Abstract
Background
There is increasing evidence that biofilms are critical to the pathophysiology of chronic infections including chronic rhinosinusitis (CRS). Until relatively recently, our understanding of biofilms was limited. Recent advances in methods for biofilm identification and molecular biology have offered new insights into the role of biofilms in CRS. With these insights, investigators have begun to investigate novel therapeutic strategies that may disrupt or eradicate biofilms in CRS.
Objective
This review seeks to explore the evidence implicating biofilms in CRS, discuss potential anti-biofilm therapeutic strategies, and suggest future directions for research.
Results
The existing evidence strongly supports the role of biofilms in the pathogenesis of CRS. Several anti-biofilm therapies have been investigated for use in CRS and these are at variable stages of development. Generally, these strategies: 1) neutralize biofilm microbes; 2) disperse existing biofilms; or 3) disrupt quorum sensing. Several of the most promising anti-biofilm therapeutic strategies are reviewed.
Conclusions
A better understanding of biofilm function and their contribution to the CRS disease process will be pivotal to the development of novel treatments that may augment and, potentially, redefine the CRS treatment paradigm. There is tremendous potential for future research.
Keywords: Sinusitis, Biofilms, Anti-bacterial agents, Quorum sensing, Surface-active agents, Active immune response, Innate immune response
The etiology of chronic rhinosinusitis is multifactorial. The interaction between many systemic, local host, and environmental factors contribute to sinus inflammation and to the pathophysiology of disease. Systemic factors include genetic diseases such as cystic fibrosis, conditions causing immunodeficiency, autoimmune disease, idiopathic conditions such as Samter's triad (aspirin exacerbated respiratory disease), and acid reflux. Local host factors include sinonasal anatomic abnormalities, iatrogenic conditions such as scarring from prior sinus surgery, neoplasm, or the presence of a foreign body, among others. Possible environmental factors include the presence of biofilms and bacterial infection, as well as fungal infection, allergy, environmental pollutants, and smoking.
Over the last 15 years, increasing evidence has implicated biofilms in more than 65% of chronic infections in humans. Biofilms may also complicate infection management as they contribute to the development of antibiotic resistance and the inconsistency of culture results in certain illnesses.1 In otolaryngology, the controversial role of biofilms in chronic rhinosinusitis has been the focus of recent research. This review seeks to explore the evidence implicating biofilms in chronic rhinosinusitis, discuss potential anti-biofilm therapeutic strategies, and suggest future directions for research.
Defining biofilms
Bacteria exist in two distinct forms: biofilm and planktonic. Biofilm is the preferred state in which an estimated 99% of bacteria exist. The bacteria that constitute a biofilm display several critical differences in regard to growth dynamics and genetic expression relative to their planktonic counterparts.2, 3
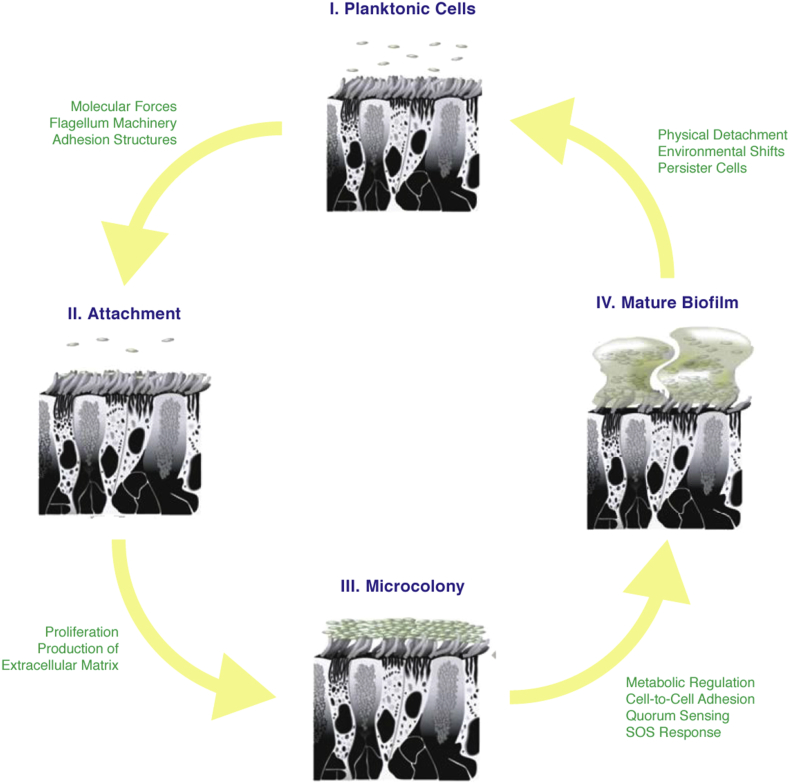
The development of a microbial biofilm is a complex process. Initially, sessile planktonic bacteria adhere to a surface and form microcolonies.4 Initial attachment is formed by weak van der Waals forces and may involve bacterial flagella.5 The expression of cell adhesion structures, including pili, is upregulated to allow for stronger, permanent interactions.6 Once attached, bacteria begin to proliferate and secrete an extracellular matrix composed of polysaccharides, nucleic acids, and proteins. This matrix protects the biofilm against harmful factors in the environment.
As the biofilm expands, the concentrations of several signaling molecules increase and lead to alterations in intracellular signaling. For example, cyclic di-guanosine monophosphate (c-di-GMP) serves to activate biofilm maturation through modulation of cell-to-cell adhesion, quorum sensing, metabolic regulation, stress response, and the phenotypic shift from the planktonic to biofilm state.7 Once mature, bacteria within the biofilm transcribe DNA in a synchronized manner exhibiting the characteristics of a single multicellular organism that colonizes host tissues. Biofilms then spread by releasing free floating planktonic bacteria from the most distal sites of the structure.8 These shed bacteria can then adhere to distant sites in the host (Fig. 1).9
Fig. 1.
The biofilm life cycle.10
Quorum sensing
Quorum sensing refers to the ability of bacterial cells to communicate. It is a cell density-dependent signal transduction process that allows for rapid coordination of behavior to stimulating factors in the environment. Through quorum sensing, biofilms can adapt to fluctuating levels of nutrients, competitive microorganisms, and toxic materials.11 Communication is mediated by small signal molecules called autoinducers (AIs) secreted by bacteria into the extracellular environment where they bind to specific bacterial cell membrane receptors. This binding initiates a signal transduction cascade modulating the expression of specific genes with downstream regulatory effectors.4 Three quorum sensing pathways have been identified. AI-1 refers to acyl-homoserine lactone (AHL) molecules which are produced by gram-negative bacteria only.12 AI-2 molecules function in both gram positive and negative communication.13 AI-3 is the least understood pathway but appears to involve molecules that influence the histidine kinase-linked receptor QseC.14
Antimicrobial resistance
Biofilms harbor a 10–1000 fold higher resistance to antimicrobials than planktonic bacteria.15 This resistance is a manifestation of the physical barrier properties of the extracellular matrix, the induction of a bacterial stress response, and coordinated behavior of the biofilm through quorum sensing. Antibiotic resistance also involves enzymatic inactivation of antibiotics, modification of antimicrobial end-targets, and efflux pump-mediated exclusion of antibiotics.4 Bacterial gene transference is also enhanced in biofilms—for example, transference of the CTX-M-15 gene confers cephalosporin resistance to Klebsiella pneumoniae biofilms.16
The extracellular matrix that encapsulates biofilms creates a physical diffusion barrier.17, 18 The viscosity of the outer slime layer prevents the diffusion of antibiotics into the deeper layers of the biofilm. Negatively charged components of the extracellular matrix repel positively charged antibiotics such as aminoglycosides.19 The extracellular matrix also harbors enzymes, such as beta-lactamases, which act to destroy the structural integrity of antibiotics.4
The spatial organization of biofilms and the induction of a bacterial stress response are closely related. Mature biofilms are structured in a stacked, multilayered topography where cells in the deeper layers are subject to a different environment than those in the more superficial layers.20 These different microenvironments alter gene expression and metabolic activity leading to heterogeneity within the community.12 Interior regions of the biofilm are also, typically, starved of nutrients and oxygen suppressing metabolism and growth rate as part of the bacterial stress response. Because antibiotics are generally more effective against fast growing cells, the stress response functions to increase antimicrobialresistance.21, 22
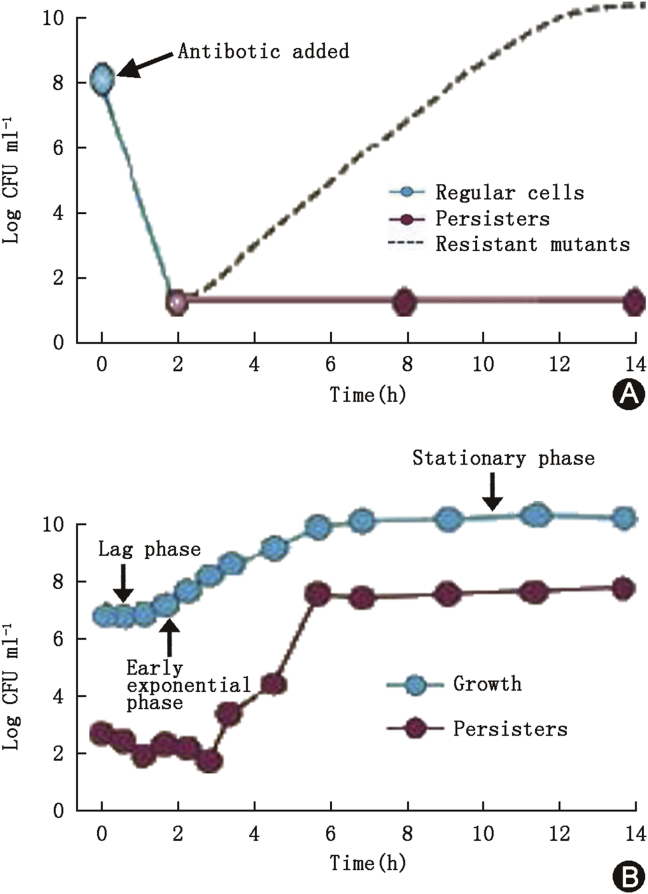
‘Persister cells’ which lie in a dormant state within the deep interior of a biofilm likely contribute to the recalcitrant nature of biofilm-mediated infections.23 The formation of this subpopulation may be triggered by the bacterial stress response and when the biofilm enters the mid-exponential growth phase.23, 24 Persister cells are able to endure high concentrations of antibiotics and promote infection by relocating to other host sites and forming new biofilms harboring the same resistant phenotype as the original population (Fig. 2).25
Fig. 2.
