Abstract
Our previous studies showed that multitarget therapy is superior in efficacy to intravenous cyclophosphamide as an induction treatment for lupus nephritis in Asian populations. We conducted an open label, multicenter study for 18 months as an extension of the prior induction therapy trial in 19 renal centers in China to assess the efficacy and safety of multitarget maintenance therapy in patients who had responded at 24 weeks during the induction phase. Patients who had undergone multitarget induction therapy continued to receive multitarget therapy (tacrolimus, 2–3 mg/d; mycophenolate mofetil, 0.50–0.75 g/d; prednisone, 10 mg/d), and patients who had received intravenous cyclophosphamide induction treatment received azathioprine (2 mg/kg per day) plus prednisone (10 mg/d). We assessed the renal relapse rate during maintenance therapy as the primary outcome. We recruited 116 patients in the multitarget group and 90 patients in the azathioprine group. The multitarget and azathioprine groups had similar cumulative renal relapse rates (5.47% versus 7.62%, respectively; adjusted hazard ratio, 0.82; 95% confidence interval, 0.25 to 2.67; P=0.74), and serum creatinine levels and eGFR remained stable in both groups. The azathioprine group had more adverse events (44.4% versus 16.4% for multitarget therapy; P<0.01), and the multitarget group had a lower withdrawal rate due to adverse events (1.7% versus 8.9% for azathioprine; P=0.02). In conclusion, multitarget therapy as a maintenance treatment for lupus nephritis resulted in a low renal relapse rate and fewer adverse events, suggesting that multitarget therapy is an effective and safe maintenance treatment for patients with lupus nephritis.
Keywords: lupus nephritis, multitarget therapy, maintenance treatment, renal relapse, adverse event
The treatment of lupus nephritis (LN) usually involves two phases: an aggressive induction therapy and a longer period of maintenance treatment. Induction therapy aims to reverse the immune-mediated inflammatory processes and achieve disease remission with the administration of high doses of immunosuppressants over a short period of time.1,2 Maintenance treatment is intended to ensure a durable response and prevent recurrences using lower and presumably less toxic levels of immunosuppressive medications, keeping patients in remission.3 Clinicians are continuously searching for optimal immune-suppressive therapies for use as induction and maintenance treatment of LN.
As shown in our previous study, the induction treatment of LN with multitarget therapy (tacrolimus [FK506] and mycophenolate mofetil [MMF] combined with glucocorticoids) for 24 weeks achieved a complete remission (CR) rate of 45.9%, which was much higher than that with intravenous cyclophosphamide therapy (IVCY) in a multicenter, randomized, controlled trial.4 However, the efficacy of maintenance treatment with multitarget therapy in patients with LN remains unclear. We continued to treat patients in remission with a multitarget maintenance treatment for an additional 18 months to assess the efficacy of multitarget therapy for LN. This continuous design has been reported in a previous study of MMF2,5 and abatacept6 as treatments for LN and rituximab as a treatment for ANCA-associated vasculitis.7,8
The ideal maintenance treatment scheme for patients with LN requires not only a low relapse rate but also, fewer adverse effects, which are suitable for long-term application. Although our previous study showed no differences of adverse events between multitarget and IVCY groups in the induction phase,4 the adverse effects, particularly the nephrotoxicity of calcineurin inhibitors, are always the focus of attention during the long-term use of these regimens.9–11
On the basis of previous multitarget induction therapy, we continued to observe the efficacy and safety of multitarget therapy as a maintenance treatment in patients with LN who had responded at 24 weeks during the induction phase and compared them with those of azathioprine (AZA) treatment.
Results
Patient Characteristics
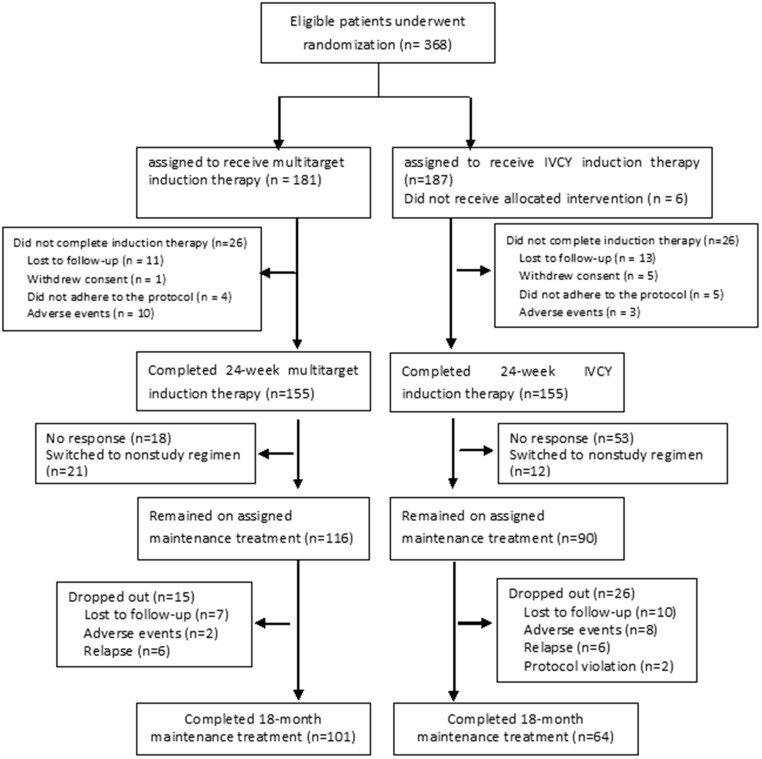
In total, 368 patients were randomized for induction therapy; 310 patients completed the induction therapy (155 in the multitarget group and 155 in the IVCY group).4 A total of 206 patients from 19 centers agreed to continue the maintenance treatment study between October of 2009 and December of 2011: 116 patients in the multitarget group and 90 patients in the AZA group. In the multitarget group, 101 patients completed the 18-month maintenance therapy, whereas 64 patients in the AZA group completed the study (Figure 1). The patients’ baseline disease and demographic characteristics at the initiation of the maintenance treatment are shown in Table 1.
