Pain is one of the most commonly reported symptoms in patients with ESRD, and it is experienced by approximately 50% of patients with ESRD.1–3 Yet, how to best treat pain in patients with ESRD is not clear.1–3A few earlier studies reported undertreatment of pain in these patients.2,4 By contrast, a recent study reported that, in 2015, 91.8 million (37.8%) United States civilian, noninstitutionalized adults used prescription opioids in the past 12 months, of whom 11.5 million misused the medications.5 Moreover, use and misuse of prescription opioids for pain management may lead to complications and serious adverse outcomes. Currently, the United States is experiencing an opioid crisis, with more than a quadrupling of prescription opioid overdose deaths between 1999 and 2015.6,7 Thus, it is important to understand the prevalence of prescription opioid use and misuse among patients with ESRD and examine how prescription opioid use and misuse are related to adverse outcomes in this population.
Addressing this topic in this issue of the Journal of the American Society of Nephrology, Kimmel et al.8 examined the prevalence of opioid medication prescription among patients on maintenance dialysis with Medicare Part A, B, and D coverage and their associations with subsequent all-cause death, dialysis discontinuation, and hospitalization using the 2006–2010 US Renal Data System data. The authors found that almost two thirds of examined patients received at least one opioid prescription each year and that over one fifth received chronic opioid prescriptions annually. Moreover, their study showed that opioid prescriptions were associated with increased risk of death, dialysis discontinuation, and hospitalization in patients on dialysis.8 Importantly, the authors reported dose-response relationships between the dose magnitude of prescribed opioids in morphine milligram equivalent (MME) and then, examined adverse outcomes. Kimmel et al.8 also found that over one quarter of patients on dialysis with prescription opioids received doses exceeding 50 MME per day.
A recent guideline developed by the Centers for Disease Control and Prevention (CDC) for practitioners prescribing opioids for chronic pain recommends that clinicians carefully reassess evidence of individual benefits and risks when increasing dosage to 50 MME or more per day.9 Another study highlighted that patients with ESRD and opioid dose exceeding 50 MME per day are at increased risk for opioid-induced sedation and respiratory depression, which can lead to death.3
The results found by Kimmel et al.8 are consistent with the recent high prevalence of prescription opioid use among the United States adult population5 and high prescription opioids–related deaths.7 Importantly, these timely results suggest the need for appropriate pain management specifically for patients with ESRD. The CDC guideline includes 12 recommendations for use of opioids in chronic pain.9 For example, the CDC guideline recommends that practitioners need to decide whether pharmacologic therapy is necessary. Pharmacologic therapy should be used after discussing known risks and realistic benefits with patients. Selection of medication should target the type and cause of pain. Also, the lowest effective dosage and duration of opioid treatment are recommended.
However, the CDC guideline does not provide specific medication guidance.9 As documented in the review that served as the platform for the CDC guideline, evidence for the effectiveness of opioids in the treatment of chronic pain is lacking.10 Moreover, the CDC guideline is not intended for patients who are in active cancer treatment, palliative care, or end of life care.9 According to the World Health Organization (WHO), palliative care is “an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.”11 Palliative care principles have been recommended for application to the diagnosis of ESRD,12,13 but there are no formal standards to inform renal palliative care.
In particular, there is a need for appropriate pain management specifically for patients with ESRD.12–14 Although evidence is limited regarding the pharmacology of many medications in this population, a few recent studies provided guides to pain management for patients with ESRD using modified WHO three-step analgesic ladder approaches.2,3,12–14 The WHO three-step analgesic ladder originally was created to guide the treatment of cancer pain,15 and it was validated in a small study showing the short-term (4-week) efficacy of pain relief in patients on hemodialysis in West Virginia.4 Thus, further large-scale, randomized, controlled trials may be useful to assess the short- and long-term efficacy and the safety of these approaches as well as the development of tolerance and adverse effects in both patients on hemodialysis and patients on peritoneal dialysis. Furthermore, special efforts are needed for elderly patients with ESRD, because the study by Barakzoy and Moss4 showed that the WHO analgesic ladder did not lead to effective pain treatment in elderly patients on hemodialysis and because elderly patients on dialysis are an important part of all patients with ESRD.
