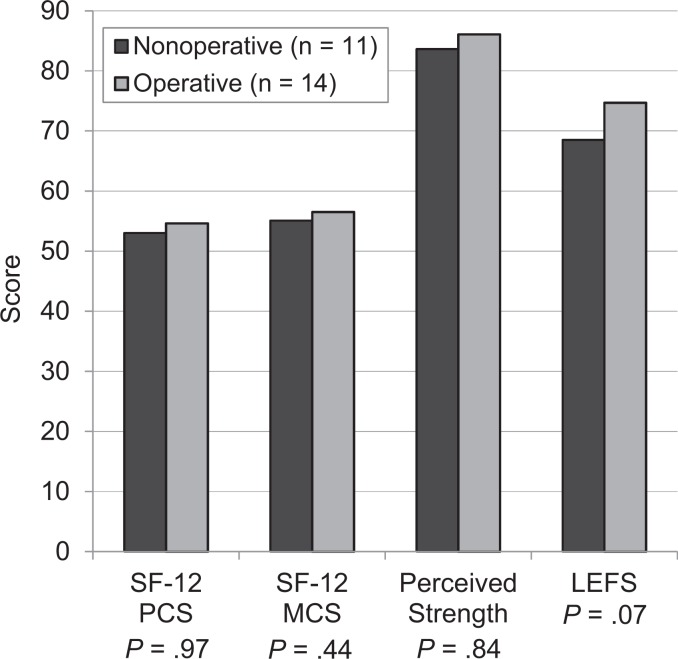
The mean LEFS scores for the nonoperative and operative groups were 68.50 ± 7.92 and 74.71 ± 5.38 (P = .07), respectively. The SF-12 mental and physical component summary scores were similar between the groups. Mean perceived strength of the injured leg in the nonoperative group was 83.64% ± 14.16% and 86.07% ± 12.12% in the operative group (P = .84) (Figure 1). The LEFS score had weak correlations to age, single-leg hop, and perceived strength (R 2 = –0.022, 0.142, and 0.469, respectively).
Figure 1.
Patient-reported outcomes for the nonoperative and operative treatment groups. LEFS, Lower Extremity Functional Scale; SF-12 PCS and MCS, Short Form–12 physical and mental component summaries, respectively.
The mean single-leg hop distance of the injured extremity in the nonoperative group was 56.1 ± 31.2 cm and 119.1 ± 27.7 cm in the operative group (P = .0001). When compared with the uninjured leg, the mean single-leg hop distance in the injured leg was 5.5 ± 12.1 cm and 1.2 ± 17.2 cm shorter in both the nonoperative and operative groups, respectively (P = .51). This corresponds to a mean hop distance of 97.82% ± 26.91% that of the uninjured leg for the nonoperative group and 95.82% ± 9.93% for the operative group (P = .84).
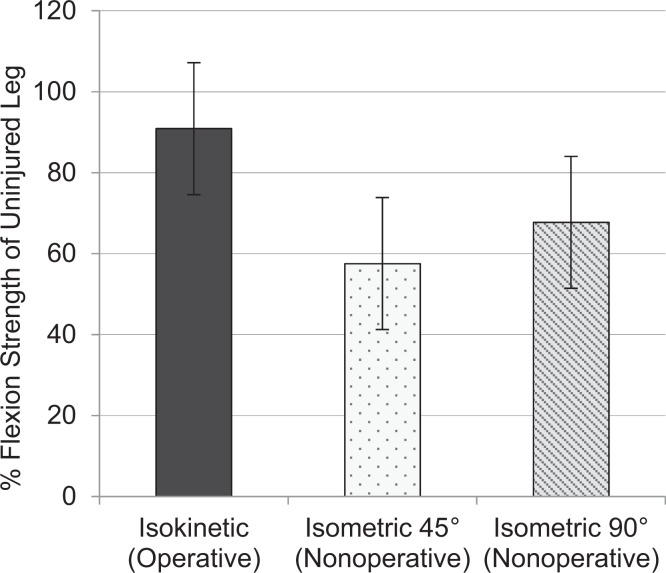
Isometric testing of the injured hamstrings in the nonoperative group demonstrated significant clinical weakness compared with the uninjured side at both 45° and 90° of flexion (57.54% ± 7.8% and 67.73% ± 18.8%, respectively). Isokinetic testing of the injured leg in the operative group demonstrated 90.87% ± 16.3% strength of the uninjured leg at 300 deg/s (Figure 2). Perception of strength did not correlate with measured strength differences in the operative (R 2 = 0.261) and nonoperative (45°: R 2 = 0.016; 90°: R 2 = 0.053) groups.
