Abstract
Background
Many hospitalized adults do not have the capacity to make their own health care decisions and thus require a surrogate decision-maker. While the ethical standard suggests that decisions should focus on a patient’s preferences, our study explores the principles that surrogates consider most important when making decisions for older hospitalized patients.
Objectives
We sought to determine how frequently surrogate decision-makers prioritized patient preferences in decision-making and what factors may predict their doing so.
Design and Participants
We performed a secondary data analysis of a study conducted at three local hospitals that surveyed surrogate decision-makers for hospitalized patients 65 years of age and older.
Main Measures
Surrogates rated the importance of 16 decision-making principles and selected the one that was most important. We divided the surrogates into two groups: those who prioritized patient preferences and those who prioritized patient well-being. We analyzed the two groups for differences in knowledge of patient preferences, presence of advance directives, and psychological outcomes.
Key Results
A total of 362 surrogates rated an average of six principles as being extremely important in decision-making; 77.8% of surrogates selected a patient well-being principle as the most important, whereas only 21.1% selected a patient preferences principle. Advance directives were more common to the patient preferences group than the patient well-being group (61.3% vs. 44.9%; 95% CI: 1.01–3.18; p = 0.04), whereas having conversations with the patient about their health care preferences was not a significant predictor of surrogate group identity (81.3% vs. 67.4%; 95% CI: 0.39–1.14; p = 0.14). We found no differences between the two groups regarding surrogate anxiety, depression, or decisional conflict.
Conclusions
While surrogates considered many factors, they focused more often on patient well-being than on patient preferences, in contravention of our current ethical framework. Surrogates more commonly prioritized patient preferences if they had advance directives available to them.
KEY WORDS: medical decision-making, patient preferences, ethics, aging, doctor–patient relationships
INTRODUCTION
Surrogate decision-makers are vital to medical decision-making for nearly half of hospitalized older adults and up to 95% of patients in the intensive care unit (ICU), whose own decisional capacities may be compromised by delirium, dementia, or critical illness.1 – 3 Largely guided by a report from the President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research in 1983, it is now widely accepted that after a patient has lost decision-making capacity, surrogates ought to make decisions in accordance with the patients’ preferences as a means to honor the ethical principle of respect for patient autonomy.4 , 5 According to the framework, surrogate decision-makers should fulfill their role by first considering evidence available to them about patient preferences, such as that found in advance directives or prior written statements, and then by making a substituted judgment regarding those preferences.6 If these preferences are unknown, they should act upon the ethical principle of beneficence by making decisions in order to maximize patient well-being; known as the best-interest standard.7 Thus, the current ethical model for surrogate decision-making is patient-centric, and first prioritizes substituted judgment so that decisions are made according to patient preferences.8
Many, however, are skeptical of the adequacy of this ethical framework for reaching decisions based upon patient preferences. Advance directives, for example, have been unsuccessful in achieving this goal.9 , 10 Tasking surrogates to decide according to substituted judgment, while admirable in principle, may be impossible to achieve pragmatically, as deciding according to patient preferences may be guesswork at best.11 – 13
Furthermore, in spite of this accepted ethical framework, it is not clear whether surrogate decision-makers actually prioritize patient preferences over patient well-being. A study of predominantly white female surrogate decision-makers for chronically ill veterans found that 36% of surrogates planned to base their decisions on more than one factor.14 Our prior qualitative analysis of 35 surrogate interviews highlighted important surrogate-centric factors, such as a wish for family consensus, that were considered in addition to the patients’ preferences.15 While these studies provide insight into the complexities of surrogate decision-making, it is still unclear how surrogates may value a patient’s preferences when having to make decisions on their behalf.
To better characterize surrogates’ perspectives, we surveyed the surrogate decision-makers of older inpatients at three hospitals in order to identify the principles they deemed most important when making actual decisions. We hypothesized that surrogates would more commonly prioritize patient preferences than patient well-being as their guiding principles. We also hypothesized that surrogates who prioritized patient preferences would be more likely to report having patient advance directives and conversations with the patient about health care preferences to guide their decision-making than those who prioritized patient well-being. Lastly, we predicted that surrogates who prioritized well-being would experience more distress throughout the decision-making process, and that this would have a negative effect on their anxiety, depression, and decisional conflict when compared to surrogates who invoked patient preferences.
METHODS
Design
We performed a secondary data analysis of a multi-hospital study of surrogate-decision makers for incapacitated hospitalized elderly patients.16 The study was conducted between April 2012 and July 2015 on the inpatient general medicine and medical ICUs of a county hospital, a tertiary referral center, and a community hospital, all affiliated with Indiana University. Research assistants screened patients for enrollment by real-time monitoring of the electronic medical record for general medicine and ICU admissions.
Participants
Hospitalized patients aged 65 years and older were eligible for enrollment if at least one decision was made by a surrogate-decision maker; decisions were defined a priori as addressing either life-prolonging treatments, procedures requiring informed consent, or post-discharge placement. The primary inpatient physician for each patient was contacted by a research assistant to determine whether they had consulted with a surrogate for any of the predefined decisions. These surrogates were then approached to give informed consent for review of the patient’s medical record as well as their own participation for the purposes of the study.
