Abstract
Intracerebral hemorrhage is the deadliest, most disabling and least treatable form of stroke despite progression in medical science. The aim of the study was to analyze the frequency, risk factors, localization and 30-day prognosis in patients with intracerebral hemorrhage.
We analyzed 352 patients with intracerebral hemorrhage (ICH) hospitalized at the Department of Neurology Tuzla during a three-year follow up. The following data were collected for all patients in a computerized database: age, sex, risk factors (hypertension, heart diseases, diabetes and smoking) and CT findings. Stroke severity was estimated with Scandinavian Stroke Scale, ICH topography was specified by CT, and outcome at 1st month after onset included information on vital status and disability (modified Rankin Scale, mRS).
The most frequent risk factors were hypertension (84%), heart diseases (31%), cigarette smoking (28%) and diabetes mellitus (14%). The most frequent localization of ICH was multilobar (38%), internal capsule/basal ganglia region (36%) and lobar (17%). Within first month died 147 patients (42%). The highest mortality rate was in patients with brain stem (83%) and multilobar hemorrhage (64%). Factors independently associated with mortality were age (odds ratio 1,05 (95% confidence interval 1,02 to 1,08); p=0,001), stroke severity (OR 0,93 (0,92 to 0,95); p<0,0001), multilobar hemorrhage (OR 5,4 (3,0 to 9,6); p<0,0001) and intraventricular hemorrhage (OR 3,9 (2,2 to 7,1); p<0,0001). Favorable outcome at first month (mRS <2) had 45% of the surviving patients with ICH. The best outcome was for the patients with cerebellar hemorrhage (63%), while only 40% of the patients with hemorrhage in internal capsule/basal ganglia region had Rankin scale 2 or less.
Hypertension is the most frequent risk factor in patients with ICH. ICHs are mainly localized in lobar and internal capsule/basal ganglia regions. Independent predictors of mortality following ICH are age, hypertension, intraventricular blood extension and stroke severity. Mortality, as well as good outcome at 1 month, is related to the localization of bleeding.
Keywords: intracerebral hemorrhage, risk factors, prognosis
INTRODUCTION
Among all the neurological diseases of adult life, the cerebrovascular ones clearly rank first in frequency and importance. Despite considerable improvement in primary prevention, diagnostic workup and therapy, stroke is on the second or third place on a mortality list, and all projections indicate that this will remain in the year 2020. Furthermore, stroke is a leading cause of disability (1). In classifying the cerebrovascular diseases (CVD) it is most practical, from the clinical viewpoint, to preserve the classic division into ischemic stroke (IS), intracerebral hemorrhage (ICH), and subarachnoid hemorrhage (SAH). Intracerebral hemorrhage accounts 10% to 15% of all strokes, with an incidence of 10-20 per 100 000 and is more common in men. The high rates of mortality and morbidity with ICH are well recognized. The 30-day case fatality ranges from 25% to 50% and a majority of deaths occurs soon after the onset (2). The most frequent risk factor in ICH patients is hypertension and other risk factors are cigarette smoking, frequent use of alcohol and low cholesterol level. In evaluation of the outcome of ICH, size of hematoma and level of consciousness were found to be predictive outcome parameters (3). The roles of age, sex, hypertension, diabetes mellitus, cigarette smoking, exact location of bleeding and intraventricular blood extension are controversial. The aim of the study was to analyze the frequency, risk factors, localization and 30-day prognosis in patients with intracerebral hemorrhage.
PATIENTS AND METHODS
During a three-year follow up, from January 1st 2003. to December 31st 2005., 2555 patients with first ever stroke were admitted at the Department of Neurology Tuzla. There were 352 patients (13,8% of all strokes) with intracerebral hemorrhage (ICH). Upon admission demographic data, clinical and neurological examinations and laboratory tests were obtained. The following data were collected for all patients in a computerized database: age, sex, risk factors (hypertension, heart diseases, diabetes and smoking) and CT findings. Stroke severity was estimated with Scandinavian Stroke Scale (SSS) (4), ICH topography was specified by CT and outcome at 1st month after onset included information on vital status and disability (modified Rankin Scale, mRS) (5). Variables in relation to the region of hemorrhage included internal capsule, basal ganglia, cerebellum, brainstem, lobar, multilobar topographic involvements and intraventricular blood extension. Prognosis was assessed as mortality at 30 days after ICH, and favorable outcome of the surviving patients as mRS 2 or less. Univariate analysis for each variable (demographic data, risk factors and neuroimaging findings) was analyzed using chi-square test and student’s t-test. Variables that were significantly related to mortality (p<0,05) or with a p-val- ue of less than 0,3 in univariate analysis were subjected to multivariate analysis with a logistical regression procedure. A value of p<0,05 was considered to be significant.
