Abstract
Objective
To assess the characteristics and quality of cost utility analyses (CUA) related to otolaryngology within the CEA registry and to summarize their collective results.
Methods
All cost-utility analyses published between 1976 and 2011 contained in the Cost-Effectiveness Analysis Registry (CEA Registry) were evaluated. Topics that fall within the care of an otolaryngologist were included in the review regardless of the presence of an otolaryngologist author. Potential associations between various study characteristics and CEA registry quality scores were evaluated using the Pearson product moment correlation coefficient.
Results
Sixty-one of 2913 (2.1%) total CUA publications screened were related to otolaryngology. Eighteen of 61 (29.5%) publications included an otolaryngologist as an author. Fourteen studies agreed on the cost effectiveness of at least unilateral cochlear implantation and six of seven (85.7%) studies demonstrated the cost effectiveness of continuous positive airway pressure (CPAP) for obstructive sleep apnea (OSA). Forty-six percent (28 of 61) of all manuscripts were published between 2008 and 2011. A more recent publication year was associated with a higher CEA registry quality score while the presence of an otolaryngologist author and journal impact factor had no significant correlation with the quality of the CUA.
Conclusion
Based on current evidence in the CEA registry, unilateral cochlear implantation for hearing loss and CPAP for OSA are both cost-effective therapeutic interventions. Although CUAs in otolaryngology have increased in quantity and improved in quality in more recent years, there is a relative lack of CUAs in otolaryngology in comparison to other subspecialties.
Keyword: Cost-utility analysis
Introduction
The cost of medicine in the United States and abroad is increasing at an exponential and economically unsustainable rate. Technological advances leading to more expensive diagnostic and therapeutic tools have contributed to this increase, which in turn has led to rising pressure to demonstrate the value of such interventions. This has ultimately led to growing governmental, professional, organizational, and academic interests in the value propositions in the healthcare system. Cost-effectiveness analysis (CEA) is the primary modality by which investigators assess the value of an intervention. CEA evaluates the price of an intervention, either to the payer or to society, for an individual measure of effectiveness of that intervention.1 This can include the years of life added and quality of life added, among others.
A subset of cost-effectiveness analysis is cost-utility analysis (CUAs), which expresses the effectiveness of an intervention using a uniform unit of cost per quality adjusted life year (QALY). The QALY describes the time spent in a certain health state, multiplied by the quality of each state (with 1 QALY being perfectly healthy for one year).2 In this way, both a treatment that improves health related quality of life from 0.5 to 1.0 for 5 years and a treatment that leads to 5 additional years of life with a health condition of 0.5 both yield 2.5 QALYs. One general way to look at value is to assess the cost of an intervention and to correlate this with the benefits rendered, either in life gained or in quality of life improved. In cost-utility analysis, interventions are considered of favorable value if their cost is less than $50,000 (USD) per QALY gained. As the cost per QALY decreases, the intervention becomes more cost effective. When comparing two interventions with the same intended goal, the intervention with the lower cost per QALY is the more economic choice.
Within all aspects of medical literature, there are an increasing number of studies evaluating cost utility. However, this is challenging within subspecialties such as otolaryngology due to a limited number of investigators and conditions compared to other specialties. Nevertheless, because otolaryngology utilizes costly diagnostic and therapeutic strategies for managing conditions such as head and neck cancer, hearing loss, and chronic sinusitis, it provides a fertile landscape for the assessment of cost effectiveness. The objectives of this study are to detail specific characteristics of CUAs within otolaryngology, to evaluate the quality of these studies and to summarize the collective results of the most common topics of economic evaluations in otolaryngology.
Methods
We performed a quantitative and qualitative assessment of studies within the spectrum of otolaryngology between 1976 and 2011 using the CEA registry.3 The CEA registry is a database updated three times per year with publically available data on all publications that are published in English, are original cost-effectiveness analyses, and measure health benefits of QALYs. The CEA registry is supported by the Center for the Evaluation of Value and Risk in Health (CEVR) and is part of the Institute for Clinical Research and Health Policy Studies at Tufts Medical Center. The total number of studies available in the registry at the time of analysis was 2913. The registry's rigorous methodology for screening cost utility analysis manuscripts is described on the website. In short, a MEDLINE search is performed with the keywords, “QALYs” “quality,” and “cost-utility analysis.” The CEA registry team screens abstracts to assess if there is an original cost-utility estimate. Each article is then abstracted for methodology, cost-effectiveness ratios, and utility weights. Two trained readers audit each article independently and a consensus audit resolves discrepancies.
Author MAC systematically reviewed all of the articles within the CEA registry and screened for publications that fall within the field of otolaryngology, which includes head and neck surgery, endocrine surgery, otology, pediatric otolaryngology, rhinology, allergy and sleep medicine. The presence of an otolaryngologist author, as determined per affiliations listed on the manuscript, was not a factor in inclusion. In the unique case that affiliations were not named, an Internet search was conducted. Study characteristics, including year of publication, journal of publication, author affiliation, country of research, type of funding, analysis perspective, intervention type, and CEA registry quality score (numbered from 1 (low) to 7 (high) by expert readers). The criteria used to determine the CEA registry quality score of each study includes: 1. accurate computation of incremental cost-effectiveness ratios, 2. comprehensive characterization of the uncertainty of results, 3. explicit specification of health economic assumptions used in the study, and 4. appropriate and explicit estimation of utility weights (Table 1). The strength and direction of association between characteristics of each study and CEA registry quality scores were measured using the Pearson product moment correlation coefficient using the Statistical Package for Social Sciences (SPSS Version 22.0, Chicago, IL). The collective results of CUAs of the most commonly evaluated interventions were also assessed in order to identify economically attractive management options within otolaryngology.
Table 1.