Figure 1.
The study design and flow diagram.
Table 1.
Patient demographics and baseline characteristics
| Characteristic | Multitarget, n=116 | AZA, n=90 | Total, n=206 |
|---|---|---|---|
| Sex, women/men | 108/8 | 81/9 | 189/17 |
| Age, yr | 30.0 (24.0, 38.0) | 33.0 (26.0, 40.0) | 32.0 (24.0, 39.0) |
| Pathologic classification, n (%) | |||
| Class III | 5 (4.3) | 7 (7.8) | 12 (5.8) |
| Class IV | 50 (43.1) | 39 (43.3) | 89 (43.2) |
| Class V | 14 (12.1) | 12 (13.3) | 26 (12.6) |
| Class III+V | 15 (12.9) | 2 (2.2) | 17 (8.3) |
| Class IV+V | 32 (27.6) | 30 (33.3) | 62 (30.1) |
| Remission condition (%)a | |||
| CR | 69 (59.5) | 40 (44.4) | 109 (52.9) |
| PR | 47 (40.5) | 50 (55.6) | 97 (47.1) |
| SLEDAIa | 4.0 (2.0, 4.5) | 4.0 (2.0, 6.0) | 4.0 (2.0, 6.0) |
| Urinary protein, g/24 ha | 0.35 (0.16, 0.63) | 0.49 (0.17, 0.90) | 0.38 (0.17, 0.77) |
| Serum albumin, g/L | 43.4±4.1 | 42.4±4.2 | 42.9±4.1 |
| SCr, μmol/L | 61.9 (54.9, 74.4) | 61.0 (54.0, 74.3) | 61.4 (54.8, 74.3) |
| eGFR, ml/min per 1.73 m2, n (%) | |||
| ≥90 | 94 (81.0) | 72 (80.0) | 166 (80.6) |
| ≥60 to <90 | 18 (15.5) | 15 (16.7) | 33 (16.0) |
| ≥30 to <60 | 3 (2.6) | 3 (3.3) | 6 (2.9) |
| <30 | 1 (0.9) | 0 (0) | 1 (0.5) |
| Serum C3, mg/dl | 85.05 (74.20, 105.00) | 80.70 (69.60, 94.60) | 82.00 (72.20, 100.00) |
| Serum C4, mg/dl | 16.55 (12.20, 21.30) | 15.60 (12.00, 19.30) | 16.00 (12.10, 20.95) |
| Hemoglobin, g/L | 118.0 (110.5, 126.5) | 121.5 (112.0, 130.0) | 119.0 (111.0, 128.0) |
| Anti-dsDNA positive rate, n (%) | 29/115 (25.2) | 24/83 (28.9) | 53/198 (26.8) |
| Renal tubular function | |||
| NAG, U/g creatinine | 5.53 (3.50, 9.80) | 4.80 (4.19, 5.81) | 5.30 (3.50, 9.60) |
| RBP, mg/L | 0.35 (0.20, 0.50) | 0.53 (0.42, 0.80) | 0.40 (0.20, 0.72) |
Data are expressed as numbers (%), medians (25th, 75th percentiles), or means (SD). Reference ranges were as follows: urinary protein, ≤0.4 g/24 h; serum albumin, 35–55 g/L; SCr, men: 45–110 μmol/L (0.51–1.24 mg/dl) and women: 45–93 μmol/L (0.51–1.05 mg/dl); eGFR, 90–120 ml/min per 1.73 m2; hemoglobin, 130–175 g/L (men) and 115–150 g/L (women); serum C3, 80–180 mg/dl; serum C4, 10–40 mg/dl; NAG, ≤16.5 U/g creatinine; RBP, ≤0.5 mg/L. Anti-dsDNA, antidouble-stranded DNA.
P<0.05.
Reasons for Premature Withdrawal from Maintenance Treatment
Forty-one patients (15 in the multitarget group and 26 in the AZA group) did not complete the 18-month maintenance treatment (Supplemental Table 1). Three patients (2.6%) in the multitarget group reached renal end point events, and comparable results (3.3%) were observed in the AZA group (P>0.99). The main reasons for early withdrawal were a loss to follow-up, relapse, and adverse events. Twelve patients withdrew because of relapse (renal relapse, n=11; extrarenal relapse, n=1), and one patient experienced renal relapse in the 18th month. The dropout rate in the multitarget group was less than that in the AZA group (7.8% versus 22.2%; P<0.01).
