The development of Poly(ADP-ribose) polymerase inhibitors (PARPi) for therapy is a successful application of bench-to-bedside medicine and nowhere is the impact more appreciated than in the treatment of advanced and recurrent ovarian cancer. Between December 2014 and July 2017, three PARPi (olaparib, rucaparib and niraparib) were approved for the treatment of recurrent ovarian cancer and approvals for additional disease indications are anticipated. In the coming years the focus will be to: define the clinical use of PARPi, examine the possibility of retreatment, and confront the inevitable challenge of PARPi resistance. This review will familiarize the reader with the science underlying PARP inhibition in ovarian cancer, the current approved indications for PARPi, the difference between available therapeutics, and finally introduce the concept of PARPi resistance and potential management strategies.
Ovarian Cancer and Homologous Recombination Repair
Homologous recombination (HR) DNA repair is involved in repairing DNA double strand breaks and functions to limit genetic instability, a hallmark of cancer. Notably, up to 50% of all high grade serous ovarian cancers (HGSOC) have detectable germline and somatic mutations or epigenetic silencing via DNA methylation of genes (e.g. BRCA1/2) involved in HR DNA repair [1]. BRCA1/2 mutation and silencing occurs in approximately 30% of HGSOC and frequently results in diminished HR activity. HR DNA repair is critical in the accurate repair of DNA following double strand breaks (DSB). HR repair is cell cycle dependent and is most active in the S to M transition [2] [Reviewed in [3, 4]]. Briefly, DNA DSBs promote the recruitment of nuclease complexes, such as Mre11/Rad50/Nbs1 (MRN) and Retinoblastoma-Binding Protein 8 (CtIP), to the sites of damage, which leads to Ataxia telangiectasia mutated (ATM) and ATM- and RAD3-related (ATR) mediated phosphorylation of histone 2Ax (γH2Ax). A BRCA1/2/PALB2-containing complex is then recruited to sites of DSBs, which facilitates the loading of a recombinase, RAD51, onto the MRN/CtIP processed DNA strands. RAD51 then plays a critical role in forming Holliday junctions (HJ) with homologous regions on the sister chromatid. HJs are then resolved through a combination of DNA helicases, nucleases, and topoisomerases, resulting in the DNA being unwound and repaired in a highly accurate fashion.
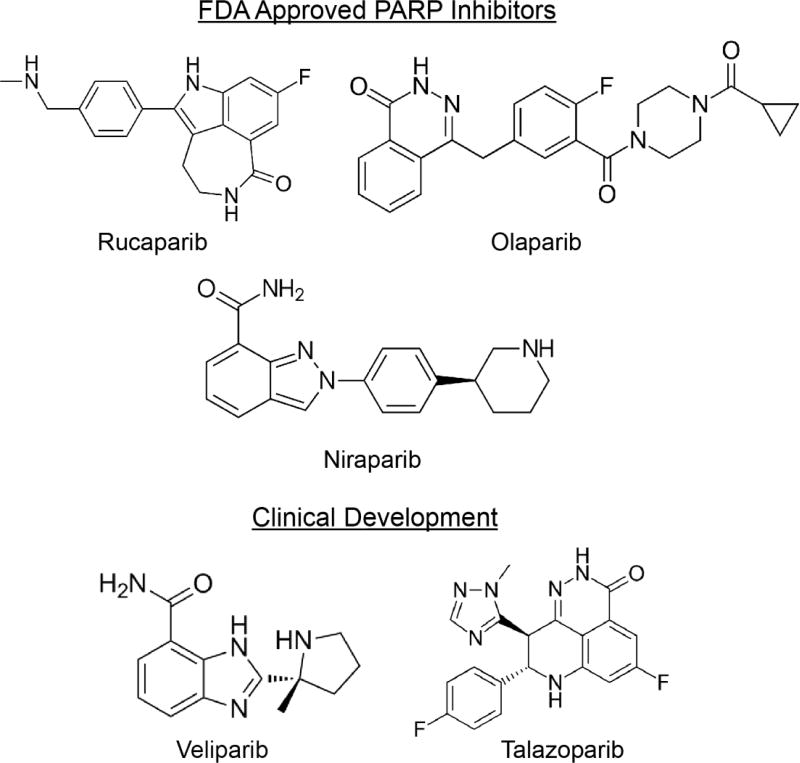
In 2005 and 2006 publications in Nature, Cancer Research and Cancer Biology and Therapy described inhibition of alternate DNA repair pathways, including base excision repair (BER) and single-strand break repair (SSBR), via PARP selectively promoted lethality in HR deficient (BRCA1/2-mutated) cancers [5–7]. There are 17 distinct PARP enzymes, however only PARP1-3 play a role in BER. PARPs function by binding to single strand DNA breaks and undergoing auto-modification (auto-PARylation) via polymerizing branched negatively charged poly(ADP-ribose) polymers. The PARP mediated increase of a localized negative electrostatic charge is hypothesized to recruit DNA repair enzymes [Reviewed in [8]]. In the context of PARP inhibition, the lack of a functional HR repair pathway leads to irreparable single-strand breaks, replication fork stalling, accumulation of DNA DSBs, and catastrophic mitotic failure [5]. Independent of BRCA1/2, mutations in other HR repair molecules, such as PALB2, ATM, BRIP1, CHEK2, and RAD51, are now appreciated to convey increased PARPi sensitivity [9–12]. However, one of the approved PARPi, niraparib, was observed to have a significant clinical benefit in patients without detectable mutations in HR components, which indicates that in addition to HR genes there are other potential predicative biomarkers and mechanisms that contribute to PARPi sensitivity. The next section will examine the status of current PARPi, including both Food and Drug Administration (FDA)-approved therapeutics and those in clinical development (Fig. 1).
Figure 1. PARP inhibitors that are FDA-approved or in clinical development.
PARP Inhibitors
FDA-Approved
FDA approval of olaparib (AstraZeneca) was announced on December 2014 for monotherapy of germline BRCA (gBRCA) mutated ovarian cancer after third line therapy based on a nonrandomized study of olaparib monotherapy in gBRCA mutated cancers [13, 14]. A subgroup of patients in this study were extracted for FDA submission and included 137 recurrent ovarian cancer patients with measurable disease after three or more lines of chemotherapy. Patients received 400 mg (8 capsules) olaparib twice daily until progression or intolerable toxicity. Retrospective BRCA1/2 mutation analysis of 61 treated patient samples demonstrated high concordance with initial testing 96.7% (59/61; 95% CI, 88.7–99.6) [14]. RECIST 1.1 objective response rate was 34% (range 26%–42%) with a median duration response of 7.9 months (5.6–9.6 months) in this heavily pretreated group. Toxicities were similar in the entire group and in ovarian cancer patients specifically and included nausea and fatigue in over 60% of patients. Most toxicities were managed by dose interruption and dose reduction. More recently, olaparib maintenance therapy of recurrent platinum sensitive gBRCA mutated ovarian cancer in the Phase III SOLO2/ENGOT-Ov21 trial showed a dramatic improvement in progression-free survival (PFS) of 19.1 months versus 5.5 months (hazard ratio [HR] = 0.3, 95% confidence interval [CI]: 0.22–0.41) in treated patients using a 300 mg (two tablets) twice daily formulation [15]. Overall survival has been not yet been calculated in SOLO2 study. The SOLO2 findings confirmed Study 19, which had demonstrated a PFS benefit and a nonsignificant survival benefit and led to European and not United States FDA approval for maintenance olaparib. The US FDA had at that time declined approval based on lack of survival benefit [16, 17]. Nausea, fatigue, vomiting and anemia were all more common with olaparib than placebo but the majority of adverse events were grades 1 and 2. A clinical trial to evaluate maintenance olaparib following first line platinum-based chemotherapy (SOLO1, NCT01844986) is on-going.