CEA registry quality score criteria, adapted from the Tufts CEA Registry.3
| CEA registry quality score criteria (in order of importance) |
|---|
|
Results
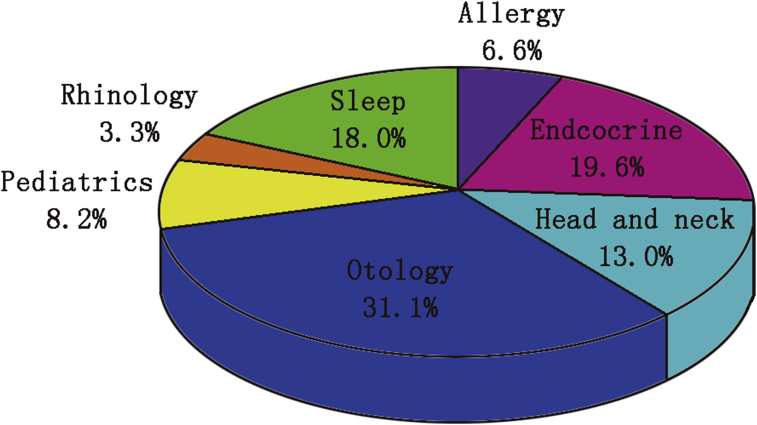
Assessment of 2913 studies revealed 61CUAs that evaluated interventions related to otolaryngology. The earliest study was published in 1991 and assessed the cost-effectiveness of tympanostomy tubes versus antibiotic prophylaxis for acute otitis media (AOM). Eighty-five percent (52 of 61) of studies were published later than 2000, with 28 (45.9%) published between 2008 and 2011 (Fig. 1). The 61 publications addressed topics within the subspecialties of otology (31.1%), endocrine surgery (19.6%), sleep medicine/surgery (18.0%), head and neck surgery (13.0%), pediatric otolaryngology (8.2%), allergy (6.6%), and rhinology (3.3%) (Fig. 2). Of the 61 manuscripts related to otolaryngology, 18 (29.5%) studies had at least one author who was an otolaryngologist. Eight (13.0%) manuscripts had a first author and seven (11.4%) had a final author primarily affiliated with a department of otolaryngology. Seventy-two percent of publications with an otolaryngologist as a first author were related to otology.
Fig. 1.
CUA publications per time period.
Fig. 2.
Publication subspecialties.
The otolaryngology CUAs were published in 41 journals, with only five journals having three or more manuscripts (Table 2). Thirty-two (52.4%) economic analyses had the United States as the country of interest. Eight studies focused on the United Kingdom and five on Canada. Ninety-eight percent of manuscripts had at least one author with an academic affiliation. Seventy-one percent of analyses had the perspective of healthcare payer. The funding sources of the manuscripts were stated as none or could not be determined in 29 (47.5%), government funding in 17 (27.9%), pharmaceutical or device in 14 (22.9%), foundation in 6 (9.8%) and healthcare organization in 3 (4.9%) (Table 2). Two studies (3.3%) evaluated primary prevention strategies, which are defined as efforts to prevent disease prior to its occurrence. One of these primary prevention strategies analyzed oral cancer screening programs for high-risk males4 and the second evaluated candidate vaccines for prevention of pediatric acute otitis media.5 Thirteen studies assessed secondary prevention interventions (methods that identify and treat asymptomatic individuals with risk factors or preclinical disease) and 46 (75.4%) evaluated tertiary prevention interventions (methods that limit disability after harm has occurred). A majority of the studies evaluated the cost utility of devices (47.5%) or pharmaceuticals (29.5%) (Table 2).
Table 2.
Demographic characteristics of CUAs.
| Study characteristic | No. Studies (%) | Mean CEA registry quality score (range) |
|---|---|---|
| Subspecialty | ||
| Otology | 19 (31.1) | 3.8 (1.5–6.0) |
| Endocrine surgery | 12 (19.7) | 4.2 (3.5–5.5) |
| Sleep medicine/surgery | 11 (18.0) | 4.2 (2.5–6.0) |
| Head and neck surgery | 8 (13.0) | 3.4 (2.5–5.0) |
| Pediatric otolaryngology | 5 (8.2) | 4.3 (3.0–5.5) |
| Allergy | 4 (6.6) | 4.5 (3.5–6.0) |
| Rhinology | 2 (3.3) | 4.5 (4.0–5.0) |
| Journal (2011 impact factor) | ||
| Laryngoscope (1.752) | 6 (9.8) | 3.3 (1.5–4.5) |
| Arch of Otolaryngology Head Neck Surg (1.63) | 4 (6.6) | 4.1 (1.5–5.0) |
| Ear Hearing (2.578) | 3 (4.9) | 4.5 (3.0–6.0) |
| Sleep (5.051) | 3 (4.9) | 4.2 (2.5–5.0) |
| Value Health (2.191) | 3 (4.9) | 5.0 (4.0–6.0) |
| Others | 36 (59) | 4.1 (1.5–6.0) |
| Total No. of Journals | 41 | 4.0 (1.5–6.0) |
| Year of publication | ||
| 1976–1991 | 1 (1.6) | 3.0 |
| 1992–1995 | 4 (6.6) | 2.1 (1.5–3.0) |
| 1996–1999 | 4 (6.6) | 3.9 (2–5.5) |
| 2000–2003 | 10 (16.4) | 3.9 (1.5–5.5) |
| 2004–2007 | 14 (22.9) | 4.0 (3.0–6.0) |
| 2008–2011 | 28 (45.9) | 4.4 (2.5–6.0) |
| Country of analysis | ||
| United States | 32 (52.4) | 3.9 (1.5–6.0) |
| United Kingdom | 8 (13.1) | 4.7 (1.5–6.0) |
| Canada | 5 (8.2) | 4.1 (2.5–5.5) |
| Australia | 3 (4.9) | 3.3 (3.0–4.0) |
| Germany | 3 (4.9) | 4.2 (4.0–4.5) |
| France | 2 (3.3) | 4.5 (3.5–5.5) |
| Netherlands | 2 (3.3) | 3.5 (2.0–5.0) |
| New Zealand | 1 (1.6) | 4.0 |
| Austria | 1 (1.6) | 3.5 |
| China | 1 (1.6) | 3.0 |
| Finland | 1 (1.6) | 3.0 |
| Belgium | 1 (1.6) | 5.0 |
| Taiwan | 1 (1.6) | 5.0 |
| Funding source | ||
| Government | 17 (27.9) | 4.1 (1.5–6.0) |
| Pharmaceutical or device | 14 (22.9) | 3.8 (1.5–5.5) |
| Could not be determined | 29 (47.5) | 3.9 (1.5–6.0) |
| Foundation | 6 (9.8) | 4.3 (3.0–5.5) |
