Abstract
Since the advent of facelift surgery, there has been a progressive evolution in technique. Methods of dissection trended towards progressively aggressive surgery with deeper dissection for repositioning of ptotic facial tissues. In recent decades, the pendulum has swung towards more minimally invasive options. Likewise, there has been a shift in focus from repositioning alone to the addition of volumization for facial rejuvenation. The techniques in this article are reviewed in a chronologic fashion with a focus on historical development as well as brief discussion on efficacy in relation to the other existing options. There is currently no gold standard technique with a plethora of options with comparable efficacy. There is controversy over which approach is optimal and future research is needed to better delineate optimal treatment options, which may vary based on the patient.
Keywords: Rhytidectomy, Facelift, Facelift techniques, History of the facelift, Facial rejuvenation, Facial fillers, Autologous fat transfer
Introduction
The last several decades have seen significant growth in facial esthetic surgery, not only in quantity, but quality. Consistent improvements in surgical technique as well as treatment strategy have grown naturally out of a greater understanding of facial anatomy and the aging process. Few procedures have seen as much innovation over the years as the facelift procedure. With this in mind, it is hard to believe that the facelift is just over 100 years old.
While esthetic surgery is relatively commonplace and socially acceptable in modern society, its early 20th century beginnings were secretive in nature. There was animosity against esthetic procedures, even by the surgeons who secretly performed the operations. In the 1920s, the American medical community attempted to ban cosmetic surgery.1 This prompted the early pioneers to perform these surgeries in private clinics or purposely mis-label cases on operative logs to avoid discovery. Publication of surgical techniques was avoided for years. For this reason, the true origin of the facelift procedure is unclear.
We do know that surgeons in both Europe and America were employing early facelift techniques by the early 1900s. Eugene von Hollander is often credited with the first facelift, stating in 1932 that his original procedure was performed on a Polish aristocrat in 1901.2 Hollander first mentions the performance of this procedure in a chapter entitled “Cosmetic Surgery” in 1912, though he did not mention the actual date of the procedure until later.3 In his chapter he discussed making elliptical skin excisions in natural skin folds near the hairline and ears. Similarly, in 1931 Lexer finally reported his performance of s-shaped excisions in the temporal region and elliptical incisions along the forehead and hairline for an actress in 1906.4
Charles Miller may have been the first American to perform a facelift, publishing an article discussing his techniques in 1907.5 Still others, including Joseph, Passot, and Bourget described similar techniques involving elliptical excisions to treat the aging face around the same time.6, 7, 8Bourguet, however, was the first to describe subcutaneous dissection with undermining, as well as fat excisions to correct periorbital fat pads.9
It was not until the end of the World War I that innovations in facial rejuvenation really gained traction. The wake of the World War I saw a high demand for reconstructive surgery, which provided a foundation for the facelift. Likewise, an increase in surgeons, the wealth of Americans, and the increasing quality of anesthesia contributed to the evolution of facelift techniques.10 More surgeons began publishing their techniques. Noel contributed to the literature in 1926, publishing a book describing facialplasty, blepharoplasty, forehead and neck lifting.11 In 1920, Bettman described a continuous temporal scalp, preauricular, postauricular, and mastoid incision that is very similar to the cutaneous incisions made in standard facelift procedures today.12
By the 1960s, surgeons began addressing the deeper tissues in order to compensate for the limitations of the subcutaneous facelift. Aufrict first promoted suturing deep to the superficial fat in 1960.13 Skoog is credited with the first description of facelifting that included dissection of the deeper fascial layers. He described dissection of the superficial fascia of the face, which he termed the “buccal fascia”, in continuity with the platysma in the neck. At the completion of the dissection, the flap was repositioned in a superoposterior direction and secured to the parotidomasseteric and mastoid fascia.14 In 1976, Mitz and Peyronie used the knowledge they gained from anatomic cadaver studies to describe the superficial musculoaponeurotic system (SMAS). They noted this layer was continuous with the platysma of the neck, the temporoparietal fascia of the scalp, and enveloped the facial mimetic musculature.15 The discovery of this fascial layer, distinct from the parotidomasseteric fascia, paved the way for modern facelifting techniques.