Formation of persister cells.23 A: Administration of antibiotic to a biofilm population resulting in cell death with the continued survival of a subpopulation of persister cells and resistant microbes. B: Frequency of isolation of persister cells as a function of the growth phase of the biofilm culture.
Biofilm-induced pathogenesis
Biofilms have been implicated in otitis media with effusion,26 cholesteatoma,27 and chronic tonsillitis.28 The contribution of biofilms to the pathogenesis of chronic rhinosinusitis remains less clear. Parsek and Singh developed specific diagnostic criteria for biofilm-associated infections in 2003 (Table 1).29
Table 1.
Diagnostic criteria for biofilm-associated infections.30
| Pathogenic bacteria must be associated with a surface |
| Direct examination of infected tissue must demonstrate aggregated cell clusters encased in a matrix, which may be of bacterial or host origin |
| Infection must be confined to a particular site of a host |
| Recalcitrance to antibiotic treatment despite demonstrated susceptibility of planktonic bacteria on sensitivity testing |
| Culture-negative results in the setting of a clinically documented high suspicion for infection |
| Evidence of ineffective host clearance as demonstrated by the presence of biofilm colonies in discrete areas in host tissue associated with host inflammatory cells |
Early research identified biofilm structures on the mucosal surfaces of patients with CRS.31, 32, 33 However, subsequent studies noted the absence of biofilms in diseased patients and their presence on the nasal mucosa of healthy controls.34, 35, 36 This variability highlights the complex multifactorial pathophysiology of CRS.9 The seemingly contradictory results noted might be partially attributable to differences in the biofilm detection methods used (Table 2).
Table 2.
Biofilm detection methods in chronic rhinosinusitis.9
| Study | Year | Detection method | CRS (%) | Control (%) |
|---|---|---|---|---|
| Ramadan et al34 | 2005 | SEM | 5/5 (100) | N/A |
| Sanclement et al32 | 2005 | SEM, TEM | 24/30 (80) | 0/4 (0) |
| Sanderson et al35 | 2006 | FISH | 14/18 (78) | 2/5 (40) |
| Psaltis et al37 | 2007 | CSLM | 17/38 (45) | 0/9 (0) |
| Healy et al36 | 2008 | FISH, epifluorescence microscopy | 9/11 (82) | 2/3 (67) |
| Bezzera et al38 | 2011 | SEM | 24/33 (73) | 13/27 (48) |
Several modalities exist for biofilm detection including scanning electron microscopy (SEM), transmission electron microscopy (TEM), fluorescence in situ hybridization (FISH), and confocal laser scanning microscopy (CLSM). Early biofilm detection studies used nonspecific techniques such as SEM and TEM, which allowed for ultrastructural analysis but did not allow for species identification.39 FISH-based studies use universal bacterial probes or species-specific primers.40, 41 FISH helped demonstrate that ex vivo nasal swab culture, used in early studies for biofilm species identification, was unreliable as it frequently sampled planktonic rather than biofilm bacteria.42, 43, 44 The main drawback of FISH is the need to presumptively identify the organism which is then probed, possibly overlooking pathogenic microbes.45 CLSM has emerged as the optimal biofilm detection approach in CRS.46, 47 CLSM allows for deep scanning of mucosal tissue, and species identification through concurrent FISH, LIVE/DEAD BacLight, or through the use of immunofluorescent markers.39, 41, 48
A complex polymicrobial community of both bacteria and fungi exists within biofilms.36, 39 Foreman et al demonstrated that Staphylococcus aureus was identified in 50% of biofilms from CRS patients, with Pseudomonas aeruginosa and Haemophilus influenza identified in 22% and 28% of cultures, respectively.39 Other bacterial species such as Streptococcus viridans, coagulase-negative staphylococci, Enterococcus faecalis, and S. viridans form biofilms in CRS patients.49 Anaerobes including Propionibacterium and Corynebacterium have been visualized.44, 45 The degree to which individual bacteria contribute to CRS disease pathogenesis remains unclear.
In 2008, twenty-five years after Katzenstein et al50 first reported fungus in the sinuses of CRS patients, Healy et al reported the coexistence of fungi and bacterial biofilms.36 In 2009, a study by Foreman et al51 found fungal biofilms in 11/50 (22%) of CRS patients with 7 of these cases demonstrating concomitant infection with S. aureus. Boase et al52 demonstrated that fungal inoculation of obstructed frontal sinuses in sheep led to robust biofilm formation, but only in the setting of S. aureus co-inoculation. Indeed, symbiotic interactions between bacteria and fungus may augment biofilm survival by enhancing the transfer of antimicrobial resistance traits, assisting surface adherence, and improving the protective effect of the extracellular matrix.53 To illustrate, Staphylococcus biofilms, when grown with Candida albicans, exhibit increased antimicrobial resistance and enhanced growth.54 Bacteria and fungi may also share molecular signaling. C. albicans secretes farnesol increasing the secretion of toxins by Pseudomonas species.55 Microbial synergism is corroborated in clinical studies. In one study, sinonasal mucosal antifungal IgE levels were significantly elevated in the presence of S. aureus.39 These findings suggest that S. aureus may either facilitate fungal growth or may, perhaps, cause mucosal injury allowing for fungal colonization and establishment of a chronic inflammatory state.
The potential significance of intracellular bacterial uptake has garnered significant attention. S. aureus is able to alter its phenotype following internalization into epithelial cells, adopting a more virulent phenotype and developing increased antibiotic resistance.56, 57 When this concept is extrapolated to CRS, it suggests that intracellular Staphylococci may play a role as a primary infectious agent and as a reservoir for reinfection.58 In a prospective trial of CRS patients, Tan et al59 demonstrated that the presence of intracellular bacteria in sinonasal tissue was associated with a significantly higher risk of late clinical and microbiological relapse, whereas the presence of biofilm on sinonasal mucosa without intracellular bacteria did not impact outcomes. Despite methodological limitations – specifically that clinical relapse was based on endoscopy and positive cultures instead of symptom scores – this study suggests that mucosal intracellular bacteria may promote disease recalcitrance.