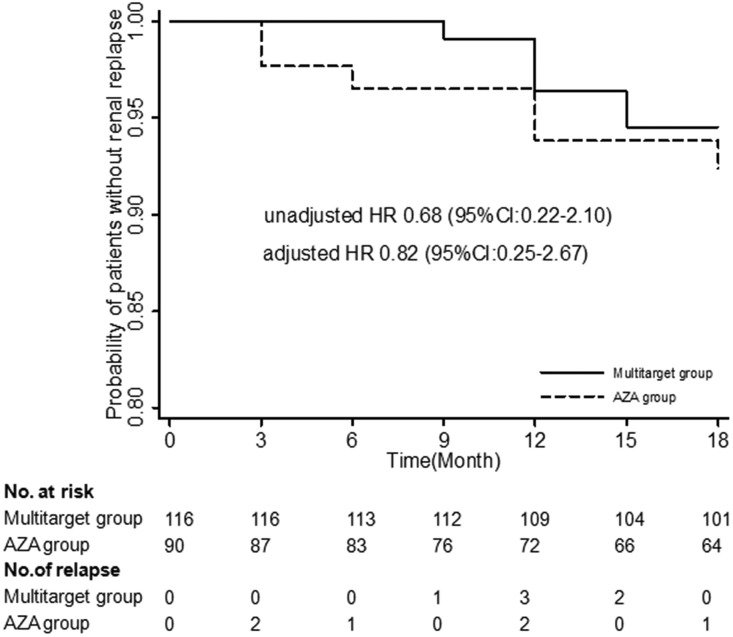
Renal Relapse Rate in the 18-Month Maintenance Treatment
Each group had six patients who experienced renal relapse, including five patients who had CR (three in the multitarget group and two in the AZA group) and seven patients who had partial remission (PR; three in the multitarget group and four in the AZA group) at beginning of the maintenance therapy. No significant differences in the cumulative renal relapse rate were observed (5.47%; 95% confidence interval [95% CI], 2.50% to 11.78% versus 7.62%; 95% CI, 3.48% to 16.26%; P=0.49; unadjusted hazard ratio [HR], 0.68; 95% CI, 0.22 to 2.10; P=0.50; adjusted HR, 0.82; 95% CI, 0.25 to 2.67; P=0.74) (Figure 2). The median time of renal relapse was 12 months (interquartile range [IQR], 12–15 months) and 9 months (IQR, 3–12 months) in the multitarget and AZA groups, respectively (P=0.24). One patient in the AZA group had experienced extrarenal relapse at the 15th month compared with no patients in the multitarget group.
Figure 2.
Probability of patients without renal relapse during the maintenance treatment.
Subgroup Analyses of Renal Relapse According to the Baseline Renal Response
A between-group difference in the CR or PR rate at baseline was observed (Table 1). Therefore, a subgroup analysis of renal relapse according to the baseline renal response was performed. The renal relapse rate did not show a statistically significance difference between patients with CR in the multitarget and AZA groups or between patients with PR in the two groups (Supplemental Table 2).
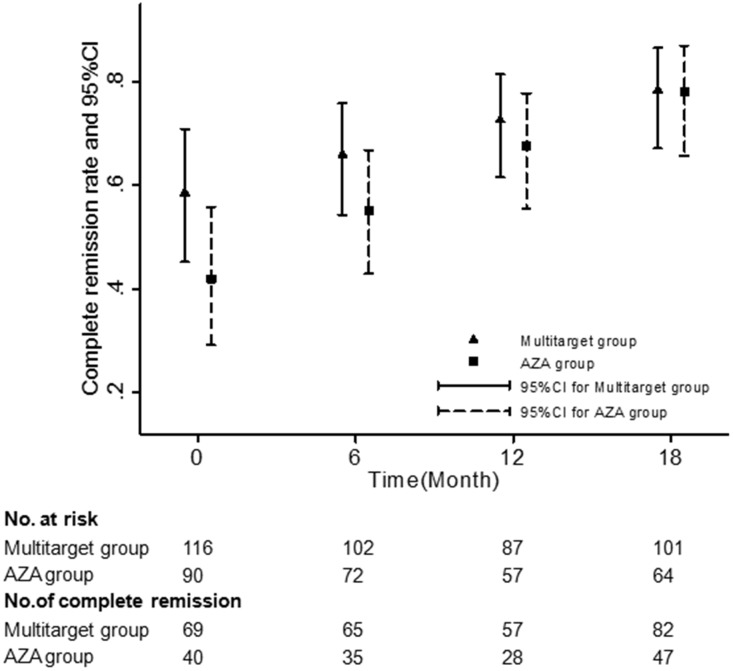
Patients in Each Group Maintained Their CR Status during Maintenance Treatment
A total of 65.9% of patients in the multitarget group achieved CR by 6 months, similar to the percentage in the AZA group (55.1%; difference, 10.8%; 95% CI, −5.5% to 27.1%; P=0.19). The percentages of patients in the multitarget group who maintained their CR status at 12 and 18 months were 72.5% and 78.3%, respectively, and the corresponding percentages in the AZA group were 67.6% and 78.0%, respectively. However, the differences were not significant between the two groups at 12 and 18 months (difference, 4.9%; 95% CI, −10.1% to 20.0%; P=0.52 and difference, 0.3%; 95% CI, −14.1% to 14.7%; P=0.97, respectively) (Figure 3).
Figure 3.
Patients in each group maintained their CR status during the maintenance treatment. The CR rates were calculated using the generalized linear mixed model.
