Abstract
Nuclear receptor corepressor 1 (NCOR1) is a transcriptional regulator bridging repressive chromatin modifying enzymes with transcription factors. NCOR1 regulates many biological processes, however its role in T cells is not known. Here we show that Cd4-Cre-mediated deletion of NCOR1 (NCOR1 cKOCd4) resulted in a reduction of peripheral T cell numbers due to a decrease in single-positive (SP) thymocytes. In contrast, double-positive (DP) thymocyte numbers were not affected in the absence of NCOR1. The reduction in SP cells was due to diminished survival of NCOR1-null postselection TCRβhiCD69+ and mature TCRβhiCD69− thymocytes. NCOR1-null thymocytes expressed elevated levels of the pro-apoptotic factor BIM and showed a higher fraction of cleaved caspase 3-positive cells upon TCR stimulation ex vivo. However, staphylococcal enterotoxin B (SEB)-mediated deletion of Vβ8+ CD4SP thymocytes was normal, suggesting that negative selection is not altered in the absence of NCOR1. Finally, transgenic expression of the pro-survival protein BCL2 restored the population of CD69+ thymocytes in NCOR1 cKOCd4 mice to a similar percentage as observed in WT mice. Together, these data identify NCOR1 as a crucial regulator of the survival of SP thymocytes and revealed that NCOR1 is essential for the proper generation of the peripheral T cell pool.
Introduction
Cell fate decisions and lineage specifications during T cell development are accompanied with the establishment and maintenance of cell lineage-specific expression patterns1. Lineage-specific genes are induced, while lineage-inappropriate genes are silenced. Epigenetic mechanisms such as DNA methylation and histone modifications regulate the chromatin accessibility for the transcriptional machinery at target genes and play a crucial role in these processes. Chromatin modifying enzymes that regulate reversible changes in histone acetylation or methylation are recruited to gene-specific transcription factors as part of larger multiprotein complexes. This leads to either transcriptional activation or repression of target genes. The outcome depends on the cellular context, the type of the recruiting transcription factor, the composition of the multiprotein complexes and the associated chromatin modifying enzymes2.
One important group of transcriptional regulators that bridge repressive chromatin modifying enzymes with specific transcription factors is formed by nuclear receptor corepressor 1 (NCOR1) and its related factor silencing mediator of retinoid and thyroid receptor (SMRT or NCOR2)3. NCOR1 was identified as a non-DNA binding corepressor of the transcription factors thyroid hormone receptors and retinoic acid receptors and is essential for mediating transcriptional repression of nuclear receptors in the absence of their ligands4, however NCOR1 interacts also with many other types of transcription factors5. The repressive activity of NCOR1-containing complexes is mediated via the recruitment of histone deacetylases (HDACs), in particular HDAC3, although association with other HDAC members such as HDAC1, 4, 5 and 7 has been shown as well2,6. NCOR1 has been implicated in many biological processes including development, differentiation, cell homeostasis and metabolism3. Germline deletion of NCOR1 results in embryonic lethality at E15.5 due to defects in central nervous system development and in definitive erythropoiesis7. Conditional gene targeting approaches as well as the generation of transgenic mouse models expressing mutant versions of NCOR1 revealed cell type- and tissue-specific functions for NCOR1 in muscle cells8, adipocytes9, macrophages10 and in the liver11.
The role of NCOR1 in T cells is not known. It has been shown in E14.5 Ncor1 −/− fetal thymic organ cultures that loss of NCOR1 leads to a severe block at the double-negative (DN) 3 stage with almost no double-positive (DP) cells after 3 days of culture7. Moreover, NCOR1 interacts with several members of the BTB domain-containing zinc finger (BTB-ZF) transcription factor family such as PLZF12,13, BCL613,14 and MAZR15, which itself are crucial regulators of T cell development and function16,17. In thymocytes, deletion of HDAC3, the main HDAC family member recruited by NCOR1 to target genes2, leads to severely reduced numbers of mature thymocytes and peripheral T cells due to defects at the DN4 to DP transition, during positive selection and post-thymic T cell maturation, dependent on the developmental stage of Hdac3 deletion18–21. Together, these data suggest important functions for NCOR1 in T cells.
Here we investigated the role of NCOR1 during T cell development by using conditional gene targeting approaches. We show that Cd4-Cre-mediated T cell-specific loss of NCOR1 (abbreviated Ncor1 f/f Cd4-Cre and designated as NCOR1 cKOCd4) led to reduced numbers of CD4 and CD8 single-positive (SP) cells, while the number of CD4+CD8+ DP cells was not affected in the absence of NCOR1. The drop in SP thymocyte numbers in NCOR1 cKOCd4 mice, which was caused by cell-intrinsic effects, resulted also in reduced numbers of peripheral T cells. SP thymocytes were reduced due to impaired survival of positively selected NCOR1-null TCRβhiCD69+/− thymocytes. Further, NCOR1-null thymocytes expressed elevated levels of the pro-apoptotic factor BIM and, upon ex vivo anti-CD3/anti-CD28 stimulation, displayed a higher fraction of cleaved caspase 3-positive cells. However, negative selection was not affected, since staphylococcal enterotoxin B (SEB)-mediated depletion of Vβ8-expressing CD4SP thymocytes was not altered. The mature SP cells that developed in the absence of NCOR1 expressed elevated levels of IL-7Rα (CD127) and BCL2, which both promote the survival of positively selected cells. This suggests compensatory mechanisms within the NCOR1 cKOCd4 SP population to overcome elevated expression levels of BIM. Finally, transgenic expression of BCL2 restored the population of TCRβhiCD69+/− thymocytes and hence the development of SP cells to a similar percentage as observed in WT mice. Together, these data identify NCOR1 as a crucial regulator of the survival of SP thymocytes and revealed that NCOR1 is essential for the proper generation of the peripheral T cell pool.
Results
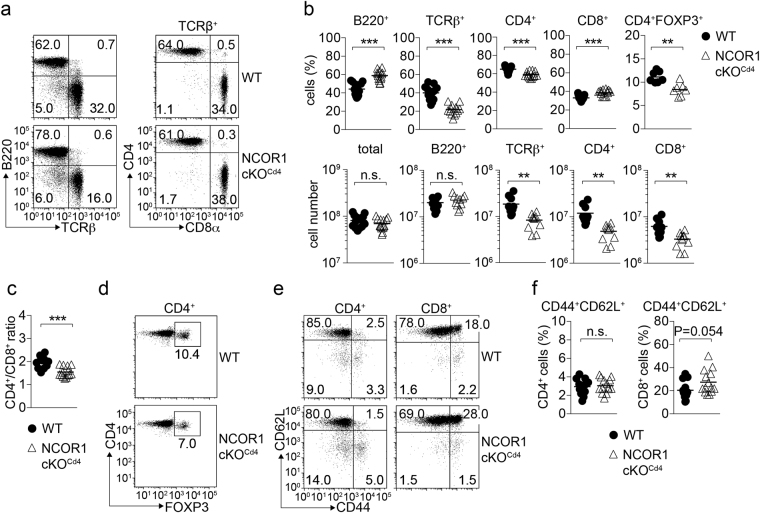
Conditional deletion of NCOR1 in T cells leads to reduced numbers of peripheral T cells
To reveal the function of NCOR1 in the T cell lineage, we generated mice with a T cell-specific deletion of Ncor1. Since it has been reported that NCOR1-null fetal thymocytes have a block at the DN stage during T cell development, we crossed mice carrying a conditional “floxed” Ncor1 allele (Ncor 1 f/f)8 with the Cd4-Cre deleter strain22 to generate Ncor 1 f/f (WT) and Ncor 1 f/f Cd4-Cre (NCOR1 cKOCd4) mice. In comparison to WT mice, NCOR1 cKOCd4 mice displayed a 2-fold reduction of the percentage and number of peripheral T cells (Fig. 1a,b). Within the TCRβ+ subset in NCOR1 cKOCd4 mice, the frequencies of CD8+ T cells and CD4+ T cells were slightly increased and decreased, respectively, (Fig. 1a,b upper panel), leading to a mild change in the CD4/CD8 ratio in the absence of NCOR1 (Fig. 1c). Further, there was a relative reduction of FOXP3+ regulatory T cells within the already reduced CD4+ T cell population (Fig. 1b and d). The CD44hiCD62L+ subset within the CD8+ T cell, but not within the CD4+ T cell population, was slightly enhanced in NCOR1 cKOCd4 mice (Fig. 1e,f). Peripheral CD4+ and CD8+ T cells did not have a remaining Ncor1 allele, indicating that no T cells escaped the deletion of Ncor1 in NCOR1 cKOCd4 mice (Supplementary Figs S1a and S2a).
