Abstract
Adrenal trauma is rarely encountered in the pediatric population, often as a component of multi-organ injury and often presenting with hematoma formation. Contrast-enhanced computed tomography (CECT) is the established imaging modality both for initial evaluation and follow-up of patients with blunt abdominal trauma. In children, radiation exposure should be minimized and alternative imaging strategies are needed. Contrast-enhanced ultrasound (CEUS) has recently been successfully used for evaluation of patients with hepatic, renal and splenic injury. We present three cases of children with post-traumatic adrenal hematomas, which were initially diagnosed with CECT and subsequently followed up with CEUS, suggesting that CEUS may be considered for follow-up of adrenal injuries in children. CEUS improves the diagnostic capabilities by increasing tissue contrast and spatial resolution, readily differentiating viable from necrotic tissue in comparison to conventional ultrasound without the risk of iodine contrast agents and ionizing radiation of repeated CECT examinations.
Keywords: Adrenal, Trauma, Ultrasound, Microbubbles, Pediatric
Sommario
Il trauma dei surreni accade raramente nella popolazione pediatrica, spesso è parte di un poli-trauma e spesso si presenta normalmente sotto forma di ematoma. La tomografia computerizzata con contrasto (TAC) è stabilita come modalità di diagnostica per immagini per la valutazione iniziale e il follow-up di pazienti con trauma addominale chiuso. Nei bambini e’ necessario ridurre al minimo l’esposizione alle radiazioni ionizzanti, pertanto sono necessarie strategie d’immagine alternative. L’ecografia con mezzo di contrasto (CEUS) e’ stata usata recentemente con successo nella valutazione di pazienti con lesioni traumatiche epatiche, renali e spleniche. Presentiamo tre casi di bambini con ematomi surrenali post-traumatici, inizialmente diagnosticati con tomografia computerizzata con contrasto (TAC) e successivamente esaminati al follow-up con ecografia con contrasto (CEUS), e suggeriamo che la CEUS può essere considerata per il follow-up delle lesioni traumatiche dei surreni nei bambini. La CEUS migliora le capacità diagnostiche aumentando contrasto tissutale e la risoluzione spaziale, differenziando prontamente il tessuto vitale da quello necrotico rispetto all’ecografia convenzionale, senza il rischio inerente ai mezzi di contrasto iodati e alle radiazioni ionizzanti legate a ripetuti esami con TAC con contrasto.
Introduction
Adrenal gland trauma is rare in children and usually affects the right adrenal gland as a part of multi-organ trauma involving the liver and right kidney [1]. Careful follow-up and monitoring of these patients is essential as blood transfusion to compensate hemorrhage may be required. Prognosis is favorable and rarely is surgery required unless there is active bleeding [1]. Imaging plays a key role in accurate evaluation of such injuries with contrast-enhanced computed tomography (CECT) considered the best tool both for initial grading and follow-up [2]. In the pediatric population, radiation exposure is a major consideration and it is essential to limit the number of computed tomography (CT) examinations [3]. Any radiation-free alternative to CT in children would thus be desirable. Ultrasound (US) has been shown to be effective for following up children with adrenal trauma [4]. The technique of contrast-enhanced ultrasound (CEUS) is a valuable complementary technique to conventional US in many clinical scenarios, with formal guidelines on many applications available [5]. Abdominal trauma investigation is an important application of CEUS, with many studies having evaluated its accuracy in hepatic, renal and splenic injuries in adults [6–9] and to a lesser extent in children [10, 11]. In addition to its effectiveness, CEUS has been shown to be a safe imaging technique both for adults [12] and children [13] with only very limited adverse reactions reported [12–14].
In the present case series, we highlight the potential use of CEUS in the follow-up of pediatric patients with adrenal injuries. We describe three cases of adrenal hematoma initially diagnosed with CECT but followed up with CEUS and present images illustrating the value of CEUS in the investigation of adrenal trauma.