Research suggests that the establishment of biofilms in the sinonasal mucosa and the resulting pathogenicity likely requires defects in adaptive and innate immunity. Innate immunity represents a first-line of defense against microbial infection and compromised function has been associated with biofilm formation. Biofilm formation has been associated with the down-regulation of antibacterial peptides such as lactoferrin and MUC7 in the nasal mucosa, and the down-regulation of toll-like receptors that recognize gram-positive bacteria.60, 61, 62 SEM studies indicate that the mucosa of CRS patients with biofilm-positive disease is markedly damaged compared to biofilm-negative mucosa. The severity of damage ranges from morphologic changes such as disarrayed cilia to reduced ciliary beat frequency to the complete absence of cilia.34, 63, 64, 65, 66 The resultant mucociliary impairment further promotes bacterial persistence.
The adaptive immune system consists of lymphocytes that identify and eliminate pathogens by recognition of surface antigens, allowing for the development of immunological memory. Hekiert et al demonstrated that biofilm presence correlated with a skewing of the adaptive immune response towards the T-helper 1 (Th1) response.67 The Th1 response is associated with the activation of cytotoxic T cells and macrophages for direct attack on pathogens. In this study, the levels of interferon-gamma, granulocyte colony-stimulating factor, macrophage inflammatory protein-1 beta, and neutrophils in the sinonasal mucosa were significantly elevated. A larger study several years later, however, demonstrated an association between S. aureus biofilms and a T-helper 2 (Th2) skewing of the adaptive response—more typically associated with hypersensitivity and allergic responses.68 Thus, the role of the T-helper response in the context of biofilm colonization remains unclear. There is increasing evidence that the presence of biofilms alters chemokine production, which may potentiate CRS. The production of interleukin-5, interleukin-6, and eosinophilic cationic protein is increased in the setting of biofilms.68, 69 This milieu of inflammatory cytokines may lead to mucosal inflammation, and osteitis of the underlying bone.70 The correlation, if any, between chemokine production, immunopathologic changes, and resultant symptoms of CRS has yet to be firmly elucidated.
Although consensus has yet to be reached, the concept of biofilm-induced CRS has been supported by a number of peer reviewed publications.(20–24) Together, these provide evidence that the expression of cytokines and cell surface proteins can be modulated in local mucosa secondary to the presence of bacterial biofilms. There is also evidence suggesting that the osteitic bone underlying biofilm-infected mucosa can stimulate the production of inflammatory cytokines and may act as a “depot” for these pro-inflammatory mediators.10
Clinical implications
Bacterial biofilms are likely a key modulator of the refractory nature of CRS. In 2006, Bendouah et al71 demonstrated that P. aeruginosa and S. aureus biofilms were associated with poor clinical improvement following surgical intervention. Prince et al42 showed that patients with recalcitrant CRS after FESS were more likely to harbor biofilm-forming bacteria. Psaltis et al72 demonstrated that CRS patients with bacterial biofilms had worse pre-operative imaging scores and, at a median of 8 months follow-up, these patients were more likely to have ongoing post-operative symptoms relative to patients without biofilms. A follow-up prospective trial confirmed these findings utilizing validated subjective and objective measures, and also showed that biofilm-positive patients had statistically worse sinus symptoms, and required extra post-operative visits and multiple antibiotic treatments.73 This conclusion requires further investigation as these results have been variably replicable in other studies.74
Recent studies have demonstrated that individual biofilm species are associated with disease phenotypes. Foreman and Wormald75 first showed that S. aureus biofilms are associated with severe, surgically recalcitrant disease in a small retrospective study. A later prospective, blinded study reinforced these findings.76 Those patients with S. aureus biofilms had worse objective symptom scores, worse nasal endoscopy scores, worse quality of life outcomes, and required more post-operative visits when compared to patients with other biofilms. These types of clinical findings have prompted the search for effective anti-biofilm therapies.
Treatment strategies
Biofilm eradication strategies are increasingly important due to the paucity of antimicrobials in development by the pharmaceutical industry, and the concurrent propagation of antimicrobial resistance. Therapeutic avenues for the elimination of biofilms include:
-
1)
Antimicrobial neutralization
-
2)
Dispersion of existing biofilms
-
3)
Disruption of quorum sensing
Antimicrobial neutralization
The extracellular matrix expressed by biofilms protects the bacteria within from host immune defense mechanisms and prevents entry of antimicrobial agents. Furthermore, within a biofilm, bacteria evolve reduced antibiotic susceptibility via heritable resistance mechanisms including adaptive mutations and horizontal gene transfer.77 Consequently, the eradication of biofilms using traditional antibiotics is challenging.
Interestingly the paucity of novel antibiotics has prompted further investigation of existing agents. Macrolides typically exert their antimicrobial effect through the inhibition of bacterial protein synthesis through reversible inhibition of the 50S bacterial ribosomal subunit. Macrolides have been shown to, potentially, harbor an anti-biofilm effect through their inhibition of the production of key molecules involved in quorum sensing.78, 79 Though the exact mechanism is unclear, it has been proposed that macrolides may indirectly interfere with an unidentified protein critical to the transcription of an autoinducer synthase.
Wallwork et al79 evaluated a prospective cohort of 64 CRS patients in a double-blind, randomized, placebo-controlled trial. Patients received either 12 weeks of roxithromycin therapy or placebo, and clinical outcomes were assessed by the Sinonasal Outcome Test-20 (SNOT-20) and a Likert-type scale. There was a statistically significant decrease in SNOT-20 by 0.4 points 12 weeks after therapy, and a 0.7-point drop in the patient response scale. No statistically significant decreases in patient response were noted after 12 weeks calling into question the long-term benefits of macrolide therapy. Critically, this type of study does delineate between benefits related to the direct antimicrobial action of macrolides versus the anti-biofilm effect, and does not account for the anti-inflammatory effect of macrolides in CRS.80, 81
The discrepancy between observed in vitro effects and clinically significant benefit in the context of macrolide usage is highlighted by a recent meta-analysis, which concluded that there was limited evidence to support the use of long-term macrolide therapy for CRS.82 Although the meta-analysis demonstrated a statistical benefit to long-term macrolide therapy, the less than 1 point changes in SNOT scores are less likely to be clinically significant.82 Further study will be necessary to determine whether the in vitro anti-biofilm effect of macrolides can be harnessed as either a monotherapy or, perhaps, in combination with other treatments to effect lasting clinical improvement in CRS patients.
Topical antibiotics have long been a subject of research focus due to their ability to deliver significantly higher doses of antibiotic to the sinonasal mucosal surface with limited systemic absorption. A study by Ha et al,83 in which strains of S. aureus susceptible to various agents were allowed to form biofilms in vitro were then subject to increased concentrations of topical antimicrobials, found that topical mupirocin could reduce S. aureus biofilm mass by more than 90%, while topical ciprofloxacin and vancomycin were both largely ineffective. In the clinical context, Jervis-Bardy et al84 demonstrated the short-term efficacy of mupirocin sinonasal rinses against S. aureus infection in surgically recalcitrant CRS in a randomized controlled clinical trial of 25 patients after FESS. Patients were randomized to one month of twice daily nasal saline rinses with 0.05% mupirocin or one month of twice daily nasal saline rinses with oral Augmentin. At one month, negative cultures were noted in 89% of patients in the mupirocin group compared to 0% in the placebo group. Mupirocin group patients were also found to have a statistically significant reduction in Lund–Kennedy endoscopic scores relative to the control arm. Interestingly, this microbiologic benefit did not translate into symptom score improvements relative to the pre-treatment baseline. Furthermore, re-assessment of the mupirocin treated cohort at 2–6 months post-treatment demonstrated that 83.3% of participants developed positive cultures for S. aureus with a return of Lund–Kennedy scores to baseline.84 The implication of this finding is that the observed clinical benefits of mupirocin therapy are, generally, short-lived. Indeed, subsequent studies demonstrate that mupirocin rinses have a microbiologic failure rate of 75% over time.
There have been efforts to develop novel non-antibiotic antimicrobial agents. One such example, N,N-dichloro-2,2-dimethyltaurine (NVC-422), is a synthetic and stable form of N,N-dichlorotaurine, a compound generated during the phagocytic antimicrobial oxidative burst. NVC-422 exerts a broad-spectrum effect with demonstrated efficacy against S. aureus, including methicillin-resistant strains, S. pneumoniae, Echerichia coli, Candida species, and viruses such as herpes simplex and adenovirus.85 Singhal et al85 report that there was no development of resistance against NVC-422 after serial passages of the targeted microbe. After establishment of S. aureus biofilms in the frontal sinuses of sheep, two sinus irrigations with NVC-422 induced a dose-dependent reduction in biomass relative to untreated control sinuses [(0.11 ± 0.11) μm3/μm2 in 0.5% NVC-422 compared to (2.01 ± 2.7) μm3/μm2 in control].85 There have been no further publications relating to this agent.