RESULTS
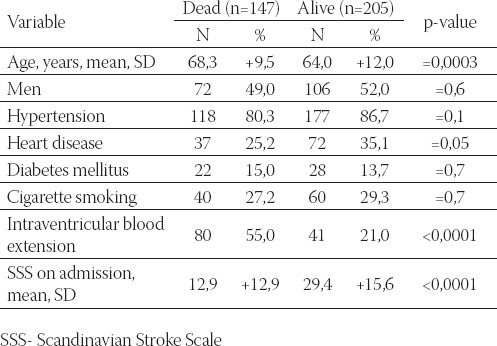
Out of 352 patients with ICH, 178 (50,6%) were men. The mean age of ICH patients was 65,7+11,2 years and women were significantly older comparing with men. The most frequent risk factors were hypertension (84%), heart diseases (31%), cigarette smoking (28%) and diabetes mellitus (14%) with some differences according to sex (Table 1). There were no differences in stroke severity on admission and hospital stay between men and women. Within first month died 147 patients (42%), 37 (25%) died within 24 hours form the onset. The localization of intracerebral hemorrhage was showen in Table 2. The most frequent localization was internal capsule/basal ganglia and multilobar. Analysis according to the site of bleeding showed significant differences with regard to mortality. The highest mortality rate was in patients with brain stem hemorrhage (83,3%), multilobar hemorrhage (64,4%) and lobar hemorrhage (31,7%). However, the lowest mortality within 30-day was in patients with internal capsule/basal ganglia hemorrhage (22,8%) and cerebellar hemorrhage (15,8%). Table 3. shows univariate analysis in among 352 patients with intracerebral hemorrhage, of whom 145 died. Deceased patients were significantly older, more often had intraventricular blood extension and had more severe deficit on admission than patients who survived first month.
TABLE 1.
General characteristics and risk factors of patients with intracerebral hemorrhage according to sex

TABLE 2.
Distribution of patients with intracerebral hemorrhage according to localization
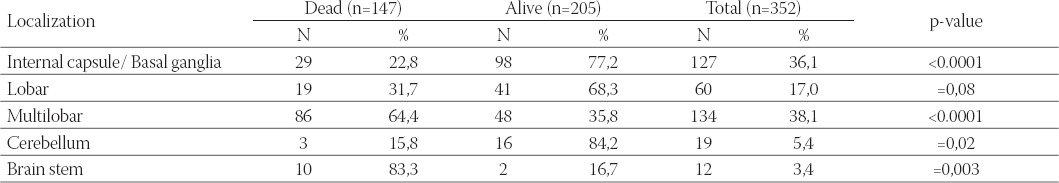
TABLE 3.
Univariate analysis in patients with intracerebral hemorrhage according to vital status at first month
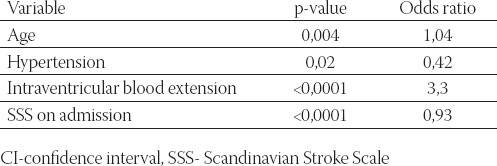
After multivariate analysis, age, hypertension, intraventricular blood extension and low Scandinavian Stroke Scale score on admission were independent factors for morality within 30-day after ICH (Table 4).
TABLE 4.
Independent predictors of 30-day mortality in patients with intracerebral hemorrhage
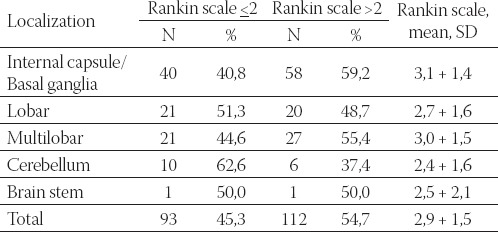
Mean value of the Rankin scale at first month for surviving patients was 2,9, which means that majority of the patients were able to walk without assistance. Favorable outcome at first month had 45% of the surviving patients with ICH. The best outcome was for the patients with cerebellar hemorrhage (62,6%), while only 40% of the patients with hemorrhage in internal capsule/ basal ganglia region had Rankin scale 2 or less (Table 5).
