Abstract
Objective:
Population aging is accelerating across the world, and older people have a higher risk of mental disorders. Most studies focus on one mental disorder, and only report the current prevalence. Besides, these studies use screening scales for symptoms of mental disorders, which may induce biased results. In this study, we used data for diagnoses based on SCID that had been administered by trained psychiatrists to explore the 1-month and lifetime prevalence of mental disorders among a Chinese aged cohort.
Methods:
Data for this study was derived from the Tianjin Mental Health Survey. Participants were first screened using a General Health Questionnaire and 9 additional items on other risk factors for mental disorders, and then diagnosed with the Chinese version of Structured Clinical Interview for Diagnostic and Statistical Manual (DSM-IV) Axis I disorders. A total of 3,325 people aged 60 and above had valid information, and 1,486 completed the SCID interview.
Results:
The weighted 1-month prevalence of mental disorders was 14.27%, whereas the lifetime prevalence of mental disorders was 24.20%. Most of these participants were female, older, currently not married, of lower education level, and with poor family economic status. Organic mental disorders had the highest 1-month prevalence (4.45%), whereas mood disorder was highest for the lifetime prevalence (9.75%).
Conclusion:
Older Chinese people had a high prevalence of mental disorders. Further research and health services innovations are needed to address the high prevalence in these subgroups among older people.
Keywords: mental disorders, Chinese population, older people
Abstract
Objectifs:
Le vieillissement de la population s'accélère partout au monde, et les personnes âgées sont à risque élevé de troubles mentaux. La plupart des études existantes ont porté sur un seul trouble mental à la fois, et n’ont fait état que de la prévalence actuelle. Par ailleurs, des échelles de dépistage des symptômes de troubles mentaux ont été utilisées et les résultats pourraient être biaisés. Dans cette étude, qui utilise des données et des diagnostics basés sur des entrevues cliniques structurées (SCID) administrées par des psychiatres compétents, nous avons cherché à explorer la prévalence d’un mois et de durée de vie des troubles mentaux chez les personnes âgées chinoises.
Méthodes:
Les données de cette étude ont été tirées du Sondage de santé mentale de Tianjin. Les participants ont d’abord été dépistés à l’aide du Questionnaire général sur la santé et de 9 items additionnels sur d’autres facteurs de risque de troubles mentaux, puis ils ont été diagnostiqués au moyen de la version chinoise de l’entrevue clinique structurée du Manuel diagnostique et statistique des troubles mentaux (DSM-IV), troubles de l’axe I. En tout, 3 325 personnes de 60 ans et plus avaient une information valide au dépistage, et 1 486 ont répondu à l’entrevue SCID.
Résultats:
La prévalence d’un mois pondérée des troubles mentaux était de 14,27 %, tandis que la prévalence de durée de vie des troubles mentaux était de 24,20 %. Les femmes, les personnes les plus âgées, les personnes non mariées présentement, les personnes au faible niveau d’instruction et celles au faible statut économique familial avaient une prévalence plus élevée de troubles mentaux. Les troubles mentaux organiques avaient la prévalence d’un mois la plus élevée (4,45 %), tandis que la prévalence de durée de vie du trouble de l’humeur était la plus élevée (9,75 %).
Conclusion:
Les personnes âgées chinoises avaient une prévalence élevée de troubles mentaux. Il faut plus de recherche et des innovations des services de santé pour aborder la prévalence élevée chez ces sous-groupes de personnes âgées.
Population aging is accelerating rapidly all over the world and has become an important public health issue.1 It was estimated that by 2050 there will be 2 billion people aged 65 years and older globally.1 In China, there were 89.3 million older people in 2000, which accounted for 7% of the total population, and it is projected there will be 332 million (23% of the total population) by 2050, which is greater than the combined older population of North American, Europe, and Japan.2 This high number will significantly challenge the current health care received by older people in China.3
Mental health is a critical component of healthy aging, and older people have a higher risk of developing various mental disorders.4,5 Common mental disorders in later life include mood disorders, anxiety disorders, alcohol use disorder, cognitive impairment, and dementia.4,5 The worldwide prevalence of late-life depression ranges from 4.7% to 16%.6 In developed countries, the prevalence of depression among older people is 0.9% to 49%,7,8 whereas, in developing countries, the prevalence is approximately 21.9%.9 Dementia and cognitive impairment are also common mental disorders among older people.10–12 More than 24.3 million people in the world suffer from dementia,11 and its prevalence ranges from 2.8% to 63.0%.13 Even though developed countries have a higher prevalence, developing countries have the largest number of people with dementia.11 Mild cognitive impairment has a prevalence of 3.6% to 38.4% globally,14–16 with a probability that 50% of cases will progress into dementia within 5 years.14 Alcohol abuse afflicts approximately 1% to 3% of older people, and dementia and depression are common co-morbidities among those who abuse alcohol.17
In China, numerous studies have been conducted on mental health among older people.18–21 However, most of these studies focused on one mental disorder, such as geriatric depression or dementia. The 1-month or current prevalence of a mental disorder is reported by most studies, but the lifetime prevalence tends to be neglected. Besides, screening scales are used to define symptoms of mental disorders in most studies. The screening scales have poorer sensitivity and specificity as compared with highly standardized tools and procedures for the diagnosis of mental disorders. Therefore, it is possible that previous results on the prevalence of mental disorders using screening scales could be biased. In this study, we used data from diagnoses by trained psychiatrists formed using SCID to explore the one-month and lifetime prevalence of mental disorders among older people in China.