Manuka honey is a natural product of New Zealand whose main active ingredient, methylglyoxal (MGO), has a high phenol content which is known to be bactericidal. Manuka honey has demonstrated significant bactericidal effect against planktonic and biofilm forms of S. aureus and P. aeruginosa, eliminating 82% of methicillin-sensitive S. aureus, 63% of MRSA biofilms, and 91% of P. aeruginosa biofilms.86 Studies conducted in sheep models of CRS revealed statistically significant reductions in biofilm biomass compared to saline flushes at concentrations of 1.8 mg/mL MGO (0.676 ± 0.079) μm3/μm2 vs. (0.114 ± 0.033) μm3/μm2, P = 0.001 and 3.6 mg/mL (0.608 ± 0.101) μm3/μm2 vs. (0.141 ± 0.039) μm3/μm2, P = 0.001.87 Animals given MGO alone were noted to have more toxic effects, including severe sinus inflammation and metaplasia of respiratory epithelium, compared to animals treated with MGO in the presence of Manuka honey suggesting natural anti-inflammatory properties in other components of the honey.86, 87 Clinical trials investigating the efficacy of Manuka honey in patients with CRS are awaited.
Following the use of antibiotics, there is an observed decrease in the diversity of the sinus microbiome with increases in non-commensal pathologic species known to form biofilms. In order to replete the microbiome, researchers have investigated Lactobacillus species, which have been found to be in high concentrations on healthy mucosa and in low concentration after antibiotic use in the setting of CRS.88, 89 The presence of L. fermentum in cultures with S. aureus and P. aeruginosa led to a 40%–50% dispersion of biofilms and marked inhibition of bacterial growth rate. After inoculation of mammalian cells in vitro with S. aureus and P. aeruginosa, mucosal cell viability was shown to decrease by 50%–60%. In contrast, the presence of L. fermentum in addition to both pathogenic bacterial strains, increased mucosal cell viability by 80–95%. Early in vitro studies are promising suggesting that Lactobacillus species may inhibit the growth, cytotoxicity and biofilm formation of several S. aureus and P. aeruginosa strains.9, 90 In the clinical setting, Mukerji et al91 evaluated the use of probiotics as an adjunctive treatment for CRS. In this prospective, placebo-controlled trial, 77 patients were randomized to receive either oral probiotic L. rhamnosus or oral placebo treatment for 4 weeks. No significant difference in SNOT-20 scores was seen.
Antimicrobial photodynamic therapy (aPDT) is a novel non-antibiotic therapy that causes microbe destruction by causing perforation of cell membranes in the presence of photo reactive dyes. Activation of these compounds by laser light generates oxygen free radicals that disrupt the bacterial cell membrane, permitting the entry of dye into the cells where it can cause lethal cellular damage. This therapy showed promise in eradicating planktonic bacteria and significantly reduced biofilm biomass by over 99.9% in vitro.92 Biel et al93 examined aPDT's effect on biofilms in a plastic model of the human maxillary sinus cavity. Their experiments revealed a 5 log reduction in P. aeruginosa biofilms and a 3.1 log reduction in MRSA biofilms after a single treatment. An earlier study by the same group demonstrated that aPDT does not appear to damage cultured human respiratory epithelial cells.94 The clinical applicability of aPDT is under investigation.
Corticosteroids have been shown to enhance some functions of the mucosal innate immune system including increased production of complement and acute phase proteins.95 A recent study found that high concentrations of fluticasone (400 μg/200 μL), budesonide (750–2000 μg/200 μL) and mometasone (200–400 μg/200 μL) directly reduced biofilm biomass by up to 99% in vitro.96 This brings to light new mechanisms of action of intranasal steroids against biofilms and warrants further study.
Dispersion of existing biofilms
Another tactic for biofilm eradication is the use of surfactants to disrupt biofilm integrity. Chiu et al97 explored the use of baby shampoo as an anti-biofilm detergent. Eighteen patients who underwent FESS were instructed to irrigate their sinonasal cavities with 1% baby shampoo in saline for 4 weeks post-operatively. At 4 weeks, the authors observed a 46.6% improvement in patient SNOT-22 scores and a 63% improvement in olfaction with a significant decrease in mucus thickness and post-nasal drainage.97 However, 10% of patients reported intolerable side effects. Furthermore, although shampoo rinses inhibited biofilm growth, this therapy failed to eradicate biofilm.
A subsequent randomized controlled trial by Farag et al98 involved 44 patients with CRS randomized to receive post-FESS baby shampoo rinses or hypertonic saline rinses. Both treatment arms demonstrated similar improvements in symptoms and olfactory thresholds. However, 52% of the shampoo group had significant side effects with 20% of the cohort withdrawing from the study compared to only 5% of patients reporting side effects in the hypertonic saline group. Specifically, baby shampoo irrigations may cause headaches and nasal burning making use as a therapy less viable.98, 99
Citric acid/Zwitterionic surfactant (CAZS) is a novel surfactant consisting of citric acid, which chelates calcium in the calcium ion bridges integral to biofilm structural integrity. The zwitterionic surfactant is then able to detach the biofilm from the mucosal surface and force it into solution. Desrosiers et al100 demonstrated in vitro that CAZS was successful in reducing S. aureus and P. aeruginosa colony forming units. CAZS induced statistically significant reductions in S. aureus and P. aeruginosa biofilm biomass, which was similar to the reduction achieved through hydrodynamic delivery of saline (2.5 and 2.9 log reduction vs. 2.3 and 2.4 log reduction, respectively, P < 0.002). However, the greatest reduction in biofilms was observed with hydrodynamic delivery of CAZS (3.9 and 5.2 log reduction in S. aureus and P. aeruginosa biomass, respectively, P = 0.001).100 Of some concern, subsequent in vivo studies by Tamashiro et al101 showed CAZS to be toxic to cilia in a rabbit model, temporarily neutralizing mucociliary clearance. The investigators observed deciliation of 80%–85% 1–3 days after treatment with 96.25% recovery 6 days after stopping CAZS, leaving the sinuses more susceptible to infection in that time frame. SinuSurf, another detergent specifically developed for nasal use, showed dramatic anti-biofilm effects in vitro, but was taken off the market due to toxic effects.102 Thus far, despite a significant effect anti-biofilm effect, the benefits of detergent agents may be outweighed by toxicity.
Targeting enzymes and polysaccharides necessary for formation of biofilms represents a potential therapeutic strategy. Poly-N-acetylglucosamine (PNAG) is a polysaccharide produced by S. aureus that is critical to the formation of the biofilm matrix. This polysaccharide helps confer biofilm resistance to host immune peptides by forming a charge barrier preventing interaction with bacterial proteins. Dispersin B is an enzyme that degrades PNAG and may be used to target biofilms and disrupt their structure.103 Izano et al104 demonstrated both the inhibition of S. aureus biofilm formation and the detachment of preformed biofilms in vitro before and after treatment with Dispersin B.
Extracellular DNA functions to stabilize the biofilm matrix, transfer plasmids carrying resistance-conferring genes, and promote biofilm adhesion to surfaces. A novel bacterial deoxyribonuclease, NucB, produced by the marine bacterium Bacillus licheniformis, potentially degrades extracellular DNA.43 Inoculation of FESS-derived biofilm cultures with NucBinduced complete eradication of biofilms originating from nuclease-producing bacteria (S. aureus, S. anginosus group, S. lugdunensis, S. salivarius), and induced a 33% reduction in biofilms consisting of non-nuclease producing strains (Corynebacterium species, Moraxella catarrhalis). NucB was not effective against planktonic bacteria, exerting its effect exclusively on the biofilm forms. The role of NucB in eradicating CRS biofilms is under investigation.43, 105
Interruption of quorum sensing
One of the most novel anti-biofilm strategies involves the interruption of quorum sensing molecules secreted by bacteria. Lee et al106 identified the bitter taste receptor, T2R38, as a key stimulator of nitric oxide production, subsequently leading to activation of the innate immune response against biofilms. T2R38 is activated in response to AHL quorum-sensing molecules secreted by P. aeruginosa and other gram-negative bacteria. AHL inhibition leads to unstructured P. aeruginosa biofilms that are more susceptible to surfactants and antimicrobials. Genetic variations in T2R38 were linked to a decreased ability to clear and kill bacteria in the upper respiratory tract and were also correlated to an increased susceptibility to gram-negative sinonasal infections. Further studies have indicated T2R38 as a risk factor for CRS that necessitates FESS. Adappa et al107 compared genotypes of T2R38 in patients with CRS undergoing primary FESS (n = 70) to the general population (n = 347) and found a significantly higher frequency of the non-functional genotype in the patient cohort (χ2(2) = 6.526, P = 0.0383). Evaluation of T2R38 pathway agonists as an anti-biofilm therapy is anticipated.