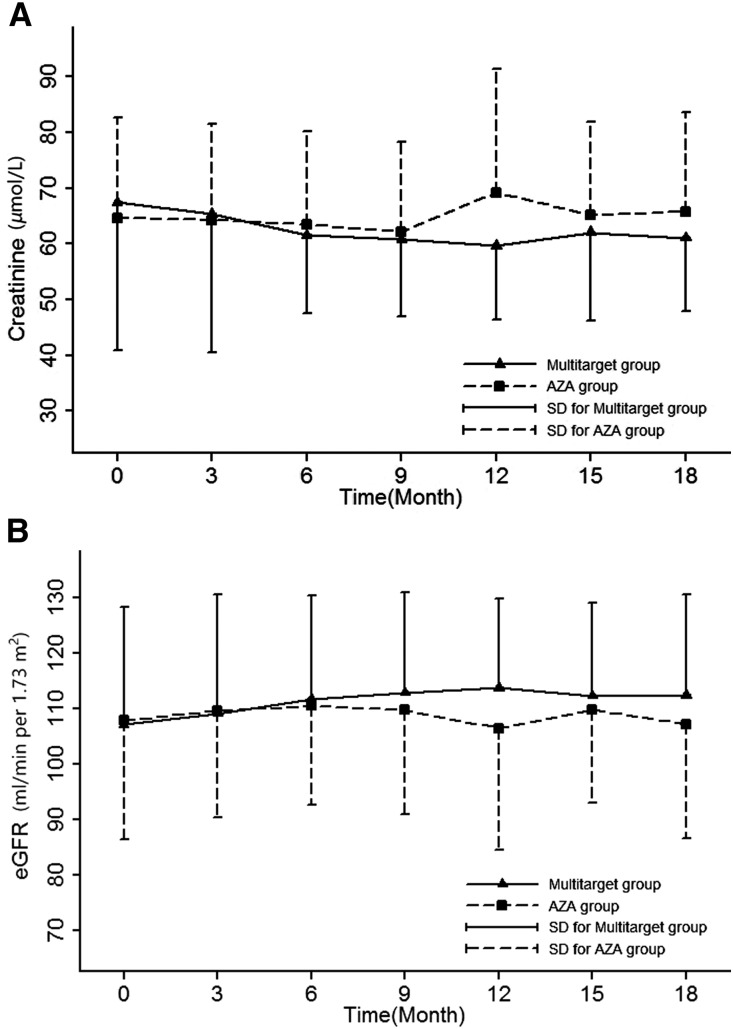
Changes in Clinical Parameters during Maintenance Treatment
The serum creatinine (SCr) level and eGFR of the multitarget and AZA groups remained stable during the maintenance treatment (Figure 4). There were no significant differences in the SCr levels (P=0.76) or eGFR (P=0.75) between the two groups.
Figure 4.
The changes in SCr levels and eGFR during the maintenance treatment. (A) SCr; (B) eGFR.
No significant differences in the proteinuria, serum albumin, and complement levels were observed between the two groups during the maintenance treatment (Supplemental Figure 1, A–D). Although a significant difference was noticed in the SLE disease activity index (SLEDAI), it was consistent with the baseline value in the AZA group compared with in the multitarget group at the beginning of the maintenance treatment (Supplemental Figure 1E).
The blood trough concentration of FK506 was measured in some patients. During the first 6 months of the maintenance treatment, their trough concentrations of FK506 were within the therapeutic window of 4–8 ng/ml. The trough concentrations of FK506 were 3.37±1.08, 3.23±1.37, and 3.55±1.20 ng/ml at 12, 15, and 18 months, respectively (Supplemental Table 3). The post hoc analysis did not reveal significant differences in the urine levels of N-acetyl-β-d-glucosaminidase (NAG) or retinol binding protein (RBP) after the multitarget therapy treatment (Supplemental Table 4).
Safety and Tolerability
There was a 16.4% (19 of 116) adverse event rate in the multitarget group, whereas it was 44.4% (40 of 90) in the AZA group (Table 2). The incidences of liver dysfunction and leukopenia in the multitarget and AZA groups were 0.9% versus 6.7%, respectively, and 7.8% versus 25.6%, respectively. Only one patient with leukopenia experienced an infection (herpes zoster); the other 22 patients with leukopenia underwent a transient withdrawal or alteration in the AZA dose. Two patients (1.7%) in the multitarget group and eight patients (8.9%) in the AZA group dropped out due to adverse events (P=0.02) (Supplemental Tables 1 and 5).
Table 2.
Adverse events during the maintenance treatments
| Adverse events | Multitarget, n=116 | AZA, n=90 | ||||
|---|---|---|---|---|---|---|
| Event No. | Crude Rate, % | Rate per 100 patient-yr | Event No. | Crude Rate, % | Rate per 100 patient-yr | |
| AEs (includes SAEs)a | 19 | 16.4 | 11.59 | 40 | 44.44 | 35.57 |
| Infection | 12 | 10.3 | 7.32 | 9 | 10.0 | 8 |
| Herpes zoster | 2 | 1.7 | 1.22 | 2 | 2.2 | 1.78 |
| Pneumonia | 2 | 1.7 | 1.22 | 0 | 0 | 0 |
| Upper respiratory tract infection | 7 | 6.0 | 4.27 | 6 | 6.7 | 5.34 |
| Herpes simplex | 1 | 0.9 | 0.61 | 0 | 0 | 0 |
| Urinary tract infection | 0 | 0 | 0 | 1 | 1.1 | 0.89 |
| Liver dysfunctionb | 1 | 0.9 | 0.61 | 6 | 6.7 | 5.34 |
| Leukopeniaa | 9 | 7.8 | 5.49 | 23c | 25.6 | 20.45 |
| Osteonecrosis | 1 | 0.9 | 0.61 | 1 | 1.1 | 0.89 |
| Upper gastrointestinal symptoms | 1 | 0.9 | 0.61 | 5 | 5.6 | 4.45 |
| Menstrual disorder | 0 | 0 | 0 | 2 | 2.2 | 1.78 |
| SAEs | 2 | 1.7 | 1.22 | 3 | 3.3 | 2.67 |
| Pneumonia | 2 | 1.7 | 1.22 | 0 | 0 | 0 |
| Liver dysfunction | 0 | 0 | 0 | 1 | 1.1 | 0.89 |
| Leukopenia | 0 | 0 | 0 | 2 | 2.2 | 1.78 |
Leukopenia was defined as a peripheral white blood cell count <4000 cells per 1 μl. The definition of liver dysfunction was a serum alanine aminotransferase and/or aspartate transaminase level >50 U/L. The crude rates were compared using the Fisher exact method. AE, adverse event; SAE, serious adverse event.