Further progress was made when Furnas described the ligaments of the midface in 1989. Knowledge of the midfacial ligaments provided an improved understanding of the support system of the facial soft tissues and the role they played in the aging process.16 More modifications of the facelift ensued culminating in a focus on retaining ligament release in a sub SMAS, or deep plane dissection. Still other surgeons developed subperiosteal techniques for facial soft tissue repositioning with the primary goal of resuspending descended malar fat to the malar eminence.17, 18, 19 In recent decades, volumizing procedures such as injectable fillers have enhanced outcomes. Likewise, an emphasis on more minimally invasive techniques has become part of the facial rejuvenation armamentarium. These include limited lifts and other non-surgical lifting procedures.
In the remainder of the article, we review the evolution of common facelifting procedures used today, with brief discussion technique and efficacy. The goal is to provide a basic understanding of both the development and role of each technique in modern facial plastic surgery.
Subcutaneous facelift
As previously described, early techniques focused on small local incisions near the hairline in natural skin creases, with excision of skin strips and closure without undermining. Modern techniques involve combining temporal hairline incisions with a pre or post-tragal incision that curves around the lobule postauricularly and ultimately terminates in the occipital scalp. Bourget and Bettman are credited with combining these incisions with undermining of a large random pattern skin flap.12 Joseph was the first to introduce the concept of the post-tragal incision to the vertical preauricular incision in 1928.13
The main purpose of the subcutaneous lift is to tighten the loose facial skin and remove the excess without addressing the deeper tissues (Fig. 1). It is an easy and safe procedure, resulting in improvement in the lower face and neck. However, this technique fails to address ptosis of the midface and does not address the effects of aging on structures deep to the skin. Without re-suspending the deeper tissues, the skin flap is naturally placed under tension leading to loss of effect secondary to the inherent elasticity of the skin. For this reason, the subcutaneous technique is typically used in selected situations where skin laxity is the main issue.
Fig. 1.

The subcutaneous lift. The flap is raised in a subcutaneous plane leaving the SMAS unaddressed. The lift is in a vertical vector.
SMAS techniques
The concept of deep tissue layer suspension marked a major paradigm shift in facelift technique. Tord Skoog was an early advocate of deeper suspension as opposed to relying on skin tension alone to achieve his facelift.14 However, it was not until 1976 that Mitz and Peyronie described the Superficial Musculoaponeurotic System, or SMAS15. The fibrous adhesions of the SMAS to the overlying subcutaneous fat and skin allowed for surgical manipulation of the SMAS to effect changes in the skin. This anatomic concept rapidly spread through the cosmetic surgery community, and SMAS lifting techniques became the standard for several decades. Management of the SMAS still remains a vital component of successful outcomes today.
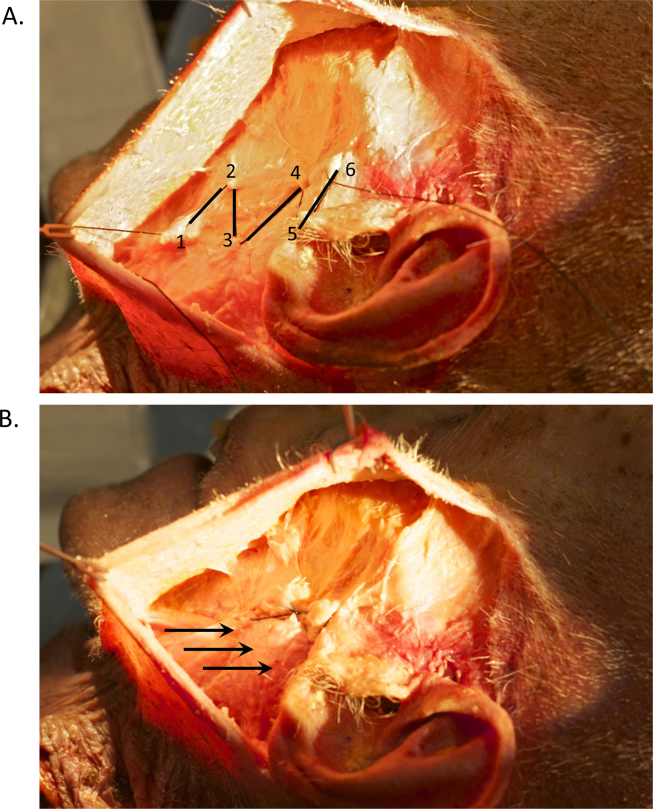
The main methods for addressing the SMAS involve either plication or imbrication. Plication involves suture suspension alone to reverse the vectors of aging. The SMAS of the lower face is drawn vertically in-folding and anchoring it to the more immobile SMAS overlying the parotid. The author uses a variation of this technique, referred to as the “buccal cerclage”, which involves a series of three separate suspension sutures to lift the neck, lower face, and improve the jaw line (Fig. 2, Fig. 3).