In the context of Pseudomonas biofilms, macrolide antibiotics have been shown to reduce the expression of the las and rhl quorum sensing systems. Each system includes a gene for a transcriptional activator, lasR and rhlR, and a gene for an autoinducer synthase, lasI and rhlI, which are necessary for the production of autoinducer molecules.78 In one study, the expression of elastase and rhamnolipid – two extracellular virulence factors whose production is regulated by the las and rhl quorum sensing systems, respectively – were measured in the presence of azithromycin. Expression of these virulence factors negatively correlates with autoinducer levels in Pseudomonas. Azithromycin therapy induced an 80% reduction in lasI and a 50% decline in rhlI levels suggesting suppression of quorum sensing. It is unknown whether these interesting in vitro results will translate to an anti-biofilm effect in the complex biologic milieu of CRS patients.78
Recently, paraoxonases (PONs) have been shown to play an important role against biofilm formation.108 PONs are enzymes expressed by the liver and kidney with the ability to degrade lactones including AHL. In vitro, PONs inactivate AHL and decrease P. aeruginosa biofilm growth.109 In a new experimental model with Drosophila melanogaster, PON transgenic flies show increased survival following infection with P. aeruginosa and Serratia marcescens, both AHL sensing bacteria.110 This understanding of innate immunity as a defense against biofilms has become increasingly important and raises the possibility of modulating the innate immune system to better respond against biofilm.
Conclusion
CRS involves a complex interplay of infectious, inflammatory, and host factors. Biofilms are the preferred state of bacterial existence. Several novel therapies directed against biofilms are in use or in development. However, the efficacy of these agents and their potential integration into the armamentarium of strategies directed against CRS will largely be reliant on better establishing the role of biofilms in the pathogenesis of chronic rhinosinusitis. With this understanding, a focus of several ongoing studies around the world, treatment strategies tailored towards the specific causes of CRS in individual patients may be developed.
Edited by Jing Li
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Potera C. Forging a link between biofilms and disease. Science. 1999;283:1837–1839. doi: 10.1126/science.283.5409.1837. [DOI] [PubMed] [Google Scholar]
- 2.Donlan R.M., Costerton J.W. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev. 2002;15:167–193. doi: 10.1128/CMR.15.2.167-193.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Costerton J.W., Lewandowski Z., Caldwell D.E., Korber D.R., Lappin-Scott H.M. Microbial biofilms. Annu Rev Microbiol. 1995;49:711–745. doi: 10.1146/annurev.mi.49.100195.003431. [DOI] [PubMed] [Google Scholar]
- 4.Donne J., Dewilde S. The challenging world of biofilm physiology. Adv Microb Physiol. 2015;67:235–292. doi: 10.1016/bs.ampbs.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 5.Belas R. Biofilms, flagella, and mechanosensing of surfaces by bacteria. Trends Microbiol. 2014;22:517–527. doi: 10.1016/j.tim.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 6.Donlan R.M. Biofilms: microbial life on surfaces. Emerg Infect Dis. 2002;8:881–890. doi: 10.3201/eid0809.020063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boyd C.D., O'Toole G.A. Second messenger regulation of biofilm formation: breakthroughs in understanding c-di-GMP effector systems. Annu Rev Cell Dev Biol. 2012;28:439–462. doi: 10.1146/annurev-cellbio-101011-155705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Romeo T. When the party is over: a signal for dispersal of Pseudomonas aeruginosa biofilms. J Bacteriol. 2006;188:7325–7327. doi: 10.1128/JB.01317-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ramakrishnan Y., Shields R.C., Elbadawey M.R., Wilson J.A. Biofilms in chronic rhinosinusitis: what is new and where next? J Laryngol Otol. 2015;129:744–751. doi: 10.1017/S0022215115001620. [DOI] [PubMed] [Google Scholar]
- 10.ND A., J P. Biofilms in chronic rhinosinusitis. In: CC C., GA I., ME G., editors. Diseases of the Sinuses. Spring; New York: 2014. p. 110. [Google Scholar]
- 11.Galloway W.R., Hodgkinson J.T., Bowden S.D., Welch M., Spring D.R. Quorum sensing in Gram-negative bacteria: small-molecule modulation of AHL and AI-2 quorum sensing pathways. Chem Rev. 2011;111:28–67. doi: 10.1021/cr100109t. [DOI] [PubMed] [Google Scholar]
- 12.Parker C.T., Sperandio V. Cell-to-cell signalling during pathogenesis. Cell Microbiol. 2009;11:363–369. doi: 10.1111/j.1462-5822.2008.01272.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rezzonico F., Smits T.H., Duffy B. Detection of AI-2 receptors in genomes of Enterobacteriaceae suggests a role of type-2 quorum sensing in closed ecosystems. Sensors (Basel) 2012;12:6645–6665. doi: 10.3390/s120506645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kendall M.M., Rasko D.A., Sperandio V. Global effects of the cell-to-cell signaling molecules autoinducer-2, autoinducer-3, and epinephrine in a luxS mutant of enterohemorrhagic Escherichia coli. Infect Immun. 2007;75:4875–4884. doi: 10.1128/IAI.00550-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.RB R., M G. Quorum-sensing inhibitors as anti-pathogenic drugs. Int J Med Microbiol. 2006;296:149–161. doi: 10.1016/j.ijmm.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 16.Hennequin C., Aumeran C., Robin F., Traore O., Forestier C. Antibiotic resistance and plasmid transfer capacity in biofilm formed with a CTX-M-15-producing Klebsiella pneumoniae isolate. J Antimicrob Chemother. 2012;67:2123–2130. doi: 10.1093/jac/dks169. [DOI] [PubMed] [Google Scholar]
- 17.Jefferson K.K., Goldmann D.A., Pier G.B. Use of confocal microscopy to analyze the rate of vancomycin penetration through Staphylococcus aureus biofilms. Antimicrob Agents Chemother. 2005;49:2467–2473. doi: 10.1128/AAC.49.6.2467-2473.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singh R., Ray P., Das A., Sharma M. Penetration of antibiotics through Staphylococcus aureus and Staphylococcus epidermidis biofilms. J Antimicrob Chemother. 2010;65:1955–1958. doi: 10.1093/jac/dkq257. [DOI] [PubMed] [Google Scholar]
- 19.Cos P., Tote K., Horemans T., Maes L. Biofilms: an extra hurdle for effective antimicrobial therapy. Curr Pharm Des. 2010;16:2279–2295. doi: 10.2174/138161210791792868. [DOI] [PubMed] [Google Scholar]
- 20.Stewart P.S., Franklin M.J. Physiological heterogeneity in biofilms. Nat Rev Microbiol. 2008;6:199–210. doi: 10.1038/nrmicro1838. [DOI] [PubMed] [Google Scholar]
- 21.Murakami K., Ono T., Viducic D. Role for rpoS gene of Pseudomonas aeruginosa in antibiotic tolerance. FEMS Microbiol Lett. 2005;242:161–167. doi: 10.1016/j.femsle.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 22.Poole K. Bacterial stress responses as determinants of antimicrobial resistance. J Antimicrob Chemother. 2012;67:2069–2089. doi: 10.1093/jac/dks196. [DOI] [PubMed] [Google Scholar]
