Abstract
Objective:
To evaluate the mode of implementation, clinical outcomes, cost-effectiveness, and the factors influencing uptake and sustainability of collaborative care for psychiatric disorders in older adults.
Design:
Systematic review.
Setting:
Primary care, home health care, seniors’ residence, medical inpatient and outpatient.
Participants:
Studies with a mean sample age of 60 years and older.
Intervention:
Collaborative care for psychiatric disorders.
Methods:
PubMed, MEDLINE, Embase, and Cochrane databases were searched up until October 2016. Individual randomized controlled trials and cohort, case-control, and health service evaluation studies were selected, and relevant data were extracted for qualitative synthesis.
Results:
Of the 552 records identified, 53 records (from 29 studies) were included. Very few studies evaluated psychiatric disorders other than depression. The mode of implementation differed based on the setting, with beneficial use of telemedicine. Clinical outcomes for depression were significantly better compared with usual care across settings. In depression, there is some evidence for cost-effectiveness. There is limited evidence for improved dementia care and outcomes using collaborative care. There is a lack of evidence for benefit in disorders other than depression or in settings such as home health care and general acute inpatients. Attitudes and skill of primary care staff, availability of resources, and organizational support are some of the factors influencing uptake and implementation.
Conclusions:
Collaborative care for depressive disorders is feasible and beneficial among older adults in diverse settings. There is a paucity of studies on collaborative care in conditions other than depression or in settings other than primary care, indicating the need for further evaluation.
Keywords: collaborative care, psychiatric disorders, older adults, clinical outcomes
Abstract
Objectifs:
Évaluer le mode de mise en œuvre, les résultats cliniques, la rentabilité et les facteurs influençant l’adoption et la durabilité de soins en collaboration pour des troubles psychiatriques chez des adultes âgés.
Méthodologie:
Revue systématique.
Contexte:
Soins de première ligne, soins de santé à domicile, résidence de personnes âgées, patients médicaux hospitalisés et externes.
Participants:
Études avec échantillon d’âge moyen de 60 ans et plus.
Intervention:
Soins en collaboration pour des troubles psychiatriques.
Méthodes:
Une recherche a été effectuée dans les bases de données Pubmed, MEDLINE, Embase et Cochrane jusqu’en octobre 2016. Des essais randomisés contrôlés (ERC) individuels, des études de cohorte, cas-témoins, et d’évaluation des services de santé ont été choisis et les données pertinentes ont été extraites pour la synthèse qualitative.
Résultats:
Sur les 552 dossiers identifiés, 53 dossiers (tirés de 29 études) ont été inclus. Très peu d’études ont évalué les troubles psychiatriques autres que la dépression. Le mode de mise en œuvre différait selon le contexte, avec l’utilisation avantageuse de la télémédecine. Les résultats cliniques de la dépression étaient significativement meilleurs comparativement aux soins habituels dans tous les contextes. Dans la dépression, il y a certaines preuves de rentabilité. Il y a des données probantes limitées de soins améliorés de la démence et de résultats issus des soins en collaboration. Il n’y a pas de données probantes d’un bénéfice dans les troubles autres que la dépression ou dans des contextes comme les soins à domicile et les patients généraux hospitalisés en soins actifs. Les attitudes et les compétences du personnel de première ligne, la disponibilité des ressources et le soutien organisationnel sont des facteurs qui influencent l’adoption et la mise en œuvre.
Conclusions:
Les soins en collaboration pour les troubles dépressifs sont faisables et bénéfiques pour les adultes âgés dans divers contextes. Il y a une rareté d’études sur les soins en collaboration pour des affections autres que la dépression ou dans des contextes autres que les soins de première ligne, ce qui indique le besoin de plus d’évaluations.
The proportion of the world population older than 60 years is predicted to double from 12% to 22% between 2015 and 2050, pushing the absolute numbers from 900 million to more than 2 billion people. Moreover, approximately 15% of this population lives with a mental disorder, the most common being dementia, unipolar depression, and anxiety.1
More than 50% of the older adults with mental illnesses do not receive treatment because of stigma or lack of identification and treatment.2 Frequent co-occurrence of medical and psychiatric disorders with age3,4 creates opportunities for their detection and treatment in general and specialist medical settings (e.g., primary care, home health care). Thus, collaboration between mental health and other medical services is crucial in this population.
Collaborative care is based on the chronic care model that includes screening, education, changes in practice, and developments in information technology.5 Widely accepted key areas of collaborative care in mental health, derived from a model defined by Gunn et al.,6 include a multiprofessional approach to patient care, structured management plan, scheduled patient follow-ups, and enhanced interprofessional communication. There is 1 systematic review of randomized controlled trials (RCTs) on collaborative care in the primary care setting for depression in older adults that showed improved depression outcomes compared with usual care.7 There has been no previous attempt to systematically assess its application among older adults in settings beyond primary care, including for psychiatric disorders comorbid with other medical conditions or psychiatric conditions other than depression.
We systematically reviewed collaborative care for psychiatric disorders across different settings, in a study population with mean age of 60 years and over, to assess 1) mode of implementation; 2) clinical outcomes of the psychiatric disorder; 3) other outcomes such as quality of life, functioning, outcome of comorbid medical conditions, caregiver burden, and cost-effectiveness, and 4) factors influencing uptake and sustainability.
Methods
Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines8 guided this review. The review includes published RCTs or prospective or historical cohort, case-control, and qualitative studies for health service evaluation, conducted in primary care, specialist medical inpatient and outpatient setting, home health care, and senior independent residential settings. Inclusion criteria included 1) at least 3 of 4 collaborative care criteria by Gunn et al.,6 2) focus on at least 1 psychiatric disorder, and 3) sample mean age of 60 years or older. Narrative review articles, protocols, editorials, commentaries and letters or case reports were excluded.
