Abstract
Objective
To evaluate the Weill Cornell Medical College (WCMC)/New York Presbyterian Hospital (NYPH) experience with intraoperative frozen (IOF) section in the management of thyroid nodules with a fine needle aspiration (FNA) diagnosis of Bethesda II–VI and to analyze the cost and pathology benefit it provides.
Methods
The surgical and cytopathology files at WCMC/NYPH were searched within the time period of January 2008 to May 2013. A total of 435 thyroid specimens were identified for which both an FNA and subsequent IOF section was performed. The FNA was correlated with the locations of the resected nodule and the nodule frozen for intraoperative diagnosis. The results of the FNA were compared to the IOF section diagnosis and final diagnosis (FD).
Results
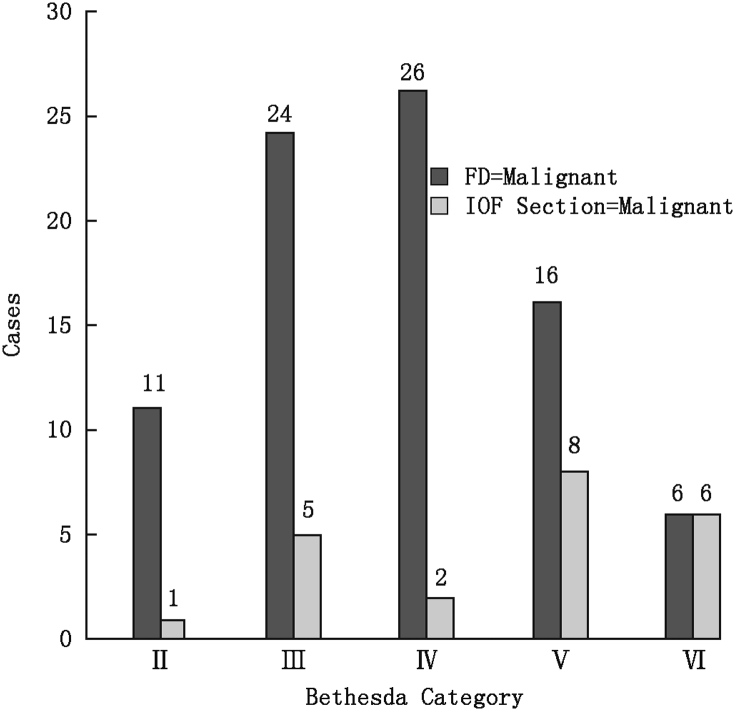
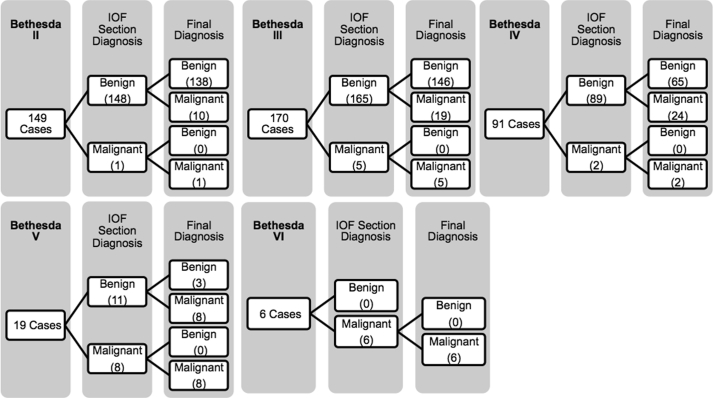
Among 435 cases, the FNA diagnosis was Bethesda II: 149 cases, Bethesda III: 170 cases, Bethesda IV: 91 cases, Bethesda V: 19 cases, and Bethesda VI: 6 cases. There were a total of 83 carcinomas identified on FD, which included 69 papillary thyroid carcinomas (PTCs), 12 follicular carcinomas, and 2 poorly differentiated carcinomas. The preoperative FNA diagnosis for these carcinomas was as follows: Bethesda II, 11/149 (7.4%), Bethesda III, 24/170 (14%), Bethesda IV, 26/91 (29%), Bethesda V, 16/19 (84%), and Bethesda VI, 6/6 (100%). IOF section contributed to the diagnosis of malignancy in 16/429 (4%) cases: 1/149 (0.7%) Bethesda II, 5/170 (3%) Bethesda III, 2/91 (1.1%) Bethesda IV, and 8/19 (42%) Bethesda V. The diagnosis of malignancy was confirmed in the 6 Bethesda VI cases by IOF section. There were no false positives on IOF section. IOF had a sensitivity and specificity of 26% and 100%, respectively.