Methods
Data and Sampling
Data for this study was derived from the Tianjin Mental Health Survey (TJMHS) conducted from July 2011 to March 2012. TJMHS aimed to describe the general mental health status of urban community dwelling adults (18 y and older) in Tianjin city. Tianjin city has 15 (urban) districts and 3 (rural) counties. This survey covered all18 districts/counties, using multistage stratified and probability proportionate to size sampling. There were 3 levels of the sampling frame, including district/county, street/town, and neighbourhood committee/village. The number of households selected at each primary sampling site (neighbourhood committee/village) was proportional to the size of the population in the district/county and street/town, and the size of the population at the site. In each neighbourhood committee/village, households were randomly selected using a systematic sampling method. In each household, one adult aged 18 y or older was randomly selected, using a computer-generated, random number sequence; this was also used in the random selection for inter-rater reliability assessment and quality assurance monitoring. Finally, a total of 15,538 households from 18 district/county, 48 street/town, and 100 neighbourhood committee/village were selected, and 12,899 people were interviewed in the survey. All of the selected households were contacted by local guides before the survey, and these local guides also assisted the interviewers in obtaining access to the household and conducting the face-to-face interviews. The responses of the participants were recorded in the paper version of the questionnaires and entered into the computer after survey. This study was approved by the medical ethics committee of Tianjin Mental Health Center. Informed consent was obtained from all participants during the survey. In the current report, people aged 60 y and older were included in the analysis, as 60 y is the age threshold commonly used by the WHO22 to define older persons.
Interview Process and Measures
Participants were firstly screened by psychiatric nurses using a Chinese version of the General Health Questionnaire (abbreviated as GHQ),23,24 and 9 additional items that assessed other risk factors for mental disorders. The 9 self-reported items included: very poor physical health, very poor mental health, frequent obsessive thoughts or compulsive behaviours, frequent restriction of behaviour because of phobia(s), frequent feelings of extreme nervousness or anxiety, frequent social problems due to drinking, previous treatment for psychological problems, previous suicidal ideation or behaviour, and observation of significant psychiatric or cognitive problems during the screening. Responses of yes were coded as 1 (positive), and no as 0 (negative). The expanded Chinese version of the GHQ has been used in many epidemiological studies in China with excellent reliability and validity.25
Based on the screening results, all participants were divided into 3 risk groups for mental disorders: high risk (GHQ score higher than 4, had any of the 9 risk factors, or could not complete the screening procedure due to psychological problems), moderate risk (had none of the 9 risk factors and had a GHQ score of 1 to 4), and low risk (had none of the 9 risk factors and had a GHQ score of 0). After the screening process, 15.4% of those with complete screening results were randomly selected for retest within 1 week after the initial screening, and 42.1% completed the retest, with 95.0% displaying a consistent classification into the 3 risk groups (Kappa value = 0.621).
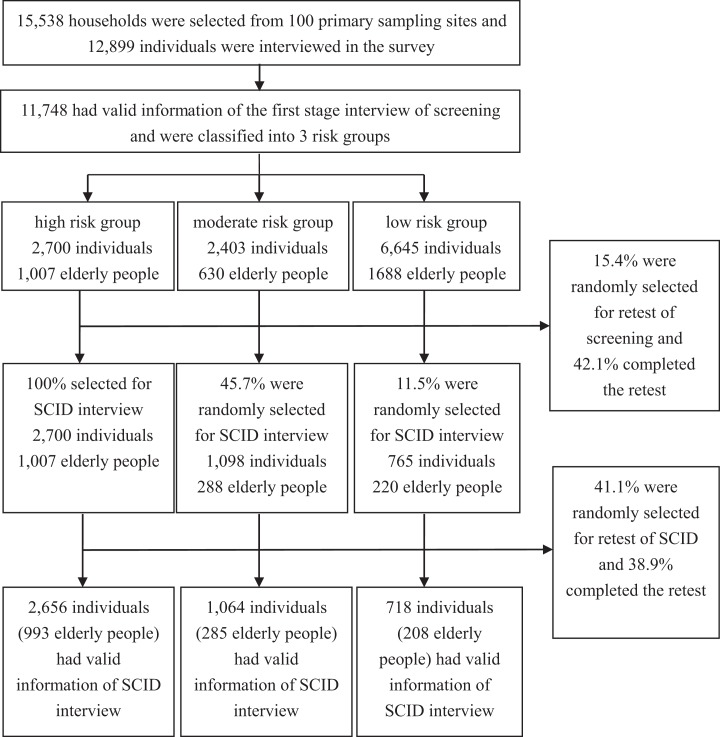
All of the subjects from the high-risk group, 45.7% of subjects from the moderate-risk group, and 11.5% of subjects from the low-risk group were selected for diagnosis of mental disorders by psychiatrists using the Chinese version of the Structured Clinical Interview for Diagnostic and Statistical Manual (DSM-IV) Axis I disorders (abbreviated as SCID).25,26 The Chinese version of SCID has been used in many epidemiological studies in China with excellent reliability and validity.25,27 After the diagnosis, 41.1% of those with complete SCID results were randomly selected for retest within 1 week after the initial diagnosis. This was conducted by a masked interviewer who was unaware of the results of the first assessment. A total of 38.9% completed the retest, with 90.1% having a consistent diagnosis of the mental disorder (there was no statistical differences among the 3 risk groups and the Kappa value was 0.683). All of the psychiatrists and psychiatric nurses were trained for 2 weeks before the survey started. More details of the survey are presented in the flowchart in Figure 1.
Figure 1.
Flowchart of the Tianjin Mental Health Survey.
