Abstract
Objective
Leptospermum Honey (Manuka honey) has proven to be effective in improving acute and chronic wound healing presumably due to its antibacterial and anti-inflammatory properties. The aim is to determine if Manuka honey decreases scar formation and results in a cosmetically appealing scar.
Methods
A prospective single-blinded randomized control trial was performed. All patients received an 8 cm incision. Patients randomized to honey treatment were instructed to apply Manuka honey paste topically to the incision site once per day post surgery for 4 weeks. The patients' scar was then analyzed objectively by a blinded observer and subjectively at 4 and 8 weeks postoperatively. The primary outcome measure used was the Patient and Observer Scar Assessment Scale (POSAS).
Results
A total of 21 patients completed the entire scar analysis (honey treatment = 9, standard treatment = 12). There was no statistically significant difference between patient scar assessment scale and observer scar assessment scale at 4 and 8 weeks postoperatively.
Conclusion
Despite Leptospermum Honey's reported anti-inflammatory and antibacterial properties, this study did not show a difference in scar appearance when applied.
Keywords: Thyroid, Thyroidectomy, Scar, Aesthetics, Honey, Topical, Wound healing, Naturopathic
Introduction
Thyroidectomy is a very common surgical procedure. The current standard of care is to perform thyroidectomy by an open technique.1, 2 This is generally well tolerated and has proven an effective and efficient way of removing thyroid tissue. Even though well tolerated, open thyroidectomy leaves the patient with an approximately eight centimeter scar – a non-cosmetic result. This fact has generated investigation into a number of cosmetically favorable approaches in performing thyroid surgery. Endoscopically assisted open thyroid surgery with reduced incision size and endoscopic thyroid surgery through the axilla or anterior chest wall are the most common surgical innovations. Although promising, thyroid surgery utilizing endoscopy has so far had limited application, and the majority of thyroidectomy must still be performed openly.1, 2 Therefore, there is need for a method to improve healing and reduce scar formation.3 Much research has gone into topical agents applied to incision sites. To date only silicone gel sheeting has consistently been shown to prevent formation and diminish appearance of hypertrophic scars.4 In this study, we were interested in evaluating the potential benefits topical Manuka honey has on wound healing and reduction of scar formation.
Manuka honey is a monofloral honey that comes from Leptospermum tree pollen in New Zealand and Australia.5 Generic honey has been used in medicine for a number of years. There is good evidence for its use topically as a barrier and an antiseptic.6, 7 Manuka honey is known to have added antibacterial benefits, which are attributed to an additional unique non-peroxidase activity described as Unique Manuka Factor (UMF).5 In addition, evidence from animal trials suggests Manuka honey improves healing of ulcers, lacerations and burns. Currently, Manuka honey is most commonly used as a topical application to treat partial to full thickness burns as well as venous leg ulcers.5, 7 Manuka honey has been used elsewhere in Otolaryngology, including in the management of chronic pilonidal sinus wounds and nasal mucosal healing following function endoscopic sinus surgery.5, 8
Materials and methods
A prospective study was performed at Vancouver General Hospital, a tertiary referral center for thyroid cancer. This study obtained University of British Columbia Clinical Research Ethics Board approval. Patients undergoing a hemi- or total thyroidectomy were included in this study. All patients had to accept an incision site of 8 cm. Any incision made to be longer than 8 cm were removed from the study. All patients were 19 years of age or older. Patients were excluded if they were allergic to pollen, honey or bees.
Consecutive patients fitting the inclusion and exclusion criteria were approached to participate in the study by the research coordinator. If patients were agreeable to the study, the research coordinator used a closed envelope system to randomize each patient to either the treatment or control arm. The primary surgeon who performed all the surgeries was not aware of the study arm throughout the study. The treatment arm consisted of patients using a honey gel paste (MediHoney®) containing 95% active Leptospermum honey. The paste was applied by hand to the incision site once per day during the 4 weeks after surgery and left in place to dry. Patients were instructed to clean the incision site daily with mild soap and water. If patients anticipated extended sun exposure, they were to place sunscreen on the incision site. In similar fashion, the control arm cleaned the incision site daily with mild soap and water and applied sunscreen on the incision site if they anticipated sun exposure; however, they did not use any form a scar reducing agent or antibacterial cream.