Case 1
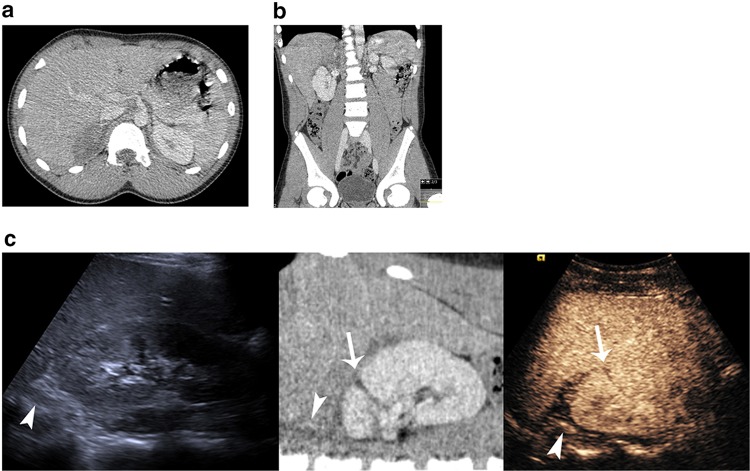
A 13-year-old boy was admitted to the emergency department after sustaining a handle bar cycling accident. On presentation, the child was hemodynamically stable but complained of pain in the right lateral abdominal region. No superficial bruising was visible at the site of symptoms. A few hours after admission, with worsening pain and signs of abdominal “guarding” on clinical examination, an abdominal CT was performed, revealing the presence of free fluid in “Morrison’s” pouch. A small laceration was seen in the upper pole of the right kidney extending to a subcapsular hematoma (Grade 2). In addition, a right adrenal hematoma was identified, with a normally enhancing underlying adrenal gland (Fig. 1a, b). The child was managed conservatively. Two days later, with stable clinical signs, CEUS was performed to evaluate the right kidney and adrenal gland. The examination was performed on a Siemens Acuson S3000 (Siemens Acuson, Mountain View, CA) with a curvilinear 6C1 transducer. For the contrast-enhanced aspect, a low mechanical index mode (Cadence Contrast Pulse Sequencing, CPS™ Siemens, Mountain View, CA) was used, in keeping with previous CEUS examination techniques in children [15–17], and 2.4 mL of SonoVue™ (Bracco, Milan) was administered. A small amount of free fluid was visible surrounding the upper pole of the right kidney. The ipsilateral adrenal gland was readily identified and demonstrated normal enhancement. The previous CECT-observed hematoma was confirmed surrounding the adrenal gland and had reduced in size. There was also evidence of size reduction of the renal laceration (Fig. 1c). The child had an uneventful recovery and was discharged 4 days after admission, remaining well on subsequent follow-up.
Fig. 1.
A 13-year-old boy with renal laceration and adrenal hematoma. Axial CT image a demonstrates a rounded hypodense lesion displacing the right adrenal gland. Coronal reformatted image b demonstrates the relation of the hematoma to the right kidney, liver and adrenal gland. A composite image c correlating US (left), CT (middle) and CEUS (right). The adrenal gland (arrowheads) can be seen hypoechoic with US and normally enhancing with CT and CEUS. The hematoma is identified surrounding the adrenal gland. It is readily identified on CT as hypodense material and is more prominent on CEUS where it is avascular distinct to adjacent normal enhancing tissues. The kidney laceration (arrow) is visible on CT and CEUS but less prominent on US
Case 2
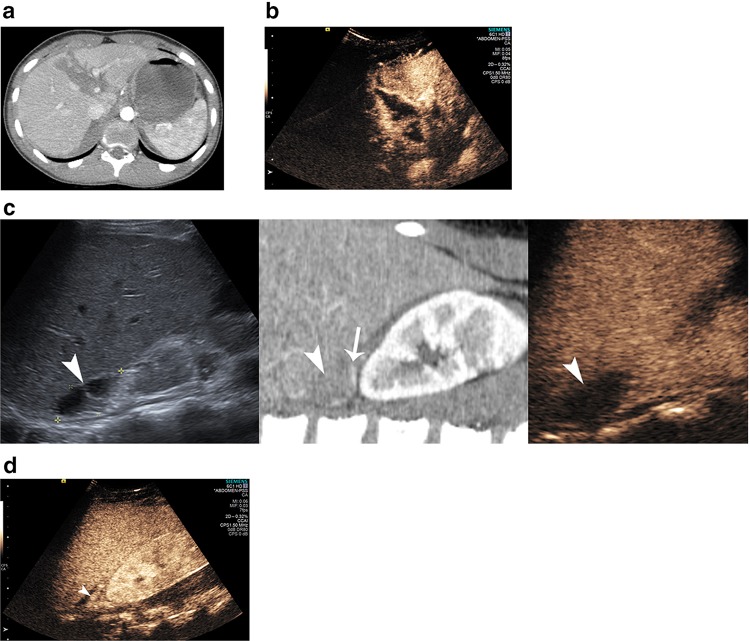