In this study, mental disorders diagnosed using SCID included 1) Mood disorders: Bipolar I disorder, Bipolar II disorders, Other bipolar disorders, Major depressive disorder, Dysthymic disorder (only current diagnosis), Depressive disorder NOS; 2) Anxiety disorders: Panic disorder, Agoraphobia without panic, Social phobia, Specific phobias, Obsessive-compulsive disorder, Post-traumatic stress disorder, Generalized anxiety disorder (only current diagnosis), Anxiety disorder NOS; 3) Substance use disorders: Alcohol use disorders, Sedative/hypnotic/anxiolytic drug use disorders, cannabis use disorders, Other substance use disorders; 4) Psychotic disorders: Schizophrenia, Schizophreniform disorder, Schizoaffective disorder, Delusional disorder, Brief psychotic disorder, Psychotic disorder NOS; 5) Organic mental disorders: Mood disorder due to GMC, Substance-induced mood disorder, Substance-induced anxiety disorder, Psychotic disorder due to GMC, Substance-induced psychotic disorder; and 6) Other mental disorders: Somatization disorder (only current diagnosis), Pain disorder (only current diagnosis), Somatoform disorder NOS, Hypochondriasis (only current diagnosis), Adjustment disorder (only current diagnosis), eating disorders, impulse control disorders not elsewhere classified.
We used the Chinese version of the Mini Mental State Examination with a theoretical total score of 39 (abbreviated as MMSE)28 and questions about the history of cognitive problems to diagnose mental retardation and dementia. Total scores of MMSE below 24 in illiterate subjects, below 28 in subjects with primary school education, and below 32 in subjects with educational attainment of junior high school or above were considered as having cognitive impairment. For the convenience of the data analysis, we incorporated mental retardation and dementia into Organic mental disorders.
The Global Assessment of Functioning (GAF)29 was used to measure the level of dysfunction due to mental disorders in the past month. Questions on help-seeking behavior were asked. Demographic information collected during the survey included: age, gender, marital status (currently married or currently not married), educational attainment (illiterate or elementary school, junior high school, senior high school, and college and above), and residence (urban area or rural area). Family economic status was asked and coded as good, fair, and poor.
Quality Control
In addition to training of interviewers and retest of SCID, we used the following measures to ensure study quality. Two psychiatrists checked the interview recording form to confirm the accuracy of SCID diagnoses. When the results of the retests were different from the first interview, the psychiatrists listened to the recorded interviews, discussed the case, and determined the final diagnosis. Field supervisors monitored the interview quality throughout the survey. Field supervisors randomly selected the interviewers, monitored the administration of the survey, and answered questions about the conduct of the interviews.
Data Analysis
We used Statistical Product and Service Solutions (SPSS) version 16.0 for data analyses.30 The original records of the responses of the subjects were double-entered and checked using Epidata 3.0, and transferred to SPSS format, with data cleaning conducted before the analysis. The results of the samples with SCID diagnoses were weighted up to reflect the number of individuals in each research site. Then, post-stratification weights were created to make the weighted sociodemographic distribution of the sample comparable in terms of residence location, gender, and age group to that of the 2010 Tianjin population in the 6th national population census of China. Taylor series linearization was used to estimate the adjusted standard errors, and complex survey procedures were used to estimate the prevalence of mental disorders in older people. We interpreted P values less than 0.05 as statistically significant. More details on the survey procedure, methods used in the survey, and data analysis were presented in a previous study.31
Results
Sample Characteristics
Of the 15,538 people selected for interview, 12,899 subjects were investigated. A total of 11,748 subjects completed the first stage of screening and had valid information on GHQ and the 9 screening items, and 4,438 subjects completed the SCID interview and had valid information on the diagnosis of mental disorders. For subjects aged 60 y and above, 3,450 subjects were interviewed and 3,325 subjects had valid information on screening results. Furthermore, 1,486 subjects had valid SCID diagnoses, among which 400 met the criteria for at least one mental disorder in the past month and 624 had experienced at least one mental disorder in their life time (Table 1). Among subjects aged 60 y and above, the response rate in the screening phase was 96.38%, and in SCID interview phase was 98.48%. More details on the non-responder analyses were presented in a previous study,31 in which the results were minimally affected by this non-response.
Table 1.
Sample characteristics of Chinese older people in Tianjin City.
| People with valid screening results | People with valid SCID diagnoses | |
|---|---|---|
| Unweighted number (%) | Unweighted number (%) | |
| Gender | ||
| Male | 1,511 (45.44) | 606 (40.78) |
| Female | 1,814 (54.56) | 880 (59.22) |
| Age | ||
| 60–69 y | 1,842 (55.40) | 751 (50.54) |
| 70–79 y | 1,084 (32.60) | 537 (36.14) |
| 80+ y | 399 (12.00) | 198 (13.32) |
| Marital status | ||
| Currently married | 2,368 (71.26) | 1,003 (67.54) |
| Currently not married | 955 (28.74) | 482 (32.46) |
| Education level | ||
| Illiterate | 546 (16.42) | 264 (17.77) |
| Primary school | 1,091 (32.81) | 518 (34.86) |
| Junior high school | 870 (26.17) | 381 (25.64) |
| Senior high school and above | 818 (24.60) | 323 (21.74) |
| Family economic status | ||
| Good | 202 (6.12) | 63 (4.27) |
| Moderate | 2,506 (75.92) | 1,082 (73.26) |
| Poor | 593 (17.96) | 332 (22.48) |
| Risk groups | ||
| High | 1,007 (29.21) | 993 (66.82) |
| Moderate | 630 (18.28) | 285 (19.18) |
| Low | 1,688 (48.97) | 208 (14.00) |
| Total | 3,325 | 1,486 |
Prevalence of Mental Disorders Older People in China
The weighted number of older people with current mental disorders was 267,322, and the weighted prevalence was 14.27% (95% CI, 11.84 to 16.71) (Table 2). For older people with lifetime mental disorders, the weighted number was 453,199 and the weighted prevalence was 24.20% (95% CI, 20.98 to 27.42) (Table 3). Subjects who were female, oldest, currently not married, of lower education, and with poor family economic status had a higher prevalence of mental disorders. The weighted 1-month prevalence of mental disorders among older people in the high-risk group was 34.24%, whereas, for those in the low-risk group, the prevalence was 5.07%.