| Healthcare organization | 3 (4.9) | 3.5 (1.5–4.5) |
| Perspective of study | ||
| Healthcare payer | 43 (70.5) | 3.9 (1.5–6.0) |
| Societal | 17 (27.9) | 4.4 (3.0–5.5) |
| Could not be determined | 1 (1.6) | 1.5 |
| Intervention type | ||
| Primary | 2 (3.3) | 4.8 (4.0–5.5) |
| Secondary | 13 (21.3) | 3.8 (2.0–6.0) |
| Tertiary | 46 (75.4) | 4.0 (1.5–6.0) |
| Authors affiliation | ||
| Academic | 60 (98.4) | 4.0 (1.5–6.0) |
| Consultant | 7 (11.5) | 4.4 (3.5–5.0) |
| Government | 1 (1.6) | 3.0 |
| Intervention assessed | ||
| Device | 29 (47.5) | 3.8 (1.5–6.0) |
| Diagnostic | 6 (9.8) | 4.0 (3.0–5.0) |
| Screening | 6 (9.8) | 3.4 (2.0–5.0) |
| Health education | 1 (1.6) | 4.0 |
| Medical procedure | 9 (14.7) | 4.1 (3.0–5.0) |
| Pharmaceutical | 18 (29.5) | 4.6 (3.5–6.0) |
| Surgical | 12 (19.7) | 3.9 (2.5–5.5) |
| Immunization | 2 (3.3) | 5.0 (4.5–5.5) |
| Care delivery | 2 (3.3) | 3.3 (3.0–3.5) |
The mean CEA registry quality score (on a scale of 1–7) for all 61 studies was 4.00. A more recent publication year was associated with a higher CEA registry quality score (r = 0.412, P < 0.01) (Table 3). The mean quality score for studies with at least one otolaryngology author was 3.77 and 4.09 for those without an otolaryngology author. There was no significant correlation between the number of otolaryngologist authors and the CEA quality score. The impact factor of the journal in which each study was published also had no significant association with the quality of the CUA. The references and topics for all 61 studies that relate to otolaryngology in the CEA database are listed in Table 4. Fourteen studies agreed on the cost-effectiveness of at least unilateral cochlear implantation and 6 of 7 studies demonstrated CPAP to be a cost-effective strategy for treating patients with OSA.
Table 3.
Correlations between CUA characteristics and CEA registry quality score.
| Variable | Correlation coefficient, r | P value |
|---|---|---|
| # of Otolaryngology authors | −0.043 | 0.749 |
| Publication year | 0.412 | 0.001a |
| Journal impact factor | 0.184 | 0.160 |
Statistically significant.
Table 4.
Summary of evaluated CUAs.
| Year | Specialty | Journal | Reference | Topic of CUA publication |
|---|---|---|---|---|
| 1991 | General | Fam Pract Res J | Bisonni et al9 | Tympanostomy tubes vs antibiotic prophylaxis for AOM |
| 1994 | Sleep | Sleep | Tousignant et al10 | Impact of nasal CPAP on quality of life for OSA |
| 1995 | Otology | Ann Otol Rhinol Laryngol Suppl | Evans et al11 | Adult unilateral cochlear implant |
| 1995 | Otology | Med Prog Technol | Lea et al12 | Cochlear implantation vs vibrotactile devices |
| 1995 | Otology | Arch Otolaryngol Head Neck Surg | Harris et al13 | Cochlear implantation for profound deafness |
| 1996 | Otology | Laryngoscope | Wyatt et al14 | Multichannel cochlear implants |
| 1996 | Pediatrics | Clin Ther | Oh et al15 | Second-line antibiotics for pediatric AOM |
| 1999 | Otology | Int J Technol Assess Health Care | Carter et al16 | Pediatric and adult cochlear implantation |
| 1999 | Otology | Arch Otolaryngol Head Neck Surg | Palmer et al17 | Adult cochlear implantation |
| 2000 | Otology | Laryngoscope | O'Neill et al18 | Pediatric cochlear implantation |
| 2000 | Otology | JAMA | Cheng et al19 | Pediatric cochlear implantation |
| 2001 | Head and neck | Cancer | Hollenbeak et al20 | FDG-PET for N0 HNSCC |
| 2002 | Endocrine | Eur J Endocrinol | Vidal-Trecan et al21 | Management of toxic thyroid adenomas |
| 2002 | Otology | Otol Neurotol | Bichey et al22 | Cochlear implantation for large vestibular aqueduct syndrome |
| 2002 | Otology | Laryngoscope | Francis et al23 | Cochlear implantation in older adults |
| 2002 | Head and neck | Community Dent Oral Epidemiol | Van der Meij et al24 | Cancer screening of patients with oral lichen planus |
| 2002 | Otology | Arch Otolaryngol Head Neck Surg | Summerfield et al25 | Unilateral vs bilateral cochlear implantation |
| 2003 | Otology | Arch Otolaryngol Head Neck Surg | Joore et al26 | Fitting of hearing aids |
| 2003 | Otology | Laryngoscope | Wilson et al27 | Intraoperative facial nerve monitoring for otologic surgery |
| 2004 | Otology | Ear Hear | Group, UKCIS et al28 | Unilateral cochlear implantation in postlingually deafened adults |
| 2004 | Endocrine | Thyroid | Vidal-Trecan et al29 | Radioiodine vs surgery for toxic thyroid adenoma |
| 2005 | Endocrine | Eur J Endocrinol | Sejean et al30 | Surgery vs medical follow-up for primary hyperparathyroidism |