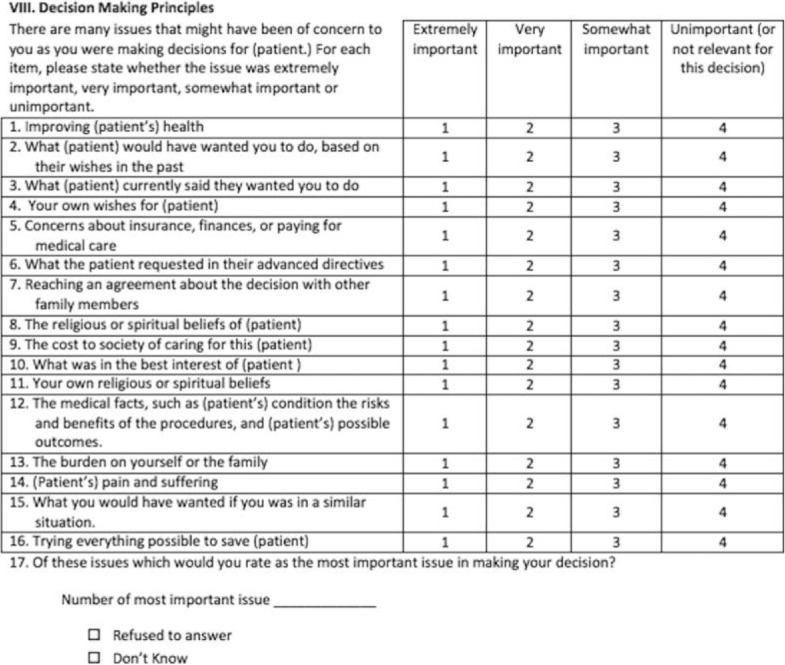
Data Collection
Demographic and medical information for enrolled patients was obtained from the electronic medical record and the identified surrogate decision-maker. Upon enrollment of the patient/surrogate dyads, the surrogates completed an initial interview, where their demographic information was obtained (Table 1). During this interview, surrogates were asked about the specific decisions they made regarding maintaining or withdrawing life-sustaining treatment, giving informed consent for procedures, and post-discharge placement, as defined by the study’s inclusion criteria. Surrogates who had made more than three of these types of decisions were asked about which three decisions were the most difficult. Then, based on those specific decisions, the surrogates were asked to rate the importance of 16 decision-making principles, previously derived from the literature and prior qualitative interviews.15 Finally, the surrogates were asked to select which of the 16 principles was the most important to them when they made those decisions.
Table 1.
Surrogates and Patient Demographics
| Surrogate | Patient | |
|---|---|---|
| No. (%) or mean (SD) | No. (%) or mean (SD) | |
| Age (years) | 58.26 (11.26) | 81.78 (8.3) |
| Female | 256 (70.7) | 223 (61.6) |
| Race | ||
| White | 249 (68.8) | 250 (69.1) |
| Black | 103 (28.5) | 101 (27.9) |
| Asian | 2 (0.6) | 3 (0.8) |
| American Indian | 1 (0.3) | 1 (0.3) |
| Multiple | 6 (1.7) | 7 (1.9) |
| Refused | 1 (0.3) | 0 (0) |
| Hispanic | 3 (0.8) | 3 (0.8) |
| Marital status | ||
| Married | 238 (65.8) | 116 (32.0) |
| Single | 52 (14.4) | 15 (4.1) |
| Divorced | 59 (16.3) | 53 (14.6) |
| Widowed | 9 (2.5) | 173 (47.8) |
| Unmarried partner | 4 (1.1) | 5 (1.4) |
| Education | ||
| < GED | 22 (6.1) | 102 (29.1) |
| GED | 236 (65.6) | 191 (54.6) |
| BS/BA | 67 (18.1) | 30 (8.6) |
| MS/MA+ | 35 (9.7) | 27 (7.7) |
| Relationship to patient | ||
| Child | 241 (66.6) | – |
| Spouse | 61 (16.9) | – |
| Unmarried partner | 1 (0.3) | – |
| Child in-law | 10 (2.8) | – |
| Grandchild | 9 (2.5) | – |
| Neighbor or friend | 2 (0.6) | – |
| Other | 38 (10.5) | – |
| Illness severity | – | |
| CIRS* | – | 24.40 (6.0) |
| Admitted to ICU | – | 90 (25.8) |
SD = standard deviation
*CIRS = Cumulative Illness Rating Scale30
The enrollment interview also included questions asking the surrogates whether the patient had advance directives and questions about their communication with the patient regarding health care preferences, as well as the Generalized Anxiety Disorder 7 (GAD7), Patient Health Questionnaire 9 (PHQ-9), and Decisional Conflict Scale (DCS) questionnaires17 – 19 to measure the surrogates’ anxiety, depression, and decisional conflict, respectively. A research assistant conducted follow-up interviews with the surrogates 6 to 8 weeks after the patient’s discharge from the hospital to re-administer the GAD7 and PHQ-9.
Surrogates rated each of the 16 principles as “extremely important,” “very important,” “somewhat important,” or “unimportant” to their decision-making processes. The surrogates also chose what they considered to be the single most important principle in their decision-making. Based upon this choice, we categorized the surrogates into two groups: those who prioritized principles reflecting advance directives and substituted judgment were assigned to the patient preferences group, and those who prioritized principles reflecting the best-interest standard were assigned to the patient well-being group (see Table 2 for the decision-making principles in each group). We chose to refer to this as the “patient well-being” group rather than the “best-interest” group, because one of the principles in this group included the term “best interest.” However, for the purposes of this discussion, what we refer to as “patient well-being” is synonymous with the best-interest standard of surrogate decision-making.
Table 2.