FDA approval of rucaparib (Clovis Oncology) was announced on December 19, 2016 based on the results of two multicenter randomized open label trials, Study 10 and ARIEL, parts 1 and 2 [18, 19]. The two phase (I/II) Study 10, reported in early 2017, enrolled 56 patients with gBRCA mutated platinum sensitive ovarian cancer with two to four lines of previous therapy. The phase II portion of Study 10 enrolled 42 patients, after establishing the phase I dose of 600 mg twice daily, and showed a 59.5% investigator-assessed overall response rate [18]. ARIEL 2 enrolled patients with gBRCA mutations and platinum-sensitive high grade ovarian carcinoma, and defined HR deficiency subgroups: BRCA mutant (deleterious germline or somatic), BRCA wild type with loss of heterozygosity (LOH) high, or BRCA wildtype with LOH low, using a cutoff of 14% or more genomic LOH for LOH high. Median PFS was significantly longer in BRCA mutant subgroup (12.8 months, 95% CI: 9.0–14.7) (HR = 0.27,95% CI: 0.16–0.44 p<0.0001), and less dramatically, but still significantly longer in the LOH high subgroup (5.7 months. 95% CI: 5.3–7.6) (HR = 0.62, 95% CI 0.42–0.90, p=0.011) as compared to the LOH low subgroup (5.2 months, 95% CI: 3.6–5.5). The most common grade 3 toxicities were anemia and liver enzyme elevations (Table 1). Based on efficacy and low toxicity, the FDA approved rucaparib for third line treatment of platinum sensitive gBRCA mutated ovarian cancer. ARIEL 3, a phase III trial investigating the maintenance of rucaparib versus placebo following a response to second line or later platinum-based chemotherapy was recently published [20]. ARIEL 3 findings demonstrated a dramatically improved investigator-reviewed PFS (primary endpoint) in BRCA-mutant tumors compared to placebo treated patients (inclusive of gBRCA mutation, 16.6 months vs. 5.4 months). Rucaparib significantly improved PFS in HR Deficient/high LOH patients compared to placebo (13.6 months vs. 5.4 months) and overall intent-to-treat populations (10.8 months vs. 5.4 months). The key secondary endpoint of blinded independent central review PFS was also significant (inclusive of gBRCA mutation, 26.8 months vs. 5.4 months) as well as HR Deficient/high LOH (22.9 months versus 5.5 months) and overall intent-to-treat populations (13.7 months vs 5.4 months). Consistent with prior studies of rucaparib, the most common side effects were gastrointestinal (nausea and vomiting), fatigue, and anemia. The ARIEL 4 trial comparing rucaparib with chemotherapy in relapsed patients is currently open for enrollment (NCT02855944).
Table 1.
Adverse Effects of PARP inhibitors
| Olaparib SOLO2/ENGOT- Ov21 (n=195) |
Niraparib NOVA/ENGOT- OV16 (n=367) |
Rucaparib ARIEL2 (n=204) / ARIEL3 (n=374) |
Veliparib Coleman, RL 2015 (n=50) |
Talazoparib NCT01286987 (n=71) |
|
|---|---|---|---|---|---|
| Grade 3 and 4 adverse events |
|
|
|
|
|
| Serious adverse events | Total 35 (18%)
|
Total 110 (30%) |
|
Total 12 (24%) | Not reported. |
| Changes in dose due to AE |
|
|
|
|
Dose reductions from 1.0mg/day dose: 26 (34%) |
Dose reductions were offered to patients with significant adverse effects.
FDA approval of niraparib (Tesaro, Inc) was announced on March 27, 2017 for maintenance therapy of recurrent platinum sensitive ovarian, fallopian tube, or primary peritoneal cancer, regardless of BRCA status based on the phase III ENGOT-OV16/NOVA trial [21]. Niraparib is commercially available as 100 mg capsules and is dosed at 300 mg daily. The NOVA trial showed that niraparib significantly increased median PFS in platinum-sensitive ovarian cancer independent of HR deficiency (HRD) and gBRCA mutations [21]. A total of 553 patients were divided into two main cohorts: gBRCA mutated and non-germline BRCA mutated. In gBRCA mutant patients niraparib significantly extended median PFS compared to placebo (21.0 months vs. 5.5 months; HR = 0.27,95% CI: 0.17–0.4). When HR deficient (HDR) tumors (myChoice HRD test; Myriad Genetics) were retrospectively analyzed in an exploratory analysis out of the non-gBRCA group, niraparib conveyed a 62% reduction in the risk of progression (PFS 12.9 months versus 3.8 months; HR = 0.38,95% CI: 0.24–0.59). Non-gBRCA mutant and negative HRD patients treated with niraparib demonstrated a smaller but significant extension of PFS compared to placebo (9.3 months vs. 3.9 months; HR = 0.45, 95% CI: 0.34–0.61). A clinical trial is currently recruiting patients to evaluate maintenance niraparib following response to first line platinum-based chemotherapy (NCT02655016). Niraparib associated toxicities included thrombocytopenia and anemia. The observed increase in PFS in patients not predicted to respond demonstrates the need for improved prediction tools independent of HR deficiency.
Clinical Development
Veliparib (ABT-888) is being developed by Abbvie and was initially demonstrated in 2007 to have high anti-tumor properties in combination with DNA alkylating agents (e.g. temozolomide) and irradiation [22]. In a phase II single agent evaluation of veliparib, 50 BRCA-mutated patients were treated with 400mg orally twice daily until progression or intolerance [23]. The overall response rate to veliparib was 26% (90%CI: 16–38%) but 61% (31/50) of patients progressed on treatment. The observed adverse events were predominantly nausea and anemia. Numerous clinical trials have been conducted with veliparib in combination with other agents (temozolomide, carboplatin/taxol, whole abdomen radiation) for several indications; however results have been mixed. In a phase I trial to determine veliparib maximum tolerated dose (MTD) in platinum refractory ovarian or basal-like breast cancer, both mutant and wildtype BRCA2 tumors responded with clinical benefit rates of 68 and 38%, respectively (NCT00892736). In contrast, a phase I clinical trial examining veliparib in combination with low-dose fractionated whole abdominal radiation found an objective response rate of 3% (1 of 32 patients), but noted a potential benefit to patients with platinum-sensitive BRCA-mutated ovarian cancer [24]. Veliparib was noted to have lower efficacy than previously reported PARPi in a similar patient population. At the 2017 ASCO meeting, a triple negative breast cancer phase III clinical trial evaluating veliparib combined with traditional chemotherapies (carboplatin/paclitaxel) and subsequent maintenance with doxorubicin cyclophosphamide, found addition of veliparib did not significantly impact pathologic complete response rates (53.2% versus 57%, p=0.36) [25]. The potential impact of veliparib in the setting of BRCA-mutated ovarian cancer remains unclear; however there are currently nine clinical trials actively recruiting patients examining veliparib with combinatorial therapies (Table 2).
Table 2.