| 2005 | Endocrine | ANZ J Surg | Blamey et al31 | Recombinant human TSH for diagnosis of recurrent thyroid cancer |
| 2005 | Sleep | Stroke | Brown et al32 | Sleep study screening of stroke victims for OSA |
| 2006 | Pediatrics | Pediatrics | Van Howe et al33 | Observation without testing for pediatric pharyngitis |
| 2006 | Sleep | Arch Int Med | Ayas et al34 | CPAP for moderate to severe OSA |
| 2006 | Otology | Ear Hear | Barton et al35 | Pediatric cochlear implantation |
| 2006 | Endocrine | Surgery | Zanocco et al36 | Management of asymptomatic primary hyperparathyroidism |
| 2007 | Pediatrics | Ann Fam Med | Coco et al37 | Management of pediatric acute otitis media |
| 2007 | Endocrine | Am J Kidney Dis | Narayan et al38 | Parathyroidectomy vs cinacalcet for hyperparathyroidism in ESRD |
| 2007 | Allergy | Curr Med Res Opin | Keiding et al39 | Immunotherapy for seasonal allergic rhinoconjunctivitis |
| 2007 | Rhinology | Am J Rhinol | Anzai et al40 | Management of acute sinusitis |
| 2007 | Otology | Genet Med | Veenstra et al41 | Testing for mitochondrial mutation (A155G) in cystic fibrosis |
| 2008 | Sleep | J Int Med Res | Lojander et al42 | Nasal CPAP for OSA |
| 2008 | Otology | Otol Neurotol | Chang et al43 | Hearing aid outcome in the elderly |
| 2008 | Allergy | Ann Allergy Asthma Immunol | Bruggenjurgen et al44 | Subcutaneous immunotherapy for allergic rhinitis and allergic asthma |
| 2008 | Head and neck | Value Health | Brown et al45 | Cetuximab plus radiotherapy for head and neck cancer |
| 2008 | Sleep | Thorax | Guest et al46 | CPAP for OSA |
| 2008 | Sleep | Can Respir J | Tan et al47 | CPAP for OSA |
| 2008 | Endocrine | Surgery | Zanocco et al48 | Parathyroidectomy vs observation for primary hyperparathyroidism |
| 2009 | Endocrine | Value Health | Mernagh et al49 | Recombinant human TSH before RAI ablation for thyroid cancer |
| 2009 | Head and neck | Ann Oncol | Sher et al50 | CT and PET-CT for determining need for neck dissection in HNSCC |
| 2009 | Head and neck | Dermatol Surg | Seidler et al51 | Mohs vs traditional surgery for nonmelanoma skin cancer |
| 2009 | Rhinology | Appl Health Encon Health Policy | Kneis et al52 | Sinfrontal, homeopathic medication, for acute maxillary sinusitis |
| 2009 | Head and neck | Acad Radiol | Yen et al53 | MRI vs PET vs MRI-PET for diagnosis of recurrent NPC |
| 2009 | Sleep | Int J Technol Assess Health Care | Weatherly et al54 | CPAP vs dental devices and lifestyle advice for OSA |
| 2009 | Allergy | Am J Epidemiol | Witt et al55 | Acupuncture for allergic rhinitis |
| 2009 | Sleep | Sleep Breath | Sadatsafavi et al56 | CPAP vs oral appliances for OSAH |
| 2009 | Otology | Fam Pract | Hernandez et al57 | Management of Bell's palsy |
| 2009 | Pediatrics | Pediatrics | O'Brien et al5 | Candidate vaccines for prevention of pediatric AOM |
| 2009 | Sleep | Sleep | Snedecor et al58 | Eszopiclone for primary chronic insomnia |
| 2009 | Endocrine | J Am Coll Surg | In et al59 | Treatment options for Graves disease |
| 2010 | Endocrine | Ann Surg Oncol | Wang et al60 | Oral calcium and calcitriol following total thyroidectomy |
| 2010 | Otology | Ear Hear | Summerfield et al61 | Bilateral pediatric cochlear implantation |
| 2010 | Endocrine | JCEM | Wang et al60 | Recombinant TSH prior to RAI for thyroid cancer |
| 2010 | Allergy | Value Health | Petrou et al62 | Topical intranasal steroids for pediatric OME |
| 2011 | Sleep | Sleep | Pietzsch et al63 | Diagnostic and therapeutic strategies for OSA |
| 2011 | Sleep | Cost Eff Resour Alloc | Scott et al64 | Treatment of insomnia |
| 2011 | Endocrine | JCEM | Li et al65 | Novel molecular test for indeterminate thyroid nodules |
| 2011 | Head and neck | Laryngoscope | Higgins et al66 | Radiation vs transoral laser surgery for early-stage glottic carcinoma |
| 2011 | Head and neck | Laryngoscope | Dedhia et al4 | Oral cancer screening programs for high-risk males |
Abbreviations: AOM, acute otitis media; PAP, continuous positive airway pressure; T, computed tomography; CUA, cost-utility analysis; ESRD, end stage renal disease; FDG-PET, 18-F fluoro-2-deoxyglucose positron emission tomography; HNSCC, head and neck squamous cell carcinoma; MRI, magnetic resonance imaging; NPC, nasopharyngeal carcinoma; OME, otitis media with effusion; OSA, obstructive sleep apnea; OSAH, obstructive sleep apnea-hypopnea; PET-CT, positron emission tomography-computed tomography; TSH, thyroid stimulating hormone; RAI, radioiodine.