Table 2.
One-month prevalence of mental disorders among older people in Tianjin City across sociodemographic characteristics.
| Unweighted number (n)a | Weighted number (n) | Weighted prevalence (%) (95% CI) | |
|---|---|---|---|
| Gender | |||
| Male | 161 | 121,927 | 13.08 (9.46 to 16.70) |
| Female | 239 | 145,396 | 15.46 (12.20 to 18.71) |
| Age | |||
| 60–69 y | 174 | 128,721 | 11.32 (8.48 to 14.15) |
| 70–79 y | 151 | 93,456 | 16.60 (11.63 to 21.57) |
| 80+ y | 75 | 45,146 | 26.18 (17.08 to 35.28) |
| Marital status | |||
| Currently married | 246 | 189,176 | 12.89 (10.13 to 15.65) |
| Currently not married | 154 | 78,146 | 19.30 (14.07 to 24.53) |
| Education level | |||
| Illiterate | 92 | 50,797 | 20.03 (13.63 to 26.42) |
| Primary school | 148 | 105,743 | 17.39 (12.31 to 22.47) |
| Junior high school | 90 | 63,855 | 11.02 (6.84 to 15.20) |
| Senior high school and above | 70 | 46,927 | 10.88 (7.02 to 14.73) |
| Family economic status | |||
| Good | 14 | 11,676 | 13.15 (3.20 to 23.09) |
| Moderate | 263 | 182,638 | 12.73 (9.93 to 15.52) |
| Poor | 119 | 71,054 | 20.57 (14.56 to 26.58) |
| Risk groups | |||
| High | 364 | 189,489 | 34.24 (30.13 to 38.36) |
| Moderate | 24 | 29,828 | 8.02 (2.48 to 13.56) |
| Low | 12 | 48,005 | 5.07 (1.91 to 8.22) |
aThe numbers may not add up to the total sample number due to missing data.
Table 3.
Lifetime prevalence of mental disorders among older people in Tianjin City across sociodemographic characteristics.
| Unweighted number (n)a | Weighted number (n) | Weighted prevalence (%) (95% CI) | |
|---|---|---|---|
| Gender | |||
| Male | 250 | 213,487 | 22.90 (18.02 to 27.79) |
| Female | 374 | 239,712 | 25.48 (21.29 to 29.67) |
| Age | |||
| 60–69 y | 314 | 266,819 | 23.46 (19.22 to 27.70) |
| 70–79 y | 225 | 135,059 | 23.99 (18.30 to 29.69) |
| 80+ y | 85 | 51,322 | 29.76 (20.00 to 39.52) |
| Marital status | |||
| Currently married | 392 | 335,734 | 22.87 (19.18 to 26.56) |
| Currently not married | 232 | 117,465 | 29.01 (22.48 to 35.54) |
| Education level | |||
| Illiterate | 122 | 70,877 | 27.94 (19.77 to 36.11) |
| Primary school | 220 | 166,674 | 27.41 (21.36 to 33.46) |
| Junior high school | 154 | 119,624 | 20.64 (15.07 to 26.21) |
| Senior high school and above | 128 | 96,024 | 22.25 (15.65 to 28.86) |
| Family economic status | |||
| Good | 21 | 15,257 | 17.18 (6.19 to 28.16) |
| Moderate | 426 | 325,632 | 22.69 (18.99 to 26.39) |
| Poor | 170 | 109,746 | 31.77 (23.80 to 39.75) |
| Risk groups | |||
| High | 533 | 280,091 | 50.62 (46.04 to 55.20) |
| Moderate | 66 | 78,692 | 21.17 (14.19 to 28.14) |
| Low | 25 | 94,416 | 9.96 (5.62 to 14.30) |
aThe numbers may not add up to the total sample number due to missing data.
Among the main groups of mental disorders, organic mental disorders showed the highest 1-month prevalence (4.45%), follow by mood disorders (3.61%), whereas, for lifetime prevalence, mood disorders showed the highest prevalence (9.75%) followed by substance use disorders (5.58%) and organic mental disorders (4.66) (Table 4).
Table 4.
Prevalence of main groups of mental disorders among older people in Tianjin City across sociodemographic characteristics.