Fig. 2.
The buccal cerclage suture. A. The key suture in the buccal cerclage technique. The suture is placed in a stair step pattern with 6 bites along the SMAS of the lower face and affixed to the immobile peri-parotid SMAS. B. The buccal cerclage suture is tightened lifting the SMAS in a vertical vector.
Fig. 3.
Pre- and post-operative facelift using the buccal cerclage. Top: Pre-operative photographs of a patient who underwent facelift using the Buccal cerclage technique. Bottom: 4 year post-operative photographs of the same patient.
Imbrication of the SMAS consists of an incision within the SMAS layer with resection of a portion of the SMAS followed by suture suspension of the incised ends to reverse vectors of aging.20, 21, 22 Imbrication generally involves limited sub SMAS dissection to the anterior edge of the parotid.
These aforementioned techniques are generally regarded as safe and easy to master. SMAS plication and imbrication, when done properly, pose little risk to the facial nerve with good long-term effectiveness. For plication, the main concern regards the ability of the suture to maintain the lift without “cheese wiring” through the lifted tissue. Both SMAS imbrication and plication are less effective in rejuvenation of the midface and melolabial fold as they are the jaw-neck line.23
Historic studies have compared the effectiveness of SMAS techniques to skin only procedures.24 Tipton25 in 1974 and Rees and Aston26 in 1977 performed mixed face-lift procedures using a skin only lift on one side and a SMAS modification on the other. Post-operative photographs were taken for comparative purposes, with no differences noted between the sides. These studies, however, suffered from lack of standardized objective measurements to effectively analyze differences between techniques.
Deep plane techniques
The major weakness of the SMAS techniques is the ability to effectively rejuvenate the midface and malar fat pad. To address this problem, Hamra described the “deep plane rhyitidectomy”, in which he elevated the midfacial soft tissues in a plane between the superficial and deep fascia. This created a thick myocutaneous flap composed of skin and subcutaneous fat to be suspended superiorly.27 The deep plane facelift was a modification of standard face-lift techniques in the 1980s and early 1990s that specifically addressed ptosis of midfacial structures and deep nasolabial folds. Hamra noted improved esthetic results in the midface, which has been supported by other authors as well.28
Though there have been several modifications of the deep plane rhytidectomy, Hamra described an initial subcutaneous dissection in the preauricular area. Once the dissection reaches a point anterior to a line extended from the lateral canthus to the angle of the mandible, dissection transitions to the sub-SMAS plane. Sub-SMAS dissection is carried medially over the zygomaticus major and minor to a point lateral to the melolabial fold (Fig. 4). The SMAS layer is released from the ligamentous attachments in the midface and vertically resuspended to rejuvenate the face.27 This technique presumably improves the nasolabial fold, neck and midface to a greater extent than possible with traditional SMAS techniques. Proponents also claim longer lasting improvement, a natural appearance, and decreased incidence of hematoma and flap compromise. The disadvantages involve greater tissue trauma, longer convalescence period, more technical dissection with increased risk to the facial nerve, and longer surgical time.
Fig. 4.
