Abstract
A 57 year old gentleman with a history of non-ischemic cardiomyopathy and paroxysmal atrial fibrillation presented with worsening lower extremity edema and dyspnea on exertion. He had been compliant with his medications including rivaroxaban (Xarelto) for atrial fibrillation that he takes with the evening meal daily. His echocardiogram showed an ejection fraction of 10-15% and a new left ventricle (LV) apical thrombus. During his hospital stay, he developed right sided weakness. Magnetic Resonance Imaging showed a subacute infarct involving the left parietal lobe. The decision was made to discontinue rivaroxaban and initiate heparin infusion instead. Meanwhile, the patient’s neurological symptoms were closely monitored. The patient was then transitioned to warfarin. He was eventually transferred to the rehabilitation floor with minimal residual neurologic weakness. Left ventricular thrombus is an important complication in the setting of systolic dysfunction. The combination of blood stasis, endothelial injury and hypercoagulability, is a prerequisite for in-vivo thrombus formation. The slow onset of action and reversal, need for frequent monitoring, narrow therapeutic range, dietary restrictions, and multiple drug interactions limit the use of vitamin K antagonists. Direct-acting oral anticoagulants (DOACs) do not have these limitations and may also reduce the risk of hemorrhagic stroke. Our patient developed an LV thrombus while on uninterrupted DOAC therapy.
Keywords: Left ventricular thrombus, direct-acting oral anticoagulants, cardiomyopathy
Introduction
The diagnosis of left ventricular (LV) thrombus is often made in patients with reduced LV systolic function with regional or extensive akinesis or hypokinesis as seen following a myocardial infarction (MI) or with aneurysmal formation [1]. Embolic events occur in 10-40% of patients with LV thrombus and no anticoagulation [2]. Currently, vitamin K antagonist therapy remains the standard of care for the treatment of LV thrombus based on observational studies. Direct oral anticoagulants (DOACs) such as dabigatran, rivaroxaban, edoxaban and apixaban were found to be non-inferior or even superior compared to warfarin in the prevention of thromboembolism in patients with non-valvular atrial fibrillation [1]. However, the role of DOACs in the management of LV thrombus is not well studied and remains unclear.
Case report
We report a 57 year old gentleman with a history of non-ischemic cardiomyopathy, paroxysmal atrial fibrillation (PAF), hypertension and diabetes mellitus who presented to the emergency department complaining of worsening lower extremity edema and dyspnea on exertion for 3 days prior to admission. The patient had been compliant with his home medications including rivaroxaban (Xarelto) for PAF that he takes with the evening meal daily.
Physical examination on admission revealed tachycardia with otherwise stable vital signs. He had an irregularly irregular rhythm, 2/6 systolic murmur at the left lower sternal border, diffuse rales bilaterally on lung exam and 2+ pitting edema in his lower extremities. The remainder of his physical examination was essentially normal.
Pertinent laboratory data revealed a brain natriuretic peptide (BNP) of 14,500. His other laboratory results were unremarkable. Electrocardiogram demonstrated atrial fibrillation with a ventricular rate of 120 beats per minute. He subsequently had an echocardiogram that showed a severely reduced left ventricular systolic function with an estimated ejection fraction (EF) of 10-15% and moderate tricuspid regurgitation. In addition, he was found to have a new LV apical thrombus (Figure 1A, 1B) in comparison to a previous echocardiogram done a year earlier (Figure 2).
Figure 1.