| Weighted 1-month prevalence (%)(95% CI) | Weighted lifetime prevalence (%) (95% CI) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mood disorders | Anxiety disorders | Substance use disorders | Psychotic disorders | Organic mental disorders | Other mental disorders | Mood disorders | Anxiety disorders | Substance use disorders | Psychotic disorders | Organic mental disorders | Other mental disorders | |
| Total | 3.61 (2.73 to 4.49) | 2.82 (1.43 to 4.21) | 2.45 (1.16 to 3.75) | 0.58 (0.22 to 0.94) | 4.45 (3.33 to 5.58) | 0.35 (0.00 to 0.79) | 9.75 (7.96 to 11.55) | 3.71 (2.23 to 5.19) | 5.58 (3.67 to 7.49) | 0.61 (0.24 to 0.97) | 4.66 (3.52 to 5.80) | 0.45 (0.00 to 0.91) |
| Gender | ||||||||||||
| Male | 2.26 (1.35 to 3.17) | 1.95 (0.27 to 3.63) | 3.75 (1.26 to 6.24) | 0.29 (0.00 to 0.58) | 4.74 (2.96 to 6.52) | 0.10 (0.00 to 0.24) | 5.72 (3.81 to 7.63) | 2.37 (0.62 to 4.12) | 9.91 (6.17 to 13.65) | 0.29 (0.00 to 0.58) | 4.84 (3.05 to 6.62) | 0.19 (0.00 to 0.39) |
| Female | 4.95 (3.46 to 6.44) | 3.68 (1.48 to 5.89) | 1.17 (0.46 to 1.89) | 0.87 (0.22 to 1.53) | 4.17 (2.77 to 5.57) | 0.60 (0.00 to 1.47) | 13.74 (10.77 to 16.71) | 5.04 (2.66 to 7.41) | 1.29 (0.56 to 2.02) | 0.92 (0.26 to 1.58) | 4.49 (3.05 to 5.92) | 0.71 (0.00 to 1.60) |
| Age | ||||||||||||
| 60-69 | 3.01 (2.02 to 4.01) | 2.17 (1.23 to 3.11) | 3.05 (1.01 to 5.10) | 0.74 (0.18 to 1.30) | 1.81 (0.79 to 2.83) | 0.53 (0.00 to 1.25) | 9.61 (7.19 to 12.03) | 3.30 (2.06 to 4.54) | 7.81 (4.78 to 10.84) | 0.74 (0.18 to 1.30) | 1.95 (0.91 to 2.99) | 0.61 (0.00 to 1.34) |
| 70-79 | 4.85 (2.89 to 6.82) | 4.74 (0.58 to 8.89) | 1.53 (0.50 to 2.56) | 0.21 (0.00 to 0.45) | 5.22 (3.40 to 7.05) | 0.05 (0.00 to 0.15) | 11.37 (8.03 to 14.71) | 5.34 (1.15 to 9.53) | 1.74 (0.68 to 2.79) | 0.22 (0.00 to 0.47) | 5.64 (3.75 to 7.54) | 0.22 (0.00 to 0.57) |
| 80+ | 3.53 (0.91 to 6.14) | 0.85 (0.10 to 1.60) | 1.52 (0.00 to 3.47) | 0.76 (0.00 to 1.84) | 19.35 (11.21 to 27.48) | 0.18 (0.00 to 0.54) | 5.40 (2.32 to 8.48) | 1.10 (0.19 to 2.01) | 3.44 (0.00 to 7.24) | 0.96 (0.00 to 2.11) | 19.34 (11.21 to 27.48) | 0.18 (0.00 to 0.54) |
| Marital status | ||||||||||||
| Currently married | 3.04 (2.08 to 4.01) | 2.89 (1.32 to 4.47) | 2.69 (1.07 to 4.30) | 0.38 (0.11 to 0.75) | 3.50 (2.40 to 4.61) | 0.38 (0.00 to 0.94) | 8.20 (6.29 to 10.11) | 3.97 (2.27 to 5.68) | 6.54 (4.13 to 8.95) | 0.38 (0.01 to 0.75) | 3.63 (2.52 to 4.75) | 0.51 (0.00 to 1.09) |
| Currently not married | 5.68 (3.60 to 7.76) | 2.56 (0.00 to 5.51) | 1.62 (0.39 to 2.85) | 1.31 (0.32 to 2.29) | 7.89 (4.58 to 11.20) | 0.24 (0.00 to 0.52) | 15.38 (10.86 to 19.89) | 2.75 (0.00 to 5.71) | 2.10 (0.79 to 3.42) | 1.41 (0.41 to 2.42) | 8.40 (5.03 to 11.77) | 0.24 (0.00 to 0.52) |
| Education level | ||||||||||||
| Illiterate | 5.72 (2.64 to 8.81) | 1.23 (0.00 to 2.53) | 1.99 (0.17 to 3.82) | 0.40 (0.00 to 1.48) | 10.27 (5.83 to 14.71) | 0.11 (0.00 to 0.33) | 12.69 (7.04 to 18.33) | 1.66 (0.10 to 3.22) | 2.10 (0.26 to 3.94) | 0.87 (0.03 to 1.71) | 10.77 (6.24 to 15.31) | 0.11 (0.00 to 0.33) |
| Primary school | 4.11 (2.46 to 5.76) | 2.65 (0.14 to 5.15) | 3.97 (0.56 to 7.39) | 0.74 (0.06 to 1.41) | 5.14 (2.93 to 7.36) | 0.77 (0.00 to 2.10) | 11.00 (7.65 to 14.35) | 4.24 (1.39 to 7.09) | 5.94 (2.23 to 9.65) | 0.74 (0.06 to 1.41) | 5.17 (2.95 to 7.39) | 1.08 (0.00 to 2.46) |
| Junior high school | 2.93 (1.50 to 4.36) | 3.93 (0.59 to 7.27) | 1.81 (0.24 to 3.37) | 0.11 (0.00 to 0.27) | 2.02 (0.66 to 3.38) | 0.22 (0.00 to 0.49) | 7.45 (4.93 to 9.97) | 4.48 (1.09 to 7.87) | 6.30 (2.88 to 9.72) | 0.11 (0.00 to 0.27) | 2.34 (0.92 to 3.76) | 0.22 (0.00 to 0.49) |
| Senior high school and above | 2.58 (1.09 to 4.06) | 2.51 (0.74 to 4.29) | 1.46 (0.00 to 3.03) | 0.93 (0.00 to 2.06) | 3.32 (1.25 to 5.40) | 0.08 (0.00 to 0.23) | 9.35 (5.36 to 13.33) | 3.13 (1.23 to 5.02) | 6.14 (1.72 to 10.57) | 0.93 (0.00 to 2.06) | 3.47 (1.37 to 5.56) | 0.08 (0.00 to 0.23) |
| Family economic status | ||||||||||||
| Good | 8.77 (0.17 to 17.37) | 1.94 (0.00 to 5.41) | 1.03 (0.00 to 3.11) | 0 | 1.41 (0.00 to 3.50) | 0 | 11.93 (2.50 to 21.36) | 1.94 (0.00 to 5.41) | 1.44 (0.00 to 3.71) | 0 | 1.87 (0.00 to 4.20) | 0 |
| Moderate | 2.58 (1.77 to 3.40) | 3.09 (1.32 to 4.86) | 2.91 (1.25 to 4.57) | 0.40 (0.09 to 0.71) | 3.65 (2.49 to 4.81) | 0.11 (0.01 to 0.20) | 8.16 (6.26 to 10.06) | 4.14 (2.25 to 6.02) | 6.48 (4.05 to 8.90) | 0.40 (0.09 to 0.71) | 3.80 (2.62 to 4.97) | 0.17 (0.01 to 0.33) |
| Poor | 6.31 (3.76 to 8.86) | 1.97 (0.59 to 3.34) | 0.96 (0.00 to 2.13) | 1.50 (0.03 to 2.98) | 8.36 (4.63 to 12.10) | 1.47 (0.00 to 3.84) | 15.47 (10.26 to 20.68) | 2.42 (0.90 to 3.95) | 2.94 (0.66 to 5.21) | 1.60 (0.11 to 3.09) | 8.75 (4.96 to 12.54) | 1.73 (0.00 to 4.12) |
Discussion
In this study, using the Tianjin Mental Health Survey, we revealed the 1-month and lifetime prevalence of mental disorders among Chinese older people. Mental disorders in the survey were diagnosed by trained psychiatrists with SCID, and the results can be considered more accurate than previous studies conducted in China using screening scales and laypeople as interviewers.