- 23.Lewis K. Persister cells, dormancy and infectious disease. Nat Rev Microbiol. 2007;5:48–56. doi: 10.1038/nrmicro1557. [DOI] [PubMed] [Google Scholar]
- 24.Dorr T., Lewis K., Vulic M. SOS response induces persistence to fluoroquinolones in Escherichia coli. PLoS Genet. 2009;5:e1000760. doi: 10.1371/journal.pgen.1000760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foreman A., Jervis-Bardy J., Wormald P.J. Do biofilms contribute to the initiation and recalcitrance of chronic rhinosinusitis? Laryngoscope. 2011;121:1085–1091. [Google Scholar]
- 26.Costerton J.W., Lewandowski Z., Caldwell D.E., Korber D.R., Lappin-Scott H.M. Mucosal biofilm formation on middle-ear mucosa in the chinchilla model of otitis media. JAMA. 2002;287:1710–1715. doi: 10.1001/jama.287.13.1710. [DOI] [PubMed] [Google Scholar]
- 27.Chole R.A., Faddis B.T. Evidence for microbial biofilms in cholesteatomas. Arch Otolaryngol Head Neck Surg. 2002;128:1129–1133. doi: 10.1001/archotol.128.10.1129. [DOI] [PubMed] [Google Scholar]
- 28.Chole R.A., Faddis B.T. Anatomical evidence of microbial biofilms in tonsillar tissues: a possible mechanism to explain chronicity. Arch Otolaryngol Head Neck Surg. 2003;129:634–636. doi: 10.1001/archotol.129.6.634. [DOI] [PubMed] [Google Scholar]
- 29.Parsek M.R., Singh P.K. Bacterial biofilms: an emerging link to disease pathogenesis. Annu Rev Microbiol. 2003;57:677–701. doi: 10.1146/annurev.micro.57.030502.090720. [DOI] [PubMed] [Google Scholar]
- 30.Hall-Stoodley L., Stoodley P., Kathju S. Towards diagnostic guidelines for biofilm-associated infections. FEMS Immunol Med Microbiol. 2012;65:127–145. doi: 10.1111/j.1574-695X.2012.00968.x. [DOI] [PubMed] [Google Scholar]
- 31.Cryer J., Schipor I., Perloff J.R., Palmer J.N. Evidence of bacterial biofilms in human chronic sinusitis. ORL J Otorhinolaryngol Relat Spec. 2004;66:155–158. doi: 10.1159/000079994. [DOI] [PubMed] [Google Scholar]
- 32.Sanclement J.A., Webster P., Thomas J., Ramadan H.H. Bacterial biofilms in surgical specimens of patients with chronic rhinosinusitis. Laryngoscope. 2005;115:578–582. doi: 10.1097/01.mlg.0000161346.30752.18. [DOI] [PubMed] [Google Scholar]
- 33.Perloff J.R., Palmer J.N. Evidence of bacterial biofilms on frontal recess stents in patients with chronic rhinosinusitis. Am J Rhinol. 2004;18:377–380. [PubMed] [Google Scholar]
- 34.Ramadan H.H., Sanclement J.A., Thomas J.G. Chronic rhinosinusitis and biofilms. Otolaryngol Head Neck Surg. 2005;132:414–417. doi: 10.1016/j.otohns.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 35.Sanderson A.R., Leid J.G., Hunsaker D. Bacterial biofilms on the sinus mucosa of human subjects with chronic rhinosinusitis. Laryngoscope. 2006;116:1121–1126. doi: 10.1097/01.mlg.0000221954.05467.54. [DOI] [PubMed] [Google Scholar]
- 36.Healy D.Y., Leid J.G., Sanderson A.R., Hunsaker D.H. Biofilms with fungi in chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2008;138:641–647. doi: 10.1016/j.otohns.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 37.Psaltis A.J., Ha K.R., Beule A.G., Tan L.W., Wormald P.J. Confocal scanning laser microscopy evidence of biofilms in patients with chronic rhinosinusitis. Laryngoscope. 2007;117:1302–1306. doi: 10.1097/MLG.0b013e31806009b0. [DOI] [PubMed] [Google Scholar]
- 38.Bezerra T.F., Padua F.G., Gebrim E.M., Saldiva P.H., Voegels R.L. Biofilms in chronic rhinosinusitis with nasal polyps. Otolaryngol Head Neck Surg. 2011;144:612–616. doi: 10.1177/0194599811399536. [DOI] [PubMed] [Google Scholar]
- 39.Foreman A., Boase S., Psaltis A., Wormald P.J. Role of bacterial and fungal biofilms in chronic rhinosinusitis. Curr Allergy Asthma Rep. 2012;12:127–135. doi: 10.1007/s11882-012-0246-7. [DOI] [PubMed] [Google Scholar]
- 40.Hochstim C.J., Masood R., Rice D.H. Biofilm and persistent inflammation in endoscopic sinus surgery. Otolaryngol Head Neck Surg. 2010;143:697–698. doi: 10.1016/j.otohns.2010.07.017. [DOI] [PubMed] [Google Scholar]
- 41.Hamilos D.L. Host-microbial interactions in patients with chronic rhinosinusitis. J Allergy Clin Immunol. 2013;131:1263–1264. doi: 10.1016/j.jaci.2013.02.020. 1264 e1261–1266. [DOI] [PubMed] [Google Scholar]
- 42.Prince A.A., Steiger J.D., Khalid A.N. Prevalence of biofilm-forming bacteria in chronic rhinosinusitis. Am J Rhinol. 2008;22:239–245. doi: 10.2500/ajr.2008.22.3180. [DOI] [PubMed] [Google Scholar]
- 43.Shields R.C., Mokhtar N., Ford M. Efficacy of a marine bacterial nuclease against biofilm forming microorganisms isolated from chronic rhinosinusitis. PloS One. 2013;8:e55339. doi: 10.1371/journal.pone.0055339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stressmann F.A., Rogers G.B., Chan S.W. Characterization of bacterial community diversity in chronic rhinosinusitis infections using novel culture-independent techniques. Am J Rhinol Allergy. 2011;25:e133–e140. doi: 10.2500/ajra.2011.25.3628. [DOI] [PubMed] [Google Scholar]
- 45.Stephenson M.F., Mfuna L., Dowd S.E. Molecular characterization of the polymicrobial flora in chronic rhinosinusitis. J Otolaryngol Head Neck Surg. 2010;39:182–187. [PubMed] [Google Scholar]
- 46.Foreman A., Singhal D., Psaltis A.J., Wormald P.J. Targeted imaging modality selection for bacterial biofilms in chronic rhinosinusitis. Laryngoscope. 2010;120:427–431. doi: 10.1002/lary.20705. [DOI] [PubMed] [Google Scholar]
- 47.Wilkins M., Hall-Stoodley L., Allan R.N., Faust S.N. New approaches to the treatment of biofilm-related infections. J Infect. 2014;69(suppl 1):S47–S52. doi: 10.1016/j.jinf.2014.07.014. [DOI] [PubMed] [Google Scholar]
- 48.Palmer R.J., Jr., Sternberg C. Modern microscopy in biofilm research: confocal microscopy and other approaches. Curr Opin Biotechnol. 1999;10:263–268. doi: 10.1016/S0958-1669(99)80046-9. [DOI] [PubMed] [Google Scholar]
- 49.Zernotti M.E., Angel Villegas N., Roques Revol M. Evidence of bacterial biofilms in nasal polyposis. J Investig Allergol Clin Immunol. 2010;20:380–385. [PubMed] [Google Scholar]
- 50.Katzenstein A.L., Sale S.R., Greenberger P.A. Allergic Aspergillus sinusitis: a newly recognized form of sinusitis. J Allergy Clin Immunol. 1983;72:89–93. doi: 10.1016/0091-6749(83)90057-x. [DOI] [PubMed] [Google Scholar]
- 51.Foreman A., Psaltis A.J., Tan L.W., Wormald P.J. Characterization of bacterial and fungal biofilms in chronic rhinosinusitis. Am J Rhinol Allergy. 2009;23:556–561. doi: 10.2500/ajra.2009.23.3413. [DOI] [PubMed] [Google Scholar]
- 52.Boase S., Valentine R., Singhal D., Tan L.W., Wormald P.J. A sheep model to investigate the role of fungal biofilms in sinusitis: fungal and bacterial synergy. Int Forum Allergy Rhinol. 2011;1:340–347. doi: 10.1002/alr.20066. [DOI] [PubMed] [Google Scholar]
- 53.Lynch A.S., Robertson G.T. Bacterial and fungal biofilm infections. Annu Rev Med. 2008;59:415–428. doi: 10.1146/annurev.med.59.110106.132000. [DOI] [PubMed] [Google Scholar]