P<0.01.
P<0.05.
Only one patient with leukopenia experienced an infection (herpes zoster); the other 22 patients with leukopenia underwent transient withdrawal or an alteration in the AZA dose.
Two patients (1.7%) in the multitarget group and three patients (3.3%) in the AZA group experienced serious adverse events. None of the patients in either treatment group died.
Discussion
Renal involvement continues to be a major contributor to the morbidity and mortality of patients with SLE. Disease relapse is a major problem for patients with LN who achieve remission after induction treatment, and it affects the long-term outcomes of patients with LN.12,13 Maintenance treatment is required after induction therapy to prevent disease relapse in patients who achieve remission.3 As shown in our previous studies, the induction treatment of LN with multitarget therapy for 24 weeks achieved a higher CR rate than IVCY therapy.4 In this study, we observed the efficacy and safety of multitarget therapy as a continuing maintenance treatment for patients with LN who had responded to induction therapy.
This study showed that the relapse rate of patients with LN treated with multitarget therapy was 5.47%, but the difference was not significant compared with that of the AZA treatment (7.62%). According to previous literatures, the relapse rate was 12.9%–19% for patients with lupus who received maintenance treatment with MMF (2.0 g/d) for 3 years, and the relapse rate of patients who underwent the AZA treatment (2 mg/kg per day) was 23.4%–25%.3,14 The relapse rate of multitarget maintenance therapy in our study was less than the rates reported in previous studies. Two reasons may contribute to the lower relapse rate observed in this trial. In this study, 59.5% of patients in the multitarget group achieved CR before the maintenance study, whereas in the Aspreva Lupus Management Study (ALMS), the rate of CR at the end of induction therapy was <10%.3 Compared with subjects who achieved CR, patients who obtained PR are more likely to experience a relapse and disease progression.15 The higher CR rate might explain why our studies showed lower relapse rates during the maintenance treatment. Thus, the superior efficacy of multitarget therapy in the induction treatment phase provides clinician an opportunity to prevent relapse and stabilize renal function during the maintenance treatment phase. Another reason for the lower relapse rate may be related to the relatively shorter time of maintenance treatment used in this study. Our observation lasted only 18 months. The relapse rate of patients with LN treated with AZA was also less than the relapse rate reported in the literature.3,14 It may also be related to the higher baseline CR rate. In this study, 44.4% of patients in the AZA group achieved CR before entering the maintenance study. The possible explanation for the relatively high incidence of remission using IVCY during induction treatment has been discussed in a previous report.4 The relapse rate would be increased with the prolonged treatment and observation period.
The long-term prognosis of patients with LN is determined by whether remission is achieved. As shown in the study by Chen et al.,16 the 10-year renal survival rate in patients who achieved CR was 94%, whereas it was 45% in patients with PR.16 With the extension of the treatment time, the number of patients who achieved CR was increased in our study. Some patients with PR achieved CR. According to the ALMS, 62.1% of patients in the MMF group (72 of 116) and 59.5% in the AZA group (66 of 111) achieved CR during maintenance therapy.3 Notably, the CR rates were 59.5% in the multitarget group and 44.4% in the AZA group at baseline; however, the CR rates increased to 78.3% and 78.0%, respectively, in these groups at 18 months. This catchup phenomenon was observed in the AZA arm, and it strengthens the value of using AZA as a maintenance therapy. On the basis of these finding, an effective maintenance treatment not only controls disease relapse but also, continually increases the CR rate during maintenance treatment, which might improve the long-term outcomes of the patients.
The clinical outcomes of patients with LN are affected directly by target organ damage and indirectly by therapy complications. The side effects of drugs must be considered during the long-term use of immunosuppressive agents. Multitarget therapy, which uses a combination of different drugs, aims to improve the efficacy and reduce the dose and side effects.4 The incidence rates of overall adverse events were 16.4% in the multitarget group and 44.4% in the AZA group. In particular, the incidences of liver dysfunction and leucopenia were higher in the AZA group than those in the multitarget group. Therefore, only 1.7% of patients in the multitarget group withdrew from the study due to adverse events, whereas 8.9% of patients in the AZA group withdrew from the study due to adverse events. Consistent with our results, the ALMS reported a lower withdrawal rate of patients treated with MMF due to adverse events of MMF than patients treated with AZA (25.2% versus 39.6%, respectively).3 In addition, the incidence of adverse events of the multitarget maintenance treatment was also lower than that reported for MMF (25.2%) and FK506 (32.4%) monotherapies as maintenance treatment.3,17
The long-term use of calcineurin inhibitors in patients with kidney transplants causes renal toxicity, including tubular atrophy, interstitial fibrosis, and hyaline degeneration of small arteries.9,18,19 According to the results of clinical trials in patients with LN, the use of cyclosporin as a maintenance treatment for LN did not induce obvious renal toxicity.20 Using the same regimen as in this study, the Symphony Study of kidney transplantation revealed that the use of low-dose FK506, MMF, and prednisone for 3 years, with a trough FK506 concentration of 3–7 ng/ml, had no effect on the patients’ eGFRs.21,22 In this study, during the 18-month maintenance treatment, the SCr levels and eGFR remained stable in the multitarget and AZA groups, with no significant difference between the two groups. Additionally, the urine NAG level and RBP excretion are used as surrogate markers to reflect renal tubular injury, and the changes in these markers were observed during treatment. Neither the urinary NAG levels nor RBP excretion increased in the two groups after treatment. On the basis of these results, multitarget therapy is a safe regimen for the maintenance treatment of LN.