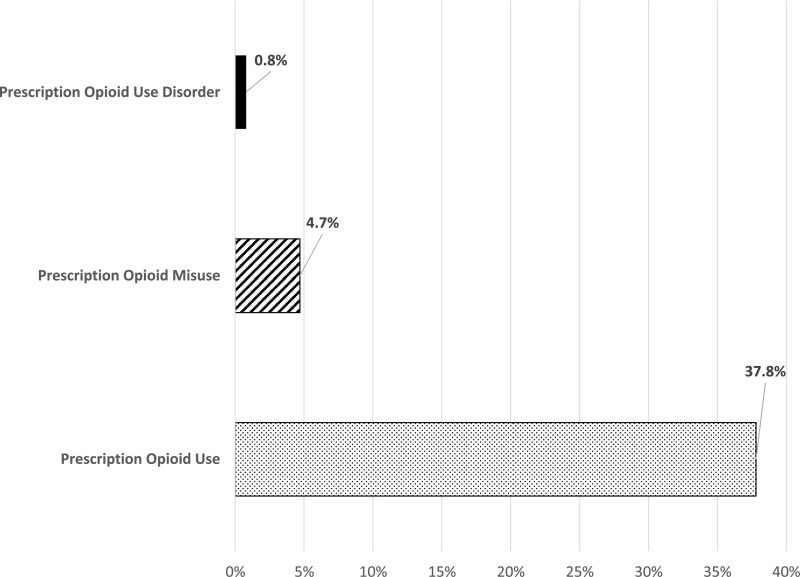
A recent study reported that, among United States civilian, noninstitutionalized adults who used prescription opioids in 2015, 12.5% reported misuse, and of those reporting misuse, 16.7% reported a prescription opioid use disorder (Figure 1).5 It is important to assess the prevalence of prescription opioid misuse and use disorders among patients with ESRD, because they are currently common among the general adult population. However, the study by Kimmel et al.8 was limited to filled prescriptions only. Further studies are needed to understand the actual use, use frequency, and dosage of prescription opioids, the prevalence of prescription opioid misuse and use disorders, and their relationships with adverse outcomes among patients with ESRD.
Figure 1.
In 2015, every one in three US adult used prescription opioids, 4.7% misused opioids, and 0.8% had a prescription opioid use disorder. Overall, prescription opioid misuse and use disorders were common among adult prescription opioid users.
Clinicians should screen for prescription opioid misuse among patients with ESRD before initiating long-term opioid therapy and during the opioid treatment course. After a prescription opioid misuse or use disorder is identified, referral to a pain management specialist may be warranted. Although its predictive power is relative low, the Opioid Risk Tool (Table 1) may be used to identify patients who may be at high risk for opioid misuse.13,14 To reduce prescription opioid–related morbidity and mortality, however, further development of screening tools for drug-related behaviors is needed. Moreover, routine use of prescription drug–monitoring programs is necessary to identify patients with ESRD with high-dose prescription, overlapping prescriptions, or prescriptions from various providers.5
Table 1.
Opioid Risk Tool (should be administered to patients on an initial visit before beginning opioid therapy for pain management)
| Item | Women | Men |
|---|---|---|
| Family history of substance abuse | ||
| Alcohol | 1 | 3 |
| Illegal drugs | 2 | 3 |
| Prescription drugs | 4 | 4 |
| Personal history of substance abuse | ||
| Alcohol | 3 | 3 |
| Illegal drugs | 4 | 4 |
| Prescription drugs | 5 | 5 |
| Age between 16 and 45 yr | 1 | 1 |
| History of preadolescent sexual abuse | 3 | 0 |
| Psychologic disease | ||
| Attention deficit/hyperactivity disorder, obsessive compulsive disorder, bipolar disorder, schizophrenia | 2 | 2 |
| Depression | 1 | 1 |
| Total score | ||
| Total score risk category for future prescription opioid abuse: 0–3, low risk; 4–7, moderate risk; ≥8, high risk |
Also found at https://www.drugabuse.gov/sites/default/files/files/OpioidRiskTool.pdf. Reprinted from Webster and Webster,16 with permission.
Depression, anxiety, and insomnia are common co-occurring disorders among patients with ESRD.2,4,12–14 Pain is a symptom of many pathologic processes.5 Pain not only can induce or exacerbate these disorders, but also, it can be intensified by these disorders.2,4 Better treatment of these underlying disorders is necessary to decrease pain, and treating pain may ameliorate these disorders.2,12–14 For example, calcium channel α2-δ ligands (e.g., gabapentin and pregabalin) can improve the symptoms of neuropathic pain, depression, and sleep disorders among patients with ESRD.14 In addition, patients with ESRD and neuropathic pain respond much better to antidepressants and anticonvulsants compared with opioids.2 However, treatment rates of these co-occurring disorders are low. More randomized, controlled trials are needed to support the efficacy and safety of related treatment regimens among patients with ESRD.12
The timely results found by Kimmel et al.8 suggest the need for appropriate pain management specifically for patients with ESRD. To reduce prescription opioids–related adverse outcomes, further development of screening tools for opioid misuse and use disorders and routine use of prescription drug–monitoring programs are needed. Future studies are needed to understand the actual use, use frequency, and dosage of prescription opioids to estimate the prevalence of prescription opioid misuse, use disorders, depression, anxiety, and insomnia, estimate the receipt of related treatments, and examine their relationships with adverse outcomes among patients with ESRD.