- 54.Harriott M.M., Noverr M.C. Candida albicans and Staphylococcus aureus form polymicrobial biofilms: effects on antimicrobial resistance. Antimicrob Agents Chemother. 2009;53:3914–3922. doi: 10.1128/AAC.00657-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Morales D.K., Hogan D.A. Candida albicans interactions with bacteria in the context of human health and disease. PLoS Pathog. 2010;6:e1000886. doi: 10.1371/journal.ppat.1000886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ellington J.K., Harris M., Hudson M.C., Vishin S., Webb L.X., Sherertz R. Intracellular Staphylococcus aureus and antibiotic resistance: implications for treatment of staphylococcal osteomyelitis. J Orthop Res. 2006;24:87–93. doi: 10.1002/jor.20003. [DOI] [PubMed] [Google Scholar]
- 57.Garzoni C., Francois P., Huyghe A. A global view of Staphylococcus aureus whole genome expression upon internalization in human epithelial cells. BMC Genomics. 2007;8:171. doi: 10.1186/1471-2164-8-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wood A.J., Fraser J.D., Swift S., Patterson-Emanuelson E.A., Amirapu S., Douglas R.G. Intramucosal bacterial micro colonies exist in chronic rhinosinusitis without inducing a local immune response. Am J Rhinol Allergy. 2012;26:265–270. doi: 10.2500/ajra.2012.26.3779. [DOI] [PubMed] [Google Scholar]
- 59.Tan N.C., Foreman A., Jardeleza C., Douglas R., Vreugde S., Wormald P.J. Intracellular Staphylococcus aureus: the Trojan horse of recalcitrant chronic rhinosinusitis? Int Forum Allergy Rhinol. 2013;3:261–266. doi: 10.1002/alr.21154. [DOI] [PubMed] [Google Scholar]
- 60.Psaltis A.J., Wormald P.J., Ha K.R., Tan L.W. Reduced levels of lactoferrin in biofilm-associated chronic rhinosinusitis. Laryngoscope. 2008;118:895–901. doi: 10.1097/MLG.0b013e31816381d4. [DOI] [PubMed] [Google Scholar]
- 61.Tan L., Psaltis A., Baker L.M., McGuckin M., Rousseau K., Wormald P.J. Aberrant mucin glycoprotein patterns of chronic rhinosinusitis patients with bacterial biofilms. Am J Rhinol Allergy. 2010;24:319–324. doi: 10.2500/ajra.2010.24.3504. [DOI] [PubMed] [Google Scholar]
- 62.Lane A.P., Truong-Tran Q.A., Schleimer R.P. Altered expression of genes associated with innate immunity and inflammation in recalcitrant rhinosinusitis with polyps. Am J Rhinol. 2006;20:138–144. [PMC free article] [PubMed] [Google Scholar]
- 63.You H., Zhuge P., Li D., Shao L., Shi H., Du H. Factors affecting bacterial biofilm expression in chronic rhinosinusitis and the influences on prognosis. Am J Otolaryngol. 2011;32:583–590. doi: 10.1016/j.amjoto.2010.11.017. [DOI] [PubMed] [Google Scholar]
- 64.Galli J., Calo L., Ardito F. Damage to ciliated epithelium in chronic rhinosinusitis: what is the role of bacterial biofilms? Ann Otol Rhinol Laryngol. 2008;117:902–908. doi: 10.1177/000348940811701207. [DOI] [PubMed] [Google Scholar]
- 65.Dlugaszewska J., Leszczynska M., Lenkowski M., Tatarska A., Pastusiak T., Szyfter W. The pathophysiological role of bacterial biofilms in chronic sinusitis. Eur Arch Otorhinolaryngol. 2015:1–6. doi: 10.1007/s00405-015-3650-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Palmer J. Bacterial biofilms in chronic rhinosinusitis. Ann Otol Rhinol Laryngol Suppl. 2006;196:35–39. doi: 10.1177/00034894061150s906. [DOI] [PubMed] [Google Scholar]
- 67.Hekiert A.M., Kofonow J.M., Doghramji L. Biofilms correlate with TH1 inflammation in the sinonasal tissue of patients with chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2009;141:448–453. doi: 10.1016/j.otohns.2009.06.090. [DOI] [PubMed] [Google Scholar]
- 68.Foreman A., Holtappels G., Psaltis A.J. Adaptive immune responses in Staphylococcus aureus biofilm-associated chronic rhinosinusitis. Allergy. 2011;66:1449–1456. doi: 10.1111/j.1398-9995.2011.02678.x. [DOI] [PubMed] [Google Scholar]
- 69.Arjomandi H., Gilde J., Zhu S. Relationship of eosinophils and plasma cells to biofilm in chronic rhinosinusitis. Am J Rhinol Allergy. 2013;27:e85–e90. doi: 10.2500/ajra.2013.27.3917. [DOI] [PubMed] [Google Scholar]
- 70.Dong D., Yulin Z., Xiao W. Correlation between bacterial biofilms and osteitis in patients with chronic rhinosinusitis. Laryngoscope. 2014;124:1071–1077. doi: 10.1002/lary.24424. [DOI] [PubMed] [Google Scholar]
- 71.Bendouah Z., Barbeau J., Hamad W.A., Desrosiers M. Biofilm formation by Staphylococcus aureus and Pseudomonas aeruginosa is associated with an unfavorable evolution after surgery for chronic sinusitis and nasal polyposis. Otolaryngol Head Neck Surg. 2006;134:991–996. doi: 10.1016/j.otohns.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 72.Psaltis A.J., Weitzel E.K., Ha K.R., Wormald P.J. The effect of bacterial biofilms on post-sinus surgical outcomes. Am J Rhinol. 2008;22:1–6. doi: 10.2500/ajr.2008.22.3119. [DOI] [PubMed] [Google Scholar]
- 73.Singhal D., Psaltis A.J., Foreman A., Wormald P.J. The impact of biofilms on outcomes after endoscopic sinus surgery. Am J Rhinol Allergy. 2010;24:169–174. doi: 10.2500/ajra.2010.24.3462. [DOI] [PubMed] [Google Scholar]
- 74.Hai P.V., Lidstone C., Wallwork B. The effect of endoscopic sinus surgery on bacterial biofilms in chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2010;142:S27–S32. doi: 10.1016/j.otohns.2009.09.022. [DOI] [PubMed] [Google Scholar]
- 75.Foreman A., Wormald P.J. Different biofilms, different disease? A clinical outcomes study. Laryngoscope. 2010;120:1701–1706. doi: 10.1002/lary.21024. [DOI] [PubMed] [Google Scholar]
- 76.Singhal D., Foreman A., Jervis-Bardy J., Wormald P.J. Staphylococcus aureus biofilms: nemesis of endoscopic sinus surgery. Laryngoscope. 2011;121:1578–1583. doi: 10.1002/lary.21805. [DOI] [PubMed] [Google Scholar]
- 77.Suh J.D., Cohen N.A., Palmer J.N. Biofilms in chronic rhinosinusitis. Curr Opin Otolaryngol Head Neck Surg. 2010;18:27–31. doi: 10.1097/MOO.0b013e328334f670. [DOI] [PubMed] [Google Scholar]
- 78.Tateda K., Comte R., Pechere J.C., Kohler T., Yamaguchi K., Van Delden C. Azithromycin inhibits quorum sensing in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2001;45:1930–1933. doi: 10.1128/AAC.45.6.1930-1933.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wallwork B., Coman W., Mackay-Sim A., Greiff L., Cervin A. A double-blind, randomized, placebo-controlled trial of macrolide in the treatment of chronic rhinosinusitis. Laryngoscope. 2006;116:189–193. doi: 10.1097/01.mlg.0000191560.53555.08. [DOI] [PubMed] [Google Scholar]
- 80.Miyanohara T., Ushikai M., Matsune S., Ueno K., Katahira S., Kurono Y. Effects of clarithromycin on cultured human nasal epithelial cells and fibroblasts. Laryngoscope. 2000;110:126–131. doi: 10.1097/00005537-200001000-00023. [DOI] [PubMed] [Google Scholar]
- 81.Inamura K., Ohta N., Fukase S., Kasajima N., Aoyagi M. The effects of erythromycin on human peripheral neutrophil apoptosis. Rhinology. 2000;38:124–129. [PubMed] [Google Scholar]
- 82.Pynnonen M.A., Venkatraman G., Davis G.E. Macrolide therapy for chronic rhinosinusitis: a meta-analysis. Otolaryngol Head Neck Surg. 2013;148:366–373. doi: 10.1177/0194599812470427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ha K.R., Psaltis A.J., Butcher A.R., Wormald P.J., Tan L.W. In vitro activity of mupirocin on clinical isolates of Staphylococcus aureus and its potential implications in chronic rhinosinusitis. Laryngoscope. 2008;118:535–540. doi: 10.1097/MLG.0b013e31815bf2e3. [DOI] [PubMed] [Google Scholar]