Conclusion
The role of IOF section is limited in the evaluation of thyroid nodules. IOF section is most useful for nodules with an FNA diagnosis of Bethesda V lesions. The diagnosis of follicular variant of PTC remains difficult on frozen section.
Keywords: Thyroid, Nodule, Frozen section, Fine-needle aspiration, Sensitivity, Specificity
Introduction
Affecting 4%–7% of the general population, palpable thyroid nodules are common.1 The incidence of thyroid cancer has nearly tripled from 4.9 to 14.3 per 100,000 individuals over a thirty-five year period ending in 2009.2 Such a high incidence mandates a cost-effective and efficient method for the preoperative evaluation of thyroid nodules. Fine needle aspiration (FNA) has emerged as a cornerstone modality in the preoperative management of thyroid lesions because of its reported high accuracy, specificity, cost-utility and low false negative rate. The widespread utilization of FNA has driven a significant reduction in unnecessary thyroidectomies worldwide as well as a decrease in the use of intraoperative frozen (IOF) sections.3 In many cases, FNA provides a definitive benign or malignant diagnosis and effectively facilitates the planning of surgical and therapeutic treatment. Among thyroid nodules that undergo FNA, about 65% are classified as benign, 8% as malignant, and 3% as suspicious for malignancy.4
Nevertheless, there are several limitations of thyroid FNA due to the nature of the procedure, the large variety of pathologies that may arise in the thyroid gland—some of which cannot be diagnosed based on cytologic features alone—and the subjectivity inherent to the interpretation of samples. Inspired by the Bethesda system for reporting cervical cytology widely used for reporting Pap smear results, the Bethesda Criteria for Reporting Thyroid Cytopathology were published in 2009 in order to help standardize FNA reporting (Table 1).5 Importantly, the system also recommends supplemental studies such as immunohistochemistry and molecular analysis that may aid in diagnosis, links each of the six diagnostic categories to an implied risk of malignancy, and provides clinical management guidelines ranging from clinical surveillance to near-total thyroidectomy.5
Table 1.
The Bethesda system for reporting thyroid cytopathology, adapted from Cibas and Ali.5
| Bethesda category |
|---|
Virtually acellular neoplasm |
Lymphocytic (Hashimoto) thyroiditis Granulomatous (subacute) thyroiditis |
|
|
Suspicious for medullary carcinoma Suspicious for metastatic carcinoma Suspicious for lymphoma |
Poorly differentiated carcinoma Medullary thyroid carcinoma Anaplastic carcinoma Squamous cell carcinoma Carcinoma with mixed features Metastatic carcinoma Non-Hodgkin lymphoma |
Although FNA is most often the diagnostic modality of choice in the management of thyroid nodules, the results are indeterminate (classified as “unsatisfactory”, “atypical cellular lesions”, “follicular neoplasm”, or “suspicious for malignancy”) in about 30% of cases.4 FNA is especially inadequate at distinguishing between follicular adenoma and follicular carcinoma because the determination of malignancy for follicular lesions requires histologic evidence of vascular and/or capsular invasion.6 In cases of thyroidectomy, IOF section is often used to aid further surgical decision-making at the operating table but its usefulness in the management of thyroid nodules after an FNA has already been performed continues to be debated.