Certain limitations exist in this study. Patients who did not respond to the induction therapy were not recruited; thus, some data were missing, which was a flaw in the design of this study. This study was conducted only in a Chinese population. A randomized, controlled trial is needed to further evaluate the efficacy and safety of multitarget therapy as a maintenance treatment for patients with LN.
In conclusion, the use of multitarget therapy as a maintenance treatment for LN resulted in a low renal relapse rate and fewer adverse events, suggesting that multitarget therapy is an effective and safe maintenance treatment for patients with LN.
Concise Methods
Study Design
This study was a continuation of the induction-phase study, the results of which have been reported.4 We continued multitarget therapy as a maintenance treatment and did not rerandomize the patients before the maintenance treatment. This study was a prospective, open label, multicenter study that compared the efficacy and safety of multitarget therapy with AZA treatment in patients who had responded to induction therapy. The study protocol was registered at ClinicalTrials.gov (NCT01056237); the full trial protocol and major changes are summarized in Supplemental Material.
Study Participants
Patients with LN ages 18–65 years old who had responded (experienced CR or PR) to multitarget therapy or IVCY during the 24-week induction treatment were recruited. The key exclusion criteria included patients who did not achieve CR or PR at the end of the 24-week induction phase, patients with liver dysfunction or a white blood cell count <3000/mm3, and patients suffering from chronic infections (Supplemental Figures 2 and 3). Details on the patient inclusion, exclusion, and withdrawal criteria are available in Supplemental Material.
The study was conducted in 19 renal centers across China. The local ethics committees approved the study, and all participants provided written informed consent. The study adhered to the principles of the Declaration of Helsinki and the principles outlined in the Guidelines for Good Clinical Practice International Conference on Harmonization Tripartite Guideline (January of 1997).
Immunosuppressive Treatment and Study Schedule
Eligible patients who underwent the multitarget therapy during the induction phase continued to receive the multitarget therapy, and patients who received the IVCY induction treatment were switched to AZA as a maintenance treatment. The patients in the multitarget group continued to receive MMF (0.75 g/d for 6 months and then tapered to 0.5 g/d for another 12 months) and FK506 (3 mg/d for 6 months and then tapered to 2 mg/d for another 12 months), whereas patients in the AZA group were orally administered AZA (2 mg/kg body wt per day for 18 months). Oral prednisone was administered to both groups at a dose of 10 mg/d.23 Angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers were continued if they were administered during the induction phase, and calcium channel blockers, diuretics, and β- or α-receptor blockers were permitted for new-onset hypertension. Patients were prohibited from taking methotrexate, leflunomide, antimalarials, nonsteroidal anti-inflammatory drugs/cyclooxygenase-2 inhibitors, and other immunosuppressants during the maintenance treatment phase. Any drugs that affected the blood concentrations of FK506 (e.g., macrolides antibiotics, estradiol, rifampicin, phenobarbital, carbamazepine, and fluconazole) were avoided.
Subjects’ visits were scheduled at 0, 1, 3, 6, 9, 12, 15, and 18 months during the study. Efficacy evaluations and safety assessments (histories, physical examinations, laboratory tests, concomitant medications, and adverse events) were performed at each visit.
Outcomes and Efficacy Assessments
The primary end point was the cumulative rate of renal relapse at 18 months as determined by the Clinical Endpoints Committee.
The secondary end points included the rate of extrarenal relapse; the time to relapse; the rate of renal end point events (including ESRD, sustained doubling of the SCr level greater than the normal level, or a 30% reduction in the eGFR compared with the baseline value); the CR status at 6, 12, and 18 months during the maintenance treatment phase; changes in proteinuria, albumin, SCr, eGFR, immunologic indices (antibodies, C3, and C4), and SLEDAI scores from baseline to month 18; and the reasons why patients withdrew or discontinued therapy.
CR was defined as a 24-hour urinary protein excretion ≤0.4 g, the absence of active urine sediments, a serum albumin level ≥35 g/L, and a normal SCr level. PR was defined as a ≥50% reduction in proteinuria, a urine protein level <3.5 g/24 h, a serum albumin level ≥30 g/L, and normal or ≤25% increase in the SCr level from baseline.4
Relapse included renal relapse and extrarenal relapse. Renal relapse was defined by the presence of any one of the following: (1) a relapse of proteinuria defined as persistent proteinuria ≥1.0 g/24 h after CR or an increase of ≥2.0 g/24 h after PR with or without hematuria and (2) an increase in SCr levels defined as a ≥50% increase in the SCr level compared with the normal level at baseline or a 30% increase in SCr level compared with an abnormal level at baseline with increased hematuria (defined as doubling of red blood cell count in urinary sediment, ten or more cells per high power field, or the appearance of red cellular casts and white cellular casts, with the exception of a urinary tract infection). Extrarenal relapse was defined as the new appearance of skin erythema, vasculitis, joint pain, blood system diseases (platelets <50,000/mm3 or hemolytic anemia), neurologic symptoms, lupus myocarditis, lupus pneumonia, serous cavity inflammation, or abnormal results on laboratory tests (antibodies, C3, and C4) associated with SLEDAI scores greater than or equal to four. These indices were reassessed 2 weeks later.