We used the following databases: PubMed, MEDLINE, Embase, Psychinfo, and Cochrane Library. We searched for publications in indexed journals until October 2016 without an early date limit, among the adult population aged greater than 18 years. This was done to broaden the scope and include studies in which the inclusion age may be less but the mean sample age was 60 years or older. Studies in the older population are few, and findings of studies with a mean sample age of 60 years and older were thought to be relevant to older adults.
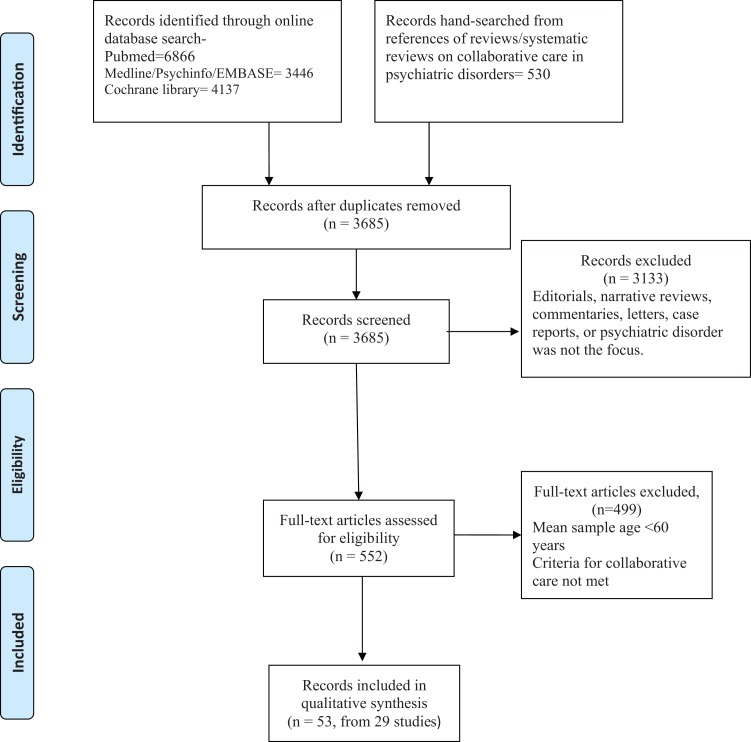
We used the following search terms and their variations: “collaborative care,” “integrated care,” “shared care” AND “mental illness,” “psychiatric disorder.” Additional records were identified from the previous reviews on collaborative care (Figure 1).
Figure 1.
Process of selection of studies for the systematic review.
The first author (P.D.) screened the titles and abstracts to assess eligibility for inclusion. Full articles were reviewed in case of doubt regarding eligibility. From the eligible studies, information was extracted using a predesigned form on 1) first author last name; 2) year of publication; 3) setting; 4) study design; 5) psychiatric disorder; 6) study population characteristics; 7) process of implementation of collaborative care; 8) outcomes including rates of intervention, clinical outcomes of psychiatric disorder, outcome of comorbid medical illness, quality of life, functioning, caregiver impact, cost-effectiveness; and 9) factors influencing uptake and implementation.
It was not feasible to carry out a meta-analysis because of methodological heterogeneity among the studies included, the lack of consistent quantitative data in some of them, the different types of information reported in the original papers, and different scales used for outcome measures. Thus, the results of the review are presented in a narrative way.
Results
Figure 1 describes the selection process of the reviewed publications. Using the search terms and limits, 6866 published articles were identified on PubMed, 3446 on MEDLINE/Psych Info/Embase, and 4137 in the Cochrane Library. After removing the duplicates, 3685 publications were identified for screening. On excluding editorials, narrative reviews, commentaries, letters, case reports, and studies that did not focus on a psychiatric disorder, 552 publications remained. Of these, 53 publications (29 individual studies) met criteria for qualitative synthesis.
Table 1 describes the studies on clinical outcomes and cost analysis clustered by settings, and Table 2 describes the studies evaluating uptake, implementation, and sustainability. More details about individual studies can be found in Supplementary Tables S1 and S2.
Table 1.