Figure 1.
Reduced numbers of peripheral T cells in the absence of NCOR1. (a) Flow cytometry analysis of B220, TCRβ, CD4 and CD8α expression on splenocytes isolated from Ncor1 f/f (WT) and Ncor1 f/f Cd4-Cre (NCOR1 cKOCd4) mice. For CD4 and CD8α expression, cells were pre-gated on TCRβ+ T cells. (b) Percentages and numbers of total cells, B220+ cells, TCRβ+ cells, CD4+ T cells, CD8+ T cells and CD4+FOXP3+ T cells (only percentages) in the spleens of WT and NCOR1 cKOCd4 mice are shown. (c) Diagram indicates CD4 to CD8 T cell ratio. (d) Flow cytometry analysis of FOXP3 expression on CD4+ T cells isolated from the spleen of WT and NCOR1 cKOCd4 mice (pre-gated on TCRβ+CD4+ T cells). (e) Flow cytometry analysis of CD44 and CD62L expression on CD4+ and CD8+ T cells isolated from the spleen of WT and NCOR1 cKOCd4 mice. (f) Percentage of CD44hiCD62L+ CD4+ and CD8+ splenic T cells in WT and NCOR1 cKOCd4 mice. (a,d,e) Numbers indicate the percentage of cells in the respective quadrants. (b,c,f) Thick horizontal bars indicate the mean. *P < 0.05, **P < 0.01 and ***P < 0.001 (unpaired two-tailed Student’s t-test). Data are representative (a,d,e) or show the summary (b,c,f) of at least 10 mice (a,b), 7 mice (d) or 13 mice (c,e,f) that were analyzed in at least 3 (a,b,d) and 4 (c,e,f) independent experiments.
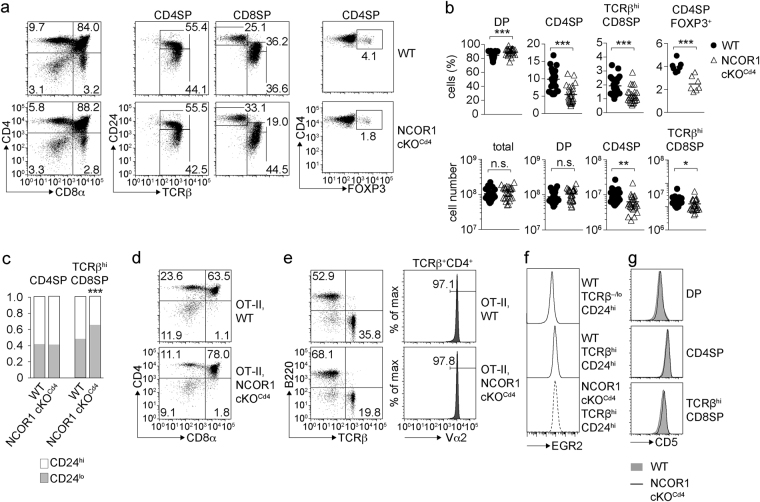
Loss of NCOR1 leads to reduced numbers of single-positive thymocytes due to a T cell-intrinsic effect
To test whether developmental alterations caused the reduction in peripheral T cell numbers, thymocyte subsets in WT and NCOR1 cKOCd4 mice were analyzed based on CD4, CD8, TCRβ and CD24 expression. This revealed that the percentages and cell numbers of CD4SP and TCRβhi CD8SP thymocytes were reduced in NCOR1 cKOCd4 mice (Fig. 2a,b). There was a slight increase in the fraction of CD24lo cells within the TCRβhi CD8SP population in the absence of NCOR1, while the distribution of CD24hi to CD24lo cells was normal within the CD4SP population (Fig. 2a,c). Ncor1 was efficiently deleted from the DP stage on (Supplementary Figs S1b and S2b). NCOR1 protein was still detected in DP thymocytes, suggesting a slow turnover rate of NCOR1 protein in DP cells. However, NCOR1 protein almost completely disappeared in CD4SP cells (Supplementary Fig. S2b). Of note, in WT mice NCOR1 was expressed at higher levels in CD4SP than in DP thymocytes (Supplementary Fig. S2b), as previously observed15, suggesting an important role for NCOR1 during the DP to CD4SP transition. Like in the peripheral T cell population of NCOR1 cKOCd4 mice, there was also a relative decrease of thymic FOXP3+ regulatory T cells within the already reduced CD4SP population (Fig. 2,b). The reduction in CD4SP and TCRβhi CD8SP thymocytes corresponded with a mild increase in the percentage of DP cells (Fig. 2a,b). However, the number of total thymocytes as well as of DP cells was similar between WT and NCOR1 cKOCd4 mice (Fig. 2b). The percentages of mature CD4SP thymocytes and peripheral T cells were also reduced in NCOR1 cKOCd4 mice transgenic for the MHC class II-restricted TCR OT-II (Fig. 2d,e). Of note, all TCR-transgenic OT-II,NCOR1 cKOCd4 CD4+ T cells were TCR Vα2+ (Fig. 2e), indicating that CD4+ T cells were positively selected on the transgenic Vα2 chain. Furthermore, WT and NCOR1 cKOCd4 TCRβhiCD24hi thymocytes upregulated the transcription factor EGR2 to a similar level (Fig. 2f) and TCRβhi SP cells that developed in NCOR1 cKOCd4 mice showed a similar upregulation of CD5 as WT SP cells, suggesting no major alteration in TCR signaling strength during positive selection (Fig. 2g). Finally, the generation of either wild-type (CD45.1+) and Ncor1 f/f (WT; CD45.2+) or wild-type (CD45.1+) and Ncor1 f/f Cd4-Cre (NCOR1 cKOCd4; CD45.2+) mixed bone marrow (BM) chimeric mice showed that the reduction in T cell numbers in the thymus and spleen was due to T cell-intrinsic effects and not due to secondary effects that affect mature T cell numbers (Fig. 3a,b).
Figure 2.
Mature SP thymocytes are reduced in NCOR1 cKOCd4 mice. (a) Flow cytometry analysis of CD4, CD8α, TCRβ, CD24 and FOXP3 expression in WT and NCOR1 cKOCd4 thymocytes. The middle panel shows CD24 and TCRβ expression on CD4SP and CD8SP thymocytes. (b) Percentages and cell numbers of all thymocytes, DP, CD4SP and TCRβhi CD8SP thymocytes, as well as percentages of FOXP3+ T cells within the CD4SP subset in WT and NCOR1 cKOCd4 mice. (c) Bar diagrams show the relative distribution of CD24hi and CD24lo cells within the CD4SP and TCRβhi CD8SP subsets. (d) Expression of CD4 and CD8α on thymocytes isolated from OT-II,WT and OT-II,NCOR1 cKOCd4 littermates. (e) Flow cytometry analysis of B220 and TCRβ expression on splenocytes isolated from OT-II,WT and OT-II,NCOR1 cKOCd4 littermates. Histograms depict Vα2 expression on TCRβ+ CD4+ OT-II T cells. (f) Histogram depicts EGR2 expression in immature (TCRβhiCD24hi) thymocytes of WT and NCOR1 cKOCd4 mice. WT TCRβ−/lo CD24hi DP thymocytes were used as a negative staining control. (g) Histograms depict CD5 expression on DP (upper panel), CD4SP (middle panel) and TCRβhi CD8SP (lower panel) thymocytes in WT and NCOR1 cKOCd4 mice. (a,d,e) Numbers indicate the percentage of cells in the respective quadrants. (b) Thick horizontal bars indicate the mean. (b,c) *P < 0.05, **P < 0.01 and ***P < 0.001 (unpaired two-tailed Student’s t-test). Data are representative (a,d,e,f,g) or show the summary (b,c) of 7–10 mice (a,c), 25–26 mice (b; except for CD4SP FOXP3+ cells, where n = 7 mice) and 5–6 mice (d,e,f,g) that were analyzed in 3–4 (a,c), 8 (b; except for CD4SP FOXP3+ cells: 3), 3 (d,e,g) and 2 (f) independent experiments.