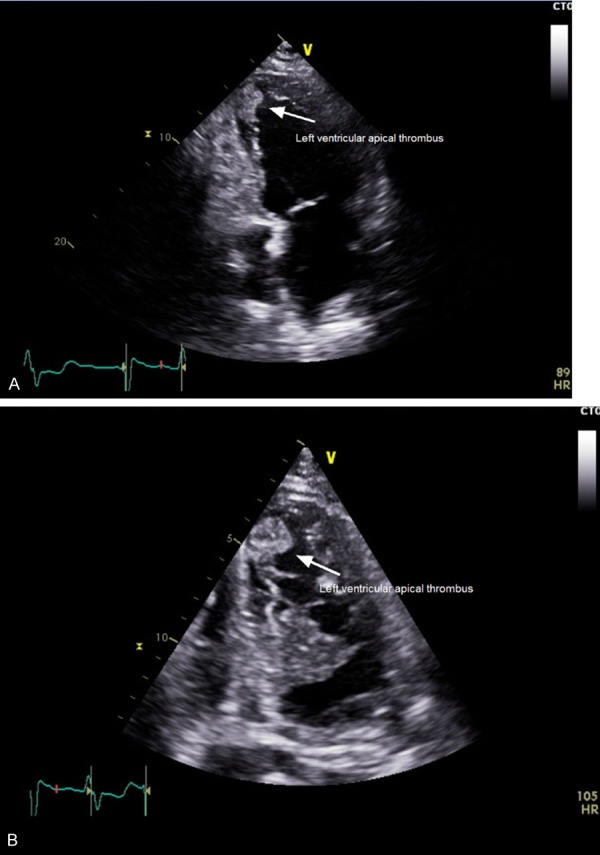
A. This is an apical view of the left atrium and left ventricle and the presence of a left ventricular thrombus in the apex. B. This is an enlarged apical view of the left ventricle again demonstrating the left ventricular apical thrombus. Due to the significant size of the thrombus, there was no need to confirm this finding with the use of contrast.
Figure 2.
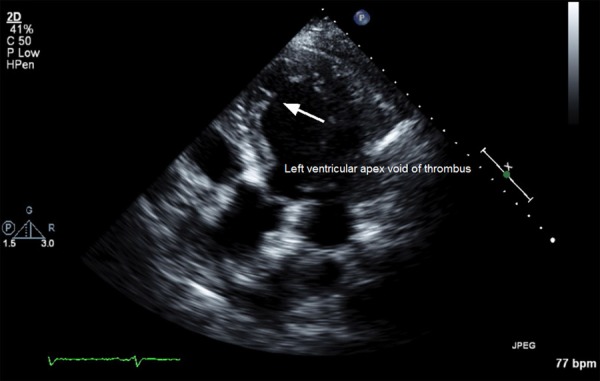
This demonstrates an echocardiogram apical view done one year prior to the discovery of the left ventricular thrombus. There was no evidence of a left ventricular apical thrombus at that time.
During his hospital stay, he developed mental status changes and right sided weakness. A Computed Tomography (CT) of the head did not demonstrate an acute intracranial process. Magnetic Resonance Imaging (MRI) and Magnetic Resonance Angiography (MRA) revealed a subacute nonhemorrhagic infarct involving the left parietal lobe. Due to the findings on MRI/MRA, the decision was made to discontinue Xarelto and initiate heparin infusion instead. This was due to the concern that anticoagulation with Xarelto may have not been adequate to prevent thromboembolism from LV thrombus. Meanwhile, the patient’s neurological symptoms were closely monitored.
The patient was then transitioned to warfarin with a target International Normalized Ratio (INR) of 2.0-3.0. He was eventually transferred to the rehabilitation floor and then discharged home with minimal residual neurologic weakness.
Discussion
Left ventricular thrombus is an important complication in the setting of systolic dysfunction. The combination of blood stasis, endothelial injury and hypercoagulability, often referred to as Virchow’s triad, is a prerequisite for in-vivo thrombus formation. Conditions that increase the risk of systemic embolization include: severe congestive heart failure, diffuse LV dilatation and systolic dysfunction, previous embolization, atrial fibrillation, and advanced patient age [3]. Rapid recognition and appropriate therapy are important because of the increased risk of systemic embolization, particularly cardioembolic stroke.
Transthoracic echocardiography (TTE) remains the most common imaging modality to make the diagnosis. When images are technically adequate, two-dimensional echocardiography provides excellent specificity (85-90%) and sensitivity (95%) in detecting LV thrombus in patients where the presence of thrombi was confirmed by surgery or autopsy. On TTE, LV thrombus is defined as a discrete echodense mass in the LV with defined margins that are distinct from the endocardium and seen throughout systole and diastole. It is almost always located adjacent to a hypokinetic or akinetic LV wall and seen from at least two views [4].