A 15-year-old boy attended the emergency department after falling from a motorbike. The child was hemodynamically stable but with severe abdominal pain. Contrast-enhanced CT demonstrated a liver fracture involving segments I, IVA and IVB measuring approximately 8 cm in length (Grade 4) with no contrast extravasation. A vertical hypodense and poorly enhancing area was identified in the neck of the pancreas representing a pancreatic transection. A laceration was detected in the upper pole of the right kidney and an adrenal hematoma (4 × 3 cm) displaced the normally enhancing adrenal gland inferiorly (Fig. 2a). The child was managed conservatively and 1 week following admission, a CEUS examination was performed using an identical technique as in the previous case. On CEUS, the hepatic lacerations were identified extending to the porta hepatis. The adrenal gland enhanced normally, with the hematoma identified, with no internal enhancement (4 × 2 cm) displacing the kidney inferiorly (Fig. 2b, c, d). The child had an uneventful recovery and a second CEUS examination was performed prior to discharge revealing overall improvement of the injuries, also confirmed on a repeat CECT essentially performed to evaluate the pancreatic fracture. The liver laceration and the adrenal gland hematoma (3 × 1 cm) were reduced in size, whilst the pancreatic neck fracture also showed improvement. The right kidney laceration was no longer visible on conventional US nor on CEUS. The child was discharged and has made a full recovery.
Fig. 2.
A 15-year-old boy with hepatic laceration, transection of the pancreatic neck and adrenal hematoma. Axial CT a shows the hypodense laceration affecting segments I, IVA and IVB. The corresponding CEUS image b readily demonstrates the non-enhancing laceration. A composite image c correlating US (left), CT (middle) and CEUS (right). The adrenal hematoma (arrowhead) appears anechoic on US, hypodense on CT and non-enhancing hypoechoic on CEUS. The inferiorly displaced adrenal gland can be identified on CT (arrow). A different plane on CEUS demonstrating the normal enhancing displaced adrenal gland (arrowhead)
Case 3
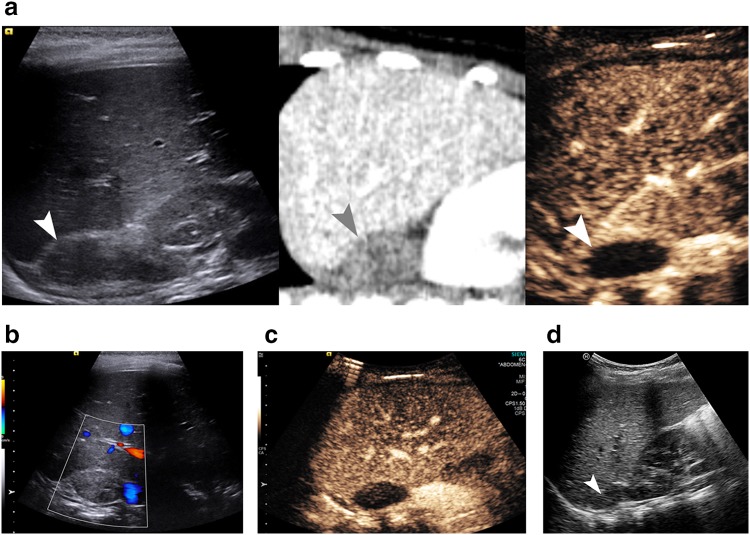
A 2-year-old girl presented to the emergency department after being hit by a car. The child underwent a CECT which revealed a frontal skull fracture with subdural hematoma, consolidation of the left lower lung and a right lung parenchyma contusion. The abdominal CECT examination demonstrated no solid viscera injury. There was an ovoid hypo-attenuating lesion in the right suprarenal fossa (2.4 × 1.5 cm), with no associated fat stranding, likely representing an adrenal hematoma. A conventional US and a CEUS examination was performed (identical technique to the previous cases, except dose of SonoVue™ was 0.6 mLs) 2 days later to evaluate the adrenal lesion, which appeared uniformly isoechoic to the liver parenchyma and avascular on color Doppler US. The adrenal lesion showed no immediate or delayed vascular enhancement, with artifact of ‘shine-through’ noted. [18] (Fig. 3a, b, c). On a second conventional US 1 week later, the lesion had decreased in size and the diagnosis of a resolving adrenal hematoma was established (Fig. 3d). The child made an uneventful recovery and was discharged, remaining well at follow-up.