Discussion
In an effort to limit healthcare expenditures and to allocate resources efficiently, many groups have focused their work on the economic appraisal of clinical interventions. As healthcare costs rise, it remains unclear how the increasing economic burden will be handled. There is an increasing need for policy makers, administrators, and physicians alike to evaluate the cost-effectiveness of the services provided. Assessment of value has been investigated for decades, with an exponential increase in cost effectiveness analyses published in the past 10 years. Cost effectiveness research in otolaryngology may have an especially profound impact on limiting healthcare expenditures, as otolaryngologists manage many conditions associated with high costs. The cost of allergic rhinitis alone has been estimated to be close to 5.3 billions dollars per year in the United States.6 Interestingly, these costs are far surpassed by that of managing sinusitis, which impacts one in seven adults and has direct costs alone estimated at 5.8 billion dollars per year.7 Within otolaryngology, the management of head and neck cancer and thyroid disease is also especially costly, with only a portion of the costs reflected in direct expenditures of imaging, surgery, and radiation therapy. As healthcare costs continue to rise, it is vital that otolaryngologists take on a more active role in assessing the cost effectiveness of various management options as more expensive innovative technologies continue to be developed.
We have evaluated the CEA registry to assess the characteristics, results and quality of CUAs, which include only those studies measuring health benefits in QALYs, in otolaryngology. Despite the high cost of managing conditions in the practice of otolaryngology, only 2% of the total CUA literature in the CEA registry evaluates intervention sutilized by otolaryngologists and only 0.61% of the cost utility literature in the CEA registry included an otolaryngologist as an author. The relative paucity of otolaryngologists with published studies in the CEA registry may be related to a relative infrequency of conditions with well-established QALYs, fewer clinicians in otolaryngology with training to perform these investigations, or perhaps decreased awareness of these issues among otolaryngologists. Regardless of the reason, it is important that otolaryngologists become more involved in conducting these studies in order to actively participate in discussions regarding the allocation of heath care resources.
In a recent review assessing the quality of 50 economic evaluations published in otolaryngology, Liu and colleagues found that study characteristics such as journal impact factor and presence of an author with a PhD in health economics were associated with higher quality studies.8 Interestingly, in our study, the subjective quality score bestowed by the CEA registry revealed no statistically significant correlation between the quality of the manuscripts and the number of otolaryngologist authors or the impact factor of the journal in which the study was published. Our review did reveal that studies with a more recent publication year are associated with a higher quality score, indicating that despite the relative lack of CUAs related to otolaryngology, the studies have been improving in both quantity and quality in recent years. Assessment of the topics addressed by all of the studies and their collective results revealed that unilateral cochlear implantation is cost effective in all settings evaluated. Furthermore, 86% of studies identified CPAP to be a cost effective strategy for the management of OSA (Table 3).
Although the relatively large number of studies evaluated and the use of the CEA registry make this review unique, there are several limitations. The CEA registry is a limited database with regards to cost effectiveness literature as a whole. It is possible that many other cost-effectiveness analyses related to otolaryngology that do not adhere to the stringent CUA criteria, yet have made important contributions to understanding the cost of interventions in otolaryngology, have not been evaluated in this particular study. We did not perform our own manual search of all English literature to ensure that no publications were missing from the CEA registry, nor did we perform our own assessment of the individual studies included in this study. Despite this, we are the first group to perform a review of the CUA literature in otolaryngology that has fit the inclusion criteria of the CEA registry. Future reviews of CUAs in otolaryngology may wish to combine search results from multiple databases in order to more comprehensively review the literature in this field.
Conclusion
Based on current evidence in the CEA registry, there is consensus that unilateral cochlear implantation for hearing loss and near consensus that CPAP for OSA are both cost effective interventions. Although CUAs in otolaryngology have increased in quantity and quality in more recent years, there is a lack of CUAs evaluating interventions in otolaryngology. A significant need exists for more otolaryngologists to become involved in evaluating the cost effectiveness of the therapeutic interventions they utilize.
Conflicts of interest/disclosures
None to report.
Funding information
No grant support was received in the preparation of this study.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Russell L.B., Gold M.R., Siegel J.E., Daniels N., Weinstein M.C. The role of cost-effectiveness analysis in health and medicine. Panel on cost-effectiveness in health and medicine. JAMA. 1996;276:1172–1177. [PubMed] [Google Scholar]