Studies on Collaborative Care Evaluating Clinical and Cost Outcomes.a
| Setting | Authors and Year | Country | Psychiatric Disorder | Study Details | Mean (SD) Age, y |
|---|---|---|---|---|---|
| Primary care clinics | IMPACT | United States | Depression | RCT, N = 1801, CC vs. UC | 71.2 (7.5) |
| PROSPECT | RCT, N=598, CC vs UC | >65 | |||
| PRISM-E | Depression, anxiety, alcohol use | RCT, N = 2022, CC vs. specialist referral | 73.5 (6.2) | ||
| Chew Graham et al., 20079 | United Kingdom | Depression | RCT, N = 105, CC vs. UC | 75.5 (7.5) | |
| Chaney et al., 201110 | United States | RCT, N = 546, CC vs. UC | 64.2 (12.2) | ||
| Abrams et al., 201511 | Depression, anxiety, alcohol | Prospective cohort, N = 1505 | 78.7 (9.8) | ||
| Callahan et al., 200612 | Dementia | RCT, N = 153, CC vs. UC | 77.5 (5.5) | ||
| Vickrey et al., 200613 Brown et al., 201314 | RCT, N = 408, CC vs. UC | 80.1 (6.6) | |||
| Home health care | Ell et al., 200715 | United States | Depression | RCT, N = 311, CC vs. UC | >65 |
| Knight and Houseman, 200816 | Quasi-experimental group design, N = 41 | >65 | |||
| Bruce et al., 201517 | Cluster RCT, N = 306, CC vs. UC | 76.5 (8) | |||
| Seniors residence | Llewellyn-Jones et al., 199918 | Australia | Depression | RCT, N = 220, CC vs. UC | 84.3 (5.8) |
| Waterreus et al., 199419 Blanchard et al., 199920 | United Kingdom | RCT, N = 96, CC vs. UC | 76 | ||
| Ciechownowski et al., 200421 | United States | RCT, N = 138, CC vs. UC | 73 (8.5) | ||
| Bartsch and Rodgers, 200922 | Prospective cohort, N = 138 | 74.1 | |||
| Telehealth | Oslin et al., 200323 | United States | Depression | RCT, N = 97, CC vs. UC | 61.9 (11) |
| Fortney et al., 200724 Pyne et al., 201025 | Prospective cohort, N = 395 | 60 (12.2) | |||
| Emery et al., 201226 | Prospective cohort, N = 150 | 71.7 (7.2) | |||
| Gellis et al., 201427 | RCT, N = 115, CC vs. UC | 79.3 (7.35) | |||
| Medical outpatient (OP) or inpatient setting (IP) | Kominski et al., 200128 | United States | Depression, anxiety, alcohol use | RCT, N = 1687, CC vs. UC | >60 |
| Cole et al., 200629 | Canada | Depression | RCT, N = 157, CC vs. UC | 78 (6.6) | |
| Williams et al., 200730 | United States | RCT, N = 188, CC vs. UC | 60 (12) | ||
| Rollman et al., 200931 | RCT, N = 302, CC vs. UC | 64 (11) | |||
| Bogner et al., 201032 | RCT, N = 58, CC vs. UC | 60.2 (7.4) | |||
| Huffman et al., 201133 Celano et al., 201634 | RCT, N = 175, CC vs. UC | 62.4 (12.5) | |||
| Walker et al., 201435 | United Kingdom | RCT, N = 142, CC vs. UC | 63.7 (8.8) |
aCC, collaborative care; IMPACT, Improving Mood—Promoting Access to Collaborative Treatment; PROSPECT, Prevention of Suicide in Primary Care in Elderly: Collaborative Trial; PRISM-E, Primary care Research In Substance abuse and Mental health for the Elderly; RCT, randomised controlled trial; UC, usual care.
Table 2.
Studies Evaluating the Process of Implementation and Factors Influencing Uptake and Sustainability.
| Authors and Year | Setting | Study Details | Psychiatric Disorder | Collaborative Care Process |
|
| Blasinsky et al., 200636 | IMPACT study in primary care practices (see Table 1) | Qualitative study: site visits and key informant interviews from 7 sites | Depression | As outlined in Table 1 | |
| Casado et al., 200837 | Community-dwelling older adults in Baltimore, MD, USA | Surveys and qualitative analysis. 94 older clients >60 y | Depression | Systematic screening, monitoring, intervention, and liaison by trained case managers from social services | |
| Blevins et al., 200838 | Rural Missouri, USA | Qualitative interviews | Depression | Five different agencies collaborated; systematic screening, assessment, monitoring, and referrals by nurse case manager | |
| Lee et al., 201439 | 16 Family health teams in primary care, Ontario, Canada | Physician surveys, staff interviews, audits; N = 529 patient-caregiver dyads; mean age: 76 (SD: 10) | Dementia | Collaborative interprofessional team-led memory clinics; scheduled follow-up and monitoring |
Our search identified 3 large RCTs (IMPACT, PROSPECT, and PRISM-E, Table 1) that generated 23 publications. Of these, 22 publications focused on clinical outcomes and cost analysis are clustered under their corresponding RCT. The other 27 publications on clinical outcomes and cost analysis are described individually and clustered by setting ( Table 1 ). Four publications (including one from IMPACT) focused on the factors influencing uptake and implementation (Table 2).
IMPACT and PROSPECT studies on collaborative care in primary care for depression in the older population evaluated different aspects of collaborative care. Done in a large sample of 1801 and 598, respectively, they consistently showed significantly better outcomes for depression in collaborative care compared with usual care.40–42
In the IMPACT study, benefit was noted in depression care even in the presence of medical comorbidities such as arthritis43,44 and diabetes45 (Supplementary Table S1). Benefit was noted in the collaborative care compared with usual care in the presence of comorbid anxiety disorders such as panic disorder or posttraumatic stress disorder.46 In the PROSPECT study, the benefit with collaborative care was noted even in the presence of medical comorbidities47 and irrespective of cognitive deficits48 (Supplementary Table S1). Ethnic differences did not influence the benefit with collaborative care compared with usual care49,50 (Supplementary Table S1).
PRISM-E, with a sample size of 2022, showed that depression care integrated within primary care had better client engagement measured as number of visits with a mental health provider.51 The outcomes in integrated care were similar to specialist referral and care52 with no cost increment53 (Supplementary Table S1). There was a reduction in alcohol use in terms of drinks per week and reduced episodes of binge drinking in both groups, with no significant difference based on the model of care54 (Supplementary Table S1).
Three RCTs on collaborative care for depression in home health care15–18 did not show significant differences in depression outcome, although some benefit was noted at 12 months in moderately to severely depressed patients in one study17 (Supplementary Table S1).