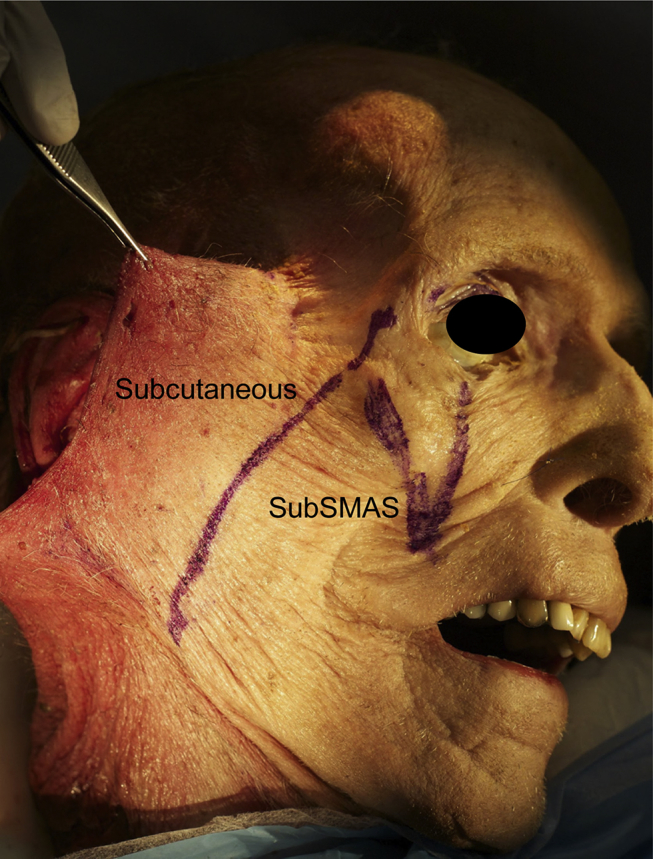
The deep plane technique. Subcutaneous dissection is performed to the point anterior to a line drawn from the lateral canthus to the mandibular angle. The dissection then precedes sub-SMAS over the zygomaticus major and minor.
Several studies have compared the deep plane technique with more traditional SMAS techniques. Adamson et al29 supported Hamra's claim that the deep plane rhytidectomy improves rejuvenation of the midface and neck compared to SMAS plication. Ivy et al,30 however, found no detectable improvements in a side to side comparison in patients with SMAS lifts versus composite rhytidectomies. Though significant reversal of midfacial ptosis was noted intra-operatively using more extensive procedures, the improvements were not noted at later follow up. Similarly, Becker and Bassichis also compared these two groups to identify ideal patients for the deep plane technique. Their results showed that patients aged 50–69 years had a trend toward obtaining better results from the SMAS plication face-lift, whereas patients aged 70–80 years had a trend toward obtaining better results with the deep plane face-lift. They concluded that the deep plane face-lift did not offer superior results over the SMAS plication facelift in patients younger than 70 years.31
Minimally invasive and noninvasive techniques
Shortly after the popularization of deep plane rhytidectomy techniques in the late 80s and early 90s, there was a predictable counter-movement towards more minimally invasive techniques. Whereas more extensive deep plane surgery required more operative time, longer convalescence, and increased risks, the development of minimally invasive surgery offered the complete opposite. These techniques could be performed under local anesthesia in the office.
One such technique that gained popularity was the threadlift. Sulamanidze first introduced the threadlift in the late 90s. This technique involved subcutaneous placement of barbed threads, which were pulled to achieve the lift and trimmed at the entry point.32 The marketed advantage was that it was a “non-surgical” technique with minimal convalescence and instant results. However, several studies have brought into question the peak effect and longevity of the procedure. Lycka et al33 showed only one-third of patients maintaining 70% of their original effect 1–2 years after surgery. A controlled case series by Abraham et al32 showed minimal improvement on blinded assessment when compared to a control group who had undergone other rejuvenation procedures.
In 1999, Saylan described a short-scar technique he termed the “S-Lift” which involved an S-shaped skin incision crossing the non-hair-bearing skin at the helical root, pre-excision of skin, and vertical purse-string sutures in the SMAS. The sutures were secured to the periosteum of the zygomatic arch to achieve the lift.34 Tonnard and Verpaele later modified this approach by altering the incision to follow the border of the sideburn, perform the skin excision after the lift, and most notably to affix the purse-string plication sutures to the temporal fascia instead of the zygomatic arch. They termed this lift the Minimal Access Cranial Suspension Lift (MACS lift). The effect of the purse-string was thought to create “microimbrications” within the SMAS35 (Fig. 5). In short term follow up, the MACS lift was noted to have comparable results to traditional SMAS techniques. Nonetheless, all minimally invasive techniques are subject to criticism regarding durable results.
Fig. 5.