Actively Recruiting Clinical Trials Evaluating PARP inhibitor combination
| Therapeutics | Indications | Phase | Clinical Trial |
Target |
|---|---|---|---|---|
| Niraparib/Bevacizu mab | Platinum-sensitive Epithelial Ovarian Cancer | I/II | NCT02354131 | VEGFR |
| Niraparib/Pembroli zumab | Triple-negative Breast Cancer or Ovarian Cancer | I/II | NCT02657889 | PD-1 |
| Olaparib/AT13387 | Metastati Solid Tumors/Cannot Be Removed by Surgery/Recurrent Ovarian/Fallopian Tube/Primary Peritoneal/Triple-Negative Breast Cancer | I | NCT02898207 | HSP90 |
| Olaparib/AZD2014/AZD5363 | Recurrent Endometrial, Triple Negative Breast, and Ovarian, Primary Peritoneal, or Fallopian Tube Cancer | I/II | NCT02208375 | mTORC1/2 or AKT |
| Olaparib/AZD2281/AZD5363/AZD1775/AZD2014 | Advanced Solid Tumors | II | NCT02576444 | PI3K/AKT, WEE1, mTORC1/2 |
| Olaparib/Cediranib | Time Ovarian Cancer Worsens on Olaparib | II | NCT02340611 | VEGFR1/2/3 |
| Olaparib/Cediranib | Patients With Recurrent Platinum-Sensitive Ovarian, Fallopian Tube, or Primary Peritoneal Cancer | III | NCT02446600 | VEGFR1/2/3 |
| Olaparib/Cediranib/MEDI4736 | Advanced Solid Tumors and Advanced or Recurrent Ovarian, Triple Negative Breast, Lung, Prostate and Colorectal Cancers | I/II | NCT02484404 | VEGFR1/2/3, PD-L1 |
| Olaparib/Prexasertib | Advanced Solid Tumors | I | NCT03057145 | CHK1 |
| Olaparib/Tremelimumab | BRCA-deficient Ovarian Cancer | I/II | NCT02571725 | CTLA4 |
| Rucaparib/Atezolizumab | Solid Tumors and Advanced Gynecologic Cancers | II | NCT03101280 | PD-L1 |
| Veliparib/Carboplatin/Paclitaxel | Maintenance Therapy in Newly Diagnosed Stage III or IV High-grade Serous/Epithelial Ovarian/Fallopian Tube/Primary Peritoneal Cancer | III | NCT02470585 | Standard-of-care |
| Veliparib/Dinaciclib | Advanced Solid Tumors (BRCA1/2 mutation) | I | NCT01434316 | CDK12 |
| Veliparib/Floxuridine | Metastatic Epithelial Ovarian, Primary Peritoneal Cavity, or Fallopian Tube Cancer | I | NCT01749397 | Nucleotide Analog |
| Veliparib/Irinotecan | Stage III, IIIB, IIIC, IV Ovarian Cancer | I | NCT00576654 | Topoisome rase |
| Veliparib/Irinotecan | Cancer That Is Metastatic or Cannot Be Removed by Surgery | I | NCT02484404 | Topoisome rase |
| Veliparib/Liposomal Irinotecan | Malignant Solid Neoplasm | I | NCT02631733 | Topoisome rase |
| Veliparib/Nivolumab | Recurrent or Refractory Stage IV Solid Tumors That Cannot Be Removed or Lymphoma With or Without Alterations in DNA Repair Genes | I | NCT03061188 | PD-1 |
| Veliparib/Topotecan | Solid Tumors, Relapsed or Refractory Ovarian Cancer, or Primary Peritoneal Cancer | I/II | NCT01012817 | Topoisome rase |
| Veliparib/VX-970/cisplatin | Refractory Solid Tumors | I | NCT02723864 | ATR |
Talazoparib (MDV3800/BMN 673), is being developed by Medivation/Pfizer, and is a more recent addition to the PARPi repertoire. Talazoparib is a selective PARP1/2 inhibitor that has demonstrated increased in vitro anti-tumor efficacy at comparable doses to other PARPi [26]. A recent phase I dose escalation trial in several tumor types, including ovarian, breast, prostate, small cell lung, found that talazoparib as a single agent had a significant clinical benefit in all tumor types. In ovarian, the maximum tolerated dose (1 mg/day) resulted in a clinical benefit rate of 76% in BRCA-mutant cancers [27]. Reported toxicities include alopecia, neutropenia, thromobocytopenia, anemia, fatigue, and nausea [27]. Based on clinicaltrials.gov, there are currently 12 trials actively recruiting patients that are utilizing talazoparib as a single agent or in combination (Table 2).
Toxicities
Adverse events to PARPi have been observed and while there is overlap in toxicities for each of the PARPi there are some marked differences. Table 1 details the grade 3 and 4 PARPi toxicities, observed adverse events, and resulting changes to therapeutic strategies. In SOLO2, NOVA, ARIEL2 and ARIEL3 grade 3 and 4 anemia was observed in 18 to 45% of patients. In contrast, grade 3 and 4 thrombocytopenia was notably higher in the NOVA trial (33.8%) compared to SOLO2 (1%), ARIEL2 (2%) and ARIEL3 trials (5%). Observed adverse events resulted in dose reduction in 25–66.5% of cases. In contrast, dose discontinuation due to adverse toxicities only occurred in 9–11% of cases.
Biomarkers
A biomarker is a biological indicator that can serve as a predictor of disease, a measure of disease, or therapeutic response. HR deficiency (HRD) testing is an example of a biomarker that predicts PARP inhibitor response [28]. Although as demonstrated by the ENGOT-OV16/NOVA clinical trial, identifying patients that are predicted to respond to niraparib through BRCA mutational status or HRD is not entirely inclusive of responders [21]. In contrast, Study 42 examined olaparib only in gBRCA mutation carriers and found an objective response rate of 34% [29]. These trials indicate that additional biomarkers are needed to increase predictive values of PARPi response. Therefore, this section examines current and in-development biomarkers utilized to predict response.
Panel of HR-related Biomarkers
Mutation and epigenetic (i.e. promoter methylation) silencing of BRCA1/2 occurs in up to 30% of high-grade serous cancer (HGSOC) cases [1]. Next-generation sequencing of HGSOC tumors revealed that, independent of BRCA1/2, mutations in HR effectors (PALB2, RAD51, ATM, BRIP1, BARD1) occurs in up to 20% of HGSOC cases [1]. As a result, about 50% of HGSOC tumors are predicted to have deficient or non-functional DNA repair pathways. To test HRD several companies such as Myriad Genetics, Ambry Genetics, and GeneDX, are now utilizing next generation sequencing to identify mutations in a panel of HR related genes. Briefly, HRD is determined by assigning HR component mutations into three categories: likely pathogenic (positive), uncertain significance, or negative [Reviewed in [30]]. In 2014, olaparib was demonstrated to convey an increased clinical benefit in patients with a positive HRD test (Myriad Genetics) [28]. HRD testing has been implemented and used as a stratification criterion for several PARPi clinical trials [20, 21, 28]. However, there are limitations of HRD testing, including prioritization and predicted impact of observed mutations, little emphasis on gene silencing via DNA methylation, and false positive rates. Building on HRD testing, recent testing of functional DNA repair has shown promise in identifying potential PARPi responders.
Functional DNA Repair
The current target population for olaparib and rucaparib are patients with deficient HR DNA repair, which includes BRCA1/2-mutation (germline-olaparib or somatic-rucaparib) or a positive HRD score. Beyond mutations within the HR pathway, the inability to repair DNA DSBs promotes genetic instability. Genetic aberrations or “scarring” are common in HGSOC and this observation has led to the development of several novel DNA sequencing-based assays to assess the extent of genetic instability to better predict PARP inhibitor response. These assays include: extent of somatic mutations (Nmut), loss-of-heterozygosity (LOH), telomeric allelic imbalance (NtAi), and mutational signature [Reviewed in [31]]. In the phase II ARIEL 2 trial, in addition to germline or somatic BRCA mutation, genomic instability (i.e. LOH) was utilized as an inclusion criterion. Notably, BRCA wildtype patients with LOH had appreciable and significant objective response rates (RECIST/CA-125) compared to BRCA wildtype patients without LOH (44% [95% CI 33–55%] versus 20% [95% CI 11–31%) [19]. In contrast, ARIEL 3 examined rucaparib in BRCA wildtype patients with high, low or indeterminate LOH and observed that LOH status did not alter clinical benefit [20]. Thus combining traditional genetic testing with DNA repair activity readouts (e.g. LOH) could improve the ability to identify potential responders; however further research is still required to elucidate the impact of LOH on PARPi response.
PARP Expression
Expression levels of PARP1/2 are hypothesized to be biomarker of inhibitor response. Olaparib and veliparib are highly selective inhibitors of PARP1 and PARP2; however other inhibitors (niraparib, rucaparib, and talazoparib) are broad PARPi. In ovarian cancer cell lines PARP1 protein expression positively correlated with PARP inhibitor response [32]. In 186 ovarian cancer patients, elevated expression of PARP/P53/FANCD2 increased the risk of recurrence and platinum resistance [33]. In contrast, a recent immunohistochemical (IHC) based approach evaluating PARP1 expression in 170 primary ovarian cancer samples concluded PARP1 did not impact patient outcome [34]. This indicates that although PARP expression does not always correlate with outcome, PARP enzymatic activity could have a higher predictive value. As an approach to examine PARP1 in vivo, a recent study examined the utility of a PARP1 radiotracer ([125I]KX1) to measure expression and activity of PARP1 with the goal of identifying potential PARPi responders [35]. PARP1 expression and activity significantly correlated to response rates of two independent PARPi (olaparib and talazoparib). Further research is required in evaluating PARP expression/activity and PARPi response; however there is an indication that PARP expression/activity could serve as an additional biomarker to predict clinical response.