- 2.Muennig P. Jossey-Bass; San Francisco: 2008. Cost-effectiveness Analyses in Health: A Practical Approach. [Google Scholar]
- 3.Alter B.P. Cancer in Fanconi anemia, 1927–2001. Cancer. 2003;97:425–440. doi: 10.1002/cncr.11046. [DOI] [PubMed] [Google Scholar]
- 4.Dedhia R.C., Smith K.J., Johnson J.T., Roberts M. The cost-effectiveness of community-based screening for oral cancer in high-risk males in the United States: a Markov decision analysis approach. Laryngoscope. 2011;121:952–960. doi: 10.1002/lary.21412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O'Brien M.A., Prosser L.A., Paradise J.L. New vaccines against otitis media: projected benefits and cost-effectiveness. Pediatrics. 2009;123:1452–1463. doi: 10.1542/peds.2008-1482. [DOI] [PubMed] [Google Scholar]
- 6.Ray N.F., Baraniuk J.N., Thamer M. Direct expenditures for the treatment of allergic rhinoconjunctivitis in 1996, including the contributions of related airway illnesses. J Allergy Clin Immunol. 1999;103:401–407. doi: 10.1016/s0091-6749(99)70463-x. [DOI] [PubMed] [Google Scholar]
- 7.Rosenfeld R.M., Andes D., Bhattacharyya N. Clinical practice guideline: adult sinusitis. Otolaryngol Head Neck Surg. 2007;137:S1–S31. doi: 10.1016/j.otohns.2007.06.726. [DOI] [PubMed] [Google Scholar]
- 8.Liu C.C., Lui J., Oddone Paolucci E., Rudmik L. Systematic review of the quality of economic evaluations in the otolaryngology literature. Otolaryngol Head Neck Surg. 2015;152:106–115. doi: 10.1177/0194599814556725. [DOI] [PubMed] [Google Scholar]
- 9.Bisonni R.S., Lawler F.H., Pierce L. Recurrent otitis media: a cost-utility analysis of simulated treatment using tympanostomy tubes vs antibiotic prophylaxis. Fam Pract Res J. 1991;11:371–378. [PubMed] [Google Scholar]
- 10.Tousignant P., Cosio M.G., Levy R.D., Groome P.A. Quality adjusted life years added by treatment of obstructive sleep apnea. Sleep. 1994;17:52–60. [PubMed] [Google Scholar]
- 11.Evans A.R., Seeger T., Lehnhardt M. Cost-utility analysis of cochlear implants. Ann Otol Rhinol Laryngol Suppl. 1995;166:239–240. [PubMed] [Google Scholar]
- 12.Lea A.R., Hailey D.M. The cochlear implant. A technology for the profoundly deaf. Med Prog Technol. 1995;21:47–52. [PubMed] [Google Scholar]
- 13.Harris J.P., Anderson J.P., Novak R. An outcomes study of cochlear implants in deaf patients. Audiologic, economic, and quality-of-life changes. Arch Otolaryngol Head Neck Surg. 1995;121:398–404. doi: 10.1001/archotol.1995.01890040024004. [DOI] [PubMed] [Google Scholar]
- 14.Wyatt J.R., Niparko J.K., Rothman M., deLissovoy G. Cost utility of the multichannel cochlear implants in 258 profoundly deaf individuals. Laryngoscope. 1996;106:816–821. doi: 10.1097/00005537-199607000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Oh P.I., Maerov P., Pritchard D., Knowles S.R., Einarson T.R., Shear N.H. A cost-utility analysis of second-line antibiotics in the treatment of acute otitis media in children. Clin Ther. 1996;18:160–182. doi: 10.1016/s0149-2918(96)80188-3. [DOI] [PubMed] [Google Scholar]
- 16.Carter R., Hailey D. Economic evaluation of the cochlear implant. Int J Technol Assess Health Care. 1999;15:520–530. [PubMed] [Google Scholar]
- 17.Palmer C.S., Niparko J.K., Wyatt J.R., Rothman M., de Lissovoy G. A prospective study of the cost-utility of the multichannel cochlear implant. Arch Otolaryngol Head Neck Surg. 1999;125:1221–1228. doi: 10.1001/archotol.125.11.1221. [DOI] [PubMed] [Google Scholar]
- 18.O'Neill C., O'Donoghue G.M., Archbold S.M., Normand C. A cost-utility analysis of pediatric cochlear implantation. Laryngoscope. 2000;110:156–160. doi: 10.1097/00005537-200001000-00028. [DOI] [PubMed] [Google Scholar]
- 19.Cheng A.K., Rubin H.R., Powe N.R., Mellon N.K., Francis H.W., Niparko J.K. Cost-utility analysis of the cochlear implant in children. JAMA. 2000;284:850–856. doi: 10.1001/jama.284.7.850. [DOI] [PubMed] [Google Scholar]
- 20.Hollenbeak C.S., Lowe V.J., Stack B.C., Jr. The cost-effectiveness of fluorodeoxyglucose 18-F positron emission tomography in the N0 neck. Cancer. 2001;92:2341–2348. doi: 10.1002/1097-0142(20011101)92:9<2341::aid-cncr1581>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 21.Vidal-Trecan G.M., Stahl J.E., Durand-Zaleski I. Managing toxic thyroid adenoma: a cost-effectiveness analysis. Eur J Endocrinol. 2002;146:283–294. doi: 10.1530/eje.0.1460283. [DOI] [PubMed] [Google Scholar]
- 22.Bichey B.G., Hoversland J.M., Wynne M.K., Miyamoto R.T. Changes in quality of life and the cost-utility associated with cochlear implantation in patients with large vestibular aqueduct syndrome. Otol Neurotol. 2002;23:323–327. doi: 10.1097/00129492-200205000-00016. [DOI] [PubMed] [Google Scholar]
- 23.Francis H.W., Chee N., Yeagle J., Cheng A., Niparko J.K. Impact of cochlear implants on the functional health status of older adults. Laryngoscope. 2002;112:1482–1488. doi: 10.1097/00005537-200208000-00028. [DOI] [PubMed] [Google Scholar]
- 24.van der Meij E.H., Bezemer P.D., van der Waal I. Cost-effectiveness of screening for the possible development of cancer in patients with oral lichen planus. Community Dent Oral Epidemiol. 2002;30:342–351. doi: 10.1034/j.1600-0528.2002.00059.x. [DOI] [PubMed] [Google Scholar]
- 25.Summerfield A.Q., Marshall D.H., Barton G.R., Bloor K.E. A cost-utility scenario analysis of bilateral cochlear implantation. Arch Otolaryngol Head Neck Surg. 2002;128:1255–1262. doi: 10.1001/archotol.128.11.1255. [DOI] [PubMed] [Google Scholar]