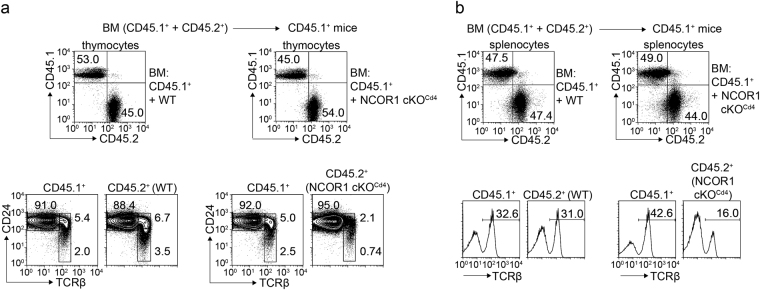
Figure 3.
The reduction of SP cells in NCOR1 cKOCd4 mice is T cell-intrinsic. Flow cytometry analysis of CD45.1 and CD45.2 expression (upper panels) on thymocytes (a) and splenocytes (b) isolated from BM chimeric CD45.1+ mice that received either Ncor1 f/f (WT) or Ncor1 f/f Cd4-Cre (NCOR1 cKOCd4) CD45.2+ BM cells that had been mixed at a 1:1 ratio with wild-type (WT, CD45.1+) BM cells. The lower panels in (a) show CD24 and TCRβ expression on thymocytes pre-gated on CD45.1+ and CD45.2+ subsets, while the lower panels in (b) depicts TCRβ expression on splenocytes pre-gated on CD45.1+ and CD45.2+ subsets. Data are representative of 9–10 mice analyzed in 3 independent experiments.
NCOR1 regulates the survival of positively selected TCRβhiCD69+/− thymocytes
Next, we investigated in detail why SP thymocytes were reduced in the absence of NCOR1. In vivo BrdU labeling experiments showed that TCRβhiCD24lo CD4SP thymocytes developed with similar kinetics in NCOR1 cKOCd4 mice in comparison to WT mice (Fig. 4a), indicating that there was no developmental block at the DP stage that results in a reduction of mature SP subsets. Ex vivo, NCOR1 cKOCd4 thymocytes showed a higher fraction of cleaved caspase 3-positive cells after overnight culture in the presence of anti-CD3/anti-CD28, while in the absence of TCR stimulation the fraction of cleaved caspase 3-positive cells was similar between WT and NCOR1 cKOCd4 (Fig. 4b,c). This suggests that the survival of thymocytes that received a TCR-mediated signal might be affected in the absence of NCOR1.
Figure 4.
NCOR1 regulates the survival of positively selected thymocytes. (a) Summary shows the percentage of DP (left diagram) and CD4SP (right diagram) thymocyte subsets in WT and NCOR1 cKOCd4 mice that have incorporated BrdU over the indicated time period. (b) Histograms depict cleaved caspase 3 in WT and NCOR1 cKOCd4 thymocytes that were cultured for 24 h with medium only or activated with anti-CD3/anti-CD28. (c) The diagram shows the summary of experiments performed as described in (b). (d) Flow cytometry analysis of CD69 and TCRβ expression on thymocytes isolated from WT and NCOR1 cKOCd4 mice. (e) Percentage and cell numbers of TCRβ−/loCD69−, TCRβloCD69+, TCRβhiCD69+ and TCRβhiCD69− thymocytes in WT and NCOR1 cKOCd4 mice. (f) Diagram summarizing the percentages of Vβ8+ and Vβ6+ CD4SP subsets of WT and NCOR1 cKOCd4 mice that have been injected with PBS or with SEB. (b,d) Numbers indicate the percentage of cells in the respective regions or quadrants. (a,c,e) Thick horizontal bars indicate the mean. *P < 0.05, **P < 0.01 and ***P < 0.001. Unpaired two-tailed Student’s t-test. Data are representative (b,d) or show the summary (a,c,e,f) of 4–6 mice (a), 6–7 mice (b,c), 14 mice (d,e; for percentages), 10–11 mice (e; for cell numbers), 5 (f; SEB injection) and 3 mice (f; PBS injection) that were analyzed in 2–3 (a), 2 (b,c,f) and 6–7 (d,e) independent experiments.
In vivo, positive and negative selection of thymocytes is dependent on persistent TCR signaling and associated with either the survival and maturation or the deletion of developing thymocytes, respectively. Thus, we investigated in more detail whether these processes are affected in NCOR1 cKOCd4 mice. To analyze the differentiation of thymocytes during positive selection, we determined the dynamic expression pattern of TCRβ and CD69 that defines distinct stages of positive selection23–25: unsignaled (pre-selection) thymocytes (TCRβ−/loCD69−); cells undergoing positive selection (TCRβloCD69+); postselection thymocytes (TCRβhiCD69+) and mature SP thymocyte subsets (TCRβhiCD69−) (Fig. 4d). In comparison to WT mice, there was a reduction in the percentages of signaled TCRβloCD69+ thymocyte subsets as well as strong reduction in the percentages and cell numbers of postselection TCRβhiCD69+ and mature TCRβhiCD69− SP cells in the absence of NCOR1 (Fig. 4e). This indicated a significant loss of positively selected thymocytes in the absence of NCOR1 in vivo. To assess whether loss of NCOR1 affected also negative selection, we determined whether SEB superantigen-induced clonal deletion of SEB-reactive Vβ8+ CD4SP thymocytes is altered in NCOR1 cKOCd4 mice26. There was a similar reduction of SEB-reactive Vβ8+ CD4SP cells in WT and NCOR1 cKOCd4 mice, while SEB-non-reactive Vβ6+ CD4SP cells were not deleted upon injection of SEB (Fig. 4f). Together, these data indicated that NCOR1 cKOCd4 SP cells are reduced as a consequence of an impaired survival of positively selected TCRβhiCD69+/− cells, rather than due to enhanced negative selection of NCOR1-deficient thymocytes.
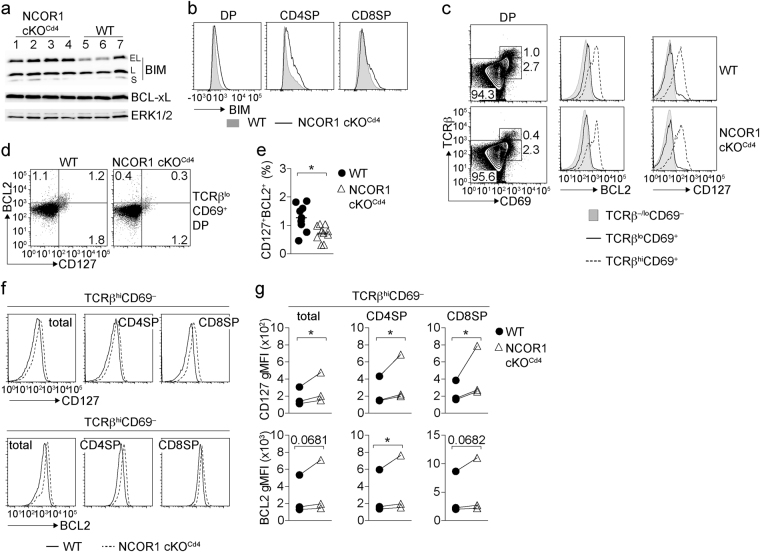
Mature NCOR1-null SP cells display elevated CD127 and BCL2 levels
The survival of DP and SP thymocytes is dependent on the balanced expression of the pro-apoptotic protein BIM and the pro-survival factors BCL-xL and BCL2 that are dynamically expressed during thymocyte development27–29. Immunoblot analysis of total NCOR1 cKOCd4 thymocytes revealed higher expression levels of the pro-apoptotic factor BIM, in particular the BIMEL isoform (Fig. 5a), which was due to increased BIM expression both in DP as well as CD4SP thymocytes and, to a lower degree, in CD8SP subsets (Fig. 5b). In contrast, the expression of BCL-xL, which is important for the survival of DP thymocytes but not of SP cells27,30, was not changed (Fig. 5a), indicating that there is no increase in BCL-xL expression to compensate for higher BIM levels. Positive selection correlates with an upregulation of the IL-7 receptor (IL-7R), a cytokine receptor which triggers the induction of BCL2 to ensure the survival of positively selected cells31. A detailed analysis of DP thymocytes revealed that TCRβhiCD69+ DP cells present in NCOR1 cKOCd4 mice upregulated BCL2 and CD127 similar to WT TCRβhiCD69+ DP thymocytes (Fig. 5c and Supplementary Fig. S4). However, NCOR1 cKOCd4 TCRβloCD69+ DP cells showed a 2-fold reduction in the fraction of cells that expressed both the IL-7Rα chain (CD127) and BCL2 (Fig. 5d,e). This suggests a reduced survival of TCR-triggered TCRβloCD69+ DP thymocyte subsets in NCOR1 cKOCd4 mice. A close examination of CD127 and BCL2 expression at later stages of thymocyte development revealed that positively selected mature TCRβhiCD69− total SP, CD4SP and CD8SP cells displayed higher CD127 expression levels (increase gMFI for total SP: 45 ± 11%; CD4SP: 46 ± 12%; CD8SP: 74 ± 27%) and mildly increased levels of BCL2 (increase gMFI for total SP: 22 ± 12%; CD4SP: 20 ± 9%; CD8SP: 18 ± 9%) in the absence of NCOR1 (Fig. 5f,g). These data indicate that mature NCOR1 cKOCd4 SP cells that survived displayed elevated CD127 and BCL2 levels, which might partially compensate for the increased BIM expression levels in NCOR1 cKOCd4 SP thymocytes.