Observational studies conducted in the pre-thrombolytic and thrombolytic eras have provided support for the hypothesis that anticoagulation reduces the risk of embolization. Both current European Society of Cardiology and American College of Cardiology/American Heart Association guidelines recommend vitamin K antagonist therapy in patients with an LV thrombus after myocardial infarction. The role of DOACs in reducing thromboembolic risk in patients with LV thrombus still needs to be clarified [3].
The slow onset of action and reversal, need for frequent monitoring, narrow therapeutic range, dietary restrictions, and multiple drug interactions limit the use of vitamin K antagonists [5]. DOACs do not have these limitations and may also reduce the risk of hemorrhagic stroke. In the 2014 American Heart Association stroke guidelines, DOACs are recommended for three months in patients with LV mural thrombus intolerant to warfarin with a new class 2b recommendation and a level of evidence C [6].
Rivaroxaban, a selective inhibitor of active factor X, is currently indicated for the prevention of stroke and systemic embolism in patients with nonvalvular atrial fibrillation, and for the prevention and treatment of venous thromboembolism. Our understanding for the role of DOACs in LV thrombus is based on several case reports. In 2014, Padilla Perez et al. presented the first case of resolution of left ventricular thrombosis with rivaroxaban [7]. Erkan Yildirim et al. reported a case showing that an LV thrombus can be successfully treated by apixaban [1]. There are additional cases demonstrating similar findings. All the previous case reports share a common scenario where the diagnosis of an LV thrombus led to the utilization of DOACs for treatment. Our case differs since the development of an LV thrombus occurred while on uninterrupted DOAC therapy as we have ascertained the patient’s strict compliance with the treatment. Previous reports may have demonstrated success in the resolution of an LV thrombus with DOACs but they have yet to prove their potential in preventing the formation of a new LV thrombus with these agents.
Further studies are necessary in order to ascertain or refute the efficacy and safety of LV thrombus treatment with DOACs. Our case report also raises concerns as to whether DOACs can sufficiently prevent LV thrombus formation in the setting of a new cardiomyopathy. Although there are now several case reports in favor of the use of DOACs for LV thrombi, the success of DOACs in this setting may not be universal. It may be safer to continue the use of vitamin K antagonists only until more convincing knowledge is obtained from further studies.
Disclosure of conflict of interest
None.
References
- 1.Yildirim E, Kalkan K, Ipek E, Demirelli S, Ermiş E. Successful resolution of left ventricular thrombus with apixaban treatment. International Journal of the Cardiovascular Academy. 2016;2:57–58. [Google Scholar]
- 2.Cousin E, Scholfield M, Faber C, Caldeira C, Guglin M. Treatment options for patients with mobile left ventricular thrombus and ventricular dysfunction: a case series. Heart Lung Vessel. 2014;6:88–91. [PMC free article] [PubMed] [Google Scholar]
- 3.Delewi R, Zijlstra F, Piek JJ. Left ventricular thrombus formation after acute myocardial infarction. Heart. 2012;98:1743–1749. doi: 10.1136/heartjnl-2012-301962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Billingsley IM, Leiong-Poi H. Left ventricular thrombus: diagnosis, prevention, and management. Cardiology Rounds. 2005:10. [Google Scholar]
- 5.Savelieva I, Camm AJ. Practical considerations for using novel oral anticoagulants in patients with atrial fibrillation. Clin Cardiol. 2014;37:32–47. doi: 10.1002/clc.22204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, Fang MC, Fisher M, Furie KL, Heck DV, Johnston SC, Kasner SE, Kittner SJ, Mitchell PH, Rich MW, Richardson D, Schwamm LH, Wilson JA American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Peripheral Vascular Disease. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:2160–2236. doi: 10.1161/STR.0000000000000024. [DOI] [PubMed] [Google Scholar]
- 7.Padilla Pérez M, Salas Bravo D, Garcelán Trigo JA, Vazquez Ruiz de Castroviejo E, Torres Llergo J, Lozano Cabezas C, Fernández Guerrero JC. Resolution of left ventricular thrombus by Rivaroxaban. Future Cardiol. 2014;10:333–336. doi: 10.2217/fca.14.12. [DOI] [PubMed] [Google Scholar]