The 1-month prevalence of mental disorders among Tianjin older subjects was 14.27%. Compared with a study also conducted in other metropolises,32 the prevalence in Tianjin was higher than that in Beijing and Shanghai. This might be explained by several reasons. In the study by Shen and colleagues, a Chinese version of the WHO Composite International Diagnostic Interview (abbreviated as CIDI) was used to assess mental disorders, whereas, in the current study, we used SCID. Schizophrenia was excluded in the study by Shen and colleagues. Besides, Beijing and Shanghai are more urbanized and modernized than Tianjian, and rural older people are more likely to have mental disorders than their urban counterparts.20,33
However, compared with a previous study conducted by Phillips and colleagues,25 which also used SCID to identify mental disorders, the prevalence of mental disorders in Tianjin was lower than that see in the study by Phillips and colleagues. This might be because of the lower proportion of rural residents in the current study (13.7%) as compared with the study by Phillips and colleagues, in which over 70% of the subjects lived in rural communities. Besides, lifestyle, socioeconomic status, and wealth level might be different in rural residents in a metropolis like Tianjin as compared with other cities of China.20,33 For example, because of housing demolition and relocation during urbanization, rural residents in metropolises are often compensated by several apartments and a large quantity of money. Findings from western literature indicate that the prevalence of mental disorders is significantly higher in urban areas as compared with rural areas.34 The high prevalence rate of mental disorders among the older rural Chinese population may be explained by the lack of mental health resources in rural China,25 the ‘empty nest’ scenario,35 or being left-behind.36 Further studies on risk factors for mental disorders in rural China are warranted.
The lifetime prevalence of mental disorders was 24.20% among Chinese older people. Few studies have reported the lifetime prevalence of mental disorders in the Chinese population, and our findings help to fill this current knowledge void. Considering the low proportion of rural residents in the Tianjin survey, the lifetime prevalence among Chinese older people is probably underestimated in our results. Compared with studies in other countries, the prevalence of mental disorders in our study was relatively low. In France, 46% of older people experience a mental disorder in their lifetime.37 In the US, the lifetime prevalence of any mental disorder is 26.1% among older people.38 In South Korea, Cho and colleagues reported that 10% of older Korean subjects had dementia, with depression in 10% to 20% of subjects, and alcohol use disorders reported for 13.6% of subjects.39
This study also revealed several characteristics of the epidemiology of mental disorders among older people in China. Females were more likely to have mood disorder, anxiety disorders, and psychotic disorder than males, whereas males were more likely to have substance use disorders. In China, men were more likely to use alcohol,25,40 which might explain why the prevalence of substance use disorders was approximately 3 times higher in older males that in older females. The prevalence of organic mental disorders was also slightly higher in older males than in females, which might be explained by two reasons: whereas females were more likely to develop dementia than males,41–43 males were at higher risk for injuries,44–47 which can lead to organic mental disorders. Age, educational attainment, and family social economic status were strongly associated with organic mental disorders. As most of the organic mental disorders were dementia, our results were consistent with previous findings that older age,48–50 lower educational attainment,51–54 and lower economic level53 were risk factors for dementia.
There are several main limitations in this study. First, as mentioned above, the rural residents accounted for a low proportion of our cohort, and the results should be interpreted with caution when applied to the entire older population of China. Second, lifetime prevalence rates were based on information collected retrospectively, which might suffer from recall bias. Third, the unequal sampling for phase 2 SCID interviews among the high-, moderate-, and low-risk groups might affect the overall prevalence of mental disorders in older people. False-negative cases of mental disorders in moderate- and low-risk groups and the relatively low sampling proportion in the low-risk group could result in missing cases and lead to an underestimation of the overall prevalence. However, with excellent reliability and validity of the screening tools, we expect the extent of bias to be minimal. Finally, we did not conduct statistical significance of prevalence rates among the different sociodemographic groups.
In conclusion, this study revealed a high prevalence of mental disorders among Chinese older people. As population ageing is rapidly accelerating in China,3 healthcare for older people will bring significant challenges to the Chinese health system as well as social security system in the next few decades. Further research and health service innovations are needed to address the higher numbers of older people in China, especially those of lower educational and economic levels.
Footnotes
Authors’ Contribution: Drs. Guangming Xu and Gong Chen designed the study and wrote the protocol. Dr. Guangming Xu participated in data collection. Dr. Qin Zhou managed the literature searches and the statistical analysis. Dr. Ning Li wrote the first draft of the manuscript, and Dr. Xiaoying Zheng revised the manuscript. All authors contributed to and have approved the final manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) declared receipt of the following financial support for the research, authorship, and/or publication of this article: We acknowledge support for this study from National Social Science Fund (15CRK012).
