Abstract
The aim of this study was to analyze cognitive dysfunction in PTSD. The testing included 79 Bosnian Army veterans, who participated in Bosnian war from 1992 to 1995. Out of 79 tested war veterans, 45 of developed PTSD while 34 did not. The veterans without PTSD where included in the control group. All the war veterans were of the same education level (secondary education) and between 30 and 50 years of age. Rivermead Behavioral Memory Test - RBMT was applied to all the subjects. The test was originally developed for the purpose of everyday memory problems identification. Clear goal of the 10 RBMT subtests is simulation of everyday life situations. PTSD group achieved significantly lower results than the control group. Results of the total score showed highly significant difference between PTSD and control group. Value of the t-test is t=10,056 with significance level of p<0,001. The same conclusion stands for any RBMT subtest. Numerous psychological studies on PTSD patients show more prominent psychological deficit in war veterans. Our study clearly confirms that finding.
Keywords: posttraumatic stress disorder, memory, trauma, war veterans, RBMT
INTRODUCTION
One possible explanation for the variety and size of neuropsychological cognitive function deficits in PTSD persons may be that PTSD, acting through different mechanisms, influences large number of cognitive functions, which are controlled by different parts of the brain. Alternative explanation acceptable to us would be that PTSD influences central, higher level of attention control mechanisms such as central executive (2) or supervisory attention system (9) that control lower level systems that are more closely related to memory and attention. From this prospective, memory disorders revealed by RBMT are more of a superficial coding function or coding disturbance kind (that is the 1st phase of memory) and not memory deficit per se (Figures 1 and 2). Overwhelming anxiety might be the main cause behind this pathological status of stress and inability to concentrate. Increased anxiety and excitement are well known to interfere with different cognitive functions (1,5,8). As already mentioned, PTSD is linked to changes in neurobiological markers, where anxiety may result from increased level of cerebrospinal noradrenalin (6,10).
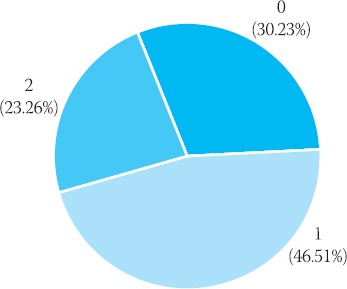
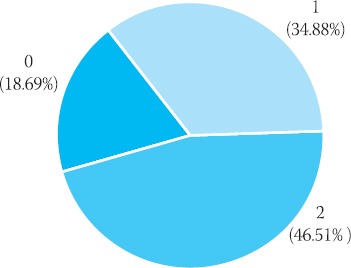
FIGURE 1.
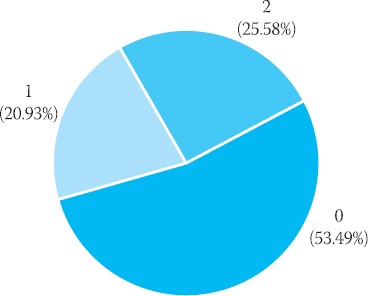
RBMT-remembering names/PTSD group
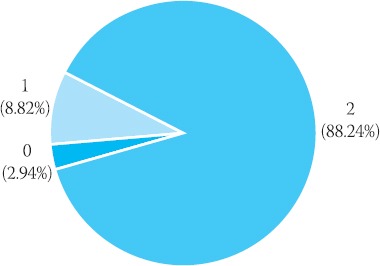
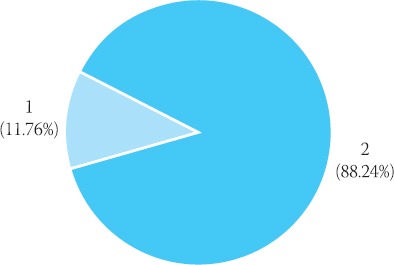
FIGURE 2.
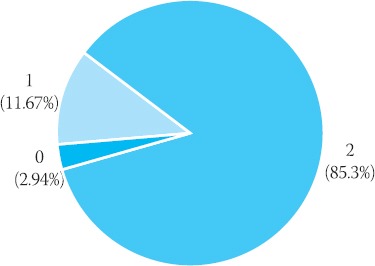
RBMT - remembering names / Control group
χ2 = 30,244 with level of significance of p < 0,001.