Statistical Analyses
This study was a continuation of our previous study of the use of multitarget therapy as an induction treatment.4 Continuous data were presented as the means±SDs and analyzed using the t test if they were normally distributed; for data with a non-normal distribution, medians (IQRs) were presented, and the Wilcoxon rank sum test was used for the analysis. Categorical data were presented as ratios or proportions and analyzed using the Fisher exact method. Time to event data were analyzed using Kaplan–Meier curves, and between-group differences were compared using the log rank test. The frailty model was used to estimate the HRs and 95% CIs, which included the center as a random effect; treatment was the only factor used to obtain the unadjusted HR, and the treatment, the condition of remission, 24-hour urinary protein levels, and SLEDAI were used to obtain adjusted HRs. Data that were measured repeatedly were analyzed using the longitudinal data analysis method. For clinical parameters, the differences between the groups were obtained using the mixed model that included the baseline value, treatment, visit, and the interaction between treatment and visit. The CR rates at 6, 12, and 18 months were obtained using by the generalized linear mixed model that included the condition of remission, treatment, visit, and the interaction between treatment and visit. The statistical analyses were performed using SAS software, version 9.3 (SAS Institute, Cary, NC). Differences were determined to be statistically significant when the two-sided P value was <0.05.
Disclosures
None.
Supplementary Material
Acknowledgments
This work was supported by National Key Technology Research and Development Program grants 2013BAI09B04 and 2015BAI12B05.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Calcineurin Inhibitors in the Treatment of Lupus Nephritis: A Hare Versus Turtle Story?,” on pages 3435–3437.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2017030263/-/DCSupplemental.
References
- 1.Appel GB, Contreras G, Dooley MA, Ginzler EM, Isenberg D, Jayne D, Li LS, Mysler E, Sánchez-Guerrero J, Solomons N, Wofsy D; Aspreva Lupus Management Study Group : Mycophenolate mofetil versus cyclophosphamide for induction treatment of lupus nephritis. J Am Soc Nephrol 20: 1103–1112, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chan TM, Li FK, Tang CS, Wong RW, Fang GX, Ji YL, Lau CS, Wong AK, Tong MK, Chan KW, Lai KN; Hong Kong-Guangzhou Nephrology Study Group : Efficacy of mycophenolate mofetil in patients with diffuse proliferative lupus nephritis. N Engl J Med 343: 1156–1162, 2000 [DOI] [PubMed] [Google Scholar]
- 3.Dooley MA, Jayne D, Ginzler EM, Isenberg D, Olsen NJ, Wofsy D, Eitner F, Appel GB, Contreras G, Lisk L, Solomons N; ALMS Group : Mycophenolate versus azathioprine as maintenance therapy for lupus nephritis. N Engl J Med 365: 1886–1895, 2011 [DOI] [PubMed] [Google Scholar]
- 4.Liu Z, Zhang H, Liu Z, Xing C, Fu P, Ni Z, Chen J, Lin H, Liu F, He Y, He Y, Miao L, Chen N, Li Y, Gu Y, Shi W, Hu W, Liu Z, Bao H, Zeng C, Zhou M: Multitarget therapy for induction treatment of lupus nephritis: A randomized trial. Ann Intern Med 162: 18–26, 2015 [DOI] [PubMed] [Google Scholar]
- 5.Chan TM, Tse KC, Tang CS, Mok MY, Li FK; Hong Kong Nephrology Study Group : Long-term study of mycophenolate mofetil as continuous induction and maintenance treatment for diffuse proliferative lupus nephritis. J Am Soc Nephrol 16: 1076–1084, 2005 [DOI] [PubMed] [Google Scholar]
- 6.ACCESS Trial Group : Treatment of lupus nephritis with abatacept: The Abatacept and Cyclophosphamide Combination Efficacy and Safety Study. Arthritis Rheumatol 66: 3096–3104, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stone JH, Merkel PA, Spiera R, Seo P, Langford CA, Hoffman GS, Kallenberg CG, St Clair EW, Turkiewicz A, Tchao NK, Webber L, Ding L, Sejismundo LP, Mieras K, Weitzenkamp D, Ikle D, Seyfert-Margolis V, Mueller M, Brunetta P, Allen NB, Fervenza FC, Geetha D, Keogh KA, Kissin EY, Monach PA, Peikert T, Stegeman C, Ytterberg SR, Specks U; RAVE-ITN Research Group : Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med 363: 221–232, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Specks U, Merkel PA, Seo P, Spiera R, Langford CA, Hoffman GS, Kallenberg CG, St Clair EW, Fessler BJ, Ding L, Viviano L, Tchao NK, Phippard DJ, Asare AL, Lim N, Ikle D, Jepson B, Brunetta P, Allen NB, Fervenza FC, Geetha D, Keogh K, Kissin EY, Monach PA, Peikert T, Stegeman C, Ytterberg SR, Mueller M, Sejismundo LP, Mieras K, Stone JH; RAVE-ITN Research Group : Efficacy of remission-induction regimens for ANCA-associated vasculitis. N Engl J Med 369: 417–427, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Naesens M, Kuypers DR, Sarwal M: Calcineurin inhibitor nephrotoxicity. Clin J Am Soc Nephrol 4: 481–508, 2009 [DOI] [PubMed] [Google Scholar]