Figure 5.
Mature NCOR1-null SP cells display elevated CD127 and BCL2 levels. (a) Immunoblot showing the three BIM isoforms (BIMEL, BIML, BIMS) and BCL-xL expression in 4 independent NCOR1 cKOCd4 (lane 1–4) and 3 independent WT (lane 5–7) thymocyte samples. Whole cell lysates from ~5 × 106 cells were loaded and ERK1/2 was used as loading control. The pictures were cropped and uncropped pictures are shown in Supplementary Fig. 3. (b) Histograms depict pan BIM expression in WT and NCOR1 cKOCd4 DP, CD4SP and CD8SP thymocytes. (c) Flow cytometry analysis of CD69 and TCRβ expression on DP thymocytes isolated from WT and NCOR1 cKOCd4 mice. Histograms on the right show surface expression of CD127 and intracellular expression of BCL2 expression in the indicated subsets. (d) Flow cytometry analysis of BCL2 and CD127 expression on TCRβloCD69+ DP thymocytes isolated from WT and NCOR1 cKOCd4 mice. (e) The diagram indicates the percentage of BCL2+CD127+ TCRβloCD69+ DP thymocytes. (f) Histograms depict CD127 (upper panel) and BCL2 (lower panel) expression in TCRβhiCD69− thymocyte subsets (total, CD4SP and CD8SP) in WT and NCOR1 cKOCd4 mice. (g) The diagrams indicate geometric mean fluorescence intensity (gMFI) of CD127 and BCL2 expression on the particular subset, and show the summary of 3 independent experiments (2–5 mice were analyzed per group in an experiment, average gMFI for each experiment is shown). The lines connect samples analyzed in the same experiment. (e) *P < 0.01, unpaired two-tailed Student’s t-test. (g) *P < 0.01, n.s., not significant, one sample t-test (columns statistics; WT was set as 1 and relative NCOR1 cKOCd4 values were calculated, diagrams show absolute gMFI levels for each experiment). Data are representative (a,b,c,d,f) or show the summary (e,g) of 7 (a), 7–8 (b), 9–10 (d,e) mice that were analyzed in 2 (a,b) and 3 (c,d,e) independent experiments. Histograms (c,f) are representative of 9–10 mice analyzed in 3 independent experiments.
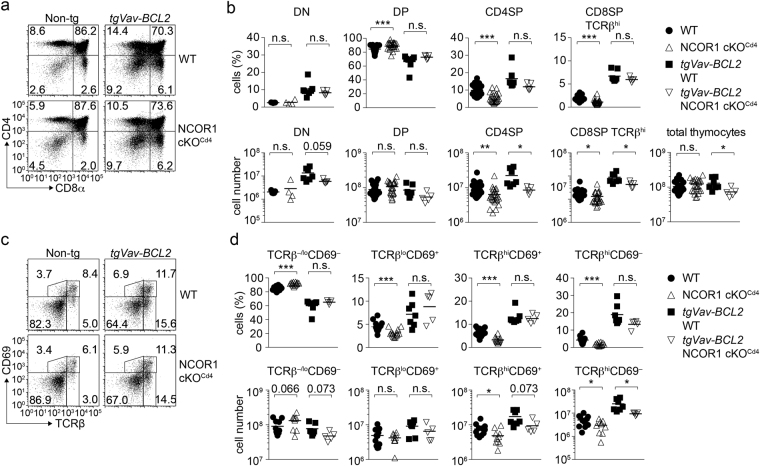
Transgenic expression of BCL2 rescues the generation of NCOR1-null SP thymocytes
The anti-apoptotic factor BCL2 is important for the survival of positively selected cells31. Mature TCRβhiCD69− SP thymocytes that survived positive selection in the absence of NCOR1 expressed mildly increased levels of BCL2 (Fig. 5f,g). Therefore, we next investigated whether the loss of CD69+ NCOR1-null thymocytes can be rescued by enforced expression of BCL2. As previously reported32, Vav promotor-driven transgenic expression of (human) BCL2 increases the percentages and numbers of DN, CD4SP and CD8SP thymocytes in WT mice with a corresponding decrease in DP thymocytes (Fig. 6a,b). As a consequence, there is also an increase in TCRβloCD69+, TCRβhiCD69+ and mature SP TCRβhiCD69− subsets (Fig. 6c,d). Similar changes in DN, DP, CD4SP and TCRβhi CD8SP thymocytes subsets due to transgenic BCL2 expression were also observed on a NCOR1 cKOCd4 background (Fig. 6a,b). Further, upon transgenic BCL2 expression in NCOR1 cKOCd4 mice, the percentages of TCRβ−/loCD69−, TCRβloCD69+, TCRβhiCD69+ and mature SP TCRβhiCD69− subsets were similar to WT mice (Fig. 6c,d), suggesting that transgenic BCL2 overexpression restored the percentages of TCRβhi cells within the NCOR1 cKOCd4 thymocyte population. The ability of BCL2 to rescue NCOR1 cKOCd4 thymocytes strongly supports our findings that signaled CD69+ thymocytes are lost due to apoptosis rather than due to a developmental block at the onset of positive selection or due to increased negative selection. In contrast to transgenic BCL2, Lck promotor-driven transgenic expression of BCL-xL33 in NCOR1 cKOCd4 mice did not rescue the percentages of TCRβhiCD69+ and TCRβhiCD69− thymocytes to levels observed in tgBCL-xL,WT mice (Supplementary Fig. S5). Since BCL-xL is a pro-survival factor important for the lifespan of DP thymocytes but dispensable for thymocyte survival during positive selection and maturation27,30, these data suggest that loss of NCOR1 affects the survival of positively selected thymocytes.
Figure 6.
Transgenic expression of BCL2 rescues the generation of NCOR1 cKOCd4 SP thymocytes. (a) Flow cytometry analysis of CD4 and CD8 expression on thymocytes isolated from WT and NCOR1 cKOCd4 mice that are non-transgenic (left panel) or transgenic for Vav-BCL2 (right panel). (b) Percentages (upper panel) and cell numbers (lower panel) of DN, DP, CD4SP and TCRβhi CD8SP thymocytes in WT and NCOR1 cKOCd4 mice that are non-transgenic or transgenic for Vav-BCL2 are shown. (c) Flow cytometry analysis of CD69 and TCRβ expression on thymocytes isolated from WT and NCOR1 cKOCd4 mice that are non-transgenic (left panel) or transgenic for Vav-BCL2 (right panel). (d) Percentages (upper panel) and cell numbers (lower panel) of TCRβ−/loCD69−, TCRβloCD69+, TCRβhiCD69+ and TCRβhiCD69− thymocytes in WT and NCOR1 cKOCd4 mice that are non-transgenic and transgenic for Vav-BCL2 are indicated. (a,c) Numbers indicate the percentage of cells in the respective quadrants or regions. (b,d) Thick horizontal bars indicate the mean; *P < 0.05, **P < 0.01 and ***P < 0.001, n.s., not significant; unpaired two-tailed Student’s t-test. Data are representative (a,c) or show the summary (b,d) of 9–15 (for non transgenic mice; non-tg) and 5–9 (for tgVav-BCL2 mice) mice that were analyzed in 4–7 independent experiments. (b,d) The data for WT and NCOR1 cKOCd4 mice in (b; except DN subsets) and (d) were already shown in Figures 2b and 4e, respectively.