Fig. 3.
A 2-year-old girl with adrenal hematoma identified after traffic accident. A composite image a correlating US (left), CT (middle) and CEUS (right). The adrenal hematoma (arrowhead) appears isoechoic on US, hypodense on CT and non-enhancing hypoechoic on CEUS. On color Doppler b the lesion was avascular. Following administration of microbubble contrast, the lesion showed no marked immediate a or delayed c enhancement. Note was made of the ‘shine-through’ artifact. Follow-up ultrasound 1 week later d demonstrating the decrease in size of the mass (arrowhead)
Discussion
Adrenal gland injury in blunt abdominal trauma is rare, estimated at 7 % in adults and found less frequently in children estimated at an incidence between 0.22 and 4 % [1, 4]. Common causes of adrenal injury include falls and motor vehicle or bicycle accidents, the precipitating cause in all our cases [2]. Adrenal gland trauma is rarely isolated, usually associated with liver, ipsilateral kidney or lower chest traumatic lesions [1, 4, 19]. In this case series, we have presented three children with multi-organ trauma which included an adrenal gland hematoma. Initial diagnosis was made by CECT but follow-up was performed using a combination of CEUS and CECT. Contrast-enhanced ultrasound proved to be a useful complementary technique to conventional US, providing increased spatial resolution and readily differentiating vascularized from non-vascularized tissue. CEUS thus provided physicians with increased confidence regarding management of these children negating the use of CT and the potential uncertainty of an isolated conventional US follow-up.
The microbubble contrast dose recommended depends on the organ under examination, with adult patients normally requiring 2.4 mL of SonoVue™ for the liver and 1.2 mL for the kidney and spleen, with dose adjustment in children. Our practice is to adapt the dose to the child’s age; a liver dose of 0.6 mL for children <6 years, 1.2 mL aged between 6 and 12 years and 2.4 mL > 12 years [20]. After administration of microbubbles, solid organs show enhancement in a dynamic pattern similar to that observed in CT and magnetic resonance (MR) imaging while the useful scanning time is approximately 3 min [15–17].
Imaging trauma patients is essential for prompt and accurate diagnosis. A focal assessment with sonography for trauma (FAST scan) examination in the emergency department often represents the first-line modality in trauma to evaluate for the presence of free intraabdominal fluid. A FAST scan is able to detect ≥250 ml of fluid but is inconsistent with solid organ injuries [2]; a FAST scan without the presence of free fluid in the abdomen may falsely reassure the physician to solid organ injury integrity [6, 21] and is no longer recommended as an appropriate imaging modality in pediatric abdominal trauma. A CECT examination is the ideal modality to evaluate multi-organ trauma patients, both adults and children, and is able to delineate adrenal gland injuries, with the typical findings of rounded hematomas causing enlargement or displacement of the adrenal gland, or features of hemorrhage [2]. Often the adrenal gland may have indistinct margins, with the impression of an underlying preexisting lesion. CECT will differentiate adrenal hemorrhage which evolves over time reducing in size, in contrast to a primary lesion of the adrenal gland [19, 22, 23]. This involves repeat exposure to ionizing radiation, particularly important to avoid in children [24, 25].
The appearance of traumatic injuries on US is dependent on their nature. In general, traumatic injuries appear as readily discernible, well or ill-defined hypoechoic areas in the organ under examination. Likewise, a hematoma is normally hypoechoic unless an underlying hemorrhagic pseudocyst is present, a recognized complication of adrenal trauma [6, 14]. This may have equivocal imaging findings on CECT and US but CEUS will clearly demonstrate the avascular nature of the lesion, by showing the lack of enhancement [26]. Microbubble contrast also enables the detection of abnormalities which are not visible on conventional US like infarcts, pseudo aneurysms and the microbubble contrast extravasation of active bleeding [14].