Figure 2.
Strength testing for the operative and nonoperative treatment groups. Isokinetic testing of the operative group was performed at 300 deg/s (in N·m). Isometric testing of the nonoperative group was performed at 45° and 90° of flexion (in kg).
All patients in the operative group were able to return to preinjury activities. Three of the 11 patients in the nonoperative group were unable to return to preinjury activities (chi-square = 4.33, P = .07). The LEFS score range was 66 to 70 in the 3 patients unable to return to activity. One patient in the operative group required a reoperation for a hematoma. One patient experienced incisional numbness, which improved after 3 months. There were no other reported complications in the operative group.
Discussion
Multiple studies have demonstrated excellent patient satisfaction and functional outcome scores with the surgical repair of complete proximal hamstring ruptures.1,3,6,7,12,14,17,20 Although there was a trend toward higher LEFS scores in our operative group, we were unable to find a significant difference in LEFS scores between the nonoperative and operative groups (68.50 ± 7.92 and 74.71 ± 5.38, respectively; P = .07). Chahal et al,5 Cohen and Bradley,6 and Skaara et al17 reported similar LEFS scores for patients of a comparable age with surgically repaired complete proximal hamstring ruptures: 75 ± 7.8 (mean age, 45 years), 75 (mean age, 48 years), and 71 ± 10 (mean age, 51 years), respectively. Hofmann et al11 previously reported an average LEFS score of 70.2 in conservatively treated complete proximal hamstring ruptures in an older cohort of patients (58.9 ± 8.8 years). There are numerous factors that may have contributed to our inability to find a statistical difference between the nonoperative and operative groups. A larger number of patients in each group may have brought this trend to statistical difference. This may also be attributed to the specific activities rated on the LEFS. The activities questioned mostly include activities of daily living and may not fully reflect the specific requisites for recreational athletes. The high mean LEFS score of the nonoperative group (68.50 ± 7.92 points of 80) is likely a reflection of this as well as a small sample size. Additionally, the LEFS can exhibit a ceiling effect, which can make it difficult to achieve a significant difference (9 points with 90% confidence)2 between the nonoperative and operative groups. We chose the LEFS based on previous studies reporting outcome measures after the surgical treatment of complete proximal hamstring ruptures.2,6,17 An activity scale targeting specific aspects of return to sport may be a more appropriate assessment of treatment outcomes in this patient population.
In a recent systematic review, the surgical repair of complete proximal hamstring ruptures resulted in mean isokinetic strength ranging from 78% to 101% compared with the unaffected side.18 Our study had similar isokinetic testing results in the injured leg of the operative group, with 90.87% ± 16.3% strength of the uninjured leg. It is important to note that not all of the studies within the systematic review reported separate data for acute and delayed repair in addition to the degree of tendon retraction, which may have affected the reported isokinetic strength measurements.18 In comparison, nonoperatively treated proximal hamstring ruptures in our study exhibited 57.54% ± 7.8% and 67.73% ± 18.8% strength of the uninjured leg during isometric testing at 45° and 90° of flexion, respectively. Hofmann et al11 also noted a large deficit in isometric strength compared with the contralateral limb in conservatively treated proximal hamstring ruptures at a mean follow-up of 31 months after the initial injury (61.8% at 45° of flexion; 66.1% at 90° of flexion).