Some previous studies do not support the use of IOF section especially when the FNA is interpreted as a Bethesda 4 (“follicular neoplasm or suspicious for a follicular neoplasm”) or 5 (“suspicious for malignancy”) secondary to concerns regarding increased cost and operative time7, 8, 9 while others support the use of IOF section to confirm malignant FNA reports, to detect false-positive FNAs and to evaluate thyroid nodules with indeterminate cytologies.1, 10 Those who support the use of IOF section at the time of hemithyroidectomy emphasize its potential to help surgeons avoid unnecessary staged completion thyroidectomy.11 Notably, most previous studies evaluating the utility of FNA and IOF section in the management of thyroid nodules were performed prior to the establishment of the Bethesda system for reporting thyroid FNAs. The objective of this study was to evaluate our institutional experience with IOF section in the management of thyroid nodules with a FNA diagnosis of Bethesda II–VI and to consider the cost and pathology benefit it provides.
Materials and methods
This retrospective assessment was approved by the WCMC Institutional Review Board. All data was obtained as per the IRB protocol and data was analyzed using Microsoft Excel for Mac 2011 software. Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS version 16.0, Chicago, IL, USA). A review of the cytopathology and surgical files from January 2008 through May 2013 at Weill Cornell Medical College was performed to identify cases evaluated for a thyroid nodule. These cases were generally performed with US guidance, although all lesions undergoing FNA, whether US was used or not were considered. Our inclusion criteria required that a FNA diagnosis of Bethesda II–VI be reported and subsequent IOF section be performed. The FNA was correlated with the locations of the resected nodule and of the nodule frozen for intraoperative diagnosis. Our exclusion criteria included nondiagnostic/unsatisfactory FNA samples (Bethesda I) and incidental microcarcinomas.
IOF section specimen was classified as “negative” if the pathologist reported “benign”, “follicular lesion”, or “nodular hyperplasia”. IOF section was classified as positive if malignancy was detected. FD was classified as either benign or malignant. The FNA results for each case were compared to the IOF section diagnosis and the FD. The sensitivity and specificity of IOF section and FNA were calculated with respect to the FD. The pathology charge at WCMC for performing an IOF section is $251 per specimen, including materials and professional fees only. Additional costs were not considered. We assessed the cost-effectiveness of performing an IOF section for thyroid nodules by determining the additional pathology charge per additional information provided.
IOF were performed by all pathologists, including the head & neck pathologist, on a weekly basis. Head & neck pathologist was consulted when available if other pathologists were on the IOF rotation.
Results
There were a total of 1866 thyroid surgeries between January 2008–May 2013 performed at WCMC. A total of 578 thyroid surgical cases had IOF sections performed. Of these cases, 435 met the inclusion criteria of having had an FNA diagnosis of Bethesda II–VI and subsequent IOF section performed. Among the 435 patients, 311 (71%) were female and 124 (29%) were male. The stratification of the FNA diagnosis for these 435 cases was 149 (35%) Bethesda II, 170 (40%) Bethesda III, 91 (21%) Bethesda IV, 19 (4%) Bethesda V, and 6 (100%) Bethesda 6 (Table 2). There were a total of 83 carcinomas identified on FD (Table 3). The final histology results for the malignancies included 69 (83%) papillary thyroid carcinomas (PTCs) (43 follicular variants, 19 classic, 3 oncocytic variants, 1 cribriform morular variant, 2 solid variants, 1 diffuse sclerosing variant), 12 (14%) follicular carcinomas, and 2 (2.4%) poorly differentiated carcinomas (Table 3).
Table 2.
Stratification of FNA biopsies according to Bethesda system.
| Bethesda category | No. of cases |
|---|---|
|
149 |
|
170 |
|
91 |
|
19 |
|
6 |
| Total | 435 |
Table 3.
Types of thyroid carcinomas identified on FD.