TABLE 5.
Outcome of surviving patients with intracerebral hemorrhage at first month according to localization
DISCUSSION
Intracerebral hemorrhage is the deadliest, most disabling and least treatable form of stroke despite progression in medical science. The frequency of ICH in this study (13,8%) is double lower than in the previously analyzed period (1996-2000) (6). Improvement in detection, better control and treatment of hypertension are the main reasons for the reduction of ICH frequency in our region. Hypertension was the most frequent vascular risk factor in patients with ICH (83%) followed by heart disease (31%), smoking (28%) and diabetes (14%) (Table 1). Other authors also reported hypertension as the most frequent vascular risk factor in patients with ICH while the frequency of other risk factors varied from study to study (7,8). Mortality at first month was 42% and 25% of deaths occurred in the first day. These results correlated with some previous reports. In the study of Karnik, Valentin and Ammerer (9) ICH mortality within first month was 49,6%, 37% died during the first 4 days after the acute event. At the other hand, in the study of Nilsson et al. (10) mortality rate among 341 cases of primary ICH was 36% at the 30-day. In the period 1996-2000 30-day ICH mortality at our region was 55% (6) and in this study was lower (42%). We think that treating of stroke as emergency and treatment of ICH according to the European Stroke Initiative (EUSI) recommendations played the leading role in the reduction of ICH mortality at our region. In our study multilobar involvement (38,1%) and internal capsule/basal ganglia (36,1%) were the most frequent sites of bleeding, and the site of bleeding had influence on the mortality (Table 2). Localization of ICH was similar in the study of Rosenow et al. (11). It this study main localizations were cerebral lobes in 49,2% and basal ganglia in 34,4% of the patients. Authors also suggested a difference in mortality according to the site of bleedeing. Togha and Bakhtavar (8) found that internal capsule/basal ganglia (28,6%) and lobar hematoma (25,4%) were more frequent sites of ICH than other regions. This study indicated significantly higher mean age among deceased patients without sex differences in mortality rate. Even though diabetes mellitus was often reported as independent factor on mortality rate among ICH patients (8,12), we could not supported this thesis. Our findings confirmed previously reported results that intraventricular blood extension and severity of ICH on admission can be predictors for death (8,13). We also found age and hypertension as independent predictors of 30-day mortality (Table 4). Rosenow et al. (11) reported that a higher case fatality correlated with ventricular extension, increasing age, surgical treatment, localization in basal ganglia and hypertension as only etiology. In the recent publication of Ruiz-Sandoval et al. (14) independent predictors of death followed ICH were age, Glasgow Coma Scale, ICH location, ICH volume, and intraventricular extension. Favourable outcome (mRS <2) at first month had 93 patients (45%) and it depended of the localization of hemorrhage (Table 5). The best outcome had patients with cerebellar bleeding and lobar ICH, while less than 50% of surviving patients with multilobar ICH and internal capsule/basal ganglia hemorrhage had favorable outcome at first month. Mortality in patients with internal capsule/basal ganglia hemorrhage within 30-day was the lowest (23%) but only 40% of them had mRS <2 at 1 month. Lampl et al. (15) reported worse functional outcome in putaminocapsular and lobar bleeding. In the study of Barber et al. (16) poor outcome at 30 days after ICH (dead or mRS at least 3) had 79% of the patients, while only 22% of survivors had mRS less than 3.
CONCLUSION
Hypertension is the most frequent risk factor in patients with ICH, followed with heart disease and cigarette smoking. ICHs are mainly localized in lobar and internal capsule/basal ganglia regions. Independent predictors of mortality following ICH are age, hypertension, intraventricular blood extension and stroke severity. Mortality, as well as good outcome at one month, is related to the localization of bleeding.