References
- 1. Kinsella K, Phillips D. Global aging: the challenge of success Washington (DC): Population Reference Bureau; 2005. [Google Scholar]
- 2. England RS. Aging China: the demographic challenge to China’s economic prospects Washington (DC): Greenwood Publishing Group; 2005. [Google Scholar]
- 3. Flaherty JH, Liu ML, Ding L, et al. China: the aging giant. J Am Geriatr Soc. 2007;55(8):1295–1300. [DOI] [PubMed] [Google Scholar]
- 4. Volkert J, Schulz H, Härter M, et al. The prevalence of mental disorders in older people in western countries - a meta-analysis. Ageing Res Rev. 2013;12(1):339–353. [DOI] [PubMed] [Google Scholar]
- 5. Gallo JJ, Lebowitz BD. The epidemiology of common late-life mental disorders in the community: themes for the new century. Psychiatr Serv. 1999;50(9):1158–1166. [DOI] [PubMed] [Google Scholar]
- 6. Barua A, Ghosh MK, Kar N, et al. Prevalence of depressive disorders in the elderly. Ann Saudi Med. 2011;31(6):620–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Blazer DG. Depression in late life: review and commentary. J Gerontol Med Sci. 2003;58(3):249–265. [DOI] [PubMed] [Google Scholar]
- 8. Djernes JK. Prevalence and predictors of depression in population of elderly: a review. Acta Psychiatr Scand. 2006;113(5):372–387. [DOI] [PubMed] [Google Scholar]
- 9. Pilania M, Bairwa M, Kumar N, et al. Elderly depression in India: An emerging public health challenge. Australas Med J. 2013;6(3):107–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ritchie K, Lovestone S. The dementias. Lancet. 2002;360(9347):1759–176 6 [DOI] [PubMed] [Google Scholar]
- 11. Ferri CP, Prince M, Brayne C, et al. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366(9503):2112–2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gauthier S, Reisberg B, Zaudig M, et al. Mild cognitive impairment. Lancet. 2006;367(9518):1262–1270. [DOI] [PubMed] [Google Scholar]
- 13. Mukadam N, Sampson EL. A systematic review of the prevalence, associations and outcomes of dementia in older general hospital inpatients. Int Psychogeriatr. 2011;23(3):344–355. [DOI] [PubMed] [Google Scholar]
- 14. Gauthier S, Reisberg B, Zaudig M, et al. Mild cognitive impairment. Lancet. 2006;367(9518):1262–1270. [DOI] [PubMed] [Google Scholar]
- 15. Ward A, Arrighi HM, Michels S, et al. Mild cognitive impairment: disparity of incidence and prevalence estimates. Alzheimers Dement. 2012;8(1):14–21. [DOI] [PubMed] [Google Scholar]
- 16. Polyakova M, Sonnabend N, Sander C, et al. Prevalence of minor depression in elderly persons with and without mild cognitive impairment: a systematic review. J Affect Disord. 2014;152-154:28–38. [DOI] [PubMed] [Google Scholar]
- 17. Caputo F, Vignoli T, Leggio L, et al. Alcohol use disorder in the elderly: a brief overview from epidemiology to treatment options. Exp Gerontol. 2012;47(6):411–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chan KY, Wang W, Wu JJ, et al. Epidemiology of Alzheimer’s diseases and other forms of dementia in China, 1990-2010: a systematic review and analysis. Lancet. 2013;381(9882):2016–2023. [DOI] [PubMed] [Google Scholar]
- 19. Li Y, Chen C, Tu H, et al. Prevalence and risk factors for depression in older people in Xi’an China: a community-based study. Int J Geriatr Psychiatry. 2012;27(1):31–39. [DOI] [PubMed] [Google Scholar]
- 20. Li N, Pang L, Chen G, et al. Risk factors for depression in older adults in Beijing. Can J Psychiatry. 2011;56(8):466–473. [DOI] [PubMed] [Google Scholar]
- 21. Nie H, Xu Y, Liu B, et al. The prevalence of mild cognitive impairment about elderly population in China: a meta-analysis. Int J Geriatr Psychiatry. 2011;26(6):558–563. [DOI] [PubMed] [Google Scholar]
- 22. World Health Organization. World report on ageing and health Geneva (Switzerland): World Health Organization; 2015. [Google Scholar]
- 23. Golderberg D, Williams P. A user’s guide to the general health questionnaire Windsor (Ontario): NFER-Nelson; 1988. [Google Scholar]
- 24. Yang TZ, Huang L, Wu ZY. Study on the appropriateness of the Chinese version of the General Health Questionnaire as a screening instrument for psychological disorders in mainland China. Chin J Epid. 2003;24(9):769–773. (in Chinese). [PubMed] [Google Scholar]
- 25. Phillips MR, Zhang J, Shi Q, et al. Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001-05: an epidemiological survey. Lancet. 2009;373(9680):2041–2053. [DOI] [PubMed] [Google Scholar]
- 26. First MB, Spitzer RL, Gibbon M, et al. Structured clinical interview for DSM-IV-TR axis i disorders. New York (NY; ): Biometrics Research Department, New York State Psychiatric Institute; 2002. [Google Scholar]
- 27. Zhou RY, Zhang YH, Peng B, et al. Comparison of three diagnostic criteria for the diagnosis of schizophrenia and mood disorders. Chin J Psychiatry. 1997;30(1):45–49 (in Chinese). [Google Scholar]
- 28. WangR, XiongW, Phillips MR. Clinical test of mini-mental state examination in 400 schizophrenia. Zhongguo Minzheng Yixue Zazhi. 1991;1(3):145–148. (in Chinese). [Google Scholar]