Disclosures
W.M.C. reports ownership of stock in General Electric Co., 3M Co., and Pfizer Inc. unrelated to the submitted work.
Acknowledgments
The findings and conclusions of this study are those of the authors and do not necessarily reflect the views of the Substance Abuse and Mental Health Services Administration, the National Institute on Drug Abuse, and the US Department of Health and Human Services.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related article, “Opioid Prescription, Morbidity, and Mortality in United States Dialysis Patients,” on pages 3658–3670.
References
- 1.Murtagh FE, Addington-Hall J, Higginson IJ: The prevalence of symptoms in end-stage renal disease: A systematic review. Adv Chronic Kidney Dis 14: 82–99, 2007 [DOI] [PubMed] [Google Scholar]
- 2.Santoro D, Satta E, Messina S, Costantino G, Savica V, Bellinghieri G: Pain in end-stage renal disease: A frequent and neglected clinical problem. Clin Nephrol 79[Suppl 1]: S2–S11, 2013 [PubMed] [Google Scholar]
- 3.Koncicki HM, Brennan F, Vinen K, Davison SN: An approach to pain management in end stage renal disease: Considerations for general management and intradialytic symptoms. Semin Dial 28: 384–391, 2015 [DOI] [PubMed] [Google Scholar]
- 4.Barakzoy AS, Moss AH: Efficacy of the world health organization analgesic ladder to treat pain in end-stage renal disease. J Am Soc Nephrol 17: 3198–3203, 2006 [DOI] [PubMed] [Google Scholar]
- 5.Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM: Prescription opioid use, misuse, and use disorders in U.S. adults: 2015 National survey on drug use and health. Ann Intern Med 167: 293–301, 2017 [DOI] [PubMed] [Google Scholar]
- 6.Han B, Compton WM, Jones CM, Cai R: Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003-2013. JAMA 314: 1468–1478, 2015 [DOI] [PubMed] [Google Scholar]
- 7.Rudd RA, Seth P, David F, Scholl L: Increases in drug and opioid-involved overdose deaths — United States, 2010–2015. MMWR Morb Mortal Wkly Rep 65: 1445–1452, 2016 [DOI] [PubMed] [Google Scholar]
- 8.Kimmel PL, Fwu CW, Abbott KC, Eggers AW, Kline PP, Eggers PW: Opioid prescription, morbidity, and mortality in United States dialysis patients. J Am Soc Nephrol 28: 3658–3670, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dowell D, Haegerich TM, Chou R: CDC guideline for prescribing opioids for chronic pain-United States, 2016. JAMA 315: 1624–1645, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agency for Healthcare Research and Quality: The Effectiveness and Risks of Long-Term Opioid Treatment of Chronic Pain, 2014. Available at: http://www.ahrq.gov/research/findings/evidence-based-reports/ opoidstp.html. Accessed September 12, 2017 [DOI] [PubMed]
- 11.World Health Organization: WHO Definition of Palliative Care, 2010. Available at: http://www.who.int/cancer/palliative/definition/en/. Accessed September 10, 2017
- 12.Davison SN: The ethics of end-of-life care for patients with ESRD. Clin J Am Soc Nephrol 7: 2049–2057, 2012 [DOI] [PubMed] [Google Scholar]
- 13.Koncicki HM, Unruh M, Schell JO: In reply to ‘opioid overuse or NSAID underuse? A response to the pain guide’. Am J Kidney Dis 69: 865–866, 2017 [DOI] [PubMed] [Google Scholar]
- 14.Koncicki HM, Unruh M, Schell JO: Pain management in CKD: A guide for nephrology providers. Am J Kidney Dis 69: 451–460, 2017 [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization: Cancer Pain Relief and Palliative Care: Report of a WHO Expert Committee, Geneva, Switzerland, World Health Organization, 1990, pp 7–21 [PubMed] [Google Scholar]
- 16.Webster LR, Webster RM: Predicting aberrant behaviors in opioid-treated patients: Preliminary validation of the Opioid Risk Tool. Pain Med 6: 432–442, 2005 [DOI] [PubMed] [Google Scholar]