Importance of Patient Well-Being and Patient Preferences Principles
| Group | Decision-making principle | Ranked most important, no. (%) | Rated “extremely important,” no. (%) |
|---|---|---|---|
| Patient well-being | (Patient’s) pain and suffering | 76 (20.99) | 244 (67.40) |
| What was in the best interests of (patient) | 67 (18.51) | 239 (66.02) | |
| Improving (patient’s) health | 68 (18.78) | 240 (66.30) | |
| Trying everything possible to save (patient) | 52 (14.36) | 168 (46.41) | |
| The medical facts, such as (patient’s) condition, the risks and benefits of the procedures, and (patient’s) possible outcomes | 13 (3.59) | 213 (58.84) | |
| Patient preferences | What (patient) would have wanted you to do, based upon their wishes in the past | 44 (12.15) | 198 (54.70) |
| What the patient requested in their advance directives | 15 (4.14) | 113 (31.22) | |
| What (patient) currently said they wanted you to do | 9 (2.49) | 96 (26.52) | |
| The religious or spiritual beliefs of (patient) | 7 (1.93) | 104 (28.73) |
The remaining uncategorized principles were “Reaching an agreement about the decision with other family members,” “Your own wishes for the patient,” “What you would have wanted if you were in a similar situation,” “Concerns about insurance, finances, or paying for medical care,” “The cost to society of caring for this patient,” “Your own religious or spiritual beliefs,” and “The burden on yourself or the family.” As only four (1%) surrogates in total rated one of these uncategorized principles as the most important, they were excluded from this part of the analysis.
Data Analysis
For each participant, a summation score was created to indicate the number of principles they considered to be “extremely important.”
In order to examine differences between the patient preferences and patient well-being groups, we performed bivariate analyses using chi-square tests for categorical variables and Student’s t-tests for continuous variables. In addition, we re-examined these relationships using logistic regression to adjust for patient and surrogate demographics. Predictive variables of interest included whether the patient had an advance directive, whether the surrogate had spoken with the patient about their preferences regarding medical care, and the surrogate’s anxiety, depression, and decisional conflict by their respective scores on the Generalized Anxiety Disorder 7 (GAD7), Patient Health Questionnaire 9 (PHQ-9), and Decisional Conflict Scale (DCS) tests.17 – 19
Analyses were performed using SAS version 9.4 software (SAS Institute, Cary, NC). All analytic assumptions were verified, with the Kruskal-Wallis non-parametric test performed in place of Student’s t-test when data were skewed.
The Indiana University Institutional Review Board approved the study. Surrogate informed consent was obtained for all participants upon enrollment, because patients were unable to make decisions.
RESULTS
Participant Characteristics
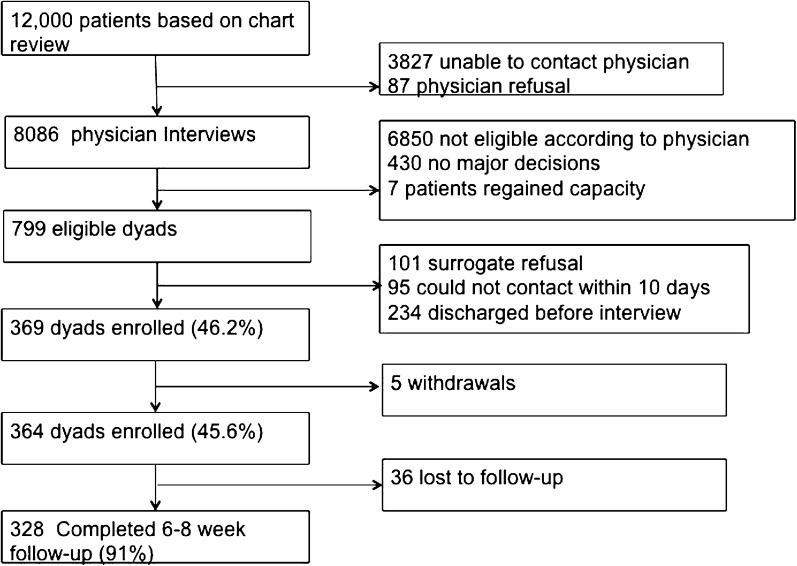
Of 799 eligible patient/surrogate dyads, 364 (46.2%) were enrolled (Fig. 1), among which 362 (99%) completed the initial decision-making principles survey. Seven surrogates were unable to answer the question as to which principle was the most important (three responded that all were important, two that none of them were important, one could not choose between two of the items, and one chose not to answer the question). Patients were mostly white and had a high school or higher level of education. Their surrogates were usually daughters and also tended to be educated at the high school level or higher (Table 1).
Figure 1.
Enrollment flow of patient/surrogate dyads in the original Communication in the Hospital: Impact on Patients and Surrogates study.
Surrogate Prioritization of Patients’ Preferences
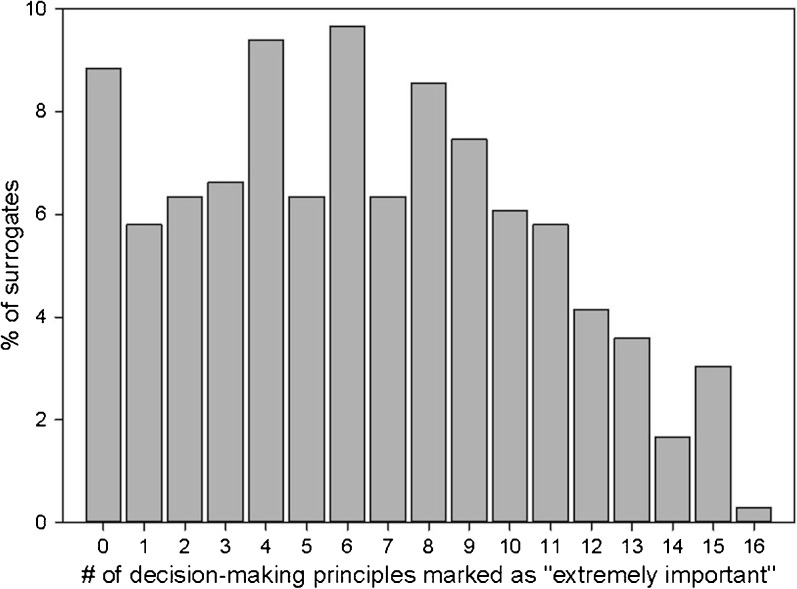
Surrogate decision-makers rated an average of six decision-making principles as extremely important (range 0–16; Fig. 2). The four principles most often chosen as most important in decision-making were 1) avoiding pain and suffering, 2) best interests, 3) improving the patient’s health, and 4) trying everything possible to save the patient, all of which are patient well-being principles.