- 29. Endicott J, Spitzer RL, Fleiss JL, et al. The global assessment scale. Arch Gen Psychiatry. 1976;33(6):766–771. [DOI] [PubMed] [Google Scholar]
- 30. SPSS Inc. SPSS for windows, version 16.0. Chicago (IL); SPSS Inc; 2007. [Google Scholar]
- 31. Yin H, Phillips MR, Wardenaar KJ, et al. The Tianjin Mental Health Survey (TJMHS): study rationale, design and methods. Int J Methods Psychiatr Res. 2016; doi:10.1002/mpr.1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Shen YC, Zhang MY, Huang YQ, et al. Twelve-month prevalence, severity, and unmet need for treatment of mental disorders in metropolitan China. Psychol Med. 2006;36(02):257–267. [DOI] [PubMed] [Google Scholar]
- 33. Ma X, Xiang YT, Li SR, et al. Prevalence and sociodemographic correlates of depression in an elderly population living with family members in Beijing, China. Psychol Med. 2008;38(12):1723–1730. [DOI] [PubMed] [Google Scholar]
- 34. Peen J, Schoevers RA, Beekman AT, et al. The current status of urban-rural differences in psychiatric disorders. Acta Psychiatr Scand, 2010;121(2):84–93. [DOI] [PubMed] [Google Scholar]
- 35. Xie LQ, Zhang JP, Peng F, et al. Prevalence and related influencing factors of depressive symptoms for empty-nest elderly living in the rural area of YongZhou, China. Arch Gerontol Geriatr. 2010;50(1):24–29. [DOI] [PubMed] [Google Scholar]
- 36. He G, Xie J, Zhou J, et al. Depression in left-behind elderly in rural China: prevalence and associated factors. Geriatr Gerontol Int. 2016;16(5):638–643. [DOI] [PubMed] [Google Scholar]
- 37. Ritchie K, Artero S, Beluche I, et al. Prevalence of DSM-IV psychiatric disorder in the French elderly population. Br J Psychiatry. 2004;184(2):147–152. [DOI] [PubMed] [Google Scholar]
- 38. Kessler RC, Wang PS. The descriptive epidemiology of commonly occurring mental disorders in the United States. Annu Rev Public Health. 2008;29:115–129. [DOI] [PubMed] [Google Scholar]
- 39. Cho MJ, Lee JY, Kim BS, et al. Prevalence of the major mental disorders among the Korean elderly. J Korean Med Sci. 2011;26(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hao W, Su Z, Liu B, et al. Drinking and drinking patterns and health status in the general population of five areas of China. Alcohol Alcohol. 2004;39(1):43–52. [DOI] [PubMed] [Google Scholar]
- 41. Li S, Yan F, Li G, et al. Is the dementia rate increasing in Beijing? Prevalence and incidence of dementia 10 years later in an urban elderly population. Acta Psychiatr Scand. 2007;115(1):73–79. [DOI] [PubMed] [Google Scholar]
- 42. Zhang Z, Zahner G, Roman G, et al. Dementia subtypes in China: prevalence in Beijing, Xian, Shanghai, and Chengdu. Arch Neurol. 2005;62(3):447–453. [DOI] [PubMed] [Google Scholar]
- 43. Zhou B, Hong Z, Zeng J, et al. Comparison of the features between Alzheimer’s disease and vascular dementia. Chin J Clin Neurosci. 2002;10(1):13–15 (in Chinese). [Google Scholar]
- 44. Wang SY, Li YH, Chi GB, et al. Injury-related fatalities in China: an under-recognised public-health problem. Lancet. 2008;372(9651):1765–1773. [DOI] [PubMed] [Google Scholar]
- 45. He J, Gu D, Wu X, et al. Major causes of death among men and women in China. N Engl J Med. 2005;353(11):1124–1134. [DOI] [PubMed] [Google Scholar]
- 46. Wu X, Hu J, Zhuo L, et al. Epidemiology of traumatic brain injury in eastern China, 2004: a prospective large case study. J Trauma. 2008;64(5):1313–1319. [DOI] [PubMed] [Google Scholar]
- 47. Fleminger S, Oliver D L, Lovestone S, et al. Head injury as a risk factor for Alzheimer’s disease: the evidence 10 years on; a partial replication. J Neurol Neurosurg Psychiatry. 2003;74(7):857–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Zhou D, Wu C, Qi H, et al. : Prevalence of dementia in rural China: impact of age, gender and education. Acta Neurol Scand. 2006;114(4):273–280. [DOI] [PubMed] [Google Scholar]
- 49. Yamada T, Hattori H, Miura A, et al. Prevalence of Alzheimer’s disease, vascular dementia and dementia with Lewy bodies in a Japanese population. Psychiatry Clin Neurosci. 2001;55(1):21–25. [DOI] [PubMed] [Google Scholar]
- 50. Qiu C, De Ronchi D, Fratiglioni L: The epidemiology of the dementias: an update. Curr Opin Psychiatry. 2007;20(4):380–385. [DOI] [PubMed] [Google Scholar]
- 51. Ritchie K, Lovestone S. The dementias. Lancet. 2002;360(9347):1759–1766. [DOI] [PubMed] [Google Scholar]
- 52. Sousa RM, Ferri CP, Acosta D, et al. Contribution of chronic diseases to disability in elderly people in countries with low and middle incomes: a 10/66 Dementia Research Group population-based survey. Lancet. 2009;374(9704):1821–1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Karp A, Kareholt I, Qiu C, et al. Relation of education and occupation-based socioeconomic status to incident Alzheimer’s disease. Am J Epidemiol. 2004;159(2):175–183. [DOI] [PubMed] [Google Scholar]
- 54. De Ronchi D, Berardi D, Menchetti M, et al. Occurrence of cognitive impairment and dementia after the age of 60: a population-based study from Northern Italy. Dement Geriatr Cogn Disord. 2005;19(2-3):97–105. [DOI] [PubMed] [Google Scholar]