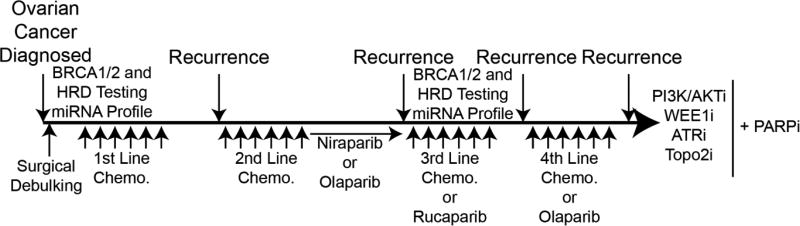
Implications of PARPi Treatment
Given the varied indications for FDA-approved PARPi, oncologists now have options when treating recurrent ovarian cancer patients. BRCA1/2-mutant tumors respond more favorably to chemotherapy and PARPi. Independent of BRCA1/2, mutations in other HR repair components (RAD51, PALB2) also convey increased sensitivity to PARPi [10, 36]. As a hypothetical case after the diagnosis of HGSOC, biomarkers should be assessed (see above) and patients treated with first line platinum and taxane chemotherapies. Following recurrence, if platinum sensitive, re-treated with platinum based combination, followed by niraparib or olaparib maintenance. Then at third recurrence if the patient is still classified as platinum sensitive they can be re-tested for BRCA mutations or other biomarkers and if positive, offered rucaparib as standard of care. On the other hand, if chemotherapy is chosen as third line instead of rucaparib, the patient (if gBRCA mutation) can be offered olaparib as a fourth line therapy. Because there is a definite sequence (Fig. 2) that involves repeated treatment with PARPi, the identification of and strategies for managing PARPi response and resistance begins to gain importance.
Figure 2. Proposed treatment regimen for platinum-sensitive, BRCA1/2-mutated or HRD positive recurrent ovarian cancer.
There are now several clinical options of PARPi. As PARPi are more widely utilized there is significant need to delineate, prioritize, and standardize treatment strategies. Depicted is a hypothetical treatment plan for an ovarian cancer patient.
PARP inhibitor resistance
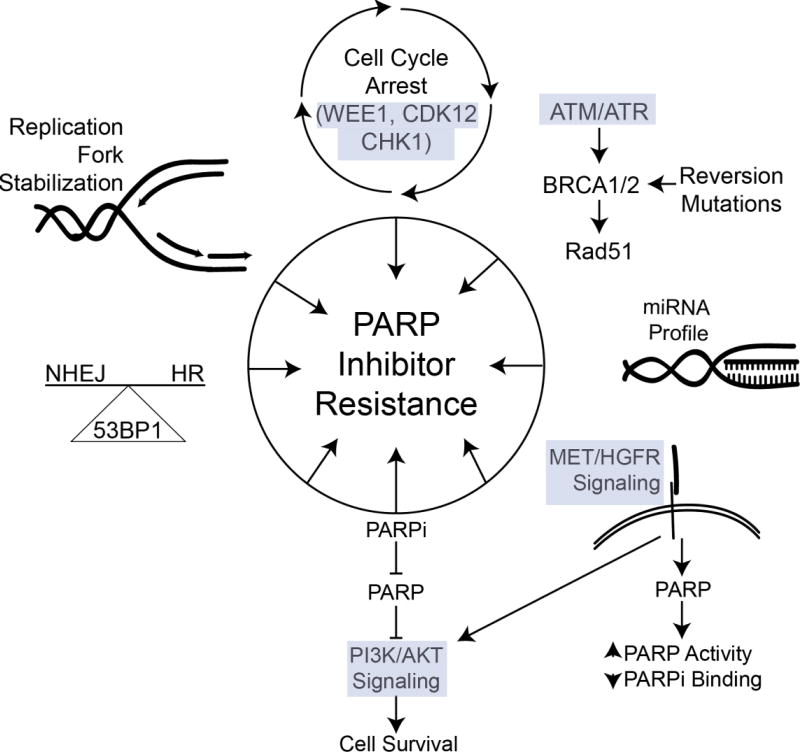
PARPi offer a significant clinical benefit and there are currently 19 clinical trials actively recruiting patients to evaluate novel PARPi combinatorial approaches (Table 2). Also, while there is an emphasis on examining PARPi resistance, there is also a significant need to better characterize patients that have sustained response to PARPi, which is evidenced by the initiation of a clinical trial to evaluate mechanisms involved in conveying a prolonged (>4 years) olaparib response (NCT02489058). The characterization of the responders will be included in future review article. This section will examine mechanism of PARPi resistance (Figure 3) and possibilities to clinically manage resistant disease.
Figure 3. PARPi resistance is mediated through a variety of targetable pathways.
The FDA has approved three PARPi for ovarian cancer and as PARPi are commonly prescribed there will be an increase in acquired resistance. Currently, several targetable pathways (HR restoration, PI3K/AKT, miRNA) have been attributed to resistance.
Homologous Recombination Repair Restoration
Secondary BRCA1/2 mutations
The most widely accepted mechanism of PARPi resistance is the restoration of the HR pathway through secondary reversion mutations. Several studies have discovered that BRCA-mutated tumors develop resistance to DNA damaging agents (platinum-based chemotherapies and PARPi) through reversion or secondary BRCA mutations [37, 38]. Norquist et al evaluated BRCA mutations in 46 recurrent ovarian carcinomas previously treated with a platinum-based chemotherapy. They observed 28% (13 of 46; 95% CI: 17.3% to 42.6%) of tumors had secondary BRCA mutations that were predicted to restore BRCA function and HR activity. The authors predicted that secondary mutations convey resistance to not only platinum-based therapies, but PARPi as well [38]. Barber et al evaluated the BRCA2 loci from an initial primary stage III HGSOC tumor, compared with a post-olaparib treated lymph node metastasis. Targeted deep sequencing of the BRCA2 loci revealed a mutation in the primary tumor, resulting in a truncated form of BRCA2. In lymph node metastasis secondary 4 and 12bp deletions that restored the open-reading frame of BRCA2 were detected [37]. These studies suggest that evaluating BRCA mutational profile in recurrent tumors could predict response to subsequent treatment with PARP inhibitors and DNA-damaging agents.
53BP1 Regulation
In the absence of BRCA1/2 reversion, hyperactivation of non-homologous end-joining (NHEJ) could be a contributor to PARPi resistance. Unlike HR, NHEJ involves only minor resection of DNA ends at sites of DSB and is typically error-prone [Reviewed in [39]]. Normally regulated by BRCA1, the TP53 binding protein 1 (53BP1) maintains the balance between HR and NHEJ, which is shifted to NHEJ in BRCA1-mutated and HRD positive tumors [40]. 53BP1 promotes NHEJ by inhibiting the extensive DNA end-resection required for HR repair, therefore loss of 53BP1 function by mutation or downregulation facilitates BRCA1-independent end-resection and conveys PARPi resistance [35]. In vitro studies showed that loss of 53BP1 in BRCA1-null cells partially restored HR function and reversed sensitivity to PARPi [40, 41] [Reviewed in [42]]. Additionally, in a BRCA1-mutated cell line, a combination of 53BP1 mutation and mutant BRCA1 stabilization via heat shock protein 90 (HSP90) led to rucaparib resistance [43]. An HSP90 inhibitor (AT13387) is being evaluated in combination with olaparib (NCT02898207). Finally, the interplay between 53BP1 and HR repair suggests a role for 53BP1 expression as a biomarker for identifying patients that could benefit from PARPi.