Discussion
In this study we provide genetic evidence that NCOR1 is essential for the generation of the peripheral T cell pool by regulating the survival of positively selected TCRβhiCD69+/− thymocytes. In our study we also observed that DP cells were present at similar numbers in WT and NCOR1 cKOCd4 mice. Of note, NCOR1 protein levels in NCOR1 cKOCd4 DP thymocytes were similar to those in WT DP cells despite an efficient genomic deletion of Ncor1. This indicates a slow turnover of NCOR1 protein and precluded conclusions about the role of NCOR1 in DP thymocytes. However, our data indicate an important role for NCOR1 beyond the DP stage, since there was a gradual decline of the percentages of NCOR1-null thymocytes from the CD69+ stage on during the DP to SP transition, which led to a significant reduction in cell numbers of TCRβhiCD69+/− cells. The DP to SP transition is also accompanied by an upregulation of NCOR1, since WT CD4SP cells expressed higher NCOR1 levels in comparison to WT DP cells. It is not known at which TCRβlo/hiCD69+/− stage NCOR1 is upregulated. This process might occur gradually, potentially leading to a progressive increase in phenotypic alterations from the onset of positive selection to the mature SP stage in the absence of NCOR1. BrdU labeling studies showed a similar appearance of BrdU+ cells within the SP thymocyte population in NCOR1 cKOCd4 mice. In addition, MHC class II-restricted OT-II TCR transgenic NCOR1 cKOCd4 CD4+ T cells, which were also reduced in the absence of NCOR1, displayed a similar expression of the transgenic Vα2 chain. Thus, it is unlikely that a block in positive selection or changes in the TCR signaling strength caused the reduction of SP cells in the absence of NCOR1. This is also supported by the observation that CD5 expression, which parallels the avidity or signaling intensity of the positively selecting TCR–MHC-ligand interaction34, is similar in WT and NCOR1 cKOCd4 SP cells. Our data rather indicate that NCOR1 is essential for the efficient survival of positively selected TCRβhiCD69+/− thymocytes. They further suggest that the first phenotypic alterations in NCOR1 cKOCd4 might be initiated already in TCRβloCD69+ cells undergoing positive selection, consistent with the observation that NCOR1 cKOCd4 signaled TCRβloCD69+ DP thymocytes showed a lower fraction of cells that upregulated both CD127 (IL-7Rα chain) and BCL2 in comparison to WT thymocytes. Together with the elevated expression of BIM, it is likely that a change in the relative abundance of BIM and BCL2 leads to reduced survival of positively selected SP thymocytes35,36. We also observed that mature NCOR1-null TCRβhiCD69− SP thymocytes that survived displayed higher expression levels of CD127 and BCL2 in comparison to mature WT SP cells, suggesting that high levels of CD127 as well as elevated BCL2 expression are sufficient to balance enhanced BIM expression. In line with this data is our observation that transgenic expression of BCL2 restored the percentages of TCRβlo/hiCD69+ thymocytes to levels observed in WT mice and as a consequence also the percentage of SP cells. Cell numbers of CD4SP and CD8SP in tgVav-BCL2,NCOR1 cKOCd4 mice were also increased but still significantly lower in comparison to tgVav-BCL2,WT control mice, suggesting that the overexpression of BCL2 does not fully complement the survival defect of NCOR1-null SP thymocytes.
Of note, we observed high BIM expression levels in NCOR1 cKOCd4 mice despite residual NCOR1 expression, suggesting that subtle changes in NCOR1 levels might be sufficient to induce BIM expression. However, this did not affect the survival of pre-selection CD69− DP thymocytes, which were present at similar numbers in WT and NCOR1 cKOCd4 mice. This finding suggests that either the increase in BIM is not sufficient to overcome the pro-survival capacity of BCL-xL in DP thymocytes, or that BIM is not activated by posttranslational modifications, such as JNK-dependent Thr112 phosphorylation37. Moreover, transgenic expression of BCL-xL, which is important for the survival of DP thymocytes27,30, in NCOR1 cKOCd4 mice did not lead to an increase in the percentages of TCRβhiCD69+ cells as well as of TCRβhiCD69− SP cells to values observed upon expression in WT mice, showing that BCL-xL did not rescue the phenotype. WT CD4 SP cells expressed higher NCOR1 levels in comparison to WT DP cells, thus TCR triggering of DP cells might induce the upregulation of NCOR1 expression and protection from apoptosis during the DP to SP transition. This suggests that signals induced by TCR triggering of DP cells make them susceptible to BIM-mediated apoptosis in the absence of NCOR1 upregulation. In addition, ex vivo anti-CD3-stimulated NCOR1-null thymocytes displayed increased levels of cleaved caspase 3 in comparison to WT cells, while there was no difference without TCR triggering. However, SEB-induced negative selection was not changed in the absence of NCOR1, pointing towards a role for NCOR1 rather in the regulation of cell survival during positive selection and SP development but not in lowering the apoptotic threshold during negative selection. The mechanism by which loss of NCOR1 leads to the upregulation of BIM is not known and whether NCOR1 directly regulates Bcl2l11 gene (encoding for BIM) expression remains to be determined. The repressive activity of NCOR1-containing complexes is mediated via the recruitment of histone deacetylases (HDACs)2,6. Interestingly, HDAC inhibitors developed for cancer therapy do exert their activity in part via increasing the expression of BIM38,39 suggesting a potential molecular mechanism of how NCOR1 might repress BIM transcription. However, since NCOR1 is also linked with metabolic homeostasis in other cell lineages such as adipocytes9, muscle cells8 and macrophages10, we cannot exclude at present that the upregulation of BIM is a consequence of alterations beyond a direct transcriptional regulation by NCOR1.