Figure 2.
The number of decision-making principles considered by surrogates to be “extremely important.” Surrogates rated a mean of six principles as “extremely important” in their decision-making. The right skew of the histogram indicates that surrogates consider a greater number of factors as important when having to make decisions.
Patient preferences and patient well-being
Seventy-five (21.1%) surrogates prioritized principles emphasizing patient preferences, while 276 (77.8%) prioritized principles emphasizing the patient's well-being (Table 2). The remaining four (1.1%) prioritized principles that did not fit either group and were excluded from the analysis.
Characteristics of patients and their surrogates, including demographics and illness severity, were similar between the patient preferences and patient well-being groups. Table 3 summarizes the unadjusted bivariate analyses comparing the two groups. Although surrogates in the patient preferences group were more likely to have had conversations with patients about their health care preferences than surrogates in the patient well-being group (81.3% vs. 67.4%), after adjusting for patient and surrogate factors (age, race, sex, education, relationship), this difference was not statistically significant (95% CI: 0.39–1.14; p = 0.14). However, remaining statistically significant after adjustment, surrogates in the patient preferences group were more often provided with documentation of patients' treatment preferences (advance directives) than surrogates in the patient well-being group (61.3% vs. 44.9%; 95% CI: 1.01–3.18; p = 0.04), and were also more likely to have found those documents helpful (91.3% vs. 66.1%; 95% CI: 1.05–4.29; p = 0.04).
Table 3.
Unadjusted Bivariate Analyses Comparing the Patient Preferences and Patient Well-Being Groups
| Variable | Patient preferences | Patient well-being | p |
|---|---|---|---|
| n (%) or mean (SD) | n (%) or mean (SD) | ||
| Knowledge of the patient’s preferences | |||
| Surrogate had conversation with the patient about health care wishes | 61 (81.3) | 186 (67.4) | 0.02 |
| Living will present | 46 (61.3) | 124 (44.9) | 0.04 |
| Surrogate found living will to be helpful | 42 (91.3) | 82 (66.1) | 0.02 |
| Emotional distress scores | |||
| GAD7 Anxiety (enrollment) | 3.7 (4.8) | 4.4 (5.0) | 0.28 |
| GAD7 Anxiety (follow-up) | 2.6 (4.1) | 3.2 (4.7) | 0.28 |
| PHQ-9 Depression (enrollment) | 4.1 (4.3) | 4.9 (5.4) | 0.21 |
| PHQ-9 Depression (follow-up) | 2.9 (4.5) | 4.0 (5.3) | 0.12 |
| DCS Decisional Conflict | 19.3 (14.5) | 22.3 (14.8) | 0.13 |
SD = standard deviation
There were no differences between groups in the surrogates’ mean levels of anxiety, depression, or decisional conflict, as measured by GAD7, PHQ-9, and DCS, respectively (Table 3).
DISCUSSION
Our study of surrogate decision-makers for hospitalized older adults revealed that surrogates consider many factors to be important in making decisions for incapacitated patients; surrogates rated an average of six different factors as “extremely important.” Additionally, while we have previously described many surrogate-centered factors that may be important in surrogate decision-making,15 the present results suggest that nearly all of the principles that surrogates value the most are patient-centered and relate to the standard ethical guiding principles of autonomy and best interests. Contrary to our hypothesis, however, we discovered that most surrogates prioritized patient well-being over patient preferences, as evidenced by the four factors that were most often rated as the most important. The overwhelming dominance of patient well-being principles among our cohort of surrogates is striking, as this contrasts with the primary autonomy-based ethical standard of surrogate decision-making.7
These results further suggest that the guidelines for decision-making in accordance with patients’ preferences may be inadequately applied in practice. Rather than relying on patients’ preferences for guidance, physicians have been shown to emphasize the best-interest standard in clinical decision-making. A prior study revealed that only a third of physicians, who endorsed patient preferences as the most appropriate ethical principle in surrogate decision-making, also rated patient preferences as most important to their actual decisions.20 Our results also challenge the application of substituted judgment, by showing that surrogates, too, rely on patient preferences only a minority of the time to guide their decision-making. Therefore, despite its place in the standard ethical model of surrogate decision-making, neither party involved in making decisions for incapacitated patients seems to be deferring to substituted judgment in practice in the way prescribed by the standard model.
It remains unclear why the surrogate decision-makers in our study frequently deviated from patient preferences as guiding principles. Surrogates in the patient preferences group more often had conversations with the patient about health care preferences than surrogates in the patient well-being group. This relationship, however, did not reach statistical significance. Our data also demonstrate that the presence and helpfulness of advance directives is associated with prioritizing patient preferences principles. This reflects the notion that the more certainty a surrogate has about a patient’s preferences, the more capable they feel in advocating for those preferences.21
On the other hand, despite having received guidance from advance directives or conversations with the patient, many of the enrolled surrogates still prioritized patient well-being over patient preferences. Critical analyses of the standard model for surrogate decision-making already describe advance directives and substituted judgment as impractical, inadequate, and inaccurate.9 – 13 , 21 Perhaps surrogates still lack sufficient empowerment, motivation, or instruction from clinicians to utilize substituted judgment, or perhaps substituted judgment is just a poor fit for the reality of surrogate decision-making. Further insight into the forces that sway surrogate decision-makers away from patient preferences is needed so that we may more appropriately analyze whether these deviations are ethically permissible, or whether we must adjust our approach to help surrogates refocus on patient preferences.