The previously noted systematic review found varying results in return to preinjury sports (76%-100%) and activity levels (55%-100%).18 The systematic review, however, had great heterogeneity in the study population. This is specifically relevant for patient age and sport participation before the injury. One included study by Folsom and Larson9 reported a return to preinjury sporting activity in 76%. Taking a closer look at their patient population, 5 were considered high-level recreational athletes, and 2 were classified as elite athletes of 21 acute, complete proximal hamstring ruptures surgically repaired. The lower rates of return to preinjury sports and activity levels may also be explained by a normal decrease in activity levels with increasing age. The mean age of the patients in the operative group in our study (46.98 ± 9.73 years) was on the upper end of the range reported in a meta-analysis (29-59 years) and consisted of mainly recreational athletes.17 These 2 factors may contribute to the high rate of return to preinjury activities in our surgically repaired group.
Nonoperative care provides unpredictable results. In a small series of 12 water skiers, complete hamstring injuries treated without surgery led to unsatisfactory rates of return to preinjury activity or sports (58%).15 Of those able to return, most patients were unable to return to preinjury functionality. In an older cohort of patients, Hofmann et al11 reported a 40% deficiency in overall strength with isometric testing, a 70% rate of return to preinjury activity, but good patient-reported outcome scores (LEFS score = 70.2). It is important to note, however, that the average age of patients in the Hofmann et al11 cohort was 58.9 ± 8.8 years versus 40 years in the series of water skiers by Sallay et al.15 The nonoperative group in our study more closely resembled that of Hofmann et al,11 with a mean age of 55.68 ± 10.45 years and a mean LEFS score of 68.50 ± 7.92.
Interestingly, we found no significant difference in the mean single-leg hop distance compared with the contralateral limb between the nonoperative and operative groups (5.5 ± 12.1 cm vs 1.2 ± 17.2 cm, respectively; P = .51). Similar results were found in the Hofmann et al11 cohort of conservatively treated complete proximal hamstring avulsions. At an average follow-up of 31 months, they found no significant difference in the average hop distance in the injured extremity nonoperatively treated versus the contralateral limb (57.2 cm vs 58.4 cm, respectively; P = .93). Comparable measurements were found in our study, with a mean hop distance of 56.1 ± 31.2 cm in the conservatively treated injured leg. The most noteworthy variation in our study was the statistically significant difference in the mean single-leg hop distance in the injured extremity between the nonoperative and operative groups (56.1 ± 31.2 cm and 119.1 ± 27.7 cm, respectively; P = .0001). The striking difference in the mean single-leg hop distance in both the injured and uninjured extremities between the study groups may be explained by selection bias, with a significant age difference between the nonoperative and operative groups (55.68 ± 10.45 years vs 46.98 ± 9.73 years, respectively; P = .048) and more male patients within the nonoperative group than the operative group (81% vs 35%, respectively; P = .02). The older group may have experienced an age-related decline in lower extremity strength and agility in addition to the potential fear of fully stressing the injured leg.
Although the complications were minimal, we had 2 notable complications in the operative group. One patient required a reoperation for a postoperative posterior thigh hematoma. The patient resumed the postoperative protocol after hematoma evacuation without further issues. Lefevre et al13 reported a similar complication in 1 of 34 surgically repaired acute proximal hamstring avulsions. They also observed that 55.9% of their patients had notable hematomas on postoperative follow-up. Additionally, 1 patient in our study experienced incisional numbness that resolved within 3 months after surgery. Previous studies have reported higher rates of incisional numbness.3,7 Birmingham et al3 observed incisional numbness at follow-up in 14 of 23 surgically treated proximal hamstring ruptures. Cohen and Bradley6 found postoperative incisional numbness in 20 of 52 patients after repair. It is important to note, however, that most patients were not subjectively symptomatic. Although postoperative incisional numbness is likely underreported, it is noteworthy when counseling patients on possible postoperative complications.