Three studies, two RCTs and another cohort study, within the community or community-based social service agencies showed improved outcomes for depression19–22 ( Supplementary Table S1). In one community study in the United Kingdom, improved outcome was noted at 3 months not sustained at 6 and 23 months.19,20 Another RCT in public housing for seniors showed significantly greater response and remission in collaborative care compared with usual care.21 Another cohort study showed significant improvement in the depression scores from baseline to discharge over 12 months. The treatment did not have a comparison group and hence it is difficult to assess if the benefit was because of collaborative interventions.22
Three RCTs in which collaborative care for depression was integrated within primary care settings9–11 had variable outcomes as compared with the larger studies in primary care such as PROSPECT and IMPACT. In one study, at 16 weeks, the ratio of those being depressed was significantly lower.9 In another study, there was no significant group difference in the depression scores at 6 months. The high variability was attributed to the uptake by primary care staff, which showed that at 24 weeks, change in depression scores from baseline in those with 2 case manager visit was significantly lower than those with 4 to 6 case manager visits10 (Supplementary Table S1).
Two RCTs23,27 and 2 prospective cohort studies24,26 used virtual modes of communication for collaborative care in depression. The 2 RCTs showed significantly better outcomes for depression compared with usual care, and benefit was noted compared with baseline, in the cohort studies (Supplementary Table S1).
Seven RCTs used collaborative care for depression in medical settings, 2 in general inpatient settings,28,29 and 5 in specialty inpatient/outpatient clinics30–33,35 (Supplementary Table S1). Of these, all RCTs in specialty services showed significantly better outcomes for depression compared with usual care. Two of these RCTs also showed improved outcomes for diabetes and cardiac disease.32,33
One RCT on collaborative care in dementia showed significantly improved neurobehavioral symptoms of dementia and caregiver stress.12 Another RCT on collaborative care in dementia showed significantly greater adherence to dementia care guidelines, significantly greater confidence among caregivers in collaborative care compared with usual care,13 and closed the disparity in dementia care quality between caregivers with less education and those with higher education14 (Supplementary Table S1).
Two studies specifically focused on process of implementation and highlighted skill level, workload, and limited resources as important barriers to implementing collaborative care37,38 (Supplementary Table S2). Qualitative analysis of the IMPACT study also revealed barriers such as organizational resistance and limited funding. The evaluation of sustainability 1 year after the end of funding found that it was sustained in 5 out of 7 sites in a modified manner. A few sites included it for adults aged more than 18 years, and all of them expanded it to other psychiatric disorders. They also modified the composition of the collaborative care team based on local resources. Sustainability was supported by effectiveness of the model, institutional support, and having trained staff36 (Supplementary Table S2). An assessment of collaborative implementation of a memory clinic in primary care showed overall satisfaction among patients, caregivers, and physicians. One clinic that failed to be sustained was located in a resource-intense area with access to specialist care.39
Discussion
This review broadens the scope of evaluation of collaborative care in older adults by including psychiatric disorders other than depression, settings beyond primary care, application in comorbid medical conditions, and various modes of implementation. It examines not only the outcome of the psychiatric disorder but also other outcomes such as quality of life, functioning, physical health, and cost-effectiveness. Lastly, it includes studies that evaluate factors affecting uptake and implementation.
Among the collaborative care studies for psychiatric disorders in adults, the numbers of studies in people aged 60 years and older are few. Using the broader criterion of mean sample age of 60 years and older in a previous review on depression and anxiety in primary care, only 15 RCTs were identified.55 Applying similar criteria of collaborative care in all psychiatric disorders, we identified 29 studies. While chronic care models using an integrated approach are being evaluated for various medical conditions in frail elderly patients,56 they do not often include mental health.
Most studies in this review focused on depression. There are 2 published studies on dementia.12,13 At-risk alcohol use was included along with depression in the PRISM-E study.51 One study targeted depression, anxiety, and alcohol abuse.28 There are no studies on collaborative care for substance use disorders, psychotic disorders, mild cognitive impairment, or bipolar disorder in late life. In people older than 60 years, the prevalence of psychiatric disorders other than depression is significant and underidentified.57 Comorbidity is common in this age group.58 Substance use or misuse of prescription medication may be frequently associated with medical or psychiatric conditions.59 Comorbidities often complicate treatments and delay recovery.58 Hence, when collaborative care is evaluated and applied in older adults, it may need to target multiple psychiatric conditions along with medical conditions.
Collaborative Care Process Based on Settings
All elements in the collaborative care process are used across most studies. There were, however, some studies that did not include at least 1 element.15,18,22 Lack of systematic follow-up and monitoring resulted in no benefit in some studies.15,18,29 In fact, the physicians involved in the IMPACT study identified proactive follow-up as one of the most helpful components of collaborative care.60 It is also emphasized as an important component for improved outcomes.61
The settings included home health care, seniors community dwellings connected to social services, primary care, specialty care clinics, and hospital inpatient units. The mode of application varied depending on the setting. Most studies integrated the mental health care within the setting. They identified and trained existing staff to assist with coordination and collaboration. In primary care clinics and medical specialty clinics, specific case managers or nurses were trained in mental health to provide screening, education, psychotherapy, monitoring, and links between primary care/specialty care and mental health services.9–11,32,35 On inpatient units, the nurses helped with screening and identification.28–31,33 In home health care settings, the staff was trained to function as mental health case managers.15–18 In community dwellings connected to social services, staff of the social services were trained to screen and identify patients with depression and refer them for appropriate assessment and care.21,37 Primary care physicians and members of the local community were trained in one study22 to screen and identify patients with depression and refer to community mental health teams.
Screening and enhanced referral to psychiatry specialist clinics or community mental health teams was examined in 2 studies.22,51 From the PRISM-E study,52 there is evidence of better engagement when specialist care is collocated within primary care compared with referral to specialist services, and outcomes are similar to specialist referral and care.51,52
Use of technology to enable the process of assessment or care provides insights into the unique ways of executing collaborative care. Telephone disease management to assess and monitor was used for depression24,26,27 and in post–coronary bypass patients with depression.31 One study used telepsychiatry to obtain specialist consultation,24 apart from using telephone assessments. Another used virtual communication and electronic networking to coordinate input from the multidisciplinary team.26 This is important, especially in remote areas where collaborations could be established even in the absence of local specialist services.