Among all the HDAC family members, NCOR1 mainly associates with HDAC3 to repress target gene transcription2,6. Interestingly, the observed phenotype in the absence of NCOR1 is reminiscent to some of the phenotypes observed in mice with an early deletion of HDAC3 mediated by Cd2-iCre (HDAC3 cKOCd2)21 or Lck-Cre (HDAC3 cKOLck)20. It is tempting to speculate that NCOR1 and HDAC3 might partially act together in regulating SP thymocyte survival. In comparison to NCOR1 cKOCd4 mice, the reduction in SP cells is much more severe in the absence of HDAC3, which might be the consequence of the early deletion of HDAC3 during thymocyte development in those studies. Since there is, as discussed above, residual NCOR1 protein expression in NCOR1 cKOCd4 DP thymocytes, it is also possible that this might prevent a more severe drop in SP thymocyte numbers. However, qualitative differences in the phenotype of HDAC3-null and NCOR1-null thymocytes suggest also unique functions for each molecule in the regulation of SP thymocyte development. For HDAC3 cKOCd2 mice, it was shown that signaled HDAC3-null DP thymocytes failed to downregulate RORγt expression during positive selection. The prolonged expression of RORγt, which correlated with increased acetylation of the Rorc gene locus (encoding RORγt), has been linked to the observed block in positive selection in the absence of HDAC321. On the contrary, NCOR1 cKOCd4 thymocytes downregulated RORγt in a similar manner as positively selected WT thymocytes (Supplementary Figs S6a and S6b). Further, HDAC3 cKOCd2 semimature TCRβhiCD24+ CD4SP thymocytes do not properly upregulate CD127 and EGR221, which both have been shown to induce BCL2 expression31,40. This is in contrast to semimature TCRβhiCD24+ thymocytes that developed in NCOR cKOCd4 mice, which expressed similar levels of EGR2. In addition, BIM expression was normal in HDAC3 cKOCd2 TCRβhiCD24+ CD4SP thymocytes21, while BIM was upregulated in SP thymocytes in the absence of NCOR1. Differences in the function of NCOR1 and HDAC3 are also underscored by the comparison of the phenotypes of NCOR1 cKOCd4 and HDAC3 cKOCd4 mice. In contrast to NCOR1, late deletion of HDAC3 in DP thymocytes using Cd4-Cre (HDAC3 cKOCd4) does not lead to major changes in the generation of conventional CD4SP and CD8SP cells18,19. However, peripheral CD4+ and CD8+ T cell numbers are almost 10-fold and 6-fold decreased in HDAC3 cKOCd4 mice, respectively18,19. By using Cd4-Cre-mediated deletion, it has also been shown that HDAC3 is important for post-thymic T cell maturation. The majority of peripheral HDAC3 cKOCd4 T cells are recent thymic emigrants blocked in their functional maturation, and are subsequently eliminated by the complement system due to a defect in sialic acid modification and binding of IgM and complement proteins19. Further, in comparison to WT cells peripheral HDAC3-null T cells express lower levels of the complement inhibitor CD5519, a marker found on matured naïve T cells41. In NCOR1 cKOCd4 mice, such a severe reduction in peripheral T cell numbers was not observed (T cells were only 2-fold reduced in the absence of NCOR1) and expression of CD55 was similar on naive WT and NCOR1 cKOCd4 CD4+ T cells (Fig. S6c). Together, these data indicate that NCOR1 and HDAC3 might not synergistically regulate the survival of SP thymocytes. The differences in how the loss of NCOR1 and HDAC3 affects the dynamic expression of EGR2, CD127, BCL2 and BIM during positive selection and in positively selected thymocytes, as well as the important role for HDAC3 in T cell maturation clearly highlight unique functions for NCOR1 and HDAC3 in the regulation of SP thymocyte survival and the generation of the peripheral T cell compartment. NCOR1 and HDAC3 might be integrated in the same as well as in different transcription factor complexes at a given developmental stage and thus regulate common but also unique target genes at crucial developmental checkpoints. NCOR1 interacts with nuclear hormone receptors and with several BTB-ZF transcription factors3,5, and NCOR1 associates with other HDACs such as HDAC1, 4, 5 and 76. Thus, NCOR1 might recruit different repressor complexes via different types of transcription factors to target genes independently of HDAC3, which might have an impact on the survival of positively selected thymocytes. Moreover, NCOR1 has been linked to the metabolic regulation of cells3 and thus changes in these processes might also lead to reduced numbers of SP thymocytes. Further studies including RNA-seq and ChIP-seq experiments with WT, HDAC3-null and NCOR1-null thymocytes are required to dissect in more detail NCOR1 and HDAC3 mediated transcriptional networks that control T cell development.
In summary, our study identified NCOR1 as an important factor controlling T cell homeostasis by regulating the survival of positively selected thymocytes and thus the size of the peripheral T cell pool.
Methods
Animal models
Animal experiments were evaluated by the ethics committee of the Medical University of Vienna and approved by the Federal Ministry for Science and Research, Vienna, Austria (GZ:BMWF-66.009/0057-II/10b/2010; GZ:BMWF-66.009/58-II/10b/2010; GZ:BMWF-66.009/0103-WF/II/3b/2014; GZ:BMWF-66.009/0105-WF/II/3b/2014). Animal husbandry and experimentation was performed under the national laws (Federal Ministry for Economy and Science, Vienna, Austria) according to the guidelines of the Federation of Laboratory Animal Science Associations (FELASA), which match that of Animal Research: Reporting In Vivo Experiments (ARRIVE). Mice carrying a loxP-flanked (floxed) Ncor1 allele have been described8. Cd4-Cre mice were kindly provided by Dr. Chris Wilson. OT-II TCR transgenic mice were kindly provided by Dr. Stoiber-Sakaguchi (Medical University of Vienna). BCL2 transgenic mice32 were kindly made available by Dr. Jerry M. Adams and provided by Dr. Veronika Sexl (University of Veterinary Medicine, Vienna). BCL-xL transgenic mice33 were kindly provided by the late Stanley J. Korsmeyer. All mice analyzed were 6–8 weeks of age and of mixed sex unless otherwise stated. Littermate controls were used for the flow cytometry analysis within one experiment.
Generation of mixed bone marrow chimeric mice
Mixed BM chimeric mice were generated as previously described42. Six to eight weeks after transplantation, the reconstituted mice were sacrificed and analyzed by flow cytometry (LSRII or LSRFortessa, BD Biosciences).
Flow cytometry analysis
Thymii and spleens of mice were removed and placed into 6 well tissue culture plates containing staining buffer (2% v/v FCS in PBS). Single cell suspensions were made by passage of the tissue through a 70μm nylon cell strainer (Corning). Erythrocytes were removed with Pharmlyse (BD Biosciences). Cell suspensions were washed once with staining buffer and 2–5 × 106 cells were incubated with Fc-block (BD Pharmingen) and stained for 30 min with fluorophore-conjugated antibodies against various surface molecules. After the staining reaction, cells were washed once with staining buffer and acquired through LSRII or LSRFortessa (BD Biosciences) flow cytometer or prepared for intracellular staining. Data were analyzed using FlowJo software (Tree Star). Doublets were excluded from analysis.
Cell isolation for Ncor1 deletion PCR
CD4+ and CD8+ T cells were isolated from WT and NCOR1 cKOCd4 spleens by negative depletion of B cells, NK cells and myeloid cells using biotinylated antibodies (anti-mouse B220, NK1.1, CD11c, CD11b, Gr-1; eBioscience or BD Biosciences) prior to sorting. Naive T cells were purified as CD4+ or CD8+ CD62L+CD44−CD25− cells. DN, DP, CD4SP and CD8SP TCRβhi thymocyte subsets were sorted from WT and NCOR1 cKOCd4 thymii by using anti-CD4, anti-CD8α and anti-TCRβ antibodies. Subsequently, 1 × 105 cells were lysed in tail lysis buffer for 2 hrs at 55 °C. The Ncor1 deletion PCR was performed from the lysate.
Intracellular transcription factor staining
Intracellular detection of FOXP3, EGR2 and RORγt was performed with the FOXP3 Transcription Factor staining buffer set (eBioscience) according to the manufacturer’s instructions. Intracellular BCL2 staining was performed sequentially with Cytofix Fixation Buffer and Perm/Wash Buffer (both from BD Biosciences) according to the manufacturer’s instructions. Viability dye (eBioscience) was used to exclude dead cells from the analysis.
Intracellular BIM staining
Total thymocytes (8 × 106) were fixed with Cytofix Fixation buffer (BD Biosciences) and permeabilized with Perm/Wash buffer (BD Biosciences). Cells were incubated with rat anti-BIM in Perm/Wash buffer. Subsequently, cells were washed once and incubated with R-Phycoerythrin (R-PE) donkey anti-rat IgG in permeabilization buffer to reveal intracellular BIM staining by flow cytometry, T cell surface marker staining was performed following intracellular BIM staining. Viability dye (eBiosciences) was used to exclude dead cells from the analysis.
Antibodies used for flow cytometry
The following antibodies were used: from eBioscience: Anti-BrdU (clone Bu20A), anti-CD127 (A7R34), anti-CD4 (RM4–5), anti-CD8α (53–6.7), anti-EGR2 (erongr2), anti-FOXP3 (FKJ-16s), anti-TCR Vα2 (B20.1), anti-TCRβ (H57-597), anti-Vβ6 TCR (RR4-7), anti-Vβ8.1/Vβ8.2 TCR (Kj16-1333); from BD Biosciences: anti-active caspase 3 (C92-105), anti-CD4 (Gk1.5), anti-CD24 (M1/69), anti-CD16/CD32 (2.4G2), anti-CD44 (IM7), anti-CD45.1 (A20), anti-CD45.2 (104), anti-CD45R/B220 (RA3-6B2), anti-CD5 (53-7,3), anti-CD62L (MEL-14), anti-CD69 (H1.2F3), anti-RORγt (Q31-378); from Biolegend: anti-BCL2 (BCL/10C4).
