Abstract
Background
We aimed to investigate the effect of automated external defibrillator (AED) feedback mechanisms on survival in out‐of‐hospital cardiac arrest (OHCA) victims. In addition, we investigated converting rates in patients with shockable rhythms according to AED shock waveforms and energy levels.
Methods
We collected data on OHCA occurring between 2011 and 2014 in the Capital Region of Denmark where an AED was applied prior to ambulance arrival. Patient data were obtained from the Danish Cardiac Arrest Registry and medical records. AED data were retrieved from the Emergency Medical Dispatch Centre (EMDC) and information on feedback mechanisms, energy waveform and energy level was downloaded from the applied AEDs.
Results
A total of 196 OHCAs had an AED applied prior to ambulance arrival; 62 of these (32%) provided audio visual (AV) feedback while no feedback was provided in 134 (68%). We found no difference in return of spontaneous circulation (ROSC) at hospital arrival according to AV‐feedback; 34 (55%, 95% confidence interval (CI) [13–67]) vs. 72 (54%, 95% CI [45–62]), P = 1 (odds ratio (OR) 1.1, 95% CI [0.6–1.9]) or 30‐day survival; 24 (39%, 95% CI [28–51]) vs. 53 (40%, 95% CI [32–49]), P = 0.88 (OR 1.1 (95% CI [0.6–2.0])). Moreover, we found no difference in converting rates among patients with initial shockable rhythm receiving one or more shocks according to AED energy waveform and energy level.
Conclusions
No difference in survival after OHCA according to AED feedback mechanisms, nor any difference in converting rates according to AED waveform or energy levels was detected.
Editorial comment.
In out of hospital cardiac arrest situations, automated external defibrillators in current use may have different functions. In this study, results from defibrillation were compared in a major city cohort, some with audio‐visual feedback from the defibrillator, and different biphasic waveforms and energies. No improvement in recovery or survival was noted in association with feedback or specific shock waveform.
Each year, around 275,000 suffers an OHCA in Europe and aggregated survival rates at hospital discharge is below 8%.1, 2, 3, 4 Many initiatives have been taken to improve survival, including efforts to strengthen and increase bystander cardiopulmonary resuscitation (CPR). The most recent European Resuscitation Council (ERC) guidelines emphasise the importance of the interaction between the emergency medical dispatcher, the bystander providing CPR, and early deployment of an AED.5 Early defibrillation with use of publicly accessible AEDs is associated with high survival rates,6, 7, 8, 9, 10 and registration of these AEDs into networks linked to EMDC may help to optimise timely deployment, thereby enhancing early defibrillation before arrival of the emergency medical services (EMS).11, 12, 13
Furthermore, ERC highlights the importance of CPR quality, including compression depth and frequency which is often found to be inadequate.14, 15, 16, 17 The use of AEDs providing feedback on CPR, either in the form of AV‐feedback with verbal prompts and visual indication of compression depth and frequency or a metronome, could be a useful strategy to improve CPR quality,18, 19 and is recommended by the Danish Health Authority and ERC.5, 20
While AED models alternate in electrical features encompassing shock waveform and shock energy levels, clinical effects of AED feedback mechanisms and electrical features are yet to be investigated.
In this study, we investigated the effect of AED feedback mechanisms on survival in OHCA victims, where an AED was applied prior to ambulance arrival. We primarily examined ROSC rates at hospital arrival according to AED feedback mechanism, as we hypothesised that the use of AEDs providing AV‐feedback on CPR quality would result in higher proportion of patients achieving ROSC. In addition, we sought to investigate converting rates in patients with shockable rhythms according to different shock waveforms and energy levels.
Methods
Study setting
The Capital Region of Denmark is one of five administrative regions in Denmark comprising approximately 2500 km2, including both urban and rural areas, with a population of 1.7 million. The region is covered by approximately 4000 AED's registered within The Danish AED online network (http://www.hjertestarter.dk/Service-Pages/InEnglish). The Network was established by the private foundation Trygfonden (trygfonden.dk) in 2007, and all AEDs are voluntarily registered with exact address, specific location and hours of accessibility. This information is available online and linked to the EMDC across the country, with the possibility of referring a bystander to the nearest available AED in the event of OHCA. The system is described in detail elsewhere.11
The EMS in the Capital Region of Denmark is a two‐tiered system comprising ambulances providing basic life support including defibrillation, and physician‐staffed mobile critical care units providing additional advanced life support. In the event of a cardiac arrest, both tiers of response are activated simultaneously. Data on each OHCA are systematically and prospectively recorded by the physician at scene in the prehospital medical record and maintained in a database at the EMDC in Copenhagen. In addition, EMS‐personnel are required to complete a short case‐report form for the Danish Cardiac Arrest Registry for every resuscitation‐attempted OHCA.