Finally, prior work has revealed that knowledge of the patient’s preferences reduced the emotional burden of making treatment decisions for others.21 , 22 However, in our analysis, focusing on these preferences was not associated with lower anxiety, depression, or decisional conflict for surrogates.
Our study has several limitations that subject our data to wide interpretation. First, our results are not generalizable. Most of the surrogate decision-makers were white, educated women, and while we asked them to rate the importance of each decision-making principle in their overall decision-making during the patient’s hospital stay, we are not able to determine to what extent they actually followed those principles when making decisions. Additionally, the surrogates almost certainly experienced a range of influences and guidance throughout the patients’ hospitalizations, and it is not known how those experiences shaped the way each surrogate later rated the decision-making principles. Thus our data are challenging to interpret, making our results more hypothesis-generating than conclusive.
Second, dividing our cohort of surrogates into patient preferences and patient well-being groups may be an artificial dichotomization. While other works have also delineated a basic social process of decision-making,23 , 24 the surrogates in our study rated many factors as extremely important, and thus the binary distinction we made likely oversimplifies their decision-making process. There may have been significant overlap between the patient’s preferences and their well-being. For example, if a patient had expressed avoidance of suffering as an explicit goal, his or her surrogate decision-maker may have chosen “avoiding pain and suffering” as the most important decision-making principle. Although we would categorize this as a patient well-being principle, it represents an expression of the patient’s preference. In this regard, we know little about the clarity and relevance of the conversations that patients may have had with their surrogate decision-makers and the potential effects on their responses to our questionnaire.
Lastly, our cohort of surrogates averaged low rates of emotional distress, making it difficult for our results to firmly contradict prior work noting an association between knowledge of patient preferences and decreased emotional burden.
Overall, our study reveals that surrogate decision-makers consider many factors when making decisions for incapacitated patients, and often decide based upon the patients’ best interests (what we have referred to as well-being) rather than the patients’ preferences. While our data are subject to interpretation, if our findings are reproducible, it may be appropriate to re-examine the recommendation to give priority to patient self-determination over best interest. Perhaps it is ethically permissible for surrogate decision-makers to have the authority to decide upon what is best for the patient, even if it conflicts with the patient's preferences.6 Patients have expressed an understanding of the burden their surrogates face,25 and many prefer shared decision-making between surrogates and physicians, sometimes at the expense of their own preferences.26 , 27 Additionally, preferences can change over time, and some patients do not wish to be involved in their own decision-making at all.28 , 29 Thus alternative shared decision-making frameworks such as “substituted interests”13 and “patient life story”12 may be ethically preferred over substituted judgments based on prior stated preferences. These models recommend decision-making according to the concept of authenticity,4 where decisions are made by eliciting a patient’s values history, ensuring respect for persons even if the decision made may be contradictory to the patient's actual preferences.
Further work is needed to expand our study of surrogate decision-making principles to a broader cohort of patients and surrogates in order to confirm that the best-interest standard is often invoked over available advance directives and substituted judgments. Subsequently, empirical investigation into why surrogates are making decisions in contravention of our current ethical framework may reveal other factors that are influencing their decision-making processes. Finally, normative analyses may allow us to examine the discrepancy between our ethical theory and our empirical findings. Such examination may determine whether this represents an inadequacy in the model itself or reveals a need to change our approach in order to better adhere to the current ethical framework of surrogate decision-making.
Conclusions
In conclusion, we found that surrogate decision-makers for older hospitalized adults consider many patient-centered principles when making decisions. Contrary to our hypothesis, they prioritize patient well-being principles over patient preferences principles, but this distinction is not associated with a difference in emotional burden. These findings suggest a discrepancy between the normative ethical framework of surrogate decision-making and the descriptive reality of how it is actually being carried out. Alternative models of surrogate decision-making may mitigate this disparity by employing a value-based approach over a strict prioritization of patient preferences. However, further investigation is needed to determine whether these alternative models should become the ethical norm, or whether other factors must be targeted to improve decision-making according to our current patient preferences-based standard.
Acknowledgements
Author contributions: R.D. and A.M.T. participated in study concept and design. L.I., K.M., and E.S.B. participated in data acquisition. J.E.S. participated in statistical analysis of data. R.D., A.M.T., J.E.S., and G.T.B. participated in data analysis and interpretation. R.D., A.M.T., J.E.S., G.T.B, L.I., K.M., and E.S.B. participated in manuscript preparation, drafting, reviewing, and editing. All authors approve of the submitted manuscript.
Appendix 1: Decision-Making Principles Survey Tool for Surrogate Decision-Makers Used in the Communication in the Hospital: Impact on Patients and Surrogates Study
Appendix 2
Table 4
Table 4.