- 10.Bock ME, Cohn RA, Ali FN: Treatment of childhood nephrotic syndrome with long-term, low-dose tacrolimus. Clin Nephrol 79: 432–438, 2013 [DOI] [PubMed] [Google Scholar]
- 11.Yuan H, Liu N, Sun GD, Jia Y, Luo P, Miao LN: Effect of prolonged tacrolimus treatment in idiopathic membranous nephropathy with nephrotic syndrome. Pharmacology 91: 259–266, 2013 [DOI] [PubMed] [Google Scholar]
- 12.El Hachmi M, Jadoul M, Lefèbvre C, Depresseux G, Houssiau FA: Relapses of lupus nephritis: Incidence, risk factors, serology and impact on outcome. Lupus 12: 692–696, 2003 [DOI] [PubMed] [Google Scholar]
- 13.Gibson KL, Gipson DS, Massengill SA, Dooley MA, Primack WA, Ferris MA, Hogan SL: Predictors of relapse and end stage kidney disease in proliferative lupus nephritis: Focus on children, adolescents, and young adults. Clin J Am Soc Nephrol 4: 1962–1967, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Houssiau FA, D’Cruz D, Sangle S, Remy P, Vasconcelos C, Petrovic R, Fiehn C, de Ramon Garrido E, Gilboe IM, Tektonidou M, Blockmans D, Ravelingien I, le Guern V, Depresseux G, Guillevin L, Cervera R; MAINTAIN Nephritis Trial Group : Azathioprine versus mycophenolate mofetil for long-term immunosuppression in lupus nephritis: Results from the MAINTAIN nephritis trial. Ann Rheum Dis 69: 2083–2089, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Illei GG, Takada K, Parkin D, Austin HA, Crane M, Yarboro CH, Vaughan EM, Kuroiwa T, Danning CL, Pando J, Steinberg AD, Gourley MF, Klippel JH, Balow JE, Boumpas DT: Renal flares are common in patients with severe proliferative lupus nephritis treated with pulse immunosuppressive therapy: Long-term followup of a cohort of 145 patients participating in randomized controlled studies. Arthritis Rheum 46: 995–1002, 2002 [DOI] [PubMed] [Google Scholar]
- 16.Chen YE, Korbet SM, Katz RS, Schwartz MM, Lewis EJ; Collaborative Study Group : Value of a complete or partial remission in severe lupus nephritis. Clin J Am Soc Nephrol 3: 46–53, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen W, Liu Q, Chen W, Tang X, Fu P, Liu F, Liao Y, Yang Z, Zhang J, Chen J, Lou T, Fu J, Kong Y, Liu Z, Li Z, Yu X: Outcomes of maintenance therapy with tacrolimus versus azathioprine for active lupus nephritis: A multicenter randomized clinical trial. Lupus 21: 944–952, 2012 [DOI] [PubMed] [Google Scholar]
- 18.Ferguson RM, Rynasiewicz JJ, Sutherland DE, Simmons RL, Najarian JS: Cyclosporin A in renal transplantation: A prospective randomized trial. Surgery 92: 175–182, 1982 [PubMed] [Google Scholar]
- 19.Vincenti F, Laskow DA, Neylan JF, Mendez R, Matas AJ: One-year follow-up of an open-label trial of FK506 for primary kidney transplantation. A report of the U.S. multicenter FK506 kidney transplant group. Transplantation 61: 1576–1581, 1996 [DOI] [PubMed] [Google Scholar]
- 20.Moroni G, Doria A, Mosca M, Alberighi OD, Ferraccioli G, Todesco S, Manno C, Altieri P, Ferrara R, Greco S, Ponticelli C: A randomized pilot trial comparing cyclosporine and azathioprine for maintenance therapy in diffuse lupus nephritis over four years. Clin J Am Soc Nephrol 1: 925–932, 2006 [DOI] [PubMed] [Google Scholar]
- 21.Ekberg H, Tedesco-Silva H, Demirbas A, Vítko S, Nashan B, Gürkan A, Margreiter R, Hugo C, Grinyó JM, Frei U, Vanrenterghem Y, Daloze P, Halloran PF; ELITE-Symphony Study : Reduced exposure to calcineurin inhibitors in renal transplantation. N Engl J Med 357: 2562–2575, 2007 [DOI] [PubMed] [Google Scholar]
- 22.Ekberg H, Bernasconi C, Tedesco-Silva H, Vítko S, Hugo C, Demirbas A, Acevedo RR, Grinyó J, Frei U, Vanrenterghem Y, Daloze P, Halloran P: Calcineurin inhibitor minimization in the Symphony study: Observational results 3 years after transplantation. Am J Transplant 9: 1876–1885, 2009 [DOI] [PubMed] [Google Scholar]
- 23.Sinclair A, Appel G, Dooley MA, Ginzler E, Isenberg D, Jayne D, Wofsy D, Solomons N: Mycophenolate mofetil as induction and maintenance therapy for lupus nephritis: Rationale and protocol for the randomized, controlled Aspreva Lupus Management Study (ALMS). Lupus 16: 972–980, 2007 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.