Treatment Outcomes
Treatment outcomes using collaborative care can be classified into various domains.
Treatment Rates
The collaborative approach helps to improve treatment initiation and possibly improved compliance. A number of studies found significantly higher treatment rates for depression intervention in terms of mental health contacts15,40,51 and antidepressant use10,12,40 or better adherence to antidepressant medications24,32 compared with usual care (Supplementary Table S1). The impact on treatment rates among ethnic minorities is unclear. It was estimated at 60% to 70% of the treatment rates in the white population in the PROPECT study49 but was no different from the white population in the IMPACT study.50 In the dementia study,14 there was greater adherence to dementia care guidelines and increased linkages to community resources in collaborative care versus usual care.
Treatment Outcomes for Psychiatric Disorder
Only a few studies showed lack of benefit for depression with collaborative care compared with usual care.10,15,18,28,29 Also, the rate of response for depression was quicker62 and remission rates significantly higher in the intervention group compared with usual care.9,21,24,30,40,42
The negative studies are in populations with high disease burden in home health care settings15,17–19 or acute inpatient settings.29,30 The authors have argued that the patients in the home health care setting have high medical morbidity and physical disability. Also, the time-based funding in home health care results in loss to follow-up and monitoring that may undermine the effectiveness of collaborative care. Two studies in the general acute inpatient setting did not show statistically significant benefit compared with usual care but showed reduced inpatient costs.28,30 In the primary care setting, a nonsignificant outcome for depression was linked to poor uptake influenced by physician attitude and skills in one study.10 Thus, acutely unwell patients and poor follow-up either due to high morbidity or lack of proactive engagement may weaken the benefits of collaborative care.
The IMPACT and PROSPECT studies also found that there was benefit with depression management even in the presence of medical comorbidities,43–45,47,63 comorbid anxiety disorders46 irrespective of cognitive function,48 and education or ethnic differences.49,50 The response and remission of depression in the collaborative care group was similar to specialist psychiatry clinics in the PRISM-E study,52 highlighting the effectiveness of collaborative care.
While the only study using collaborative care in dementia showed significant improvement in behavioral and psychological symptoms compared with treatment as usual,12 this is the only study that evaluated clinical outcomes in patients with dementia, and thus, firm conclusions on its impact in dementia cannot be drawn.
Collaborative care models for psychiatric disorders other than depression have not been well studied, with existing studies having mixed results. For at-risk alcohol use included in the PRISM-E study, there was a reduction in alcohol use and binge-drinking episodes in both groups with integrated care and specialist referral.52 No significant difference was noted in terms of outcomes for depression, anxiety, or alcohol use in the only study that evaluated collaborative care for 3 different conditions occurring on their own or in combination.28 The reasons for this are unclear and could relate to lack of specific intervention for these conditions in the study or that tackling multiple psychiatric morbidities is challenging through collaborative care. This needs further investigation.
Secondary Outcomes (Suicidal Ideation, Quality of Life, Social Functioning, Physical Health, Long-term Mortality)
Collaborative care appears to have a positive impact on other aspects of care. Studies show reduction in suicidal ideation62,64 and improved quality of life, functioning, and subjective distress.9,21,24,35,40,41 In the study on dementia patients, it helped reduce caregiver distress12 and improved caregiver confidence in providing care.14
Only a few studies evaluated the impact on physical health status, of which the data from the IMPACT study showed significant improvement in pain scores in patients with arthritis,43 while pain was found to influence treatment outcomes of depression in the PRISM-E study.65 Long-term follow-up of participants in the PROSPECT study showed reduced mortality rates by 24% at 96 months in the intervention group compared with the comparison group (hazard ratio, 0.76; 95% confidence interval CI, 0.57 to 1.00; p = 0.05; Supplementary Table S1).66 When collaborative care was incorporated into the management of medical illness, improvement was noted in diabetes control and cardiac care.32,33 The impact on physical health status is, however, not consistent, with no benefit seen in some studies15,21,22,26 (Supplementary Table S1). In post–coronary bypass and cancer patients with depression, the rates of hospital readmission or mortality were not affected by the collaborative care interventions31,35 (Supplementary Table S1).
The improved outcome in areas other than primary psychiatric disorder could relate to the improvement in mental health or overall improvements in quality of care and monitoring associated with collaborative care.
Health Care Costs
Refer to Supplementary Table S1 for more details. Although there is an overall increased cost with the use of collaborative care, accounting for depression-free days and quality-adjusted life-years (QALYs), the studies suggest a cost benefit. The IMPACT study found that the total outpatient costs were USD $295 higher during the study period, but it was cost-effective after accounting for QALYs.67,68 The PRISM-E study noted a cost benefit in Veterans Affairs settings.53 Telemedicine, however, has higher costs per QALY than other studies on collaborative care (incremental cost of $85 637/QALY).25 In cardiac patients, the cost of collaborative care was $175.27 higher per participant but was cost-effective because of depression-free days and improvement in QALYs (incremental cost-effectiveness of $3337.06/QALY).34
Factors Influencing Uptake and Barriers to Implementation of Collaborative Care
There is a perceived need among various services for this model and a high degree of satisfaction. Effectiveness of the model, institutional support, and presence of trained staff were found to facilitate the process of collaboration and encourage sustainability. Some of the barriers identified are absence of staff skills and attitude, increased workload, and lack of organizational support or funding.36–38 There are only 2 studies evaluating sustainability. The IMPACT study showed that 5 out of 7 sites sustained the model after the funding ended but modified it to include other conditions and local staff members.36 In the case of memory clinics within primary care, it was found that the clinic in a resource-intensive area with easy access to specialists could not be sustained.55
Limitations
Most of the studies were focused on depression, with relatively few evaluating collaborative care in other psychiatric disorders. Hence, it is premature to draw conclusions about its impact in psychiatric disorders other than depression. In addition, nearly half of the publications reviewed were from 3 large RCTs, thus limiting the findings and interpretations. However, the results for collaborative care in depression are consistently positive, even in smaller studies across settings. A final limitation is that we included studies with a sample mean age of 60 years and older, which may not be truly representative of the older population.