The truly intravascular properties of the microbubbles allow for a greater diagnostic confidence in the investigation of solid organ injury and we have demonstrated the ability to extend this to the evaluation of adrenal gland injury. There was concordance with CECT imaging, and with adrenal gland injuries, CEUS may substitute CECT in the follow-up of these children. The potential and desirable benefit of CEUS over conventional US in this situation is clear; a truly intravascular agent that clearly depicts vascularity of a lesion or absence (hematoma), which is repeatable, safe and accurate [3, 5]. It has been calculated that medical imaging radiation-induced cancer affects one in 500 children [25]. CEUS is gaining acceptance for pediatric investigations, primarily in an effort to reduce ionizing radiation and iodinated contrast exposure. CEUS has been shown to be safe in adults and when used in children adverse reactions are rare, [13] rendering CEUS acceptable even if the intravenous use in children remains off-label [13, 27]. We have used CEUS to successfully monitor hematoma resolution in three children with blunt abdominal trauma although conventional US alone has been used successfully and confidently monitored hematoma resolution over 3 months following trauma [4].
The added value of CEUS includes improved visualization of tissues characterized by increased tissue contrast and spatial resolution along with real-time dynamic evaluation of the perfusion pattern of organs. The incorporation of CEUS in the follow-up of adrenal gland injuries increased the diagnostic confidence of both the US practitioner and the treating physicians allowing for safe patient discharge following conservative treatment. This factor along with avoidance of CT-induced radiation highlights the advantages of CEUS patient follow-up, prompting use in these cases. A normal adrenal gland may be difficult to locate with US, but normally can be readily identified when enlarged and surrounded by a hematoma, and more clearly with CEUS. On follow-up US, an adrenal gland hematoma should alter from a rounded and isoechoic area (compared to the surrounding hyperechoic fat) gradually becoming hypo- or anechoic [28, 29]. An alternative imaging strategy for following up children with adrenal injuries should involve US with the addition of CEUS.
Contrast-enhanced ultrasound is feasible for the evaluation of adult adrenal glands but is of limited value in differentiating benign from malignant adrenal masses, albeit with good correlation with CT and MR imaging [17, 30]. A single case report of the evaluation of an adrenal phaeochromocytoma using CEUS in a child reported the usefulness of the technique [17]. In adult abdominal trauma, the value of CEUS has been shown to increase diagnostic accuracy compared to conventional US in the assessment of liver, renal and spleen injuries, [6, 7, 31] with the diagnostic accuracy of CEUS not significantly inferior compared to the gold standard CECT [8, 9]. False-negative results were attributed to minor injuries with no clinical significance and no influence on patient management. As such, the use of CEUS is advocated for initial diagnostic evaluation of abdominal trauma patients [6]. Valentino et al. evaluated the diagnostic accuracy of US and CEUS with CECT as the reference standard in children with blunt abdominal trauma. Similar to findings in adults, CEUS was superior to US and nearly as accurate as CECT in identifying solid organ traumatic lesions [10]. With the efficacy of CEUS demonstrated in blunt abdominal trauma, the European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) published guidelines recommending the use of CEUS instead of CECT in hemodynamically stable patients with limited moderate-energy blunt abdominal trauma to exclude solid organ injuries. Moreover, CEUS is recommended for evaluation of inconclusive CECT findings and follow-up of patients managed conservatively, primarily to reduce repeated CT examinations, as was our practice with the patients described in this case series [9, 14, 31].
Conclusion
Adrenal gland trauma is uncommon and usually part of a multi-organ trauma. US and especially CT are well-established techniques for the initial evaluation of such patients. Follow-up with repeated CECT examinations is a reliable strategy but carries the burden of radiation which is unacceptable for the pediatric population. CEUS is an emerging ultrasonographic technique which adequately evaluates adrenal injuries and potentially offers an alternative to CECT, especially for follow-up.
Compliance with ethical standards
Conflict of interest
Author AD has received lecture fees from Bracoo company. Author MES has received lecture fees from Bracco company. Author PSS has received lecture fees from Siemens, Hitachi, GE, Bracco companies.
Ethical approval
For this type of study formal consent is not required.