SUBJECTS AND METHODS
The study included 79 Bosnian Army veterans, who participated in Bosnian war from 1992 to 1995. Out of 79 veterans, 45 developed PTSD while 34 did not. The veterans without PTSD where included in the control group. All 79 war veterans were of the same education level (secondary education) and were between 30 and 50 years of age. Rivermead Behavioral Memory Test - RBMT was applied to all the subjects. The test was originally developed for the purpose of everyday memory problems identification. RBMT clearly aims at simulation of everyday life situations and consists of 10 subtests:
remembering names,
remembering the hiding places of certain things,
remembering a meeting,
recognizing pictures,
remembering a story,
remembering a short direction of movement,
remembering a message,
orientation,
date,
recognizing faces.
In selecting PTSD patients we adhered to the DSM IV classification scheme. PTSD evaluation is based on MISSISSIPPI SCALE (7). All the patients that were included into this study had MISSISSIPPI SCALE score of 110 (7). Thus, duration of symptoms was considered in patients selection. Only chronic PTSD was taken into account. Patients who either experienced head injury or surgical treatment or had a history of neurological disorders, psychotic disorders, alcohol or drug abuse were excluded from the study. PTSD group was examined either at PTSD section of University of Sarajevo Clinics Centre Psychiatric Clinic or at Mental Health Centers of the Sarajevo Canton Public Healthcare Institution. Participants without PTSD were examined at the Home Office outpatient section. They reported to the doctor’s office for various reasons (in most cases to obtain health certificate).
RESULTS
PTSD characteristics are intense memory of the trauma details (trauma memory), memory gaps, flashbacks and nightmares. These types of memory disorders are all linked to the experienced trauma. Memory gaps are, most likely, a consequence of damage in the process of transfer of information from working memory to long-lasting memory (Figures 5 and 6). Traumatic stress actually disrupts the whole process of encoding the information from working to long-lasting memory. Thus, the issue is not forgetting the event but disorder in remembering that occurs in the moment of particular event or immediately after it.
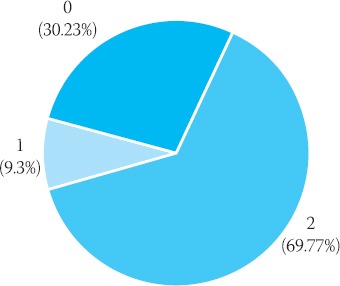
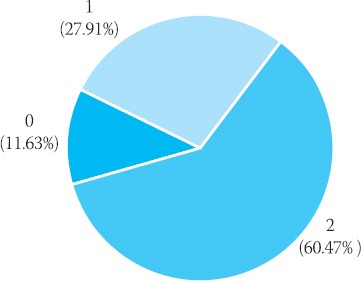
FIGURE 3.
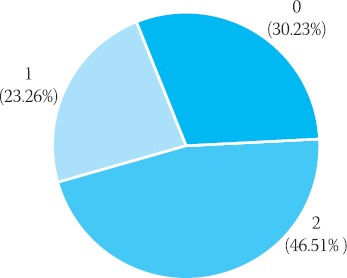
RBMT - remembering a place / PTSD group
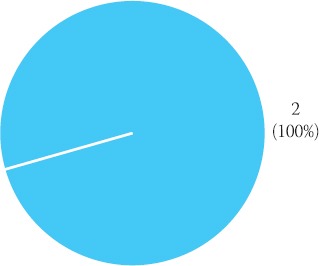
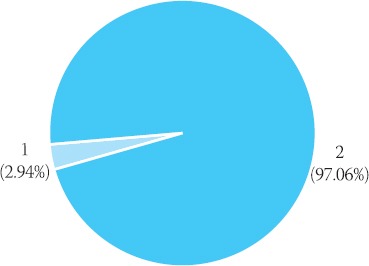
FIGURE 4.
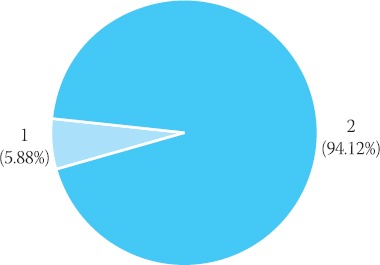
RBMT - remembering a place / Control group
FIGURE 5.
RBMT - Remembering a story/ immediate memory/ PTSD group
FIGURE 6.