Replication Fork Dynamics
PARP1 is recruited to sites of single-strand DNA damage and subsequent auto-PARylation leads to the recruitment of HR effectors. During replication the recruitment of HR effectors promotes slowing of replication fork and facilitates DNA repair [44]. A recent report observed that independent of BRCA1/2 reversion mutations, increased stabilization of replication forks confers resistance to PARPi. The loss of a HR repair protein, Pax2 transactivation domain-interacting protein (PTIP), reduces the recruitment of MRN to stalled replication forks, which protects these replication forks from degradation and ultimately confers resistance to PARPi [45]. During DNA replication, topoisomerase unwinds the DNA to prevent accumulation of torsional forces. Topoisomerase inhibition leads to the de-stabilization of replication forks and promotes DNA breakage [46]. Topoisomerase inhibition is an approved anti-cancer therapeutic approach. Taken together targeting stalled replication forks through topoisomerase inhibition in combination with PARPi could promote an increased anti-tumor response. This approach has been evaluated in vitro and anti-tumor effects due to topoisomerase inhibition were potentiated following PARP inhibition [47, 48]. In 2012, a phase I clinical trial examining olaparib in combination with topotecan in solid tumors observed an objective response rate of 32% (6/9 patients); however the investigators did not recommend the use of this combination given increased adverse effects, primarily neutropenia [49]. Also, the authors noted decreased bioavailability of olaparib with concomitant topotecan treatment potentially due to overlap in drug efflux action, suggesting an altered dosing schedule could prove to be more effective. There are currently several clinical trials underway in ovarian cancer investigating the combination of a topoisomerase inhibitors (topotecan/irinotecan) and PARPi (veliparib/olaparib) (Table 2).
Resistance mechanisms discussed thus far depend on the reactivation of HR repair. Tumors with restored HR repair activity present a clinical challenge given DNA damaging agents are more effective in the absence of HR activity. Therefore, a potential path forward for these patients is to reestablish “BRCAness” by targeting HR repair upstream of BRCA1/2. This next section will examine the potential of promoting PARPi resensitization in HR repair restored PARPi resistant tumors.
Exploiting Altered Cell Cycle Regulation
HR repair is highly dependent on the cell cycle phase, because signaling occurring during G1 to S phases induces the upregulation of many HR repair effectors [2]. In a genome-wide RNA interference screen in an olaparib resistant cell line, established factors (BRCA1/2 and RAD51) were identified to convey increased PARPi sensitivity. Also, knockdown of a cell cycle regulator, cyclin-dependent kinase 12 (CDK12), was found to promote olaparib sensitivity [50]. Mechanistically, knockdown of CDK12 leads to the concomitant downregulation of DNA repair proteins (such as BRCA1, FANC1, and ATR) thereby artificially establishing a “BRCAness” phenotype [51]. In late 2016 two in vitro studies reported that pharmacological inhibition of CDK12 with Dinaciclib reverses acquired PARPi resistance [52, 53]. Increased expression of WEE1, another cell cycle regulator, promotes de-sensitization of PARPi [54]. WEE1 promotes a reversible cell cycle arrest to allow for DNA repair to occur. Thus, inhibition of WEE1 will force the cells to enter the S-phase of the cell cycle and in the context of HR deficiency and PARP inhibition- will lead to the further accumulation of DNA DSBs. In a pancreatic cancer mouse model, combining WEE1 and PARP inhibitors with radiation (RT) led to a significant inhibition in tumor growth [55]. A phase I clinical trial examining a WEE1 inhibitor as a single agent observed that at the maximum tolerated dose (MTD; 225mg twice a day) there was a partial clinical benefit in 2 of 6 BRCA 1/2-mutated patients (head/neck and ovarian cancers) [56]. Observed toxicities were diarrhea, myelosuppression, and supraventricular tachyarrhythmia. In the context of HR restored PARPi resistant tumors, inhibiting CDK12 or WEE1 in combination could be an approach to overcome resistance.
ATM/ATR are serine/threonine kinases involved in HR repair through the phosphorylation of Histone H2A at sites of DNA damage and recruitment of repair complexes (i.e. BRCA1/2). In gynecologic cancer cell lines (ovarian, endometrial, and cervical) ATM and ATR inhibitors were evaluated in combination with cisplatin or irradiation [57]. ATR inhibition promoted an enhanced response to cisplatin and irradiation. Notably, the ovarian cancer cell line (OVCAR3) utilized is predicted to have functional DNA repair pathway. As mentioned above, tumors that are PARPi resistant due to HR restoration could be subsequently treated by targeting earlier events in HR repair, for example ATM/ATR phosphorylation at sites of DNA damage (γH2Ax). A clinical trial in advanced ovarian cancer evaluating talazoparib assessed ATR mutations and activity pre- and post-treatment (NCT01989546). The study completed in June of 2017 and when reported will give insight into the importance of ATR on talazoparib response. There are several clinical trials actively recruiting ovarian cancer patients to evaluate PARP inhibition in combination (CDK12, WEE1, and ATR; Table 2).
The restoration or temporary induction of “BRCAness” via manipulation of the HR repair pathway or cell cycle could prolong PARPi response and potentially offer a clinical approach for PARPi resistant disease. The next sections will examine mechanism of resistance independent of restored HR activity.
Drug Efflux
Regardless of chemotherapy or targeted therapy, tumor cells are able to overcome therapeutic response through the upregulation of drug efflux pump (p-glycoproteins). In Brca1-null and p53-null mouse mammary gland tumors, several p-glycoproteins (Abcb1a, Abcb1b, Abcc1, Abcg2) were upregulated in response to both treatment and maintenance dosing of olaparib [58]. Furthermore, treatment with a p-glycoprotein inhibitor, tariquidar, following relapse of olaparib treated tumors resensitized tumors to olaparib and promoted tumor regression. There have been a multitude of pre-clinical studies that have effectively targeted p-glycoprotein to overcome therapeutic resistance. However, the clinical impact of p-glycoprotein inhibitors has been stymied by toxicity and lack of specificity. Given the observed upregulation of p-glycoproteins in resistant tumors the field has shifted to elucidating upstream mechanisms of p-glycoprotein regulation, which could prove to be more targetable and better tolerated [Reviewed in [59]]. Targeting p-glycoprotein activity in the context of PARPi resistance could be a highly effective approach to overcome therapy resistance, but further research is needed.
Signal Transduction
The MET/HGFR and PI3K/AKT signaling cascades are highly dependent on kinase activity for signal propagation. Aberrant MET/HGFR and PI3K/AKT signaling have both been described to contribute to tumorigenesis and PARPi resistance. The receptor tyrosine kinase MET/HGFR is amplified or upregulated in 10% of ovarian cancers [1]. MET directly phosphorylates PARP1, which increases PARP activity and reduces the binding affinity of PARPi [60]. The observed upregulation or amplification of MET correlated with PARPi insensitivity and resistance. There are currently seven clinical trials investigating MET inhibitors as a single agent in solid tumors. There is a need for further pre-clinical models to evaluate the safety profile of MET and PARPi combination.
The PI3K/AKT pathway is an oncogenic signaling pathway that plays a critical role in tumorigenesis in a number of cancer types including ovarian cancer. Reduction of PARP1 activity via PARPi can lead to the upregulation of the PI3K/AKT pro-survival pathway [61–63]. This suggests that increased PI3K/AKT signaling could promote PARPi resistance. Given increased MET and PI3K/AKT activity contribute to decreased PARPi response, combining small molecules targeting these pathways with PARPi would potentially provide a greater clinical benefit. Currently, there are two clinical trials actively recruiting to examine PARPi and PI3K/AKT combinatorial therapies (Table 2).
miRNA Environment
Alterations in microRNA (miR) profiles modulate PARPi sensitivity through downregulation of critical DNA repair genes [Reviewed in [64]]. A recent example is the regulation of miR-622, which promotes PARPi resistance by modulating the balance of DNA repair pathways [65]. MiR-622 selectively inhibits the expression of NHEJ components (Ku70/80), which promotes genome stabilization following the exposure to DNA damaging agents or PARPi. Upon examination of miR-622 expression in BRCA-inactivated ovarian cancer, high expression of miR-622 predicted a worse disease free survival (14.7 versus 19.8 months; log rank p = 0.03) and overall survival (39 versus 49.3 months; log rank p = 0.03) [65]. Another miRNA (miRNA-182) was also observed to increase PARPi sensitivity via downregulation of BRCA1 [66]. Although not clinically targetable, examining miRNA expression - specifically miR-182 and miR-622 could serve as biomarkers to aid in predicting PARPi response.