To conduct systematic follow‐up, all applied AEDs are brought to the EMDC in Copenhagen where electrocardiogram (ECG)‐data are retrieved. ECG data are sent to the receiving hospital and the AED is returned to the owner.21
AED models, electrical waveforms and energy levels
Reflecting the voluntariness of AED registration, The AED network covering the Capital Region of Denmark consists of approximately 27 different AED models with different designs and electrical features. Some AEDs provide AV‐feedback while others use a metronome to guide CPR or provide no feedback or guidance at all. Devices using AV‐feedback are designed differently according to type, but all AV‐feedback devices in this study included visual feedback on the display of the AED, indicating current compression depth and frequency whilst marking the ideal interval, and verbal prompts, encouraging and correcting the CPR provider while giving CPR. Moreover, some devices with AV‐feedback also provide a metronome.
Regarding AED shock waveforms, all models operate with biphasic waveforms, either Rectilinear Biphasic Waveform (RBW) or Biphasic Truncated Exponential (BTE) waveform that operate at different energy levels (Joule) according to recommendations and manufacturers.
Study population and data collection
In this observational study, we included patients in whom an AED was applied prior to ambulance arrival from 27 October 2011 through 26 October 2014.
All OHCA cases were included regardless of cause. Baseline data on OHCA were obtained from the prehospital medical records maintained by the EMDC, and from the Danish Cardiac Arrest Registry. These data included age, sex, public location, response time, bystander witness, bystander CPR, and if a shockable rhythm was present.
Data on ROSC outcome were acquired from The Danish Cardiac Arrest Registry; in case of missing information, medical records from the admitting hospital were reviewed to extract the information. Information on 30‐day survival was acquired from the Danish Civil Registration System22, which contains information on patients’ survival status. The reporting of OHCA cases was in accordance with the Utstein template.23
Information on first recorded heart rhythm, shocks and potential conversion was obtained by evaluation of ECG downloads from applied AEDs. Each ECG was analysed independently by two of the authors and subsequently compared. A third assessor reviewed the ECG in case of disagreement. Information on AED models was retrieved from the online AED network. A questionnaire was sent to AED manufactures acquiring data on feedback mechanisms, waveforms and energy levels according to model.
Ethics
According to Danish law, ethical approval is not required for registry‐based studies.
The study, and the processing of personal data, was approved by the Danish Health Authority (J. no. 7‐604‐04‐2/319/KWH) and the Danish Data Protection Agency (J. no. 30‐0616).
Statistics
Continuous variables are reported as medians with their associated inter quartile range [IQR] and a Mann‐Whitney U test was used for comparisons between groups. For categorical data, we report absolute numbers and proportions. Comparisons were done using Fisher's exact test. For all analyses, a two‐sided value of P < 0.05 was considered statistically significant.
Power calculation: we calculated that a sample of 190 OHCAs, assuming equal distribution of AV‐feedback mechanisms, would allow us to detect a difference in the proportion of ROSC upon hospital arrival between 40% and 60% with a statistical power of at least 80% at the 5% significance level. With unequal group sizes according to AV‐feedback in the ratio 1 : 2, a sample of 214 OHCAs was appropriate.
Statistical analyses were performed using the SAS Enterprise Guide statistical software package, version 6.1 (SAS Institute Inc., Cary, NC, USA).
Results
During the 3‐year study period, a total of 5821 OHCA patients in The Capital Region of Denmark, were registered in The Danish Cardiac Arrest Registry. Of these, 218 (3.7%) cases had an AED applied prior to ambulance arrival; 22 cases were excluded because no civil registration number was recorded. Hence, we included 196 OHCA cases for further analyses (Fig. 1). Overall, 3580 AEDs were registered within the Danish AED online network at the end of 2014. AED characteristics are shown in Table S1.
Figure 1.
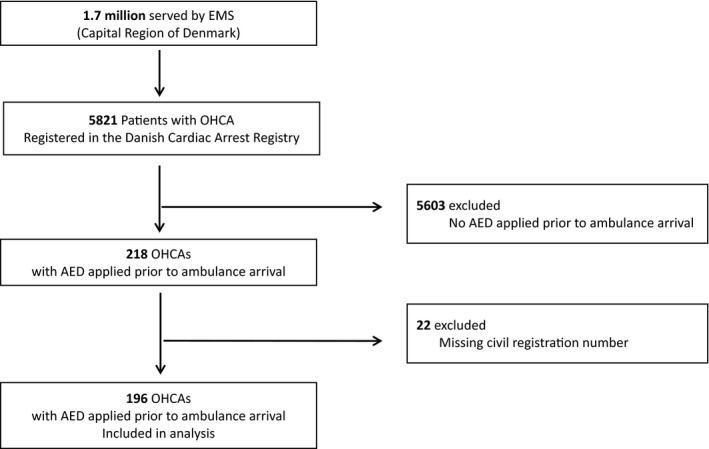
Patient flow, 27 October 2011 to 26 October 2014. EMS, Emergency Medical Services; OHCA, Out‐Of‐Hospital Cardiac Arrest; AED, Automated External Defibrillator.