Unadjusted bivariate analyses comparing the Patient preferences and Patient well-being groups. Data taken from surrogate enrollment and follow-up surveys, as well as physician enrollment survey. Values are frequency (percentage) for categorical variables and mean (standard deviation) for continuous variables. P-values are from chi-Square tests for categorical variables and the omnibus ANOVA test for continuous variables
| Variable | Patient preferences (n = 75) | Patient well-being (n = 272) | p |
|---|---|---|---|
| Patient female | 41 (54.7) | 174 (64.0) | 0.14 |
| Patient white | 54 (72.0) | 185 (68.0) | 0.46 |
| Surrogate relationship | |||
| Spouse | 13 (17.3) | 45 (16.5) | 0.90 |
| Son/Daughter | 48 (64.0) | 185 (68.0) | |
| Child-in-law | 2 (2.7) | 6 (2.2) | |
| Grandchild | 3 (4.0) | 6 (2.2) | |
| Neighbor/Friend | 1 (1.3) | 1 (0.4) | |
| Other | 8 (10.7) | 28 (10.3) | |
| Patient marital status | |||
| Married | 27 (36.0) | 84 (30.9) | 0.42 |
| Single | 1 (1.3) | 13 (4.8) | |
| Divorced | 13 (17.3) | 40 (14.7) | |
| Widowed | 34 (45.3) | 130 (47.8) | |
| Patient education | |||
| < GED | 28 (38.4) | 71 (27.0) | 0.27 |
| GED (no BS/BA) | 34 (46.6) | 150 (57.0) | |
| BS/BA | 5 (6.9) | 23 (8.8) | |
| MS/MA+ | 6 (8.2) | 19 (7.2) | |
| Surrogate female | 50 (66.7) | 194 (71.3) | 0.43 |
| Surrogate white | 53 (70.7) | 185 (68.0) | 0.50 |
| Surrogate marital status | |||
| Married | 56 (74.7) | 173 (63.6) | 0.44 |
| Single | 7 (9.3) | 44 (16.2) | |
| Divorced | 10 (13.3) | 45 (16.5) | |
| Widowed | 1 (1.3) | 7 (2.6) | |
| With opposite sex partner | 1 (1.3) | 3 (1.1) | |
| Surrogate education | |||
| < GED | 2 (2.7) | 19 (7.0) | 0.46 |
| GED (no BS/BA) | 51 (68.0) | 173 (64.1) | |
| BS/BA | 16 (21.3) | 50 (18.5) | |
| MS/MA+ | 6 (8.0) | 28 (10.4) | |
| Patient lives with you | 23 (30.7) | 96 (35.3) | 0.45 |
| Would you define yourself as a caregiver for the patient? | 42 (79.3) | 163 (76.9) | 0.71 |
| Before this event, had you been involved as a family member of a patient in the hospital? | 70 (93.3) | 239 (87.9) | 0.18 |
| Were you involved in decision-making for that patient? | 55 (78.6) | 188 (78.7) | 1.00 |
| Have you ever had experience caring for a dying family member? | 38 (50.7) | 123 (45.2) | 0.74 |
| Were you involved in decision-making for that family member? | 27 (71.1) | 86 (69.9) | 0.89 |
| Was patient’s hospitalization unexpected? | 60 (80.0) | 205 (75.4) | 0.58 |
| Is this the first time the patient has been admitted with this health issue? | 45 (60.0) | 156 (57.6) | 0.81 |
| Do you feel you are the primary decision-maker for the patient? | 61 (81.3) | 216 (79.4) | 0.73 |
| Conflict with patient | |||
| No conflict | 51 (68.0) | 183 (67.3) | 0.56 |
| Some conflict | 20 (26.7) | 81 (29.8) | |
| High conflict | 4 (5.3) | 8 (2.9) | |
| In the past, has patient discussed wishes about medical care with anyone? | 63 (84.0) | 190 (69.9) | 0.05 |
| Has patient discussed these with you? | 61 (96.8) | 182 (95.8) | 0.71 |
| Has patient discussed with family doctor? | 29 (46.0) | 57 (30.0) | 0.07 |
| Has patient discussed with hospital doctor? | 14 (22.2) | 25 (13.2) | 0.21 |
| Has patient discussed with anyone else? | 11 (17.5) | 18 (9.5) | 0.23 |
| How helpful were those wishes during this hospital stay? | |||
| Not helpful at all | 8 (12.7) | 26 (13.7) | 0.06 |
| Somewhat helpful | 10 (15.9) | 56 (29.5) | |
| Very helpful | 45 (71.4) | 103 (54.2) | |
| Was there a living will? | 46 (61.3) | 124 (45.6) | 0.05 |
| How helpful was the living will? | |||
| Not helpful at all | 4 (8.7) | 33 (26.6) | 0.02* |
| Somewhat helpful | 13 (28.3) | 26 (21.0) | |
| Very helpful | 29 (63.0) | 56 (45.2) | |
| Is there a power of attorney? | 64 (85.3) | 210 (77.2) | 0.27 |
| Full code? | 24 (32.0) | 116 (42.7) | 0.02* |
| Preferred course of treatment | |||
| Life-extending | 8 (10.7) | 45 (16.5) | 0.05 |
| Comfort care | 36 (48.0) | 87 (32.0) | |
| In-between | 31 (41.3) | 134 (49.3) | |
| How do you like to make decisions? | |||
| I make final selection of treatment | 6 (8.0) | 8 (2.9) | 0.04* |
| I make selection after seriously considering doctor input | 38 (58.7) | 102 (37.5) | |
| Share responsibility with doctor | 26 (34.7) | 131 (48.2) | |
| Doctor makes decision after seriously considering my input | 4 (5.3) | 23 (8.5) | |
| Doctor makes all decisions | 1 (1.3) | 8 (2.9) | |
| Agreement/Disagreement/Conflict composite score | 17.1 (3.1) | 16.9 (2.7) | 0.55 |
| PHQ Depression (enrollment) | 4.1 (4.3) | 4.9 (5.3) | 0.22 |
| PHQ Depression (follow-up) | 3.9 (4.5) | 4.0 (5.3) | 0.12 |
| GAD Anxiety (enrollment) | 3.7 (4.8) | 4.4 (5.0) | 0.31 |
| GAD Anxiety (follow-up) | 2.6 (4.1) | 3.2 (4.7) | 0.28 |
| K6 Total | 2.3 (2.8) | 2.7 (3.2) | 0.28 |
| Physician – are you aware of patient’s wishes about future care? | |||