| Tumor type | No. of cases |
|---|---|
| Papillary thyroid carcinoma, follicular variant | 43 |
| Papillary thyroid carcinoma, classical type | 19 |
| Follicular carcinoma | 12 |
| Papillary thyroid carcinoma, oncocytic type | 3 |
| Papillary thyroid carcinoma, solid variant | 2 |
| Poorly differentiated thyroid carcinoma | 2 |
| Papillary thyroid carcinoma, cribriform morular variant | 1 |
| Papillary thyroid carcinoma, diffuse sclerosing variant | 1 |
| Total | 83 |
The preoperative FNA diagnosis for the 77 cases identified as carcinomas on FD were as follows: 11 (7.4%) Bethesda II, 24 (14%) Bethesda III, 26 (29%) Bethesda IV, and 16 (84%) Bethesda V (Table 4). Of cases with a diagnosis of Bethesda II by FNA, 7.4% were malignant on FD, yet only 1/149 (0.7%) were positive on IOF sections (Table 4, Fig. 1). For Bethesda III cases, 14% were malignant on FD yet IOF section suggested malignancy in only 5/170 (3%) of these cases (Table 4, Fig. 1). 29% of cases with a Bethesda IV diagnosis were positive on FD and only 2/91 (1.1%) were positive on IOF sections (Table 4, Fig. 1). Among cases with a FNA Bethesda V diagnosis, 84% were positive for malignancy on FD, 8/19 (42%) of which were identified as malignant on IOF sections (Table 4, Fig. 1). IOF section thereby contributed to the diagnosis of malignancy in 16/429 (4%) cases by correctly suggesting malignancy (Table 4). The final histology for these 16 cases included 9 (56%) classic PTCs, 3 (19%) follicular variants of PTC, 1 (6.3%) cribriform morular variant of PTC, 1 (6.3%) oncocytic variant of PTC, 1 (6.3%) poorly differentiated carcinoma, and 1 (6.3%) diffuse sclerosing variant (Table 4). Excluding Bethesda V lesions, IOF contributed to the diagnosis in 8/429 (1.9%) of cases (Fig. 1).
Table 4.
Diagnostic correlation of FNA, IOF section, and FD and types of carcinoma identified by IOF section.
| Bethesda category | No. of cases | No. of cases malignant on FD | No. of cases malignant on IOF section | Diagnosis of malignant cases identified on IOF section |
|---|---|---|---|---|
|
149 | 11 (7.4%) | 1 (0.7%) | 1 Classic PTC |
|
170 | 24 (14%) | 5 (3%) | 4 Classic PTC 1 Follicular variant PTC |
|
91 | 26 (29%) | 2 (1.1%) | 1 Oncocytic PTC 1 Poorly differentiated carcinoma |
|
19 | 16 (84%) | 8 (42%) | 4 Classic PTC 2 Follicular variant PTC 1 Cribriform morular variant PTC 1 Diffuse sclerosing variant PTC |
|
6 | 6 (100%) | 6 (100%) | 6 Classic PTC |
| Total | 435 | 83 (19%) | 22 (5%) |
Fig. 1.
Number of malignant cases identified by IOF section for each Bethesda category. FD = Malignant describes the number of thyroid carcinomas identified upon final diagnosis. IOF section = Malignant describes the number of cases which were identified to be malignant upon examination of IOF sections.
There were 61/77 (79%) false negatives on IOF and there were no false positives on IOF section (Fig. 2). The specificity and sensitivity for malignancy of IOF section was 100% and 21%, respectively. The additional pathology charge alone per positive diagnosis by IOF section for the entire cohort was $6730. The additional pathology charge alone per positive diagnosis was $37,399 for Bethesda II, $8534 for Bethesda III, $11,420 for Bethesda IV and $596 for Bethesda V.
Fig. 2.
Diagnosis correlation of FNA, IOF section and FS.