- 26.Joore M.A., Van Der Stel H., Peters H.J., Boas G.M., Anteunis L.J. The cost-effectiveness of hearing-aid fitting in the Netherlands. Arch Otolaryngol Head Neck Surg. 2003;129:297–304. doi: 10.1001/archotol.129.3.297. [DOI] [PubMed] [Google Scholar]
- 27.Wilson L., Lin E., Lalwani A. Cost-effectiveness of intraoperative facial nerve monitoring in middle ear or mastoid surgery. Laryngoscope. 2003;113:1736–1745. doi: 10.1097/00005537-200310000-00015. [DOI] [PubMed] [Google Scholar]
- 28.Group UKCIS Criteria of candidacy for unilateral cochlear implantation in postlingually deafened adults II: cost-effectiveness analysis. Ear Hear. 2004;25:336–360. doi: 10.1097/01.aud.0000134550.80305.04. [DOI] [PubMed] [Google Scholar]
- 29.Vidal-Trecan G.M., Stahl J.E., Eckman M.H. Radioiodine or surgery for toxic thyroid adenoma: dissecting an important decision. A cost-effectiveness analysis. Thyroid. 2004;14:933–945. doi: 10.1089/thy.2004.14.933. [DOI] [PubMed] [Google Scholar]
- 30.Sejean K., Calmus S., Durand-Zaleski I. Surgery versus medical follow-up in patients with asymptomatic primary hyperparathyroidism: a decision analysis. Eur J Endocrinol. 2005;153:915–927. doi: 10.1530/eje.1.02029. [DOI] [PubMed] [Google Scholar]
- 31.Blamey S., Barraclough B., Delbridge L., Mernagh P., Standfield L., Weston A. Using recombinant human thyroid-stimulating hormone for the diagnosis of recurrent thyroid cancer. ANZ J Surg. 2005;75:10–20. doi: 10.1111/j.1445-2197.2005.03281.x. [DOI] [PubMed] [Google Scholar]
- 32.Brown D.L., Chervin R.D., Hickenbottom S.L., Langa K.M., Morgenstern L.B. Screening for obstructive sleep apnea in stroke patients: a cost-effectiveness analysis. Stroke. 2005;36:1291–1293. doi: 10.1161/01.STR.0000166055.52742.2b. [DOI] [PubMed] [Google Scholar]
- 33.Van Howe R.S., Kusnier L.P., 2nd Diagnosis and management of pharyngitis in a pediatric population based on cost-effectiveness and projected health outcomes. Pediatrics. 2006;117:609–619. doi: 10.1542/peds.2005-0879. [DOI] [PubMed] [Google Scholar]
- 34.Ayas N.T., FitzGerald J.M., Fleetham J.A. Cost-effectiveness of continuous positive airway pressure therapy for moderate to severe obstructive sleep apnea/hypopnea. Arch Intern Med. 2006;166:977–984. doi: 10.1001/archinte.166.9.977. [DOI] [PubMed] [Google Scholar]
- 35.Barton G.R., Stacey P.C., Fortnum H.M., Summerfield A.Q. Hearing-impaired children in the United Kingdom, IV: cost-effectiveness of pediatric cochlear implantation. Ear Hear. 2006;27:575–588. doi: 10.1097/01.aud.0000233967.11072.24. [DOI] [PubMed] [Google Scholar]
- 36.Zanocco K., Angelos P., Sturgeon C. Cost-effectiveness analysis of parathyroidectomy for asymptomatic primary hyperparathyroidism. Surgery. 2006;140:874–881. doi: 10.1016/j.surg.2006.07.032. discussion 881–872. [DOI] [PubMed] [Google Scholar]
- 37.Coco A.S. Cost-effectiveness analysis of treatment options for acute otitis media. Ann Fam Med. 2007;5:29–38. doi: 10.1370/afm.626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Narayan R., Perkins R.M., Berbano E.P. Parathyroidectomy versus cinacalcet hydrochloride-based medical therapy in the management of hyperparathyroidism in ESRD: a cost utility analysis. Am J Kidney Dis. 2007;49:801–813. doi: 10.1053/j.ajkd.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 39.Keiding H., Jorgensen K.P. A cost-effectiveness analysis of immunotherapy with SQ allergen extract for patients with seasonal allergic rhinoconjunctivitis in selected European countries. Curr Med Res Opin. 2007;23:1113–1120. doi: 10.1185/030079907x187865. [DOI] [PubMed] [Google Scholar]
- 40.Anzai Y., Jarvik J.G., Sullivan S.D., Hollingworth W. The cost-effectiveness of the management of acute sinusitis. Am J Rhinol. 2007;21:444–451. doi: 10.2500/ajr.2007.21.3009. [DOI] [PubMed] [Google Scholar]
- 41.Veenstra D.L., Harris J., Gibson R.L., Rosenfeld M., Burke W., Watts C. Pharmacogenomic testing to prevent aminoglycoside-induced hearing loss in cystic fibrosis patients: potential impact on clinical, patient, and economic outcomes. Genet Med. 2007;9:695–704. doi: 10.1097/gim.0b013e318156dd07. [DOI] [PubMed] [Google Scholar]
- 42.Lojander J., Rasanen P., Sintonen H., Roine R.P., Group H.U.S.Q.S. Effect of nasal continuous positive airway pressure therapy on health-related quality of life in sleep apnoea patients treated in the routine clinical setting of a university hospital. J Int Med Res. 2008;36:760–770. doi: 10.1177/147323000803600418. [DOI] [PubMed] [Google Scholar]
- 43.Chang W.H., Tseng H.C., Chao T.K., Hsu C.J., Liu T.C. Measurement of hearing aid outcome in the elderly: comparison between young and old elderly. Otolaryngol Head Neck Surg. 2008;138:730–734. doi: 10.1016/j.otohns.2008.02.012. [DOI] [PubMed] [Google Scholar]
- 44.Bruggenjurgen B., Reinhold T., Brehler R. Cost-effectiveness of specific subcutaneous immunotherapy in patients with allergic rhinitis and allergic asthma. Ann Allergy Asthma Immunol. 2008;101:316–324. doi: 10.1016/S1081-1206(10)60498-X. [DOI] [PubMed] [Google Scholar]
- 45.Brown B., Diamantopoulos A., Bernier J. An economic evaluation of cetuximab combined with radiotherapy for patients with locally advanced head and neck cancer in Belgium, France, Italy, Switzerland, and the United Kingdom. Value Health. 2008;11:791–799. doi: 10.1111/j.1524-4733.2007.00302.x. [DOI] [PubMed] [Google Scholar]
- 46.Guest J.F., Helter M.T., Morga A., Stradling J.R. Cost-effectiveness of using continuous positive airway pressure in the treatment of severe obstructive sleep apnoea/hypopnoea syndrome in the UK. Thorax. 2008;63:860–865. doi: 10.1136/thx.2007.086454. [DOI] [PubMed] [Google Scholar]