| No | 35 (46.7) | 153 (56.7) | 0.12 |
| Yes | 40 (53.3) | 117 (43.3) | |
| Physician – how helpful have those wishes been in making decisions? | |||
| Very helpful | 26 (65.0) | 62 (53.0) | 0.38 |
| Somewhat helpful | 11 (27.5) | 40 (34.2) | |
| Not helpful at all | 3 (7.5) | 15 (12.8) | |
| Physician – at this time, the best course of treatment would be… | |||
| Extending life | 12 (16.0) | 53 (19.6) | 0.78 |
| Relieving pain | 27 (36.0) | 93 (34.4) | |
| In-between | 36 (48.0) | 124 (45.9) | |
| Physician – the current course of treatment is… | |||
| Extending life | 15 (20.0) | 73 (27.0) | 0.46 |
| Relieving pain | 13 (17.3) | 41 (15.2) | |
| In-between | 47 (62.7) | 156 (57.8) | |
| Physician– Moral distress | 9.56 (1.88) | 9.70 (2.00) | 0.60 |
| Surrogate Distrust Scale | 23.29 (5.42) | 22.38 (6.13) | 0.24 |
| Surrogate Decisional Conflict at enrollment (max) | 19.34 (14.51) | 22.50 (14.71) | 0.11 |
| Surrogate IES (6–8-week follow-up) | 6.89 (12.11) | 10.49 (14.95) | 0.06 |
| Surrogate IES (6-month follow-up) | 7.08 (11.98) | 7.53 (12.52) | 0.82 |
| Surrogate IES change (6 months – 6 weeks) | 0.55 (14.49) | −1.14 (9.68) | 0.37 |
| Patient CIRS (illness severity) | 23.47 (5.69) | 24.77 (6.08) | 0.10 |
| Surrogate anxiety with GAD ≥10 at enrollment | 9 (12.0) | 40 (14.8) | 0.54 |
| Surrogate anxiety with PHQ ≥ 10 at enrollment | 7 (9.3) | 39 (14.4) | 0.25 |
*Indicates a statistically significant p-value
Appendix 3
Table 5
Table 5.
Unadjusted bivariate analyses comparing surrogate emotional distress in the Patient preferences and Patient well-being groups for a subset of data where the patients died within 6 months of enrollment (n = 149). Values are frequency (percentage) for categorical variables and mean (standard deviation) for continuous variables. P-values are from chi-Square tests for categorical variables and the omnibus ANOVA test for continuous variables
| Emotional distress variable | Patient preferences group (n = 31) | Patient well-being group (n = 106) | p |
|---|---|---|---|
| Agreement/Disagreement/Conflict composite score | 17.06 (3.30) | 17.29 (2.67) | 0.70 |
| PHQ Depression (enrollment) | 4.48 (4.77) | 5.02 (5.58) | 0.63 |
| PHQ Depression (follow-up) | 4.45 (5.28) | 5.65 (6.11) | 0.34 |
| GAD Anxiety (enrollment) | 4.00 (4.29) | 4.71 (5.27) | 0.50 |
| GAD Anxiety (follow-up) | 3.93 (4.57) | 3.87 (4.94) | 0.95 |
| K6 Total | 3.19 (3.38) | 2.98 (3.29) | 0.75 |
| Surrogate Distrust Scale | 24.16 (5.77) | 21.61 (6.08) | 0.04* |
| Surrogate Decisional Conflict at enrollment (max) | 18.50 (14.43) | 21.00 (14.50) | 0.40 |
| IES (6–8-week follow-up) | 9.34 (14.61) | 14.96 (18.52) | 0.13 |
| IES (6-month follow-up) | 9.40 (12.30) | 14.44 (18.15) | 0.28 |
| IES change (6 months – 6 weeks) | 1.72 (12.41) | 1.11 (11.40) | 0.87 |
*Indicates statistically significant p-value
Funding
This study was funded by the Research in Palliative and End-of Life Communication and Training (RESPECT) Center, Indiana University–Purdue University Indianapolis and the National Institute on Aging (R01 AG044408)
Prior Presentations
None.
Conflict of Interest
Dr. Torke reports grants from National Institute on Aging, grants from Research in Palliative and End-of Life Communication and Training (RESPECT) Center, Indiana University Purdue University Indianapolis, during the conduct of the study, and is a member of the American Geriatrics Society Ethics Committee
Otherwise the authors of this manuscript have nothing else to disclose
References
- 1.Torke AM, Sachs GA, Helft PR, Montz K, Hui SL, Slaven JE, et al. Scope and outcomes of surrogate decision making among hospitalized older adults. JAMA Intern Med. 2014;174(3):370-7. 10.1001/jamainternmed.2013.13315 [DOI] [PMC free article] [PubMed]
- 2.Raymont V, Bingley W, Buchanan A, David AS, Hayward P, Wessely S, et al. Prevalence of mental incapacity in medical inpatients and associated risk factors: cross-sectional study. Lancet. 2004;364(9443):1421-7. 10.1016/S0140-6736(04)17224-3 [DOI] [PubMed]
- 3.Luce JM. End-of-life decision making in the intensive care unit. Am J Res Crit Care Med. 2010;182(1):6-11. 10.1164/rccm.201001-0071CI [DOI] [PubMed]
- 4.Brudney D. Choosing for another: beyond autonomy and best interests. Hastings Cent Rep. 2009;39(2):31–7. doi: 10.1353/hcr.0.0113. [DOI] [PubMed] [Google Scholar]
- 5.Deciding to Forego Life-Sustaining Treatment: A Report on the Ethical, Medical, and Legal Issues in Treatment Decisions. President's Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. United States of America. 1983.
- 6.Emanuel EJ, Emanuel LL. Proxy decision making for incompetent patients. An ethical and empirical analysis. JAMA. 1992;267(15):2067-71. [PubMed]
- 7.Buchanan AE, Brock DW. Deciding For Others: The Ethics of Surrogate Decision Making: Cambridge University Press; 1990.