The MACS lift. A posterior narrow purse-string suture is followed anteriorly by a 30° oblique wider purse-string suture on through the SMAS and both sutures are anchored to the deep temporal fascia.
In recent years, even less invasive, non-surgical techniques have been developed which offer skin-tightening effects. These include the use of radiofrequency, laser, and ultrasound energy. All of these non-invasive techniques target collagenous tissue such as the papillary and reticular dermis to exert their effects. Though the impact of these options may not be as dramatic as that of surgical lifting, they offer a viable alternative to those unwilling or unable to undergo surgery.
Addition of volumetric techniques
Facial aging is a dynamic and fluid process that not only involves soft tissue descent, but deflation and loss of facial volume as well. Over time the face loses both fat and volume and the skin loses collagen and elasticity.36 The once full cheeks and heart-shaped facial appearance of youth give way to an aged hollowed face with bony contours and thin skin. The previously described facelift procedures focus on reversing facial descent and do not address facial deflation. In recent years, through contributions such as those by Lambros, a better understanding of facial aging has developed resulting in the incorporation of volumization into the treatment algorithm of modern facelift surgeons.37
Interestingly, the idea of fillers for soft tissue augmentation has been around since the late 1800s. In 1893, Neuber described filling a depressed facial scar with fat transfer.38 Paraffin, a purified mixture of solid hydrocarbons from petroleum, was also used as a tissue filler. Prominent historical surgeons, such as Billroth, Gersuny, and Delangre were noted to use paraffin injections to treat various ailment. Kolle published a paper in 1911 depicting the correction of a saddle nose by paraffin injection. He also noted the myriad of complications, including severe granulomas, emboli, blindness, and even death.39 For this reason, paraffin as a filler fell out of favor by the 1920s. Silicone is yet another filler that has been used in the past, though has largely fallen out of favor due to its side effect profile and technique sensitive application.
Though several filler materials have fallen by the wayside, there are many options available for facial rejuvenation. These include collagen, calcium hydroxyapatite, poly-l-lactic acid, and hyaluronic acid products. Of these, hyaluronic acid fillers are among the most widely used secondary to their longevity, efficacy, safety, and most importantly, reversibility. Injection of hyaluronidase can be employed if needed to breakdown the injected hyaluronic acid.40 This is particularly important in the rare case of intra-arterial infiltration as the consequences can be devastating.
All of the FDA approved, commercially available fillers are temporary in nature. These products ultimately resorb, requiring repeated injections for maintenance of the effects. For this reason, autologous fat transfer is a popular alternative. This “permanent” option is safe and easily performed with facelift surgery as an adjunct for volumization of the midface. One must keep in mind that fat injection can suffer from the same potential issues as the temporary fillers.
Yet another option for midface volumizations the malar implant. Malar implants fill the infraorbital rim and buccal hollows. However, they do not offer the plasticity and natural appearance of soft-tissue fillers.40
The combination of facelift surgery with volumization, particularly in the midface, comprehensively addresses the effects of aging (Fig. 6). Not only is suspension of soft-tissue vital to facial rejuvenation, but replacement of atrophy as well. When used in conjunction with facelifting, volumization can result in dramatic improvements in appearance.
Fig. 6.

Pre and post-op lower blepharoplasty and fat transfer. Top: Pre-operative photograph of a patient who underwent lower lid blepharoplasty and fat transfer. Bottom: 3-year post-operative photograph of the same patient.
Conclusion
The practice of facelifting has seen a dramatic transformation in the century since its inception. The knowledge gained from preceding surgeons has led to the development of many safe, reproducible, and effective techniques. Currently, there is no consensus in the literature regarding the best approach. This indicates that multiple available surgical options are equivalent in the hands of an experienced surgeon. Many advocates for the various modern techniques have made convincing arguments in support of their preference.
The fact no consensus exists underscores the importance of continued innovation to perfect surgical outcomes, improve longevity, and keep pace with patient expectations. Likewise, further scrutiny of existing techniques through well-designed studies is necessary for the eventual development of a “gold standard”. The next 100 years in the development of facelifting will likely see a similar degree of advancement with a focus on application of new technologies and a trend toward less invasive procedures.
Edited by Jing Li
Footnotes
Peer review under responsibility of Chinese Medical Association.