PARP Expression
There are 17 PARP enzymes with varied activity and PARP1-3 are directly involved in BER/SSBR. Of the current PARPi, olaparib and veliparib are highly selective inhibitors of PARP1 and PARP2; however other inhibitors (niraparib, rucaparib, and talazoparib) are broader PARPi. Chemical structures of all PARP inhibitors are different and have diverse off-target effects [67]. These differences indicate that the use of a secondary PARPi could potentially be effective in a resistant tumor. For example, a patient that develops to resistance to olaparib could subsequently be treated with niraparib. Further research on the impact of compensatory expression of other PARPs to promote PARPi resistance is needed.
Conclusion
In this review we discussed FDA approved PARPi, their disease indications, related toxicities, mechanisms of resistance, and options to overcome resistance. Moving forward, there is adequate data to indicate expansion of PARPi use in the treatment and maintenance setting for platinum-sensitive high grade ovarian cancer regardless of BRCA-status or HR deficiency. However, there is still a significant paucity in understanding the mechanisms contributing to clinical PARPi responses in the absence of HR deficiency. In the future, elucidating HR-independent mechanisms of PARPi sensitivity will be a vital area of research. Importantly, expansion of PARPi use in the clinical setting should result in an increase the availability of biological samples from PARPi treated ovarian tumors. The increased availability of PARPi treated specimens will accelerate investigations and hopefully provide insight into novel biomarkers and acquired resistance mechanisms. Overall, PARP inhibition represents a significant shift in the clinical management of high grade serous ovarian cancers.
Highlights.
Indications and toxicities of clinically applicable PARP inhibitors
Novel biomarkers to predict PARP inhibitor response
Molecular mechanisms of PARP inhibitor resistance
Managing PARP inhibitor resistant ovarian cancer
Acknowledgments
The authors wish to thank Chanel Mansfield for comments and critical reading. B.G. Bitler is supported by a NIH/NCI grant (R00CA194318).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: Dr. Behbakht reports other support from Genentech, which outside the submitted work. The other authors declare no conflict interests.
References
- 1.Integrated genomic analyses of ovarian carcinoma. Nature. 2011;474:609–15. doi: 10.1038/nature10166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ira G, Pellicioli A, Balijja A, Wang X, Fiorani S, Carotenuto W, et al. DNA end resection, homologous recombination and DNA damage checkpoint activation require CDK1. Nature. 2004;431:1011–7. doi: 10.1038/nature02964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jasin M, Rothstein R. Repair of strand breaks by homologous recombination. Cold Spring Harb Perspect Biol. 2013;5:a012740. doi: 10.1101/cshperspect.a012740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Konstantinopoulos PA, Ceccaldi R, Shapiro GI, D’Andrea AD. Homologous Recombination Deficiency: Exploiting the Fundamental Vulnerability of Ovarian Cancer. Cancer discovery. 2015;5:1137–54. doi: 10.1158/2159-8290.CD-15-0714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farmer H, McCabe N, Lord CJ, Tutt AN, Johnson DA, Richardson TB, et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature. 2005;434:917–21. doi: 10.1038/nature03445. [DOI] [PubMed] [Google Scholar]
- 6.McCabe N, Lord CJ, Tutt AN, Martin NM, Smith GC, Ashworth A. BRCA2-deficient CAPAN-1 cells are extremely sensitive to the inhibition of Poly (ADP-Ribose) polymerase: an issue of potency. Cancer Biol Ther. 2005;4:934–6. doi: 10.4161/cbt.4.9.2141. [DOI] [PubMed] [Google Scholar]
- 7.McCabe N, Turner NC, Lord CJ, Kluzek K, Bialkowska A, Swift S, et al. Deficiency in the repair of DNA damage by homologous recombination and sensitivity to poly(ADP-ribose) polymerase inhibition. Cancer Res. 2006;66:8109–15. doi: 10.1158/0008-5472.CAN-06-0140. [DOI] [PubMed] [Google Scholar]
- 8.Hakme A, Wong HK, Dantzer F, Schreiber V. The expanding field of poly(ADP-ribosyl)ation reactions. ‘Protein Modifications: Beyond the Usual Suspects’ Review Series. EMBO Rep. 2008;9:1094–100. doi: 10.1038/embor.2008.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aguilar-Quesada R, Munoz-Gamez JA, Martin-Oliva D, Peralta A, Valenzuela MT, Matinez-Romero R, et al. Interaction between ATM and PARP-1 in response to DNA damage and sensitization of ATM deficient cells through PARP inhibition. BMC Mol Biol. 2007;8:29. doi: 10.1186/1471-2199-8-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buisson R, Dion-Cote AM, Coulombe Y, Launay H, Cai H, Stasiak AZ, et al. Cooperation of breast cancer proteins PALB2 and piccolo BRCA2 in stimulating homologous recombination. Nat Struct Mol Biol. 2010;17:1247–54. doi: 10.1038/nsmb.1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rafnar T, Gudbjartsson DF, Sulem P, Jonasdottir A, Sigurdsson A, Jonasdottir A, et al. Mutations in BRIP1 confer high risk of ovarian cancer. Nature genetics. 2011;43:1104–7. doi: 10.1038/ng.955. [DOI] [PubMed] [Google Scholar]
- 12.Walsh T, Casadei S, Lee MK, Pennil CC, Nord AS, Thornton AM, et al. Mutations in 12 genes for inherited ovarian, fallopian tube, and peritoneal carcinoma identified by massively parallel sequencing. Proc Natl Acad Sci U S A. 2011;108:18032–7. doi: 10.1073/pnas.1115052108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaufman B, Shapira-Frommer R, Schmutzler RK, Audeh MW, Friedlander M, Balmana J, et al. Olaparib monotherapy in patients with advanced cancer and a germline BRCA1/2 mutation. J Clin Oncol. 2015;33:244–50. doi: 10.1200/JCO.2014.56.2728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim G, Ison G, McKee AE, Zhang H, Tang S, Gwise T, et al. FDA Approval Summary: Olaparib Monotherapy in Patients with Deleterious Germline BRCA-Mutated Advanced Ovarian Cancer Treated with Three or More Lines of Chemotherapy. Clin Cancer Res. 2015;21:4257–61. doi: 10.1158/1078-0432.CCR-15-0887. [DOI] [PubMed] [Google Scholar]
- 15.Pujade-Lauraine E, Ledermann JA, Selle F, Gebski V, Penson RT, Oza AM, et al. Olaparib tablets as maintenance therapy in patients with platinum-sensitive, relapsed ovarian cancer and a BRCA1/2 mutation (SOLO2/ENGOT-Ov21): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2017;18:1274–84. doi: 10.1016/S1470-2045(17)30469-2. [DOI] [PubMed] [Google Scholar]
- 16.Ledermann J, Harter P, Gourley C, Friedlander M, Vergote I, Rustin G, et al. Olaparib maintenance therapy in platinum-sensitive relapsed ovarian cancer. N Engl J Med. 2012;366:1382–92. doi: 10.1056/NEJMoa1105535. [DOI] [PubMed] [Google Scholar]
- 17.Ledermann JA, Harter P, Gourley C, Friedlander M, Vergote I, Rustin G, et al. Overall survival in patients with platinum-sensitive recurrent serous ovarian cancer receiving olaparib maintenance monotherapy: an updated analysis from a randomised, placebo-controlled, double-blind, phase 2 trial. Lancet Oncol. 2016;17:1579–89. doi: 10.1016/S1470-2045(16)30376-X. [DOI] [PubMed] [Google Scholar]
- 18.Kristeleit R, Shapiro GI, Burris HA, Oza AM, LoRusso P, Patel MR, et al. A Phase I-II Study of the Oral PARP Inhibitor Rucaparib in Patients with Germline BRCA1/2-Mutated Ovarian Carcinoma or Other Solid Tumors. Clin Cancer Res. 2017 doi: 10.1158/1078-0432.CCR-16-2796. [DOI] [PubMed] [Google Scholar]