Discussion
IOF section has traditionally been performed for thyroid nodules for which an intraoperative diagnosis is critical in deciding between a total thyroidectomy and lobectomy with the potential to immediately alter the management plan.12 An intraoperative diagnosis of malignancy may help the surgeon avoid having to perform a second completion procedure while a benign diagnosis may help prevent unnecessary complete removal of the gland.8 However, the frequency with which IOF sections are performed for thyroid nodules has decreased due to the high accuracy and specificity of FNA in the diagnosis of papillary thyroid carcinoma and the inability of neither FNA nor IOF section to reliably recognize follicular and Hürthle cell carcinomas as well as the follicular variant of papillary carcinoma.8, 13, 14 In our cohort, the high false negative IOF rate (79%) is related to those lesions described as follicular lesion with deference to permanent being ascribed as benign; this demonstrates the challenges of IOF for Bethesda II–IV lesions. In addition, IOF sections have also lost favor because they lead to the prolongation of OR time, increased costs, and the possibility of an inaccurate diagnosis that may misguide management.13
Previous studies of IOF section have noted other disadvantages—especially significant for thyroid lesions measuring less than 1 cm in greatest dimension—such as sampling errors, introducing artifacts in the tissue, and wasting specimen that may be necessary to make a final diagnosis.12 Other opinions in the literature have reported the lack of clinical utility of IOF section subsequent to an FNA Bethesda diagnosis of follicular neoplasm, suspicious for follicular neoplasm or suspicious for malignancy.7 Meanwhile, some studies favor the use of IOF section to confirm FNA diagnoses and to identify malignancies in patients with indeterminate or unsatisfactory FNA reports.1, 11 Chang HY et al. noted that when there was a discrepancy between the FNA and IOF section diagnosis for the same case, the FS was more accurate (FS accuracy = 78.9% vs. FNA accuracy = 21.1%).11 Other studies note that IOF section may be particularly useful when it is positive for malignancy because of reports of a false-positive rate as low as 0%.10 FNA has recently been reported to have a sensitivity for the detection of malignant thyroid nodules ranging from 36% to 89% and a specificity ranging from 94% to more than 99% with an overall diagnostic accuracy between 84% and 94%.The same studies reported a sensitivity, specificity and accuracy for the ability of IOF section to detect malignancy to be 56%–67%, 99%–100%, and 89%–90%, respectively.1, 10
Among a total of 1866 thyroid surgeries performed at our institution over a five-year period, IOF section evaluation was performed on 578 (31%) thyroid nodules. The present study sought to evaluate the diagnostic utility of IOF section for cases of nodular thyroid disease with a Bethesda diagnosis of II–VI at our institution. The percentage of malignant cases that had a final histologic result of papillary carcinoma in this series is similar to that previously published (82% vs. 87% in a series of 704 thyroid carcinomas).8 IOF section was found to have a wider disparity between its specificity and sensitivity (100% and 21%, respectively) for identifying malignant thyroid lesions compared to values reported in previous studies.1, 10 Intraoperative evaluation correctly identified malignancy in 16/429 (4%) of cases in this series. Half (8/16) of these cases were classified as Bethesda V lesions prior to IOF sections and thus, IOF contributed to the diagnosis of malignancy in only 8/410 (2.0%) of Bethesda II–IV lesions. Such data suggests that the potential of IOF section to alter the surgical plan is limited outside of Bethesda V nodules. The value of frozen section in benign nodules diagnosed on FNA is also questionable due to a high false negative rate of 79% (61/77). IOF section also appears to lack the ability to reliably identify cases of follicular variant PTC, detecting only 3/43 (7%) of this tumor type. Consequently, the charge per IOF section added diagnosis of malignancy is highest in the Bethesda II cohort ($37,399) and lowest for Bethesda V nodules ($596). However, despite the lack of reliability of diagnosis of Bethesda II–IV lesions, some surgeons may argue that any diagnoses discovered on frozen prove some utility of this assessment. While this may be true, the feasibility of a false positive on frozen section, which was not encountered in our cohort, may limit this argument. Further study, including formal cost effectiveness research is necessary to answer this question.
The current study is not without limitations. Diagnostic modalities such as FNA and IOF section are highly subjective due to factors such as the heterogeneous nature of thyroid pathologies and the inability of such modalities to reliably detect malignancy in cases that are multifocal. Because all FNAs and IOFs were not performed by the same clinician or interpreted by a single pathologist, variables inherent to the operator of the modality and the interpreter of the results could not be controlled for. The pathologists who interpreted the IOF sections were also not necessarily blind to FNA diagnoses.
Conclusion
Our data indicates that IOF sections performed for cases with a Bethesda diagnosis of II–IV do not allow for a significant improvement in diagnosis of malignancy. The role of IOF section appears to be limited outside of Bethesda V nodules and lacks the ability to reliably discern cases of follicular variant PTC. IOF section should be likely be used on a selective basis in the evaluation of thyroid nodules in order to maximize its clinical and cost utility. Improvements in its sensitivity for detecting thyroid malignancies and especially follicular variant PTCs would be needed to justify its widespread use. Further research, including cost effectiveness research is needed to answer this question.