Contributor Information
Dane M. Barrett, Email: Barredan@ohsu.edu.
Fernando J. Casanueva, Email: fjcasanueva@gmail.com.
Tom D. Wang, Email: Wangt@ohsu.edu.
References
- 1.Ryan R.F. A 1927 view of cosmetic surgery. Plast Reconstr Surg. 2000;106:1211. doi: 10.1097/00006534-200010000-00042. [DOI] [PubMed] [Google Scholar]
- 2.Hollander E. Plastische(Kosmetische) Operation: KritischeDarstellungihresgegenwartigen, Stands. Urban and Schwarzenberg; Berlin: 1932. pp. 1–17. [Google Scholar]
- 3.Hollander E. diekosmetischechirurgie. In: Joseph M., editor. Handbuch der kosmetik. Verlag von Viet; Leipzig: 1912. p. 668. [Google Scholar]
- 4.Lexer E. Leipzig: JA Barth; 1931.
- 5.Miller C. Oak Printing; Chicago: 1907. The Correction of Featural Imperfections. [Google Scholar]
- 6.Joseph J. Hangewangenplastik (melomioplastik) Dtsch Med Wochenschr. 1921;47:287. [Google Scholar]
- 7.Passot R. La chirurgieesthetique des rides du visages. Presse Med. 1919;27:258. [Google Scholar]
- 8.Bourguet J. Les herniesgraisseuses de l'orbite. notretraitement chirurgical. Bull Acad Med. 1919;27:258. [Google Scholar]
- 9.Bourget J. La disparitionchiurgicale des rides etplis du visage. Bull Acad Med Paris. 1919;82:183. [Google Scholar]
- 10.Haiken E. The making of the modern face: cosmetic surgery. Soc Res (New York) 2000;67:81–97. [PubMed] [Google Scholar]
- 11.Noel A. Masson et Cite; Paris: 1926. La Chirurgieesthetique: Son Role Social. [Google Scholar]
- 12.Bettman A. Plastic and cosmetic surgery of the face. Northwest Med. 1920:205. [Google Scholar]
- 13.Adamson P.A., Moran M.L. Historical trends in surgery for the aging face. Facial Plast Surg. 1993;9:133–142. doi: 10.1055/s-2008-1064604. [DOI] [PubMed] [Google Scholar]
- 14.Skoog T. W.B. Saunders; Philadelphia: 1974. Plastic Surgery: New Methods and Refinements. [Google Scholar]
- 15.Mitz V., Peyronie M. The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plast Reconstr Surg. 1976;58:80–88. doi: 10.1097/00006534-197607000-00013. [DOI] [PubMed] [Google Scholar]
- 16.Furnas D.W. The retaining ligaments of the cheek. Plast Reconstr Surg. 1989;83:11–16. doi: 10.1097/00006534-198901000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Tessier P. Transactions of the Seventh International Congress of Plastic and Reconstructive Surgery. Ely Jf; Rio de Janiero: 1980. Facelifting and frontal rhytidectomy; p. 39. [Google Scholar]
- 18.Psillakis J.M., Rumley T.O., Camargos A. Subperiosteal approach as an improved concept for correction of the aging face. Plast Reconstr Surg. 1988;82:383–394. doi: 10.1097/00006534-198809000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Ramirez O.M., Maillard G.F., Musolas A. The extended subperiosteal face lift: a definitive soft-tissue remodeling for facial rejuvenation. Plast Reconstr Surg. 1991;88:227–236. discussion 237–238. [PubMed] [Google Scholar]
- 20.Baker D.C. Lateral SMA sectomy. Plast Reconstr Surg. 1997;100:509–513. doi: 10.1097/00006534-199708000-00039. [DOI] [PubMed] [Google Scholar]
- 21.Berry M.G., Davies D. Platysma-SMAS plication facelift. J Plast Reconstr Aesthet Surg. 2010;63:793–800. doi: 10.1016/j.bjps.2009.02.067. [DOI] [PubMed] [Google Scholar]
- 22.Mendelson B.C. Surgery of the superficial musculoaponeurotic system: principles of release, vectors, and fixation. Plast Reconstr Surg. 2001;107:1545–1552. discussion 1553–1555, 1556–1557, 1558–1561. [PubMed] [Google Scholar]