Future Directions
We need studies on the impact of collaborative care in older adults for psychiatric conditions other than depression and co-occurring psychiatric disorders with and without medical illnesses. The role of proactive follow-up as well as attitudes and skills of primary care staff need specific focus in future studies since these may have undermined the collaborative care benefit in some situations. More studies are also needed on cost analysis and factors influencing uptake and sustainability, especially in settings other than primary care.
Conclusions
While evidence for the effectiveness of collaborative care in multiple psychiatric disorders with or without medical illnesses is poor and needs further evaluation, it is reasonable to conclude the following in the case of depression:
It is feasible to implement collaborative care models in various settings.
The means of implementation may vary depending on the available local resources. Further, the use of technology may help to overcome limitations without compromising benefits.
There is compelling evidence for depression outcomes using collaborative care.
Some of the implementation barriers identified are staff skills and attitude, workload in primary care, mobilization of resources, and organizational support.
Supplementary Material
Footnotes
Author Contributions: All authors were involved in the study concept and design. Pallavi Dham mainly worked on data acquisition and consolidation. All authors were involved with preparation of the manuscript. All authors have seen and approved the final version of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported in part by a grant received from the CAMH foundation and McMaster foundation as part of the collaborative care initiative. Carrie McAiney is supported in part by the grant received.
Supplemental Material: Supplementary material for this article is available online.
References
- 1. World Health Organization. World report on ageing and health. 2015. WHO http://www.who.int/ageing/publications/world-report-2015/en/.
- 2. Karlin BE, Fuller JD. Meeting the mental health needs of older adults. Geriatrics. 2007;62(1):26–35 [PubMed] [Google Scholar]
- 3. Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43 [DOI] [PubMed] [Google Scholar]
- 4. Fabbri E, An Y, Zoli M, et al. Aging and the burden of multimorbidity: associations with inflammatory and anabolic hormonal biomarkers. J Gerontol A Biol Sci Med Sci. 2015;70(1):63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wagner EH, Austin BT, Von Korff M. Improving outcomes in chronic illness. Manag Care Q. 1996;4(2):12–25. [PubMed] [Google Scholar]
- 6. Gunn J, Diggens J, Hegarty K, et al. A systematic review of complex system interventions designed to increase recovery from depression in primary care. BMC Health Serv Res. 2006;6:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chang-Quan H, Bi-Rong D, Zhen-Chan L, et al. Collaborative care interventions for depression in the elderly: a systematic review of randomized controlled trials. J Investig Med. 2009;57(2):446–455. [DOI] [PubMed] [Google Scholar]
- 8. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chew-Graham CA, Lovell K, Roberts C, et al. A randomised controlled trial to test the feasibility of a collaborative care model for the management of depression in older people. Br J Gen Pract. 2007;57(538):364–370. [PMC free article] [PubMed] [Google Scholar]
- 10. Chaney EF, Rubenstein LV, Liu CF, et al. Implementing collaborative care for depression treatment in primary care: a cluster randomized evaluation of a quality improvement practice redesign. Implement Sci. 2011;6:121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Abrams RC, Bone B, Reid MC, et al. Psychiatric assessment and screening for the elderly in primary care: design, implementation, and preliminary results. J Geriatr. 2015;2015:792043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Callahan CM, Boustani MA, Unverzagt FW, et al. Effectiveness of collaborative care for older adults with Alzheimer disease in primary care: a randomized controlled trial. JAMA. 2006;295(18):2148–2157. [DOI] [PubMed] [Google Scholar]
- 13. Vickrey BG, Mittman BS, Connor KI, et al. The effect of a disease management intervention on quality and outcomes of dementia care: a randomized, controlled trial. Ann Intern Med. 2006;145(10):713–726. [DOI] [PubMed] [Google Scholar]
- 14. Brown AF, Vassar SD, Connor KI, et al. Collaborative care management reduces disparities in dementia care quality for caregivers with less education. J Am Geriatr Soc. 2013;61(2):243–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ell K, Unutzer J, Aranda M, et al. Managing depression in home health care: a randomized clinical trial. Home Health Care Serv Q. 2007;26(3):81–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Knight MM, Houseman EA. A collaborative model for the treatment of depression in homebound elders. Issues Ment Health Nurs. 2008;29(9):974–991. [DOI] [PubMed] [Google Scholar]
- 17. Bruce ML, Raue PJ, Reilly CF, et al. Clinical effectiveness of integrating depression care management into Medicare home health: the Depression CAREPATH Randomized trial. JAMA Intern Med. 2015;175(1):55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Llewellyn-Jones RH, Baikie KA, Smithers H, et al. Multifaceted shared care intervention for late life depression in residential care: randomised controlled trial. BMJ. 1999;319(7211):676–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Waterreus A, Blanchard M, Mann A. Community psychiatric nurses for the elderly: well tolerated, few side-effects and effective in the treatment of depression. J Clin Nurs. 1994;3(5):299–306. [DOI] [PubMed] [Google Scholar]