RBMT - Remembering a story/ immediate memory/ Control group
FIGURE 7.
RBMT - Remembering a story/ prolonged memory/ PTSD group
FIGURE 8.
RBMT - Remembering a story /prolonged memory/Control group
FIGURE 9.
RBMT - Remembering a short direction of movement/ immediate memory/ PTSD group
FIGURE 10.
RBMT - Remembering a short direction of movement/ immediate memory/ Control group
FIGURE 11.
RBMT - Remembering a short direction of movement/ delayed memory/ PTSD-group
FIGURE 12.
RBMT - Remembering a short direction of movement/ delayed memory/ Control group
χ2 = 20,543 with level of significance of p < 0,001.
χ2 = 14,613 with level of significance of p < 0,01.
χ2 = 12,143 with level of significance of p < 0,01.
χ2 = 14,872 with level of significance of p < 0,01.
χ2 = 11,669 with level of significance of p < 0,01.
RBMT test is too simple for the participants with no memory problems. It is not sensitive enough for differentiation of tiny differences in memory capacity within the same group. It is, however, very sensitive for patients with damaged memory functions.
Substandard results of immediate (short-term) memory were observed in PTSD group. This probably indicates limitations in memory consolidation in PTSD patients.
DISCUSSION
The main goal of our research was to examine cognitive functions of individuals diagnosed with PTSD. Based on the results of previous studies and theoretical background we expected test performance of individuals with PTSD to be inferior to those of persons without PTSD diagnosis (Table 1). In a few studies, researchers concluded that PTSD is linked to memory deficit (4). PTSD patients, who participated in our study also, showed deficit in all RBMT subtests (Graph 1-12). According to RBMT test results, it can be stated that subjects that suffer from PTSD have damaged explicit, immediate and prolonged memory. Since RBMT was deliberately developed to predict memory problems in everyday life, significantly lower performance of persons with PTSD in almost all sub-tests indicate that they encounter large and different memory problems in everyday activities. How classical memory tests that are based on implementation and retention of experimental materials are related to everyday life problems is generally not well understood (3). Therefore, RBMT was developed and its results are considered a good evaluation of everyday memory.
TABLE 1.
RBMT - Rivermead behavioral memory test
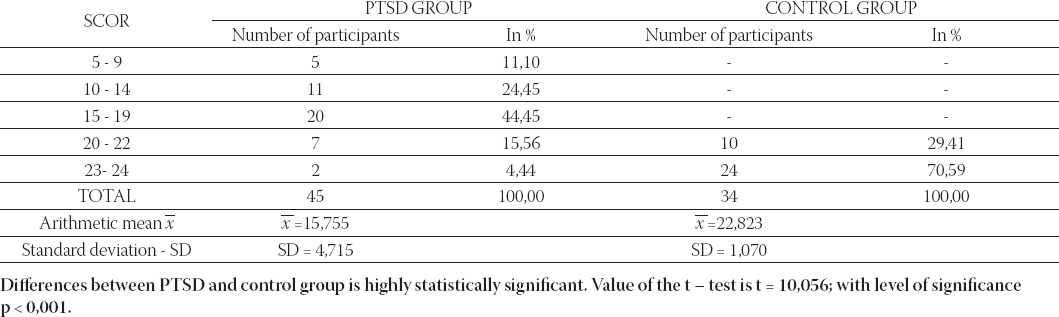
When comparing the differences in the results of neuropsychological testing of cognitive functions obtained between experimental and control group with similar studies (11,12), we can state that deficits present in our participants are more pronounced and pertain to all aspects of memory and attention aspects (Table 1). In the above mentioned studies only certain aspects of cognitive functions are affected while other remained unchanged. Only the results of studies performed on Vietnam War veterans indicated significant degradation of cognitive functions (3). It seems possible that variety and scope of neuropsychological symptoms, which are found in our participants, may be related to a very specific type of trauma. Earlier studies were performed on Vietnam War veterans who experienced trauma 30 years ago, while only 10 years elapsed from traumatic experiences of our participants. Besides, our participants were constantly exposed to war related stress for 4 years all the while having to take care about their loved ones who were in constant danger as well. Also, inadequate posttraumatic care and lack of relevant treatment might cause such results.