- 84.Jervis-Bardy J., Boase S., Psaltis A., Foreman A., Wormald P.J. A randomized trial of mupirocin sinonasal rinses versus saline in surgically recalcitrant staphylococcal chronic rhinosinusitis. Laryngoscope. 2012;122:2148–2153. doi: 10.1002/lary.23486. [DOI] [PubMed] [Google Scholar]
- 85.Singhal D., Jekle A., Debabov D. Efficacy of NVC-422 against Staphylococcus aureus biofilms in a sheep biofilm model of sinusitis. Int Forum Allergy Rhinol. 2012;2:309–315. doi: 10.1002/alr.21038. [DOI] [PubMed] [Google Scholar]
- 86.Alandejani T., Marsan J., Ferris W., Slinger R., Chan F. Effectiveness of honey on Staphylococcus aureus and Pseudomonas aeruginosa biofilms. Otolaryngol Head Neck Surg. 2009;141:114–118. doi: 10.1016/j.otohns.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 87.Paramasivan S., Drilling A.J., Jardeleza C., Jervis-Bardy J., Vreugde S., Wormald P.J. Methylglyoxal-augmented Manuka honey as a topical anti-Staphylococcus aureus biofilm agent: safety and efficacy in an in vivo model. Int Forum Allergy Rhinol. 2014;4:187–195. doi: 10.1002/alr.21264. [DOI] [PubMed] [Google Scholar]
- 88.Liu C.M., Soldanova K., Nordstrom L. Medical therapy reduces microbiota diversity and evenness in surgically recalcitrant chronic rhinosinusitis. Int Forum Allergy Rhinol. 2013;3:775–781. doi: 10.1002/alr.21195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jain R., Douglas R. When and how should we treat biofilms in chronic sinusitis? Curr Opin Otolaryngol Head Neck Surg. 2014;22:16–21. doi: 10.1097/MOO.0000000000000010. [DOI] [PubMed] [Google Scholar]
- 90.Varma P., Nisha N., Dinesh K.R., Kumar A.V., Biswas R. Anti-infective properties of Lactobacillus fermentum against Staphylococcus aureus and Pseudomonas aeruginosa. J Mol Microbiol Biotechnol. 2011;20:137–143. doi: 10.1159/000328512. [DOI] [PubMed] [Google Scholar]
- 91.Mukerji S.S., Pynnonen M.A., Kim H.M., Singer A., Tabor M., Terrell J.E. Probiotics as adjunctive treatment for chronic rhinosinusitis: a randomized controlled trial. Otolaryngol Head Neck Surg. 2009;140:202–208. doi: 10.1016/j.otohns.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 92.Biel M.A., Sievert C., Usacheva M., Teichert M., Balcom J. Antimicrobial photodynamic therapy treatment of chronic recurrent sinusitis biofilms. Int Forum Allergy Rhinol. 2011;1:329–334. doi: 10.1002/alr.20089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Biel M.A., Pedigo L., Gibbs A., Loebel N. Photodynamic therapy of antibiotic-resistant biofilms in a maxillary sinus model. Int Forum Allergy Rhinol. 2013;3:468–473. doi: 10.1002/alr.21134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Biel M.A., Jones J.W., Pedigo L., Gibbs A., Loebel N. The effect of antimicrobial photodynamic therapy on human ciliated respiratory mucosa. Laryngoscope. 2012;122:2628–2631. doi: 10.1002/lary.23502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Schleimer R.P. Glucocorticoids suppress inflammation but spare innate immune responses in airway epithelium. Proc Am Thorac Soc. 2004;1:222–230. doi: 10.1513/pats.200402-018MS. [DOI] [PubMed] [Google Scholar]
- 96.Goggin R., Jardeleza C., Wormald P.J., Vreugde S. Corticosteroids directly reduce Staphylococcus aureus biofilm growth: an in vitro study. Laryngoscope. 2014;124:602–607. doi: 10.1002/lary.24322. [DOI] [PubMed] [Google Scholar]
- 97.Chiu A.G., Palmer J.N., Woodworth B.A. Baby shampoo nasal irrigations for the symptomatic post-functional endoscopic sinus surgery patient. Am J Rhinol. 2008;22:34–37. doi: 10.2500/ajr.2008.22.3122. [DOI] [PubMed] [Google Scholar]
- 98.Farag A.A., Deal A.M., McKinney K.A. Single-blind randomized controlled trial of surfactant vs hypertonic saline irrigation following endoscopic endonasal surgery. Int Forum Allergy Rhinol. 2013;3:276–280. doi: 10.1002/alr.21116. [DOI] [PubMed] [Google Scholar]
- 99.Isaacs S., Fakhri S., Luong A., Whited C., Citardi M.J. The effect of dilute baby shampoo on nasal mucociliary clearance in healthy subjects. Am J Rhinol Allergy. 2011;25:e27–e29. doi: 10.2500/ajra.2011.25.3583. [DOI] [PubMed] [Google Scholar]
- 100.Desrosiers M., Myntti M., James G. Methods for removing bacterial biofilms: in vitro study using clinical chronic rhinosinusitis specimens. Am J Rhinol. 2007;21:527–532. doi: 10.2500/ajr.2007.21.3069. [DOI] [PubMed] [Google Scholar]
- 101.Tamashiro E., Banks C.A., Chen B. In vivo effects of citric acid/zwitterionic surfactant cleansing solution on rabbit sinus mucosa. Am J Rhinol Allergy. 2009;23:597–601. doi: 10.2500/ajra.2009.23.3398. [DOI] [PubMed] [Google Scholar]
- 102.Kofonow J.M., Adappa N.D. In vitro antimicrobial activity of SinuSurf. ORL J Otorhinolaryngol Relat Spec. 2012;74:179–184. doi: 10.1159/000339585. [DOI] [PubMed] [Google Scholar]
- 103.Donelli G., Francolini I., Romoli D. Synergistic activity of dispersin B and cefamandole nafate in inhibition of staphylococcal biofilm growth on polyurethanes. Antimicrob Agents Chemother. 2007;51:2733–2740. doi: 10.1128/AAC.01249-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Izano E.A., Amarante M.A., Kher W.B., Kaplan J.B. Differential roles of poly-N-acetylglucosamine surface polysaccharide and extracellular DNA in Staphylococcus aureus and Staphylococcus epidermidis biofilms. Appl Environ Microbiol. 2008;74:470–476. doi: 10.1128/AEM.02073-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Shakir A., Elbadawey M.R., Shields R.C., Jakubovics N.S., Burgess J.G. Removal of biofilms from tracheoesophageal speech valves using a novel marine microbial deoxyribonuclease. Otolaryngol Head Neck Surg. 2012;147:509–514. doi: 10.1177/0194599812442867. [DOI] [PubMed] [Google Scholar]
- 106.Lee R.J., Xiong G., Kofonow J.M. T2R38 taste receptor polymorphisms underlie susceptibility to upper respiratory infection. J Clin Invest. 2012;122:4145–4159. doi: 10.1172/JCI64240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Adappa N.D., Zhang Z., Palmer J.N. The bitter taste receptor T2R38 is an independent risk factor for chronic rhinosinusitis requiring sinus surgery. Int Forum Allergy Rhinol. 2014;4:3–7. doi: 10.1002/alr.21253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Camps J., Pujol I., Ballester F., Joven J., Simo J.M. Paraoxonases as potential antibiofilm agents: their relationship with quorum-sensing signals in Gram-negative bacteria. Antimicrob Agents Chemother. 2011;55:1325–1331. doi: 10.1128/AAC.01502-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ozer E.A., Pezzulo A., Shih D.M. Human and murine paraoxonase 1 are host modulators of Pseudomonas aeruginosa quorum-sensing. FEMS Microbiol Lett. 2005;253:29–37. doi: 10.1016/j.femsle.2005.09.023. [DOI] [PubMed] [Google Scholar]
- 110.Estin M.L., Stoltz D.A., Zabner J. Paraoxonase 1, quorum sensing, and P. aeruginosa infection: a novel model. Adv Exp Med Biol. 2010;660:183–193. doi: 10.1007/978-1-60761-350-3_17. [DOI] [PubMed] [Google Scholar]