- 20. Blanchard MR, Waterreus A, Mann AH. Can a brief intervention have a longer-term benefit? The case of the research nurse and depressed older people in the community. Int J Geriatr Psychiatry. 1999;14(9):733–738. [PubMed] [Google Scholar]
- 21. Ciechanowski P, Wagner E, Schmaling K, et al. Community-integrated home-based depression treatment in older adults: a randomized controlled trial. JAMA. 2004;291(13):1569–1577. [DOI] [PubMed] [Google Scholar]
- 22. Bartsch DA, Rodgers VK. Senior reach outcomes in comparison with the Spokane Gatekeeper program. Care Manag J. 2009;10(3):82–88. [DOI] [PubMed] [Google Scholar]
- 23. Oslin DW, Sayers S, Ross J, et al. Disease management for depression and at-risk drinking via telephone in an older population of veterans. Psychosom Med. 2003;65(6):931–937. [DOI] [PubMed] [Google Scholar]
- 24. Fortney JC, Pyne JM, Edlund MJ, et al. A randomized trial of telemedicine-based collaborative care for depression. J Gen Intern Med. 2007;22(8):1086–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pyne JM, Fortney JC, Tripathi SP, et al. Cost-effectiveness analysis of a rural telemedicine collaborative care intervention for depression. Arch Gen Psychiatry. 2010;67(8):812–821. [DOI] [PubMed] [Google Scholar]
- 26. Emery EE, Lapidos S, Eisenstein AR, et al. The Brighten Program: implementation and evaluation of a program to bridge resources of an interdisciplinary geriatric health team via electronic networking. Gerontologist. 2012;52(6):857–865. [DOI] [PubMed] [Google Scholar]
- 27. Gellis ZD, Kenaley BL, Ten Have T. Integrated telehealth care for chronic illness and depression in geriatric home care patients: the Integrated Telehealth Education and Activation of Mood (I-TEAM) study. J Am Geriatr Soc. 2014;62(5):889–895. [DOI] [PubMed] [Google Scholar]
- 28. Kominski G, Andersen R, Bastani R, et al. Upbeat: the impact of a psychogeriatric intervention in VA medical centers Unified psychogeriatric biopsychosocial evaluation and treatment. Med Care. 2001;39(5):500–512. [DOI] [PubMed] [Google Scholar]
- 29. Cole MG, McCusker J, Elie M, et al. Systematic detection and multidisciplinary care of depression in older medical inpatients: a randomized trial. CMAJ. 2006;174(1):38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Williams LS, Kroenke K, Bakas T, et al. Care management of poststroke depression: a randomized, controlled trial. Stroke. 2007;38(3):998–1003. [DOI] [PubMed] [Google Scholar]
- 31. Rollman BL, Belnap BH, LeMenager MS, et al. Telephone-delivered collaborative care for treating post-CABG depression: a randomized controlled trial. JAMA. 2009;302(19):2095–2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bogner HR, de Vries HF. Integrating type 2 diabetes mellitus and depression treatment among African Americans: a randomized controlled pilot trial. Diabetes Educ. 2010;36(2):284–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Huffman JC, Mastromauro CA, Sowden G, et al. Impact of a depression care management program for hospitalized cardiac patients. Circ Cardiovasc Qual Outcomes. 2011;4(2):198–205. [DOI] [PubMed] [Google Scholar]
- 34. Celano CM, Healy B, Suarez L, et al. Cost-effectiveness of a collaborative care depression and anxiety treatment program in patients with acute cardiac illness. Value Health. 2016;19(2):185–191. [DOI] [PubMed] [Google Scholar]
- 35. Walker J, Hansen CH, Martin P, et al. Integrated collaborative care for major depression comorbid with a poor prognosis cancer (SMaRT Oncology-3): a multicentre randomised controlled trial in patients with lung cancer. Lancet Oncol. 2014;15(10):1168–1176. [DOI] [PubMed] [Google Scholar]
- 36. Blasinsky M, Goldman HH, Unutzer J. Project IMPACT: a report on barriers and facilitators to sustainability. Adm Policy Ment Health. 2006;33(6):718–729. [DOI] [PubMed] [Google Scholar]
- 37. Casado BL, Quijano LM, Stanley MA, et al. Healthy ideas: implementation of a depression program through community-based case management. Gerontologist. 2008;48(6):828–838. [DOI] [PubMed] [Google Scholar]
- 38. Blevins D, Morton B, McGovern R. Evaluating a community-based participatory research project for elderly mental healthcare in rural America. Clin Interv Aging. 2008;3(3):535–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lee L, Hillier LM, Heckman G, et al. Primary care-based memory clinics: expanding capacity for dementia care. Can J Aging. 2014;33(3):307–319. [DOI] [PubMed] [Google Scholar]
- 40. Unutzer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288(22):2836–2845. [DOI] [PubMed] [Google Scholar]
- 41. Hunkeler EM, Katon W, Tang L, et al. Long term outcomes from the impact randomised trial for depressed elderly patients in primary care. BMJ. 2006;332(7536):259–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Alexopoulos GS, Katz IR, Bruce ML, et al. Remission in depressed geriatric primary care patients: a report from the prospect study. Am J Psychiatry. 2005;162(4):718–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lin EH, Katon W, Von Korff M, et al. Effect of improving depression care on pain and functional outcomes among older adults with arthritis: a randomized controlled trial. JAMA. 2003;290(18):2428–2429. [DOI] [PubMed] [Google Scholar]