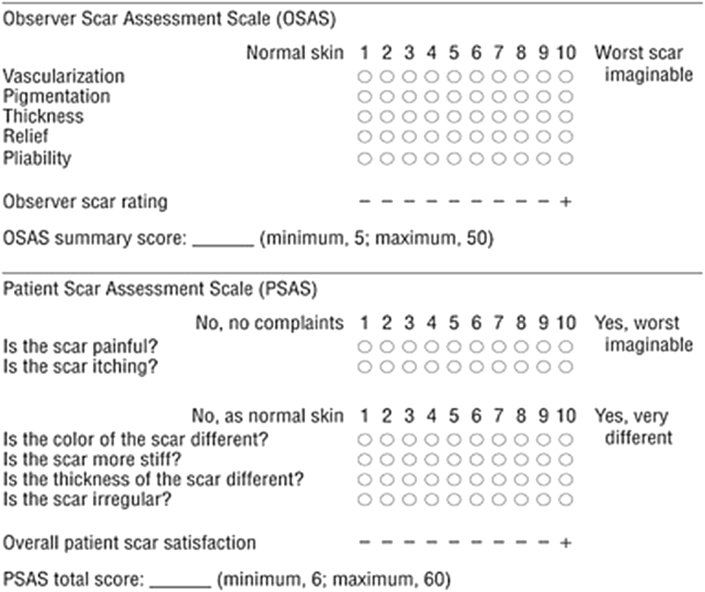
Patients underwent formal objective and subjective analysis at 4 and 8 weeks postoperatively. At the scar analysis visit, patient's sex, age, and Fitzpatrick skin classification was recorded. The scar was then assessed subjectively and then objectively using a validated scar assessment scale used known as the Patient and Observer Scar Assessment Scale (POSAS) (Fig. 1).9 Objective scoring was performed by the senior resident, who was also unaware of the treatment arm of each patient.
Fig. 1.
Patient and observer scar assessment scale (POSAS). Subjective and objective, validated scale used to evaluate scarring. Data shown represents scores 4 and 8 weeks following thyroidectomy.
A priori, it was determined that a minimum of nine patients were required in each study arm to appropriately power the study based on a study by O'Connel et al.10 They based their calculations after determining the minimal important clinical difference required in using the POSAS based on an α of 0.05 and a power of 0.80. Statistical analysis was performed using GraphPad 5.0. Continuous data was assessed using the Mann–Whitney test and the Fischer exact for categorical data.
Results
A total of 21 patients completed the entire scar analysis study. Thirty-seven patients consented to partake in the study, 18 of whom never completed the long-term scar analysis assessment. The cohort that completed the study was analyzed, which consisted of 12 control arm patients and 9 treatment arm patients. There were 4 males in the control arm and 2 males in the treatment arm. The average age was 49 years old and 53 years old for the control and treatment arm, respectively. With respect to the Fitzpatrick skin classification, the control group had 1 individual with type 1 skin, 3 with type 2 skin, 4 with type 3 skin and 4 with type 4 skin. The treatment arm had 2 with type 2 skin, 3 with type 3 skin, 2 with type 4 skin and 2 with type 5 skin. Given the limited number of patients in this study and the varying Fitzpatrick skin classification observed in these 21 participants, statistical comparison based on skin classification was not performed. Qualitatively speaking, no difference in healing was observed among patients in the different classifications.
The objective measures of vascularization, pigmentation, thickness and pliability within the control group significantly improved between the 4th and 8th week. Those using the honey only saw significant improvement in thickness and pliability between the 4th and 8th week (Table 1). Interestingly, at the 8th week mark, the mean pigmentation score for those applying honey was much lower than those in the control arm (P = 0.008). The remaining descriptive means at the 8th week were similar to those in the control arm (P > 0.05).
Table 1.
Observer scar assessment scale score for each subheading at 4th and 8th week.