- 23.Warren R. Plastic Surgery. 3rd ed. Elsevier; New York: 2012. Facelift. [Google Scholar]
- 24.Chang S., Pusic A., Rohrich R.J. A systematic review of comparison of efficacy and complication rates among face-lift techniques. Plast Reconstr Surg. 2011;127:423–433. doi: 10.1097/PRS.0b013e3181f95c08. [DOI] [PubMed] [Google Scholar]
- 25.Tipton J.B. Should the subcutaneous tissue be plicated in a face lift? Plast Reconstr Surg. 1974;54:1–5. doi: 10.1097/00006534-197407000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Rees T.D., Aston S.J. A clinical evaluation of the results of submusculo-aponeurotic dissection and fixation in face lifts. Plast Reconstr Surg. 1977;60:851–859. doi: 10.1097/00006534-197712000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Hamra S.T. The deep-plane rhytidectomy. Plast Reconstr Surg. 1990;86:53–61. discussion 62–63. [PubMed] [Google Scholar]
- 28.Kamer F.M. One hundred consecutive deep plane face-lifts. Arch Otolaryngol Head Neck Surg. 1996;122:17–22. doi: 10.1001/archotol.1996.01890130013002. [DOI] [PubMed] [Google Scholar]
- 29.Adamson P.A., Dahiya R., Litner J. Midface effects of the deep-plane vs the superficial musculoaponeurotic system plication face-lift. Arch Facial Plast Surg. 2007;9:9–11. doi: 10.1001/archfaci.9.1.9. doi: 9/1/9 [pii] [DOI] [PubMed] [Google Scholar]
- 30.Ivy E.J., Lorenc Z.P., Aston S.J. Is there a difference? A prospective study comparing lateral and standard SMAS face lifts with extended SMAS and composite rhytidectomies. Plast Reconstr Surg. 1996;98:1135–1143. doi: 10.1097/00006534-199612000-00001. discussion 1144–1147. [DOI] [PubMed] [Google Scholar]
- 31.Becker F.F., Bassichis B.A. Deep-plane face-lift vs superficial musculoaponeurotic system plication face-lift: a comparative study. Arch Facial Plast Surg. 2004;6:8–13. doi: 10.1001/archfaci.6.1.8. [DOI] [PubMed] [Google Scholar]
- 32.Abraham R.F., DeFatta R.J., Williams E.F., 3rd Thread-lift for facial rejuvenation: assessment of long-term results. Arch Facial Plast Surg. 2009;11:178–183. doi: 10.1001/archfacial.2009.10. [DOI] [PubMed] [Google Scholar]
- 33.Lycka B., Bazan C., Poletti E., Treen B. The emerging technique of the antiptosissubdermal suspension thread. Dermatol Surg. 2004;30:41–44. doi: 10.1111/j.1524-4725.2004.30000.x. discussion 44. doi: 30000 [pii] [DOI] [PubMed] [Google Scholar]
- 34.Saylan Z. The S-lift: less is more. Aesthet Surg J. 1999;19:406. [Google Scholar]
- 35.Tonnard P., Verpaele A., Monstrey S. Minimal access cranial suspension lift: a modified S-lift. Plast Reconstr Surg. 2002;109:2074–2086. doi: 10.1097/00006534-200205000-00046. [DOI] [PubMed] [Google Scholar]
- 36.Gilchrest B. Cellular and molecular changes in aging skin. J Geriatr Dermatol. 1994:3–6. [Google Scholar]
- 37.Lambros V.S. What age(s) for face lifts? Plast Reconstr Surg. 1999;103:1076. [PubMed] [Google Scholar]
- 38.Neuber F. Fat transplantation. ChirKongrVerhandlDtschGesellechChir. 1893;22:66. [Google Scholar]
- 39.Goldwyn R.M. The paraffin story. Plast Reconstr Surg. 1980;65:517–524. doi: 10.1097/00006534-198004000-00024. [DOI] [PubMed] [Google Scholar]
- 40.Bassichis B.A. Volumetric facelift with intra- and post-operative midface volume replacement “the four-dimensional facelift”. Facial Plast Surgclin North Am. 2009;17:539–547. doi: 10.1016/j.fsc.2009.06.004. v–vi. [DOI] [PubMed] [Google Scholar]