- 47.Tan M.C., Ayas N.T., Mulgrew A. Cost-effectiveness of continuous positive airway pressure therapy in patients with obstructive sleep apnea-hypopnea in British Columbia. Can Respir J. 2008;15:159–165. doi: 10.1155/2008/719231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zanocco K., Sturgeon C. How should age at diagnosis impact treatment strategy in asymptomatic primary hyperparathyroidism? A cost-effectiveness analysis. Surgery. 2008;144:290–298. doi: 10.1016/j.surg.2008.03.044. [DOI] [PubMed] [Google Scholar]
- 49.Mernagh P., Suebwongpat A., Silverberg J., Weston A. Cost-effectiveness of using recombinant human thyroid-stimulating hormone before radioiodine ablation for thyroid cancer: the Canadian perspective. Value Health. 2010;13:180–187. doi: 10.1111/j.1524-4733.2009.00650.x. [DOI] [PubMed] [Google Scholar]
- 50.Sher D.J., Tishler R.B., Annino D., Punglia R.S. Cost-effectiveness of CT and PET-CT for determining the need for adjuvant neck dissection in locally advanced head and neck cancer. Ann Oncol. 2010;21:1072–1077. doi: 10.1093/annonc/mdp405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Seidler A.M., Bramlette T.B., Washington C.V., Szeto H., Chen S.C. Mohs versus traditional surgical excision for facial and auricular nonmelanoma skin cancer: an analysis of cost-effectiveness. Dermatol Surg. 2009;35:1776–1787. doi: 10.1111/j.1524-4725.2009.01291.x. [DOI] [PubMed] [Google Scholar]
- 52.Kneis K.C., Gandjour A. Economic evaluation of Sinfrontal in the treatment of acute maxillary sinusitis in adults. Appl Health Econ Health Policy. 2009;7:181–191. doi: 10.1007/BF03256151. [DOI] [PubMed] [Google Scholar]
- 53.Yen R.F., Yen M.F., Hong R.L., Tzen K.Y., Chien C.R., Chen T.H. The cost-utility analysis of 18-fluoro-2-deoxyglucose positron emission tomography in the diagnosis of recurrent nasopharyngeal carcinoma. Acad Radiol. 2009;16:54–60. doi: 10.1016/j.acra.2008.06.012. [DOI] [PubMed] [Google Scholar]
- 54.Weatherly H.L., Griffin S.C., Mc Daid C. An economic analysis of continuous positive airway pressure for the treatment of obstructive sleep apnea-hypopnea syndrome. Int J Technol Assess Health Care. 2009;25:26–34. doi: 10.1017/S0266462309090047. [DOI] [PubMed] [Google Scholar]
- 55.Witt C.M., Reinhold T., Jena S., Brinkhaus B., Willich S.N. Cost-effectiveness of acupuncture in women and men with allergic rhinitis: a randomized controlled study in usual care. Am J Epidemiol. 2009;169:562–571. doi: 10.1093/aje/kwn370. [DOI] [PubMed] [Google Scholar]
- 56.Sadatsafavi M., Marra C.A., Ayas N.T., Stradling J., Fleetham J. Cost-effectiveness of oral appliances in the treatment of obstructive sleep apnoea-hypopnoea. Sleep Breath. 2009;13:241–252. doi: 10.1007/s11325-009-0248-4. [DOI] [PubMed] [Google Scholar]
- 57.Hernandez R.A., Sullivan F., Donnan P., Swan I., Vale L., Group B.T. Economic evaluation of early administration of prednisolone and/or aciclovir for the treatment of Bell's palsy. Fam Pract. 2009;26:137–144. doi: 10.1093/fampra/cmn107. [DOI] [PubMed] [Google Scholar]
- 58.Snedecor S.J., Botteman M.F., Bojke C., Schaefer K., Barry N., Pickard A.S. Cost-effectiveness of eszopiclone for the treatment of adults with primary chronic insomnia. Sleep. 2009;32:817–824. doi: 10.1093/sleep/32.6.817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.In H., Pearce E.N., Wong A.K., Burgess J.F., McAneny D.B., Rosen J.E. Treatment options for Graves disease: a cost-effectiveness analysis. J Am Coll Surg. 2009;209:170–179. doi: 10.1016/j.jamcollsurg.2009.03.025. e171–172. [DOI] [PubMed] [Google Scholar]
- 60.Wang T.S., Cheung K., Mehta P., Roman S.A., Walker H.D., Sosa J.A. To stimulate or withdraw? A cost-utility analysis of recombinant human thyrotropin versus thyroxine withdrawal for radioiodine ablation in patients with low-risk differentiated thyroid cancer in the United States. J Clin Endocrinol Metab. 2010;95:1672–1680. doi: 10.1210/jc.2009-1803. [DOI] [PubMed] [Google Scholar]
- 61.Summerfield A.Q., Lovett R.E., Bellenger H., Batten G. Estimates of the cost-effectiveness of pediatric bilateral cochlear implantation. Ear Hear. 2010;31:611–624. doi: 10.1097/AUD.0b013e3181de40cd. [DOI] [PubMed] [Google Scholar]
- 62.Petrou S., Dakin H., Abangma G., Benge S., Williamson I. Cost-utility analysis of topical intranasal steroids for otitis media with effusion based on evidence from the GNOME trial. Value Health. 2010;13:543–551. doi: 10.1111/j.1524-4733.2010.00711.x. [DOI] [PubMed] [Google Scholar]
- 63.Pietzsch J.B., Garner A., Cipriano L.E., Linehan J.H. An integrated health-economic analysis of diagnostic and therapeutic strategies in the treatment of moderate-to-severe obstructive sleep apnea. Sleep. 2011;34:695–709. doi: 10.5665/SLEEP.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Scott G.W., Scott H.M., O'Keeffe K.M., Gander P.H. Insomnia – treatment pathways, costs and quality of life. Cost Eff Resour Alloc. 2011;9:10. doi: 10.1186/1478-7547-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Li H., Robinson K.A., Anton B., Saldanha I.J., Ladenson P.W. Cost-effectiveness of a novel molecular test for cytologically indeterminate thyroid nodules. J Clin Endocrinol Metab. 2011;96:E1719–E1726. doi: 10.1210/jc.2011-0459. [DOI] [PubMed] [Google Scholar]
- 66.Higgins K.M. What treatment for early-stage glottic carcinoma among adult patients: CO2 endolaryngeal laser excision versus standard fractionated external beam radiation is superior in terms of cost utility? Laryngoscope. 2011;121:116–134. doi: 10.1002/lary.21226. [DOI] [PubMed] [Google Scholar]