| Arm | Time point | Vascularization | Pigmentation | Thickness | Relief | Pliability | |
|---|---|---|---|---|---|---|---|
| Control arm | 4th Week | Mean | 3.17 | 4.67 | 3.75 | 3 | 4.42 |
| SD | 2.03 | 1.78 | 1.96 | 2 | 2.15 | ||
| 8th Week | Mean | 1.17 | 3.25 | 1.67 | 2.25 | 1.92 | |
| SD | 0.39 | 1.71 | 0.89 | 2.05 | 1.24 | ||
| P value | 0.001 | 0.049 | 0.003 | 0.233 | 0.001 | ||
| Honey arm | 4th Week | Mean | 2.33 | 4.67 | 3.17 | 3.17 | 3.67 |
| SD | 2.16 | 3.27 | 0.75 | 2.92 | 1.03 | ||
| 8th Week | Mean | 1.67 | 1.83 | 1.17 | 1.5 | 1.33 | |
| SD | 0.82 | 0.98 | 0.41 | 1.22 | 0.52 | ||
| P value | 0.999 | 0.134 | 0.004 | 0.067 | 0.031 |
The objective scare rating score (out of 10) with a higher scar indicating “worst scar imaginable” illustrated no difference between the honey arm and control arm at the 4th and 8th week (Table 2). Both groups also showed similar improvement in their scar between fourth and eighth week (Fig. 2). Subjective analysis also illustrated similar results. There was no difference between the control and honey arm at the fourth and eighth week (Table 3, Fig. 3, Fig. 4). Given the lack of significance in patient scar assessment and observer scar assessment scales between the two arms at 8 weeks, data was not collected over a longer period of time.
Table 2.
Observer scar rating score at 4th and 8th week.
| Arm | 4th week | 8th week | Δ 8−4th week | |
|---|---|---|---|---|
| Control arm | Mean | 4.08 | 2.92 | −1.16 |
| SD | 1.31 | 1.56 | 1.64 | |
| Honey arm | Mean | 4.17 | 2.83 | −1.34 |
| SD | 2.4 | 2.64 | 3.5 | |
| P value | 0.75 | 0.525 | 0.512 |
Δ = change; means and standard deviations were determined from the POSAS. Similar differences in scores were observed at 4 and 8 weeks post-thyroidectomy in both the control and treatment groups.
Fig. 2.
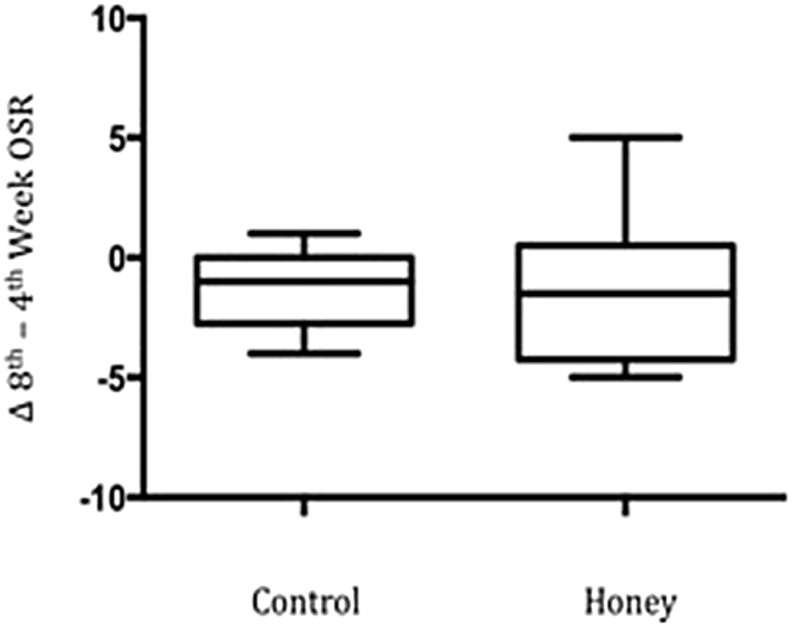
Change in observer scar rating score between 8th and 4th weeks. Box-and-whisker plot showing difference in OSR between 8th and 4th weeks post-thyroidectomy in treatment and control groups. (OSR = Observer Scar Rating).
Table 3.
Overall patient scar satisfaction score at 4th and 8th week.
| Arm | 4th week | 8th week | Δ 8−4th week | |
|---|---|---|---|---|
| Control arm | Mean | 3.42 | 1.92 | −1.5 |
| SD | 1.83 | 1.65 | 1.62 | |
| Honey arm | Mean | 3.33 | 1.5 | −1.83 |
| SD | 1.5 | 0.84 | 1.6 | |
| P value | 0.999 | 0.457 | 0.672 |
Δ = change; overall scores collected from POSAS. No significant mean difference demonstrated between treatment and control group at 4 and 8 weeks postoperatively.
Fig. 3.