- 19.Swisher EM, Lin KK, Oza AM, Scott CL, Giordano H, Sun J, et al. Rucaparib in relapsed, platinum-sensitive high-grade ovarian carcinoma (ARIEL2 Part 1): an international, multicentre, open-label, phase 2 trial. Lancet Oncol. 2017;18:75–87. doi: 10.1016/S1470-2045(16)30559-9. [DOI] [PubMed] [Google Scholar]
- 20.Coleman RL, Oza AM, Lorusso D, Aghajanian C, Oaknin A, Dean A, et al. Rucaparib maintenance treatment for recurrent ovarian carcinoma after response to platinum therapy (ARIEL3): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017 doi: 10.1016/S0140-6736(17)32440-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mirza MR, Monk BJ, Herrstedt J, Oza AM, Mahner S, Redondo A, et al. Niraparib Maintenance Therapy in Platinum-Sensitive, Recurrent Ovarian Cancer. N Engl J Med. 2016;375:2154–64. doi: 10.1056/NEJMoa1611310. [DOI] [PubMed] [Google Scholar]
- 22.Donawho CK, Luo Y, Luo Y, Penning TD, Bauch JL, Bouska JJ, et al. ABT-888, an orally active poly(ADP-ribose) polymerase inhibitor that potentiates DNA-damaging agents in preclinical tumor models. Clin Cancer Res. 2007;13:2728–37. doi: 10.1158/1078-0432.CCR-06-3039. [DOI] [PubMed] [Google Scholar]
- 23.Coleman RL, Sill MW, Bell-McGuinn K, Aghajanian C, Gray HJ, Tewari KS, et al. A phase II evaluation of the potent, highly selective PARP inhibitor veliparib in the treatment of persistent or recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer in patients who carry a germline BRCA1 or BRCA2 mutation - An NRG Oncology/Gynecologic Oncology Group study. Gynecol Oncol. 2015;137:386–91. doi: 10.1016/j.ygyno.2015.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reiss KA, Herman JM, Armstrong D, Zahurak M, Fyles A, Brade A, et al. A final report of a phase I study of veliparib (ABT-888) in combination with low-dose fractionated whole abdominal radiation therapy (LDFWAR) in patients with advanced solid malignancies and peritoneal carcinomatosis with a dose escalation in ovarian and fallopian tube cancers. Gynecol Oncol. 2017;144:486–90. doi: 10.1016/j.ygyno.2017.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Geyer CE, O’Shaughnessy J, Untch M, Sikov W, Hope RSMDM, et al. Phase 3 study evaluating efficacy and safety of veliparib (V) plus carboplatin (Cb) or Cb in combination with standard neoadjuvant chemotherapy (NAC) in patients (pts) with early stage triple-negative breast cancer (TNBC) J Clin Oncol. 2017;35 (suppl; abstr 520)2017. [Google Scholar]
- 26.Shen Y, Rehman FL, Feng Y, Boshuizen J, Bajrami I, Elliott R, et al. BMN 673, a novel and highly potent PARP1/2 inhibitor for the treatment of human cancers with DNA repair deficiency. Clin Cancer Res. 2013;19:5003–15. doi: 10.1158/1078-0432.CCR-13-1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de Bono J, Ramanathan RK, Mina L, Chugh R, Glaspy J, Rafii S, et al. Phase I, Dose-Escalation, Two-Part Trial of the PARP Inhibitor Talazoparib in Patients with Advanced Germline BRCA1/2 Mutations and Selected Sporadic Cancers. Cancer discovery. 2017;7:620–9. doi: 10.1158/2159-8290.CD-16-1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ledermann J, Harter P, Gourley C, Friedlander M, Vergote I, Rustin G, et al. Olaparib maintenance therapy in patients with platinum-sensitive relapsed serous ovarian cancer: a preplanned retrospective analysis of outcomes by BRCA status in a randomised phase 2 trial. Lancet Oncol. 2014;15:852–61. doi: 10.1016/S1470-2045(14)70228-1. [DOI] [PubMed] [Google Scholar]
- 29.Domchek SM, Aghajanian C, Shapira-Frommer R, Schmutzler RK, Audeh MW, Friedlander M, et al. Efficacy and safety of olaparib monotherapy in germline BRCA1/2 mutation carriers with advanced ovarian cancer and three or more lines of prior therapy. Gynecol Oncol. 2016;140:199–203. doi: 10.1016/j.ygyno.2015.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Frey MK, Pothuri B. Homologous recombination deficiency (HRD) testing in ovarian cancer clinical practice: a review of the literature. Gynecol Oncol Res Pract. 2017;4:4. doi: 10.1186/s40661-017-0039-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Watkins JA, Irshad S, Grigoriadis A, Tutt AN. Genomic scars as biomarkers of homologous recombination deficiency and drug response in breast and ovarian cancers. Breast Cancer Res. 2014;16:211. doi: 10.1186/bcr3670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sander Effron S, Makvandi M, Lin L, Xu K, Li S, Lee H, et al. PARP-1 Expression Quantified by [18F]FluorThanatrace: A Biomarker of Response to PARP Inhibition Adjuvant to Radiation Therapy. Cancer Biother Radiopharm. 2017;32:9–15. doi: 10.1089/cbr.2016.2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wysham WZ, Mhawech-Fauceglia P, Li H, Hays L, Syriac S, Skrepnik T, et al. BRCAness profile of sporadic ovarian cancer predicts disease recurrence. PloS one. 2012;7:e30042. doi: 10.1371/journal.pone.0030042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hjortkjaer M, Waldstrom M, Jakobsen A, Kanstrup H, Sogaard-Andersen E, Dahl Steffensen K. The Prognostic Value of BRCA1 and PARP Expression in Epithelial Ovarian Carcinoma: Immunohistochemical Detection. International journal of gynecological pathology : official journal of the International Society of Gynecological Pathologists. 2017;36:180–9. doi: 10.1097/PGP.0000000000000310. [DOI] [PubMed] [Google Scholar]
- 35.Makvandi M, Xu K, Lieberman BP, Anderson RC, Effron SS, Winters HD, et al. A Radiotracer Strategy to Quantify PARP-1 Expression In Vivo Provides a Biomarker That Can Enable Patient Selection for PARP Inhibitor Therapy. Cancer Res. 2016;76:4516–24. doi: 10.1158/0008-5472.CAN-16-0416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ameziane N, May P, Haitjema A, van de Vrugt HJ, van Rossum-Fikkert SE, Ristic D, et al. A novel Fanconi anaemia subtype associated with a dominant-negative mutation in RAD51. Nature communications. 2015;6:8829. doi: 10.1038/ncomms9829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barber LJ, Sandhu S, Chen L, Campbell J, Kozarewa I, Fenwick K, et al. Secondary mutations in BRCA2 associated with clinical resistance to a PARP inhibitor. The Journal of pathology. 2013;229:422–9. doi: 10.1002/path.4140. [DOI] [PubMed] [Google Scholar]
- 38.Norquist B, Wurz KA, Pennil CC, Garcia R, Gross J, Sakai W, et al. Secondary somatic mutations restoring BRCA1/2 predict chemotherapy resistance in hereditary ovarian carcinomas. J Clin Oncol. 2011;29:3008–15. doi: 10.1200/JCO.2010.34.2980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chang HHY, Pannunzio NR, Adachi N, Lieber MR. Non-homologous DNA end joining and alternative pathways to double-strand break repair. Nat Rev Mol Cell Biol. 2017 doi: 10.1038/nrm.2017.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bunting SF, Callen E, Wong N, Chen HT, Polato F, Gunn A, et al. 53BP1 inhibits homologous recombination in Brca1-deficient cells by blocking resection of DNA breaks. Cell. 2010;141:243–54. doi: 10.1016/j.cell.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bouwman P, Aly A, Escandell JM, Pieterse M, Bartkova J, van der Gulden H, et al. 53BP1 loss rescues BRCA1 deficiency and is associated with triple-negative and BRCA-mutated breast cancers. Nat Struct Mol Biol. 2010;17:688–95. doi: 10.1038/nsmb.1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Panier S, Boulton SJ. Double-strand break repair: 53BP1 comes into focus. Nat Rev Mol Cell Biol. 2014;15:7–18. doi: 10.1038/nrm3719. [DOI] [PubMed] [Google Scholar]