Our study is the first attempt, to date, to directly compare the nonoperative and operative treatment of acute proximal hamstring ruptures. The nonoperative group had fair results (LEFS score = 68.50) with a 72% rate of return to prior activity, despite significant deficits in hamstring strength, which is similar to the results of Hofmann et al.11 There was an overall trend in the operative group toward improved outcomes (LEFS score = 74.7; P = .07), ability to return to preinjury activities (100%; P = .07), and hamstring strength compared with the nonoperative group.
There are several strengths of our study. This is the first case series comparing the nonoperative and operative care of proximal hamstring ruptures in the literature. Second, the LEFS is a validated outcome measure that has been used to assess outcomes in the surgical treatment of proximal hamstring injuries in prior studies.2,6,17 Additionally, the LEFS scores after surgical repair in our study are similar to those reported previously in the literature.5,6,17
Weaknesses of this study include its small sample size, nonrandomized design, demographic differences between the nonoperative and operative groups, only 50% rate of study participation in eligible patients, and lack of data for the nonparticipant group. The study was underpowered (β = 0.712), and more patients were required in each arm of the study to detect true differences in the LEFS score. The second weakness of the study is the significant difference in age, patient sex, and overall physical conditioning between the 2 groups. The nonoperative group was 9 years older (P = .048), had a higher percentage of male patients (P = .02), and had a significantly shorter single-leg hop distance (63 cm shorter; P = .0001). Although not statistically significant, the difference in follow-up times between the nonoperative and operative groups may have affected outcomes (2.48 ± 3.66 years vs 3.56 ± 2.11 years, respectively; P = .36). We also used different means of testing hamstring strength at follow-up in the nonoperative and operative groups because access to a Biodex isokinetic testing device was obtained after initial isometric testing of the nonoperative group with a handheld dynamometer. Although both groups performed their respective testing on both the injured and uninjured extremities for comparison, there may have been some quantitative variation in strength measurements between the different testing methods. We felt that the higher quality of strength measurements associated with isokinetic testing of the operative group outweighed the ability to directly compare strength measurements between the nonoperative and operative groups. Additionally, we only had a 50% participation rate in eligible patients, and therefore, the results of our study may not be applicable to the entire patient population with complete proximal hamstring ruptures. This may have introduced selection bias, as we did not have demographic data on the 25 patients who declined participation because of limitations in the institutional review board–approved protocol and retrospective nature of this study.
In summary, this study is a valid preliminary effort to isolate differences in patient-reported outcomes and rates of return to prior activities between the nonoperative and operative treatment of proximal hamstring injuries. The surgical treatment of acute proximal hamstring ruptures provided excellent functional outcomes and rates of return to preinjury activities. Nonsurgical treatment led to slightly inferior patient outcomes, notable hamstring weakness, and lower rates of return to sport, but further studies are needed to fully elucidate true clinical differences.
Footnotes
Presented at the AOSSM annual meeting, Orlando, Florida, July 2015.
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from the New England Baptist Hospital Institutional Review Board.