In vivo SEB injections
Mice were injected (i.p.) with 10 μg staphylococcal enterotoxin B (SEB) (Sigma-Aldrich) (0.1 mg/ml in sterile PBS) on days 0, 2 and 4. Mice were sacrificed on day 7 and thymocytes were isolated, stained for surface markers and analyzed by flow cytometry.
Cleaved caspase 3 staining
Total thymocytes (3 × 106 cells/well of a 24 well plate) were activated for 24 h with plate-bound anti-CD3ε (1 μg/ml) and anti-CD28 (3 μg/ml) in 1 ml T cell medium (RPMI, GlutaMAX-I supplemented with 10% v/v FCS, antibiotics and 2-mercapthoethanol; all from Sigma-Aldrich) or left non-activated. After harvesting, thymocytes were stained with the various antibodies. Viability dye (eBioscience) was added before the surface staining to detect dead cells during the analysis. Intracellular cleaved caspase 3 staining was performed with Cytofix Fixation Buffer and Perm/Wash Buffer (BD Biosciences) according to the manufacturer’s instructions.
BrdU incorporation assay
Mice were injected (i.p.) with 1 mg BrdU (eBioscience or BD Pharmingen) (10 mg/ml in PBS). Thymocytes were isolated 24, 48, 72 or 96 hrs later and stained for surface markers. Subsequently, BrdU was detected with eBioscience BrdU Staining Kit for Flow cytometry or BD Pharmingen APC BrdU Flow Kit according to the manufacturer’s protocol.
Immunoblot analysis to detect BIM, BCL-xL and ERK1/2 expression
Thymocytes (5 × 106) were lysed in 25 μl RIPA buffer (25 mM Tris pH 8.0, 150 mM NaCl, 1.0% Triton-X, 0.1% SDS, 1% sodium deoxycholate, 1 mM EDTA) supplemented with complete protease inhibitors (Roche) and phosphatase inhibitors 1 mM Na3VO4 and 1 mM NaF. Proteins were separated on 12% SDS-polyacrylamide gels and electroblotted on AmershamTM HybondTM-ECL nitrocellulose membranes (GE Healthcare) according to standard protocols. Membranes were blocked in 5% (w/v) milk in PBST for 1 h and incubated with primary antibodies overnight. The following primary antibodies were used: rat anti-BIM (3C5/WEHI/Alexis), rabbit anti-BCL-xL (clone 54H6, Cell Signalling) and rabbit anti-ERK1/2 (clone 9102, Cell Signaling). All primary antibodies were diluted in 5% (w/v) milk in PBST. HRP-conjugated rabbit anti-rat IgG and goat anti-rabbit IgG (JacksonImmunoResearch Laboratories) were used as secondary antibodies. Immunoblots were developed using Western Bright ECL Spray (Advansta) and HRP chemiluminescence signals were detected with a Fujifilm LAS-4000 image analyzer (GE Healthcare) and analyzed with the Multi Gauge V3.0 software.
Immunoblot analysis to detect NCOR1 and α-Tubulin expression
Total thymocytes as well as sorted DP and CD4SP thymocytes (2 × 106) were lysed in 25 μl Carin Lysis buffer (20 mM Tris-HCl pH 8.0, 138 mM, NaCl, 10 mM EDTA, 1% Nonidet P-40, 10% glycerol) supplemented with complete protease inhibitors (Roche) and phosphatase inhibitors Na3VO4 (1 mM) and NaF (1 mM). Proteins were separated on 6% SDS-polyacrylamide gels and electroblotted on AmershamTM HybondTM-ECL nitrocellulose membranes (GE Healthcare) according to standard protocols. Membranes were blocked in 3% (w/v) milk in PBST for 1 h and incubated with primary antibodies for 3 hrs on room temperature. The following primary antibodies were used: rabbit polyclonal anti-NCOR1 (PA1-844A, Invitrogen), goat anti-NCOR1 (clone C-20, Santa Cruz) and mouse anti-α-Tubulin (clone DM1A, Sigma Aldrich). All primary antibodies were diluted in 3% (w/v) milk in PBST. HRP-conjugated goat anti-rabbit IgG and mouse anti-goat IgG (JacksonImmunoResearch Laboratories) were used as secondary antibodies. Immunoblots were developed using either Western Bright ECL Spray (Advansta) or Clarity Max Western ECL substrate (Bio Rad). HRP chemiluminescence signals were detected with a Fujifilm LAS-4000 image analyzer (GE Healthcare) and analyzed with the Multi Gauge V3.0 software.
Primers
The following primers were used: Ncor1 floxed and Δ allele: Ncor1 (#31), 5′- TTG GCC TTG GAG TAA ATG CTG TGA G; Ncor1 (#32), 5′- GGA AAC TAC CTA CCT GAA TCC ATG G; Ncor1 (#29) 5′- GAA CTA AGG ACA GGA AGG TAC AGG G. tgLck-BCL-xL: BCL-xL TG fwd, 5′- GCA TTC AGT GAC CTG ACA TC; BCL-xL TG rev, 5′-CTG AAG AGT GAG CCC AGC AGA CC. TgVav-BCL2: Vav BCL2 #1, 5′- ACG GTG GTG GAG GAG CTC TTC; Vav BCL2 #2, 5′- AAA ACC TTC CCA CAC CTC CCC CTG AA. Cd4-Cre: CD4-Cre F2, 5′-ACG GTA GTT TGT CTT TGG CAC C, CD4-Cre R2, 5′- CTT CTT GGG TGC CAT GCT CG.
Statistical analysis
No statistical methods were used to predetermine the sample size. The data shown indicate the mean. All experiments that required a statistical analysis were performed at least three times. The statistical analyses were performed using Prism Software (GraphPad Inc). As indicated in each figure legend, P-values were calculated with either an unpaired two-tailed Student’s t test (a normal distribution of data points was assumed; variances were assessed and if necessary an unpaired t-test with Welch’s correction was applied) or with an one sample t-test (columns statistics; Fig. 5g and Supplementary Fig. S4). No data were excluded and no specific randomization of animals or blinding of investigators was applied.
Electronic supplementary material
Acknowledgements
The work in the laboratory of W.E. was supported by the Austrian Science Fund (FWF) and MedUni Vienna doctoral program (DK W1212) “Inflammation and Immunity” and by FWF projects (P23641, P26193, I00698). S.S. was supported by FWF project P27747 and N.B. by FWF project P24265. A.V. acknowledges grant support by the FWF (I-1298). The studies in laboratory of J.A. were supported by Ecole Polytechnique Fédérale de Lausanne (EPFL), and Swiss National Science Foundation (310030B_160318).