- 43.Johnson N, Johnson SF, Yao W, Li YC, Choi YE, Bernhardy AJ, et al. Stabilization of mutant BRCA1 protein confers PARP inhibitor and platinum resistance. Proc Natl Acad Sci U S A. 2013;110:17041–6. doi: 10.1073/pnas.1305170110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sugimura K, Takebayashi S, Taguchi H, Takeda S, Okumura K. PARP-1 ensures regulation of replication fork progression by homologous recombination on damaged DNA. J Cell Biol. 2008;183:1203–12. doi: 10.1083/jcb.200806068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ray Chaudhuri A, Callen E, Ding X, Gogola E, Duarte AA, Lee JE, et al. Replication fork stability confers chemoresistance in BRCA-deficient cells. Nature. 2016;535:382–7. doi: 10.1038/nature18325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Avemann K, Knippers R, Koller T, Sogo JM. Camptothecin, a specific inhibitor of type I DNA topoisomerase, induces DNA breakage at replication forks. Mol Cell Biol. 1988;8:3026–34. doi: 10.1128/mcb.8.8.3026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Patel AG, Flatten KS, Schneider PA, Dai NT, McDonald JS, Poirier GG, et al. Enhanced killing of cancer cells by poly(ADP-ribose) polymerase inhibitors and topoisomerase I inhibitors reflects poisoning of both enzymes. J Biol Chem. 2012;287:4198–210. doi: 10.1074/jbc.M111.296475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Znojek P, Willmore E, Curtin NJ. Preferential potentiation of topoisomerase I poison cytotoxicity by PARP inhibition in S phase. Br J Cancer. 2014;111:1319–26. doi: 10.1038/bjc.2014.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Samol J, Ranson M, Scott E, Macpherson E, Carmichael J, Thomas A, et al. Safety and tolerability of the poly(ADP-ribose) polymerase (PARP) inhibitor, olaparib (AZD2281) in combination with topotecan for the treatment of patients with advanced solid tumors: a phase I study. Invest New Drugs. 2012;30:1493–500. doi: 10.1007/s10637-011-9682-9. [DOI] [PubMed] [Google Scholar]
- 50.Bajrami I, Frankum JR, Konde A, Miller RE, Rehman FL, Brough R, et al. Genome-wide profiling of genetic synthetic lethality identifies CDK12 as a novel determinant of PARP1/2 inhibitor sensitivity. Cancer Res. 2014;74:287–97. doi: 10.1158/0008-5472.CAN-13-2541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Blazek D, Kohoutek J, Bartholomeeusen K, Johansen E, Hulinkova P, Luo Z, et al. The Cyclin K/Cdk12 complex maintains genomic stability via regulation of expression of DNA damage response genes. Genes Dev. 2011;25:2158–72. doi: 10.1101/gad.16962311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Johnson SF, Cruz C, Greifenberg AK, Dust S, Stover DG, Chi D, et al. CDK12 Inhibition Reverses De Novo and Acquired PARP Inhibitor Resistance in BRCA Wild-Type and Mutated Models of Triple-Negative Breast Cancer. Cell reports. 2016;17:2367–81. doi: 10.1016/j.celrep.2016.10.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Alagpulinsa DA, Ayyadevara S, Yaccoby S, Shmookler Reis RJ. A Cyclin-Dependent Kinase Inhibitor, Dinaciclib, Impairs Homologous Recombination and Sensitizes Multiple Myeloma Cells to PARP Inhibition. Mol Cancer Ther. 2016;15:241–50. doi: 10.1158/1535-7163.MCT-15-0660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Garcia TB, Snedeker JC, Baturin D, Gardner L, Fosmire SP, Zhou C, et al. A small molecule inhibitor of WEE1, AZD1775, synergizes with olaparib by impairing homologous recombination and enhancing DNA damage and apoptosis in acute leukemia. Mol Cancer Ther. 2017 doi: 10.1158/1535-7163.MCT-16-0660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Karnak D, Engelke CG, Parsels LA, Kausar T, Wei D, Robertson JR, et al. Combined inhibition of Wee1 and PARP1/2 for radiosensitization in pancreatic cancer. Clin Cancer Res. 2014;20:5085–96. doi: 10.1158/1078-0432.CCR-14-1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Do K, Wilsker D, Ji J, Zlott J, Freshwater T, Kinders RJ, et al. Phase I Study of Single-Agent AZD1775 (MK-1775), a Wee1 Kinase Inhibitor, in Patients With Refractory Solid Tumors. J Clin Oncol. 2015;33:3409–15. doi: 10.1200/JCO.2014.60.4009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Teng PN, Bateman NW, Darcy KM, Hamilton CA, Maxwell GL, Bakkenist CJ, et al. Pharmacologic inhibition of ATR and ATM offers clinically important distinctions to enhancing platinum or radiation response in ovarian, endometrial, and cervical cancer cells. Gynecol Oncol. 2015;136:554–61. doi: 10.1016/j.ygyno.2014.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rottenberg S, Jaspers JE, Kersbergen A, van der Burg E, Nygren AO, Zander SA, et al. High sensitivity of BRCA1-deficient mammary tumors to the PARP inhibitor AZD2281 alone and in combination with platinum drugs. Proc Natl Acad Sci U S A. 2008;105:17079–84. doi: 10.1073/pnas.0806092105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Callaghan R, Luk F, Bebawy M. Inhibition of the multidrug resistance P-glycoprotein: time for a change of strategy? Drug Metab Dispos. 2014;42:623–31. doi: 10.1124/dmd.113.056176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Du Y, Yamaguchi H, Wei Y, Hsu JL, Wang HL, Hsu YH, et al. Blocking c-Met-mediated PARP1 phosphorylation enhances anti-tumor effects of PARP inhibitors. Nat Med. 2016;22:194–201. doi: 10.1038/nm.4032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tapodi A, Debreceni B, Hanto K, Bognar Z, Wittmann I, Gallyas F, Jr, et al. Pivotal role of Akt activation in mitochondrial protection and cell survival by poly(ADP-ribose)polymerase-1 inhibition in oxidative stress. J Biol Chem. 2005;280:35767–75. doi: 10.1074/jbc.M507075200. [DOI] [PubMed] [Google Scholar]
- 62.Veres B, Gallyas F, Jr, Varbiro G, Berente Z, Osz E, Szekeres G, et al. Decrease of the inflammatory response and induction of the Akt/protein kinase B pathway by poly-(ADP-ribose) polymerase 1 inhibitor in endotoxin-induced septic shock. Biochem Pharmacol. 2003;65:1373–82. doi: 10.1016/s0006-2952(03)00077-7. [DOI] [PubMed] [Google Scholar]
- 63.Veres B, Radnai B, Gallyas F, Jr, Varbiro G, Berente Z, Osz E, et al. Regulation of kinase cascades and transcription factors by a poly(ADP-ribose) polymerase-1 inhibitor, 4-hydroxyquinazoline, in lipopolysaccharide-induced inflammation in mice. The Journal of pharmacology and experimental therapeutics. 2004;310:247–55. doi: 10.1124/jpet.104.065151. [DOI] [PubMed] [Google Scholar]
- 64.Neijenhuis S, Bajrami I, Miller R, Lord CJ, Ashworth A. Identification of miRNA modulators to PARP inhibitor response. DNA Repair (Amst) 2013;12:394–402. doi: 10.1016/j.dnarep.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 65.Choi YE, Meghani K, Brault ME, Leclerc L, He YJ, Day TA, et al. Platinum and PARP Inhibitor Resistance Due to Overexpression of MicroRNA-622 in BRCA1-Mutant Ovarian Cancer. Cell reports. 2016;14:429–39. doi: 10.1016/j.celrep.2015.12.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Moskwa P, Buffa FM, Pan Y, Panchakshari R, Gottipati P, Muschel RJ, et al. miR-182-mediated downregulation of BRCA1 impacts DNA repair and sensitivity to PARP inhibitors. Mol Cell. 2011;41:210–20. doi: 10.1016/j.molcel.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Antolin AA, Mestres J. Linking off-target kinase pharmacology to the differential cellular effects observed among PARP inhibitors. Oncotarget. 2014;5:3023–8. doi: 10.18632/oncotarget.1814. [DOI] [PMC free article] [PubMed] [Google Scholar]