Human and animal studies
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Gabal-Shehab L, Alagiri M. Traumatic adrenal injuries. J Urol. 2005;173:1330–1331. doi: 10.1097/01.ju.0000155459.11926.61. [DOI] [PubMed] [Google Scholar]
- 2.Lee YS, Jeong JJ, Nam KH, et al. Adrenal injury following blunt abdominal trauma. World J Surg. 2010;34:1971–1974. doi: 10.1007/s00268-010-0537-x. [DOI] [PubMed] [Google Scholar]
- 3.Leung RS. Radiation protection of the child from diagnostic imaging. Curr Pediatr Rev. 2015;11:235–242. doi: 10.2174/1573396311666150729121930. [DOI] [PubMed] [Google Scholar]
- 4.Soundappan SV, Lam AH, Cass DT. Traumatic adrenal haemorrhage in children. ANZ J Surg. 2006;76:729–731. doi: 10.1111/j.1445-2197.2006.03842.x. [DOI] [PubMed] [Google Scholar]
- 5.Claudon M, Dietrich CF, Choi BI, et al. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver–update 2012: a WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultraschall Med. 2013;34:11–29. doi: 10.1055/s-0032-1325499. [DOI] [PubMed] [Google Scholar]
- 6.Catalano O, Aiani L, Barozzi L, et al. CEUS in abdominal trauma: multi-center study. Abdom Imaging. 2009;34:225–234. doi: 10.1007/s00261-008-9452-0. [DOI] [PubMed] [Google Scholar]
- 7.Valentino M, Ansaloni L, Catena F, et al. Contrast-enhanced ultrasonography in blunt abdominal trauma: considerations after 5 years of experience. Radiol Med. 2009;114:1080–1093. doi: 10.1007/s11547-009-0444-0. [DOI] [PubMed] [Google Scholar]
- 8.Valentino M, De Luca C, Galloni SS, et al. Contrast-enhanced US evaluation in patients with blunt abdominal trauma. J Ultrasound. 2010;13:22–27. doi: 10.1016/j.jus.2010.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Valentino M, Serra C, Zironi G, et al. Blunt abdominal trauma: emergency contrast-enhanced sonography for detection of solid organ injuries. AJR Am J Roentgenol. 2006;186:1361–1367. doi: 10.2214/AJR.05.0027. [DOI] [PubMed] [Google Scholar]
- 10.Valentino M, Serra C, Pavlica P, et al. Blunt abdominal trauma: diagnostic performance of contrast-enhanced US in children-initial experience. Radiology. 2008;246:903–909. doi: 10.1148/radiol.2463070652. [DOI] [PubMed] [Google Scholar]
- 11.Durkin N, Deganello A, Sellars ME, et al. Post-traumatic liver and splenic pseudoaneurysms in children: diagnosis, management, and follow-up screening using contrast enhanced ultrasound (CEUS) J Pediatr Surg. 2015;51:289–292. doi: 10.1016/j.jpedsurg.2015.10.074. [DOI] [PubMed] [Google Scholar]
- 12.Piscaglia F, Bolondi L, Italian Society for Ultrasound in M et al (2006) The safety of Sonovue in abdominal applications: retrospective analysis of 23188 investigations. Ultrasound Med Biol 32:1369–1375. doi:10.1016/j.ultrasmedbio.2006.05.031 [DOI] [PubMed]
- 13.Rosado E, Riccabona M. Off-label use of ultrasound contrast agents for intravenous applications in children: analysis of the existing literature. J Ultrasound Med. 2016;35:487–496. doi: 10.7863/ultra.15.02030. [DOI] [PubMed] [Google Scholar]
- 14.Piscaglia F, Nolsoe C, Dietrich CF, et al. The EFSUMB guidelines and recommendations on the clinical practice of contrast enhanced ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med. 2012;33:33–59. doi: 10.1055/s-0031-1281676. [DOI] [PubMed] [Google Scholar]
- 15.Jacob J, Deganello A, Sellars ME, et al. Contrast enhanced ultrasound (CEUS) characterization of grey-scale sonographic indeterminate focal liver lesions in pediatric practice. Ultraschall Med. 2013;34:529–540. doi: 10.1055/s-0033-1355785. [DOI] [PubMed] [Google Scholar]