- 8.Lang F, Quill T. Making decisions with families at the end of life. Am Fam Physician. 2004;70(4):719–23. [PubMed] [Google Scholar]
- 9.Fagerlin A, Schneider CE. Enough. The failure of the living will. Hastings Cent Rep. 2004;34(2):30–42. doi: 10.2307/3527683. [DOI] [PubMed] [Google Scholar]
- 10.Dresser R. Precommitment: a misguided strategy for securing death with dignity. Tex Law Rev. 2003;81(7):1823–47. [PubMed] [Google Scholar]
- 11.Shalowitz DI, Garrett-Mayer E, Wendler D. The accuracy of surrogate decision makers: a systematic review. Arch Intern Med. 2006;166(5):493-7. 10.1001/archinte.166.5.493 [DOI] [PubMed]
- 12.Torke AM, Alexander GC, Lantos J. Substituted judgment: the limitations of autonomy in surrogate decision making. J Gen Int Med. 2008;23(9):1514-7. 10.1007/s11606-008-0688-8 [DOI] [PMC free article] [PubMed]
- 13.Sulmasy DP, Snyder L. Substituted interests and best judgments: an integrated model of surrogate decision making. JAMA. 2010;304(17):1946-7. 10.1001/jama.2010.1595 [DOI] [PubMed]
- 14.Vig EK, Taylor JS, Starks H, Hopley EK, Fryer-Edwards K. Beyond substituted judgment: How surrogates navigate end-of-life decision-making. J Am Ger Soc. 2006;54(11):1688–93. doi: 10.1111/j.1532-5415.2006.00911.x. [DOI] [PubMed] [Google Scholar]
- 15.Fritsch J, Petronio S, Helft PR, Torke AM. Making decisions for hospitalized older adults: ethical factors considered by family surrogates. J Clin Ethics. 2013;24(2):125–34. [PMC free article] [PubMed] [Google Scholar]
- 16.Torke AM, Monahan P, Callahan CM, Helft PR, Sachs GA, Wocial LD, et al. Validation of the Family Inpatient Communication Survey. J Pain Symptom Manage. 2017;53(1):96-108 e4. 10.1016/j.jpainsymman.2016.08.010 [DOI] [PMC free article] [PubMed]
- 17.Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. 2016;39:24-31. 10.1016/j.genhosppsych.2015.11.005 [DOI] [PubMed]
- 18.Kroenke K, Spitzer RL, Williams JB, Lowe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345-59. 10.1016/j.genhosppsych.2010.03.006 [DOI] [PubMed]
- 19.O'Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995;15(1):25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 20.Torke AM, Moloney R, Siegler M, Abalos A, Alexander GC. Physicians' views on the importance of patient preferences in surrogate decision-making. J Am Ger Soc. 2010;58(3):533-8. 10.1111/j.1532-5415.2010.02720.x [DOI] [PMC free article] [PubMed]
- 21.Braun UK, Naik AD, McCullough LB. Reconceptualizing the experience of surrogate decision making: reports vs genuine decisions. Ann Fam Med. 2009;7(3):249-53. 10.1370/afm.963 [DOI] [PMC free article] [PubMed]
- 22.Wendler D, Rid A. Systematic review: the effect on surrogates of making treatment decisions for others. Ann Intern Med. 2011;154(5):336-46. 10.7326/0003-4819-154-5-201103010-00008 [DOI] [PubMed]
- 23.Meeker MA. Family surrogate decision making at the end of life: seeing them through with care and respect. Qual Health Res. 2004;14(2):204-25. 10.1177/1049732303260501 [DOI] [PubMed]
- 24.Moorman SM, Carr D. Spouses' effectiveness as end-of-life health care surrogates: accuracy, uncertainty, and errors of overtreatment or undertreatment. Gerontologist. 2008;48(6):811–9. doi: 10.1093/geront/48.6.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berger JT. Patients' interests in their family members’ well-being: an overlooked, fundamental consideration within substituted judgments. J Clin Ethics. 2005;16(1):3–10. [PubMed] [Google Scholar]
- 26.Sehgal A, Galbraith A, Chesney M, Schoenfeld P, Charles G, Lo B. How strictly do dialysis patients want their advance directives followed? JAMA. 1992;267(1):59–63. doi: 10.1001/jama.1992.03480010067026. [DOI] [PubMed] [Google Scholar]
- 27.Sulmasy DP, Hughes MT, Thompson RE, Astrow AB, Terry PB, Kub J, et al. How would terminally ill patients have others make decisions for them in the event of decisional incapacity? A longitudinal study. J Am Ger Soc. 2007;55(12):1981-8. 10.1111/j.1532-5415.2007.01473.x [DOI] [PMC free article] [PubMed]
- 28.Butow PN, Maclean M, Dunn SM, Tattersall MH, Boyer MJ. The dynamics of change: cancer patients' preferences for information, involvement and support. Ann Oncol. 1997;8(9):857–63. doi: 10.1023/A:1008284006045. [DOI] [PubMed] [Google Scholar]
- 29.Braun UK, Beyth RJ, Ford ME, Espadas D, McCullough LB. Decision-making styles of seriously ill male Veterans for end-of-life care: Autonomists, Altruists, Authorizers, Absolute Trusters, and Avoiders. Patient Educ Couns. 2014;94(3):334-41. 10.1016/j.pec.2013.10.013 [DOI] [PubMed]
- 30.Salvi F, Miller MD, Grilli A, Giorgi R, Towers AL, Morichi V, et al. A manual of guidelines to score the modified cumulative illness rating scale and its validation in acute hospitalized elderly patients. J Am Ger Soc. 2008;56(10):1926-31. 10.1111/j.1532-5415.2008.01935.x [DOI] [PubMed]