Author Contributions
L.M. designed the research, performed most of the experiments, analyzed the data and wrote the manuscript; D.H., V.S., P.H., H.H., T.P. and N.B. performed some of the experiments; G.J.W. and A.V. provided reagents and analyzed data; S.S. analyzed data; J.A. provided mice; W.E. designed the research, analyzed the data and wrote the manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-017-15918-0.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Carpenter AC, Bosselut R. Decision checkpoints in the thymus. Nat Immunol. 2010;11:666–673. doi: 10.1038/ni.1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Perissi V, Jepsen K, Glass CK, Rosenfeld MG. Deconstructing repression: evolving models of co-repressor action. Nat Rev Genet. 2010;11:109–123. doi: 10.1038/nrg2736. [DOI] [PubMed] [Google Scholar]
- 3.Mottis A, Mouchiroud L, Auwerx J. Emerging roles of the corepressors NCoR1 and SMRT in homeostasis. Genes Dev. 2013;27:819–835. doi: 10.1101/gad.214023.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Horlein AJ, et al. Ligand-independent repression by the thyroid hormone receptor mediated by a nuclear receptor co-repressor. Nature. 1995;377:397–404. doi: 10.1038/377397a0. [DOI] [PubMed] [Google Scholar]
- 5.Jepsen K, Rosenfeld MG. Biological roles and mechanistic actions of co-repressor complexes. J Cell Sci. 2002;115:689–698. doi: 10.1242/jcs.115.4.689. [DOI] [PubMed] [Google Scholar]
- 6.Joshi P, et al. The functional interactome landscape of the human histone deacetylase family. Mol Syst Biol. 2013;9:672. doi: 10.1038/msb.2013.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jepsen K, et al. Combinatorial roles of the nuclear receptor corepressor in transcription and development. Cell. 2000;102:753–763. doi: 10.1016/S0092-8674(00)00064-7. [DOI] [PubMed] [Google Scholar]
- 8.Yamamoto H, et al. NCoR1 is a conserved physiological modulator of muscle mass and oxidative function. Cell. 2011;147:827–839. doi: 10.1016/j.cell.2011.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li P, et al. Adipocyte NCoR knockout decreases PPARgamma phosphorylation and enhances PPARgamma activity and insulin sensitivity. Cell. 2011;147:815–826. doi: 10.1016/j.cell.2011.09.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li P, et al. NCoR repression of LXRs restricts macrophage biosynthesis of insulin-sensitizing omega 3 fatty acids. Cell. 2013;155:200–214. doi: 10.1016/j.cell.2013.08.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Astapova I, et al. The nuclear corepressor, NCoR, regulates thyroid hormone action in vivo. Proc Natl Acad Sci USA. 2008;105:19544–19549. doi: 10.1073/pnas.0804604105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guidez F, et al. Reduced retinoic acid-sensitivities of nuclear receptor corepressor binding to PML- and PLZF-RARalpha underlie molecular pathogenesis and treatment of acute promyelocytic leukemia. Blood. 1998;91:2634–2642. [PubMed] [Google Scholar]
- 13.Melnick A, et al. Critical residues within the BTB domain of PLZF and Bcl-6 modulate interaction with corepressors. Mol Cell Biol. 2002;22:1804–1818. doi: 10.1128/MCB.22.6.1804-1818.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huynh KD, Bardwell VJ. The BCL-6 POZ domain and other POZ domains interact with the co-repressors N-CoR and SMRT. Oncogene. 1998;17:2473–2484. doi: 10.1038/sj.onc.1202197. [DOI] [PubMed] [Google Scholar]
- 15.Bilic I, et al. Negative regulation of CD8 expression via Cd8 enhancer-mediated recruitment of the zinc finger protein MAZR. Nat Immunol. 2006;7:392–400. doi: 10.1038/ni1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bilic I, Ellmeier W. The role of BTB domain-containing zinc finger proteins in T cell development and function. Immunology letters. 2007;108:1–9. doi: 10.1016/j.imlet.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 17.Ellmeier W, Taniuchi I. The Role of BTB-Zinc Finger Transcription Factors During T Cell Development and in the Regulation of T Cell-mediated Immunity. Curr Top Microbiol Immunol. 2014;381:21–49. doi: 10.1007/82_2014_374. [DOI] [PubMed] [Google Scholar]
- 18.Thapa P, et al. The transcriptional repressor NKAP is required for the development of iNKT cells. Nat Commun. 2013;4:1582. doi: 10.1038/ncomms2580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hsu FC, et al. Histone Deacetylase 3 Is Required for T Cell Maturation. J Immunol. 2015;195:1578–1590. doi: 10.4049/jimmunol.1500435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stengel KR, et al. Histone Deacetylase 3 Is Required for Efficient T Cell Development. Mol Cell Biol. 2015;35:3854–3865. doi: 10.1128/MCB.00706-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Philips RL, et al. HDAC3 Is Required for the Downregulation of RORgammat during Thymocyte Positive Selection. J Immunol. 2016;197:541–554. doi: 10.4049/jimmunol.1502529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wolfer A, et al. Inactivation of Notch 1 in immature thymocytes does not perturb CD4 or CD8T cell development. Nat Immunol. 2001;2:235–241. doi: 10.1038/85294. [DOI] [PubMed] [Google Scholar]
- 23.Bendelac A, Matzinger P, Seder RA, Paul WE, Schwartz RH. Activation events during thymic selection. J Exp Med. 1992;175:731–742. doi: 10.1084/jem.175.3.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Swat W, Dessing M, von Boehmer H, Kisielow P. CD69 expression during selection and maturation of CD4+8+ thymocytes. Eur J Immunol. 1993;23:739–746. doi: 10.1002/eji.1830230326. [DOI] [PubMed] [Google Scholar]
- 25.Yamashita I, Nagata T, Tada T, Nakayama T. CD69 cell surface expression identifies developing thymocytes which audition for T cell antigen receptor-mediated positive selection. Int Immunol. 1993;5:1139–1150. doi: 10.1093/intimm/5.9.1139. [DOI] [PubMed] [Google Scholar]
- 26.White J, et al. The V beta-specific superantigen staphylococcal enterotoxin B: stimulation of mature T cells and clonal deletion in neonatal mice. Cell. 1989;56:27–35. doi: 10.1016/0092-8674(89)90980-X. [DOI] [PubMed] [Google Scholar]
- 27.Grillot DA, Merino R, Nunez G. Bcl-XL displays restricted distribution during T cell development and inhibits multiple forms of apoptosis but not clonal deletion in transgenic mice. J Exp Med. 1995;182:1973–1983. doi: 10.1084/jem.182.6.1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Veis DJ, Sentman CL, Bach EA, Korsmeyer SJ. Expression of the Bcl-2 protein in murine and human thymocytes and in peripheral T lymphocytes. J Immunol. 1993;151:2546–2554. [PubMed] [Google Scholar]
- 29.Strasser A. The role of BH3-only proteins in the immune system. Nat Rev Immunol. 2005;5:189–200. doi: 10.1038/nri1568. [DOI] [PubMed] [Google Scholar]
- 30.Ma A, et al. Bclx regulates the survival of double-positive thymocytes. Proc Natl Acad Sci USA. 1995;92:4763–4767. doi: 10.1073/pnas.92.11.4763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yu Q, Erman B, Bhandoola A, Sharrow SO, Singer A. In vitro evidence that cytokine receptor signals are required for differentiation of double positive thymocytes into functionally mature CD8+ T cells. J Exp Med. 2003;197:475–487. doi: 10.1084/jem.20021765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ogilvy S, et al. Constitutive Bcl-2 expression throughout the hematopoietic compartment affects multiple lineages and enhances progenitor cell survival. Proc Natl Acad Sci USA. 1999;96:14943–14948. doi: 10.1073/pnas.96.26.14943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chao DT, et al. Bcl-XL and Bcl-2 repress a common pathway of cell death. J Exp Med. 1995;182:821–828. doi: 10.1084/jem.182.3.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Azzam HS, et al. CD5 expression is developmentally regulated by T cell receptor (TCR) signals and TCR avidity. J Exp Med. 1998;188:2301–2311. doi: 10.1084/jem.188.12.2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Willis SN, Adams JM. Life in the balance: how BH3-only proteins induce apoptosis. Curr Opin Cell Biol. 2005;17:617–625. doi: 10.1016/j.ceb.2005.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wojciechowski S, et al. Bim/Bcl-2 balance is critical for maintaining naive and memory T cell homeostasis. J Exp Med. 2007;204:1665–1675. doi: 10.1084/jem.20070618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hubner A, Barrett T, Flavell RA, Davis RJ. Multisite phosphorylation regulates Bim stability and apoptotic activity. Mol Cell. 2008;30:415–425. doi: 10.1016/j.molcel.2008.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhao Y, et al. Inhibitors of histone deacetylases target the Rb-E2F1 pathway for apoptosis induction through activation of proapoptotic protein Bim. Proc Natl Acad Sci USA. 2005;102:16090–16095. doi: 10.1073/pnas.0505585102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Inoue S, Riley J, Gant TW, Dyer MJ, Cohen GM. Apoptosis induced by histone deacetylase inhibitors in leukemic cells is mediated by Bim and Noxa. Leukemia. 2007;21:1773–1782. doi: 10.1038/sj.leu.2404760. [DOI] [PubMed] [Google Scholar]
- 40.Lauritsen JP, et al. Egr2 is required for Bcl-2 induction during positive selection. J Immunol. 2008;181:7778–7785. doi: 10.4049/jimmunol.181.11.7778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hsu FC, et al. Immature recent thymic emigrants are eliminated by complement. J Immunol. 2014;193:6005–6015. doi: 10.4049/jimmunol.1401871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hassan H, et al. Cd8 enhancer E8I and Runx factors regulate CD8alpha expression in activated CD8+ T cells. Proc Natl Acad Sci USA. 2011;108:18330–18335. doi: 10.1073/pnas.1105835108. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.