References
- 1. Barnett AJ, Negus JJ, Barton T, Wood DG. Reattachment of the proximal hamstring origin: outcome in patients with partial and complete tears. Knee Surg Sports Traumatol Arthrosc. 2015;23(7):2130–2135. [DOI] [PubMed] [Google Scholar]
- 2. Binkley JM, Stratford PW, Lott SA, Riddle DL. The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network. Phys Ther. 1999;79(4):371–383. [PubMed] [Google Scholar]
- 3. Birmingham P, Muller M, Wickiewicz T, Cavanaugh J, Rodeo S, Warren R. Functional outcome after repair of proximal hamstring avulsions. J Bone Joint Surg Am. 2011;93(19):1819–1826. [DOI] [PubMed] [Google Scholar]
- 4. Bohannon RW. Test-retest reliability of hand-held dynamometry during a single session of strength assessment. Phys Ther. 1986;66(2):206–209. [DOI] [PubMed] [Google Scholar]
- 5. Chahal J, Bush-Joseph CA, Chow A, et al. Clinical and magnetic resonance imaging outcomes after surgical repair of complete proximal hamstring ruptures: does the tendon heal? Am J Sports Med. 2012;40(10):2325–2330. [DOI] [PubMed] [Google Scholar]
- 6. Cohen S, Bradley J. Acute proximal hamstring rupture. J Am Acad Orthop Surg. 2007;15(6):350–355. [DOI] [PubMed] [Google Scholar]
- 7. Cohen SB, Rangavajjula A, Vyas D, Bradley JP. Functional results and outcomes after repair of proximal hamstring avulsions. Am J Sports Med. 2012;40(9):2092–2098. [DOI] [PubMed] [Google Scholar]
- 8. Feiring DC, Ellenbecker TS, Derscheid GL. Test-retest reliability of the Biodex isokinetic dynamometer. J Orthop Sports Phys Ther. 1990;11(7):298–300. [DOI] [PubMed] [Google Scholar]
- 9. Folsom GJ, Larson CM. Surgical treatment of acute versus chronic complete proximal hamstring ruptures: results of a new allograft technique for chronic reconstructions. Am J Sports Med. 2008;36(1):104–109. [DOI] [PubMed] [Google Scholar]
- 10. Harris JD, Griesser MJ, Best TM, Ellis TJ. Treatment of proximal hamstring ruptures: a systematic review. Int J Sports Med. 2011;32(7):490–495. [DOI] [PubMed] [Google Scholar]
- 11. Hofmann KJ, Paggi A, Connors D, Miller SL. Complete avulsion of the proximal hamstring insertion: functional outcomes after nonsurgical treatment. J Bone Joint Surg Am. 2014;96(12):1022–1025. [DOI] [PubMed] [Google Scholar]
- 12. Klingele KE, Sallay PI. Surgical repair of complete proximal hamstring tendon rupture. Am J Sports Med. 2002;30(5):742–747. [DOI] [PubMed] [Google Scholar]
- 13. Lefevre N, Bohu Y, Naouri JF, Klouch S, Herman S. Returning to sports after surgical repair of acute proximal hamstring ruptures. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):534–539. [DOI] [PubMed] [Google Scholar]
- 14. Sallay PI, Ballard G, Hamersly S, Schrader M. Subjective and functional outcomes following surgical repair of complete ruptures of the proximal hamstring complex. Orthopedics. 2008;31(11):1092. [PubMed] [Google Scholar]
- 15. Sallay PI, Friedman RL, Coogan PG, Garrett WE. Hamstring muscle injuries among water skiers: functional outcome and prevention. Am J Sports Med. 1996;24(2):130–136. [DOI] [PubMed] [Google Scholar]
- 16. Sarimo J, Lempainen L, Mattila K, Orava S. Complete proximal hamstring avulsions: a series of 41 patients with operative treatment. Am J Sports Med. 2008;36(6):1110–1115. [DOI] [PubMed] [Google Scholar]
- 17. Skaara HE, Moksnes H, Frihagen F, Stuge B. Self-reported and performance-based functional outcomes after surgical repair of proximal hamstring avulsions. Am J Sports Med. 2013;41(11):2577–2584. [DOI] [PubMed] [Google Scholar]
- 18. van der Made AD, Reurink G, Gouttebarge V, Tol JL, Kerkhoffs GM. Outcome after surgical repair of proximal hamstring avulsions: a systematic review. Am J Sports Med. 2015;43(11):2841–2851. [DOI] [PubMed] [Google Scholar]
- 19. Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. [DOI] [PubMed] [Google Scholar]
- 20. Wood DG, Packham I, Trikha SP, Linklater J. Avulsion of the proximal hamstring origin. J Bone Joint Surg Am. 2008;90(11):2365–2374. [DOI] [PubMed] [Google Scholar]