Conflicts of interest/disclosures
None to report.
Funding information
No grant support was received in the preparation of this study.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Prades J.M., Querat C., Dumollard J.M. Thyroid nodule surgery: predictive diagnostic value of fine-needle aspiration cytology and frozen section. Eur Ann Otorhinolaryngol Head Neck Dis. 2013;130:195–199. doi: 10.1016/j.anorl.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 2.Davies L., Welch H.G. Current thyroid cancer trends in the United States. JAMA Otolaryngol Head Neck Surg. 2014;140:317–322. doi: 10.1001/jamaoto.2014.1. [DOI] [PubMed] [Google Scholar]
- 3.McKee G. The role of fine needle aspiration cytology in the diagnosis of thyroid lesions. J R Soc Med. 1998;91(suppl 33):28–32. doi: 10.1177/014107689809133s07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang J., Schnadig V., Logrono R. Fine-needle aspiration of thyroid nodules: a study of 4703 patients with histologic and clinical correlations. Cancer. 2007;111:306–315. doi: 10.1002/cncr.22955. [DOI] [PubMed] [Google Scholar]
- 5.Cibas E.S., Ali S.Z. NCI Thyroid FNA State of the Science Conference. The Bethesda system for reporting thyroid cytopathology. Am J Clin Pathol. 2009;132:658–665. doi: 10.1309/AJCPPHLWMI3JV4LA. [DOI] [PubMed] [Google Scholar]
- 6.Davidov T., Trooskin S.Z., Shanker B.A. Routine second-opinion cytopathology review of thyroid fine needle aspiration biopsies reduces diagnostic thyroidectomy. Surgery. 2010;148:1294–1299. doi: 10.1016/j.surg.2010.09.029. discussion 1299–1301. [DOI] [PubMed] [Google Scholar]
- 7.Kahmke R., Lee W.T., Puscas L. Utility of intraoperative frozen sections during thyroid surgery. Int J Otolaryngol. 2013;2013:496138. doi: 10.1155/2013/496138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Antic T., Taxy J.B. Thyroid frozen section: supplementary or unnecessary? Am J Surg Pathol. 2013;37:282–286. doi: 10.1097/PAS.0b013e318267aee6. [DOI] [PubMed] [Google Scholar]
- 9.Zanocco K., Heller M., Elarai D. Cost effectiveness of intraoperative pathology examination during diagnostic hemithyroidectomy for unilateral follicular thyroid neoplasms. J Am Coll Surg. 2013;217:702–710. doi: 10.1016/j.jamcollsurg.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 10.Mandell D.L., Genden E.M., Mechanick J.I. Diagnostic accuracy of fine-needle aspiration and frozen section in nodular thyroid disease. Otolaryngol Head Neck Surg. 2001;124:531–536. doi: 10.1067/mhn.2001.115372. [DOI] [PubMed] [Google Scholar]
- 11.Chang H.Y., Lin J.D., Chen J.F. Correlation of fine needle aspiration cytology and frozen section biopsies in the diagnosis of thyroid nodules. J Clin Pathol. 1997;50:1005–1009. doi: 10.1136/jcp.50.12.1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tallini G., Gallo C. Fine-needle aspiration and intraoperative consultation in thyroid pathology: when and how? Int J Surg Pathol. 2011;19:141–144. doi: 10.1177/1066896910394842. [DOI] [PubMed] [Google Scholar]
- 13.Chen H., Nicol T.L., Udelsman R. Follicular lesions of the thyroid. Does frozen section evaluation alter operative management? Ann Surg. 1995;222:101–106. doi: 10.1097/00000658-199507000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Udelsman R., Westra W.H., Donovan P.I. Randomized prospective evaluation of frozen-section analysis for follicular neoplasms of the thyroid. Ann Surg. 2001;233:716–722. doi: 10.1097/00000658-200105000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]