LIST OF ABBREVIATIONS
CVD - cerebrovascular diseases
IS - ischemic stroke
ICH - intracerebral hemorrhage
SAH - subarachnoid hemorrhage
CT - computed tomography
SSS - Scandinavian Stroke Scale
mRS - modified Rankin Scale
SD - standard deviation
CI - confidence interval
EUSI - European Stroke Initiative
REFERENCES
- 1.Warlow C. Epidemiology of stroke. Lancet. 1998;352(suppl III):1–4. doi: 10.1016/s0140-6736(98)90086-1. [DOI] [PubMed] [Google Scholar]
- 2.Dennis M.S. Outcome after brain hemorrhage. Cerebrovasc. Dis. 2003;16(suppl 1):9–13. doi: 10.1159/000069935. [DOI] [PubMed] [Google Scholar]
- 3.Garibi J, Bilbao G, Pomposo I, Hostalot C. Prognostic factors in a series of 185 consecutive spontaneous supratentorial intracerebral haematomas. Br. J. Neurosurg. 2002;16:355–361. doi: 10.1080/0268869021000007579. [DOI] [PubMed] [Google Scholar]
- 4.Boysen G. The Scandinavian Stroke. Scale. Cerebrovasc. Dis. 1992;2:239–247. doi: 10.1159/000086280. [DOI] [PubMed] [Google Scholar]
- 5.Rankin J. Cerebral vascular accidents in patients over the age of 60, II: prognosis. Scott. Med. J. 1957;2:200–215. doi: 10.1177/003693305700200504. [DOI] [PubMed] [Google Scholar]
- 6.Smajlović Dž, Ibrahimagić O, Dostović Z, Tupković E, Sinanović O. Main epidemiological characteristics of cerebro-vascular diseases at the Department of neurology Tuzla during a five-year post-war period (1996-2000) Acta Clin. Croat. 2002;41(suppl 3):57. [Google Scholar]
- 7.Ariesen M.J, Claus S.P, Rinkel G.J.E, Algra A. Risk factors for intarcerebral hemorrhage in the general population: a systematic review. Stroke. 2003;34:2060–2065. doi: 10.1161/01.STR.0000080678.09344.8D. [DOI] [PubMed] [Google Scholar]
- 8.Togha M, Bakhtavar K. Factors associated with in-hospital mortality following intracerebral hemorrhage: a three-year study in Teheran, Iran. BMC Neurology. 2004;4:9. doi: 10.1186/1471-2377-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karnik R, Valentin A, Ammerer H.P. Outcome in patients with intracerebral hemorrhage;predictor of survival. Wien Klin. Wachenscher. 2000;112(4):169–173. [PubMed] [Google Scholar]
- 10.Nilsson O.G, Lindgren A, Brandt L, Säveland H. Prediction of death in patients with primary intracerebral hemorrhage: a prospective study of a defined population. J Neurosurg. 2002;97(3):531–536. doi: 10.3171/jns.2002.97.3.0531. [DOI] [PubMed] [Google Scholar]
- 11.Rosenow F, Hojer C, Meyer-Lohmann C, Hilgers R.D, Mühlhofer H, Kleindienst A, Owega A, Köning W, Heiss W.D. Spontaneous intracerebral hemorrhage. Prognostic factors in 896 cases. Acta Neurol. Scand. 1997;96(3):174–182. [PubMed] [Google Scholar]
- 12.Arboix A, Massons J, Garcia-Eroles L. Diabetes is an independent risk factor for in-hospital mortality from acute spontaneous intracerebral hemorrhage. Diabetes Care. 2000;23(10):1527–1531. doi: 10.2337/diacare.23.10.1527. [DOI] [PubMed] [Google Scholar]
- 13.Cheung R.T.F, Yuzou L. Use of original, modified, or new intracerebral hemorrhage score to predict mortality and morbidity after intracerebral hemorrhage. Stroke. 2003;34:1717–1724. doi: 10.1161/01.STR.0000078657.22835.B9. [DOI] [PubMed] [Google Scholar]
- 14.Ruiz-Sandoval J.L, Chiquete E, Romero-Vargas S, Padilla-Martínez J.J, González-Cornejo S. Grading scale for prediction of outcome in primary intracerebral hemorrhages. Stroke. 2007;38(5):1641–1644. doi: 10.1161/STROKEAHA.106.478222. [DOI] [PubMed] [Google Scholar]
- 15.Lampl Y, Gilad R, Sarova-Pinhas Y.E.I. Neurological and functional outcome in patients with supratentorial hemorrhages. Stroke. 1995;26:2249–2253. doi: 10.1161/01.str.26.12.2249. [DOI] [PubMed] [Google Scholar]
- 16.Barber M, Roditi G, Stott D.J, Langhorne P. Poor outcome in primary intracerebral haemorrhage: results of a matched comparison. Postgrad. Med. J. 2004;80:89–92. doi: 10.1136/pmj.2003.010967. [DOI] [PMC free article] [PubMed] [Google Scholar]