- 16.Yusuf GT, Sellars ME, Huang DY, et al. Cortical necrosis secondary to trauma in a child: contrast-enhanced ultrasound comparable to magnetic resonance imaging. Ped Radiol. 2014;44:484–487. doi: 10.1007/s00247-013-2818-7. [DOI] [PubMed] [Google Scholar]
- 17.Al Bunni F, Deganello A, Sellars ME, et al. Contrast-enhanced ultrasound (CEUS) appearances of an adrenal phaeochromocytoma in a child with Von Hippel-Lindau disease. J Ultrasound. 2014;17:307–311. doi: 10.1007/s40477-014-0083-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dietrich CF, Ignee A, Hocke M, et al. Pitfalls and artefacts using contrast enhanced ultrasound. Z Gastroenterol. 2011;49:350–356. doi: 10.1055/s-0029-1245851. [DOI] [PubMed] [Google Scholar]
- 19.Daly KP, Ho CP, Persson DL, et al. Traumatic retroperitoneal injuries: review of multidetector CT findings. Radiographics. 2008;28:1571–1590. doi: 10.1148/rg.286075141. [DOI] [PubMed] [Google Scholar]
- 20.Sidhu PS, Cantisani V, Deganello A, Dietrich CF, Duran C, Franke D et al (2016) Role of contrast-enhanced ultrasound (CEUS) in paediatric practice: an EFSUMB position statement. Ultraschall Med Jul 14 [Epub ahead of print]. doi: 10.1055/s-0042-110394 [DOI] [PubMed]
- 21.Skerritt CHS, Makin E. Focused assessment with sonography in trauma (FAST) scans are not sufficiently sensitive to rule out significant injury in pediatric trauma patients. Open J Pediatr. 2014;4:236–242. doi: 10.4236/ojped.2014.43031. [DOI] [Google Scholar]
- 22.Johnson PT, Horton KM, Fishman EK. Adrenal imaging with MDCT: nonneoplastic disease. AJR Am J Roentgenol. 2009;193:1128–1135. doi: 10.2214/AJR.09.2551. [DOI] [PubMed] [Google Scholar]
- 23.Rana AI, Kenney PJ, Lockhart ME, et al. Adrenal gland hematomas in trauma patients. Radiology. 2004;230:669–675. doi: 10.1148/radiol.2303021345. [DOI] [PubMed] [Google Scholar]
- 24.Claudon M, Guillaume L. Diagnostic imaging and radiation hazards. Rev Prat. 2015;65:79–81. [PubMed] [Google Scholar]
- 25.Brenner D, Elliston C, Hall E, et al. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol. 2001;176:289–296. doi: 10.2214/ajr.176.2.1760289. [DOI] [PubMed] [Google Scholar]
- 26.Cantisani V, Petramala L, Ricci P, et al. A giant hemorragic adrenal pseudocyst: contrast-enhanced examination (CEUS) and computed tomography (CT) features. Eur Rev Med Pharmacol Sci. 2013;17:2546–2550. [PubMed] [Google Scholar]
- 27.Darge K, Papadopoulou F, Ntoulia A, et al. Safety of contrast-enhanced ultrasound in children for non-cardiac applications: a review by the Society for Pediatric Radiology (SPR) and the International Contrast Ultrasound Society (ICUS) Pediatr Radiol. 2013;43:1063–1073. doi: 10.1007/s00247-013-2746-6. [DOI] [PubMed] [Google Scholar]
- 28.Knorr M, Evans D. Bedside ultrasound of acute adrenal hemorrhage. Am J Emerg Med. 2012;30(2088):e2081–e2082. doi: 10.1016/j.ajem.2011.12.025. [DOI] [PubMed] [Google Scholar]
- 29.Huang YC, Lee WJ, Lin HJ, et al. Isolated post-traumatic adrenal hematoma: detection by bedside ultrasound in the Emergency Department. J Emerg Med. 2012;42:e17–e18. doi: 10.1016/j.jemermed.2009.08.052. [DOI] [PubMed] [Google Scholar]
- 30.Friedrich-Rust M, Glasemann T, Polta A, et al. Differentiation between benign and malignant adrenal mass using contrast-enhanced ultrasound. Ultraschall Med. 2011;32:460–471. doi: 10.1055/s-0031-1273408. [DOI] [PubMed] [Google Scholar]
- 31.Cokkinos D, Antypa E, Stefanidis K, et al. Contrast-enhanced ultrasound for imaging blunt abdominal trauma: indications, description of the technique and imaging review. Ultraschall Med. 2012;33:60–67. doi: 10.1055/s-0031-1273442. [DOI] [PubMed] [Google Scholar]