- 44. Lin EH, Tang L, Katon W, et al. Arthritis pain and disability: response to collaborative depression care. Gen Hosp Psychiatry. 2006;28(6):482–486. [DOI] [PubMed] [Google Scholar]
- 45. Williams JW, Jr, Katon W, Lin EH, et al. The effectiveness of depression care management on diabetes-related outcomes in older patients. Ann Intern Med. 2004;140(12):1015–1024. [DOI] [PubMed] [Google Scholar]
- 46. Hegel MT, Unutzer J, Tang L, et al. Impact of comorbid panic and posttraumatic stress disorder on outcomes of collaborative care for late-life depression in primary care. Am J Geriatr Psychiatry. 2005;13(1):48–58. [DOI] [PubMed] [Google Scholar]
- 47. Bogner HR, Cary MS, Bruce ML, et al. The role of medical comorbidity in outcome of major depression in primary care: the PROSPECT study. Am J Geriatr Psychiatry. 2005;13(10):861–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bogner HR, Bruce ML, Reynolds CF, III, et al. The effects of memory, attention, and executive dysfunction on outcomes of depression in a primary care intervention trial: the prospect study. Int J Geriatr Psychiatry. 2007;22(9):922–929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bao Y, Alexopoulos GS, Casalino LP, et al. Collaborative depression care management and disparities in depression treatment and outcomes. Arch Gen Psychiatry. 2011;68(6):627–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Arean PA, Ayalon L, Hunkeler E, et al. Improving depression care for older, minority patients in primary care. Med Care. 2005;43(4):381–390. [DOI] [PubMed] [Google Scholar]
- 51. Bartels SJ, Coakley EH, Zubritsky C, et al. Improving access to geriatric mental health services: a randomized trial comparing treatment engagement with integrated versus enhanced referral care for depression, anxiety, and at-risk alcohol use. Am J Psychiatry. 2004;161(8):1455–1462. [DOI] [PubMed] [Google Scholar]
- 52. Krahn DD, Bartels SJ, Coakley E, et al. PRISM-E: comparison of integrated care and enhanced specialty referral models in depression outcomes. Psychiatr Serv. 2006;57(7):946–953. [DOI] [PubMed] [Google Scholar]
- 53. Wiley-Exley E, Domino ME, Maxwell J, et al. Cost-effectiveness of integrated care for elderly depressed patients in the prism-e study. J Ment Health Policy Econ. 2009;12(4):205–213. [PubMed] [Google Scholar]
- 54. Oslin DW, Grantham S, Coakley E, et al. PRISM-E: Comparison of integrated care and enhanced specialty referral in managing at-risk alcohol use. Psychiatr Serv. 2006;57(7):954–958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Archer J, Bower P, Gilbody S, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. 2012;10:CD006525. [DOI] [PubMed] [Google Scholar]
- 56. MacAdam M. Frameworks of integrated care for the elderly: a systematic review. CPRN Research Report. Ottawa: Canadian Policy Research Networks; April 2008. Available from: http://nasuad.org/sites/nasuad/files/hcbs/files/139/6911/elder_care_framework.pdf [Google Scholar]
- 57. Lish JD, Zimmerman M, Farber NJ, et al. Psychiatric screening in geriatric primary care: should it be for depression alone? J Geriatr Psychiatry Neurol. 1995;8(3):141–153. [DOI] [PubMed] [Google Scholar]
- 58. Gum AM, Cheavens JS. Psychiatric comorbidity and depression in older adults. Curr Psychiatry Rep. 2008;10(1):23–29. [DOI] [PubMed] [Google Scholar]
- 59. Wu LT, Blazer DG. Substance use disorders and psychiatric comorbidity in mid and later life: a review. Int J Epidemiol. 2014;43(2):304–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Levine S, Unutzer J, Yip JY, et al. Physicians’ satisfaction with a collaborative disease management program for late-life depression in primary care. Gen Hosp Psychiatry. 2005;27(6):383–391. [DOI] [PubMed] [Google Scholar]
- 61. Solberg LI, Trangle MA, Wineman AP. Follow-up and follow-through of depressed patients in primary care: the critical missing components of quality care. J Am Board Fam Pract. 2005;18(6):520–527. [DOI] [PubMed] [Google Scholar]
- 62. Bruce ML, Ten Have TR, Reynolds CF, III, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291(9):1081–1091. [DOI] [PubMed] [Google Scholar]
- 63. Harpole LH, Williams JW, Jr, Olsen MK, et al. Improving depression outcomes in older adults with comorbid medical illness. Gen Hosp Psychiatry. 2005;27(1):4–12. [DOI] [PubMed] [Google Scholar]
- 64. Unutzer J, Tang L, Oishi S, et al. Reducing suicidal ideation in depressed older primary care patients. J Am Geriatr Soc. 2006;54(10):1550–1556. [DOI] [PubMed] [Google Scholar]
- 65. Mavandadi S, Ten Have TR, Katz IR, et al. Effect of depression treatment on depressive symptoms in older adulthood: the moderating role of pain. J Am Geriatr Soc. 2007;55(2):202–211. [DOI] [PubMed] [Google Scholar]
- 66. Gallo JJ, Morales KH, Bogner HR, et al. Long term effect of depression care management on mortality in older adults: follow-up of cluster randomized clinical trial in primary care. BMJ. 2013;346:f2570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Katon WJ, Schoenbaum M, Fan MY, et al. Cost-effectiveness of improving primary care treatment of late-life depression. Arch Gen Psychiatry. 2005;62(12):1313–1320. [DOI] [PubMed] [Google Scholar]
- 68. Unutzer J, Katon WJ, Fan MY, et al. Long-term cost effects of collaborative care for late-life depression. Am J Manag Care. 2008;14(2):95–100. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.