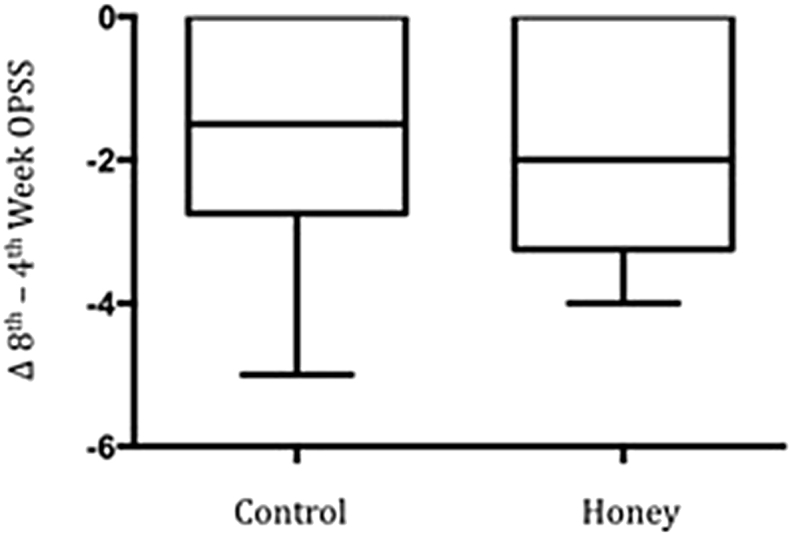
Change in overall patient scar satisfaction score between 8th and 4th weeks. Box-and-whisker plot demonstrating difference in OPSS between 8th and 4th weeks postoperatively for treatment and control groups. (OPSS = Overall Patient Scar Satisfaction).
Fig. 4.
Scars in both treatment arms at 8 weeks postoperatively. Images depicting scars at 8 weeks postoperatively in the control (left) and treatment (right) arms.
Discussion
Honey is a supersaturated sugar solution that is viscous in nature. Honeybees, Apis mellifera, gather nectar from flowering plants for its production. Honey is composed of approximately 40% fructose, 30% glucose, 5% sucrose, and 20% water, as well as vitamins, minerals, enzymes and amino acids in combinations unique to each variety.5, 7 Honey has long been used in medicine, but its use in modern medicine has been limited until recently. Looking back, Discords and Hippocrates advocated for the use of honey as a vehicle for carrying therapeutic agents.7, 11, 12 One of the first recorded uses of honey as a medicinal treatment is from the Edwin Smith papyrus; it describes the Egyptians using honey as treatment to prevent infection in surgical wounds.7
Honey has well-established antibacterial properties. Research has shown the hyperosmotic nature and low pH-value of honey contributes to its antibacterial properties. In addition, its hydrogen peroxide activity acts like a detergent giving it comparable antibacterial activity to phenolic acid.12, 13 Manuka honey has additional antibiotic properties, which are not dependent on peroxidase activity. This has been described as unique manuka factor and has recently been linked to methylglyoxal. It is for this reason that Manuka honey has become the most prominently used variety of honey for medical purposes.13
In terms of healing, honey works in a number of ways. As a result of its hypersaturated nature it is thought to act osmotically drawing fluid and nutrients to the area of application in tandem with keeping the wound moist.12 In histological studies, it appears to stimulate growth of developing tissues, leading to faster tissue repair.6 Honey has also been observed to attenuate the inflammatory phase of healing.14 In addition, animal studies have documented improvement in epitheliazation.15
Unfortunately, there are a number of downfalls regarding the topical use of honey over the anterior aspect of the neck. The honey arm had trouble maintaining compliancy, and a number of patients dropped out of the study. A major complaint of the “honey arm” involved the sticky and viscous nature of Manuka honey. Participants complained that the Manuka honey got on their clothing and trapped foreign debris in the area of their incision. Participants also found the daily application of the honey excessive. There were no reported complications from patients or the blinded observer. This study illustrated there is essentially no difference between those applying honey and those in the control arm. The only significant benefit with those using honey is the potential improvement in pigmentation.
Conclusions
In summary, although animal and histological studies have shown improved epithelial repair with the application of honey, this study demonstrates that no clinical effect can be appreciated when applying honey for scar reduction. The cause of the discordance between this study and prior animal and histological studies is unclear and requires further evaluation. Regardless of these findings, however, honey continues to have its place in modern medicine.