CONCLUSION
The results of this study confirmed connection between PTSD and degradation of cognitive function. The results are obtained using focused neuropsychological instrument that does not allow for differentiation among memory components involved in everyday situations.
Persons with PTSD have diminished short term memory capacity.
Persons with PTSD have affected verbal intellectual capability.
Compared to the control group, persons with PTSD achieve significantly worse results in tests that measure explicit, long-term, delayed and immediate memory.
In comparison to the control group, persons with PTSD achieve significantly lower results in tests that measure focused attention, maintained attention and cognitive flexibility.
ACKNOWLEDGMENTS
The authors would like to express their gratitude to Miss. Stefica Sergetlija for help with statistical analyses.
REFERENCES
- 1.Ashcraft M.H, Kirk E.P. The relationships among working memory, math anxiety and performance. Journal of Experimental Psychology: General. 2001;130:224–237. doi: 10.1037//0096-3445.130.2.224. [DOI] [PubMed] [Google Scholar]
- 2.Baddeley A. The episodic buffer: a new component of working memory? Trends in Cognitive Sciences. 2000;11:417–423. doi: 10.1016/s1364-6613(00)01538-2. [DOI] [PubMed] [Google Scholar]
- 3.Bremner J.D. Does stress damage the brain. Biological Psychiatry. 1999;45:797–805. doi: 10.1016/s0006-3223(99)00009-8. [DOI] [PubMed] [Google Scholar]
- 4.Elzing B.M, Bremner J.D. Are the neural substrates of memory the final common pathway in posttraumatic stress disorder (PTSP) Journal of Affective Disorders. 2002;70:1–17. doi: 10.1016/s0165-0327(01)00351-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eysenck M.W. Anxiety and Cognition: Theory and Research. In: Archer T, Nilsson LG, editors. Aversion, Avoidance and anxiety, perspectives on aversively motivated behavioral. New Jersey: Lawrence Erlbaum Associates; 1989. pp. 323–334. [Google Scholar]
- 6.Geracioti T.D, Baker D.G, Ekhator N.N, West S.A, Hill K.K, Bruce A.B, Schmidt D, Rounds-Kugler B, Yehuda R, Keck P.E, Kasckow J.W. CSF norepinephrine concentrations in post-traumatic stress disorder. Am. J. Psych. 2001;158:1227–1229. doi: 10.1176/appi.ajp.158.8.1227. [DOI] [PubMed] [Google Scholar]
- 7.Keane T.M, Caddell J.M, Taylor K.L. Mississippi scale for combat related posttraumatic stress disorder: three studies in reliability and validity. J. Consult. Clin. Psychol. 1988;56(1):85–90. doi: 10.1037//0022-006x.56.1.85. [DOI] [PubMed] [Google Scholar]
- 8.Robbins T.W. Arousal systems and attentional processes. Biological Psychiatry. 1997;45:57–71. doi: 10.1016/s0301-0511(96)05222-2. [DOI] [PubMed] [Google Scholar]
- 9.Shallice T. From Neuropsychology to Mental Structure Cambridge. New York: University Press; 1998. [Google Scholar]
- 10.Southwick S.M, Bremner J.D, Rasmusson A, Morgan CA, Arnsten A, Charney D.S. Role of norephrine in the patophysiology and treatment of posttraumatic stress disorder. Biological Psychiatry. 1999;46:1192–1204. doi: 10.1016/s0006-3223(99)00219-x. [DOI] [PubMed] [Google Scholar]
- 11.Stein M.B, Kennedy C.M, Twamley E.W. Neuropsychological function in female victims of intimate partner violence with and without posttraumatic stress disorder. Biological Psychiatry. 2002;52:1079–1088. doi: 10.1016/s0006-3223(02)01414-2. [DOI] [PubMed] [Google Scholar]
- 12.Vasterling J.J, Brailey K, Constans I.J, Sutker P.B. Attention and memory dysfunction in posttraumatic stress disorder. Neuropsychology. 1998;12:125–133. doi: 10.1037//0894-4105.12.1.125. [DOI] [PubMed] [Google Scholar]
- 13.Wilson B, Cockburn J, Baddeley A, Hiorns R. The development and validation of a test battery for detecting and monitoring everyday memory problems. J. Clin. Exp. Neuropsychol. 1989;11:855–870. doi: 10.1080/01688638908400940. [DOI] [PubMed] [Google Scholar]