Conflict of interest statement
The authors declare no conflicts of interest relevant to this report.
Financial disclosures
The authors have not received any funding sources for this study.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Dionigi G., Boni L., Duran-Poveda M. Evolution of endoscopic thyroidectomy. Surg Endosc. 2011;25:3951–3952. doi: 10.1007/s00464-011-1763-5. [DOI] [PubMed] [Google Scholar]
- 2.Ikeda Y., Takami H., Sasaki Y., Takayama J., Niimi M., Kan S. Comparative study of thyroidectomies. Endoscopic surgery versus conventional open surgery. Surg Endosc. 2002;16:1741–1745. doi: 10.1007/s00464-002-8830-x. [DOI] [PubMed] [Google Scholar]
- 3.Doillon C.J., Dunn M.G., Bender E., Silver F.H. Collagen fiber formation in repair tissue: development of strength and toughness. Coll Relat Res. 1985;5:481–492. doi: 10.1016/s0174-173x(85)80002-9. [DOI] [PubMed] [Google Scholar]
- 4.McGrath M.H., Chang D.S. Topical scar modification: hype or help? Aesthet Surg J. 2005;25:304–306. doi: 10.1016/j.asj.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 5.Thomas M., Hamdan M., Hailes S., Walker M. Manuka honey as an effective treatment for chronic pilonidal sinus wounds. J Wound Care. 2011;20 doi: 10.12968/jowc.2011.20.11.528. 530–523. [DOI] [PubMed] [Google Scholar]
- 6.Bergman A., Yanai J., Weiss J., Bell D., David M.P. Acceleration of wound healing by topical application of honey. An animal model. Am J Surg. 1983;145:374–376. doi: 10.1016/0002-9610(83)90204-0. [DOI] [PubMed] [Google Scholar]
- 7.Jull A.B., Rodgers A., Walker N. Honey as a topical treatment for wounds. Cochrane Database Syst Rev. 2008:CD005083. doi: 10.1002/14651858.CD005083.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Chang E.H., Alandejani T., Akbari E., Ostry A., Javer A. Double-blinded, randomized, controlled trial of medicated versus nonmedicated merocel sponges for functional endoscopic sinus surgery. J Otolaryngol Head Neck Surg. 2011;40:S14–S19. [PubMed] [Google Scholar]
- 9.Draaijers L.J., Tempelman F.R., Botman Y.A. The patient and observer scar assessment scale: a reliable and feasible tool for scar evaluation. Plast Reconstr Surg. 2004;113:1960–1967. doi: 10.1097/01.prs.0000122207.28773.56. [DOI] [PubMed] [Google Scholar]
- 10.O'Connell D.A., Diamond C., Seikaly H., Harris J.R. Objective and subjective scar aesthetics in minimal access vs conventional access parathyroidectomy and thyroidectomy surgical procedures: a paired cohort study. Arch Otolaryngol Head Neck Surg. 2008;134:85–93. doi: 10.1001/archotol.134.1.85. [DOI] [PubMed] [Google Scholar]
- 11.Eteraf-Oskouei T., Najafi M. Traditional and modern uses of natural honey in human diseases: a review. Iran J Basic Med Sci. 2013;16:731–742. [PMC free article] [PubMed] [Google Scholar]
- 12.Molan P.C. Why honey is effective as a medicine. Its use in modern medicine. Bee World. 1999;80:80–92. [Google Scholar]
- 13.Mavric E., Wittmann S., Barth G., Henle T. Identification and quantification of methylglyoxal as the dominant antibacterial constituent of Manuka (Leptospermum scoparium) honeys from New Zealand. Mol Nutr Food Res. 2008;52:483–489. doi: 10.1002/mnfr.200700282. [DOI] [PubMed] [Google Scholar]
- 14.Postmes T.J., Bosch M.M.C., Dutrieux R., van Baare J., Hoekstra M.J. Speeding up healing of burns with honey. An experimental study with histological assessment of wound biopsies. In: LYes Mizrahi A., editor. Bee Products: Properties, Applications and Apitherapy. Plenum Press; New York: 1997. [Google Scholar]
- 15.Oryan A., Zaker S.R. Effects of topical application of honey on cutaneous wound healing in rabbits. Zentralbl Veterinarmed A. 1998;45:181–188. doi: 10.1111/j.1439-0442.1998.tb00815.x. [DOI] [PubMed] [Google Scholar]