Feedback mechanisms and outcome
In 62 (32%) cases, the applied AED provided AV‐feedback while no feedback was provided in 134 (68%) cases. In the latter group, an AED with a metronome was used in 77 cases. There was no difference in Utstein core elements between groups (Table 1).
Table 1.
Out‐of‐hospital cardiac arrest patients with an AED applied prior to ambulance arrival
| AEDs with AV‐feedback (n = 62)a | AEDs without AV‐feedback (n = 134)a | P value | |
|---|---|---|---|
| Age, median (IQR), years | 66 (49–76) | 69 (58–81) | 0.10 |
| Men, n (%) | 41 (66.1) | 87 (64.9) | 1 |
| Public Location, n (%)b | 37 (80.4) | 80 (86.9) | 0.32 |
| Response Time, median (IQR), minc | 6 (5–8) | 7 (5–9) | 0.39 |
| Bystander Witnessed, n (%) | 39 (73.6) | 73 (72.3) | 1 |
| Bystander CPR, n (%) | 53 (100) | 95 (94.1) | 0.09 |
| Shockable Rhythm, n (%)d | 30 (48.4) | 64 (47.8) | 1 |
Number of patients with missing value for the cardiac arrest‐related variables: ‘Bystander Witnessed’, ‘Bystander CPR’ and ‘Public Location’: n = 9, n = 9, and n = 33, respectively.
Public Location defined as all areas accessible to the general public all hours all day.
Interval between call to the EMS and ambulance arrival.
First recorded rhythm.
AED, Automated External Defibrillator; AV, Audio Visual; IQR, Inter Quartile Range; CPR, Cardiopulmonary Resuscitation.
Overall, ROSC upon hospital arrival was achieved in 106 (54%, 95% CI [47–61]) and 30‐day survival in 77 (40%, 95% CI [33–47]).
When the AED provided AV‐feedback, ROSC upon hospital arrival was achieved in 34 (55%, 95% CI [13–67]) cases and if no feedback was provided, ROSC was achieved in 72 (54%, 95% CI [45–62]) cases, P = 1 (OR 1.1, 95% CI [0.6–1.9]). Moreover, we found no difference in 30‐day survival according to AV‐feedback. Accordingly, 30‐day survival rates were 24 (39%, 95% CI [28–51]) with AV‐feedback and 53 (40%, 95% CI [32–49]) without AV‐feedback, P = 0.88 (OR 1.1 (95% CI [0.6–2.0])) (Table 2).
Table 2.
Outcome in out‐of‐hospital cardiac arrest patients with an AED applied prior to ambulance
| AEDs with Audio‐Visual feedback | AEDs without Audio‐Visual feedback | P value | |
|---|---|---|---|
| ROSC at Hospital Admission, n (%) | |||
| All Rhythm (n = 62 vs. n = 134)a | 34 (55%, 95% CI [43–67]) | 72 (54%, 95% CI [45–62]) | 1 |
| Shockable Rhythm (n = 30 vs. n = 64)b | 24 (80%, 95% CI [62–91]) | 50 (78%, 95% CI [67–87]) | 1 |
| Non‐Shockable Rhythm (n = 31 vs. n = 71)c | 10 (31%, 95% CI [18–49]) | 22 (31%, 95% CI [22–43]) | 1 |
| 30‐day Survival, n (%) | |||
| All Rhythm (n = 62 vs. n = 132)a , d | 24 (39%, 95% CI [28–51]) | 53 (40%, 95% CI [32–49]) | 0.88 |
| Shockable Rhythm (n = 30 vs. n = 62)b , d | 20 (67%, 95% CI [49–81]) | 41 (66%, 95% CI [54–77]) | 1 |
| Non‐Shockable Rhythm (n = 31 vs. n = 71)c | 4 (13%, 95% CI [12–58]) | 12 (17%, 95% CI [10–30]) | 0.77 |
All Rhythm: ventricular fibrillation, pulseless ventricular tachycardia, asystole or pulseless electrical activity.
Shockable Rhythm: ventricular fibrillation or pulseless ventricular tachycardia.
Non‐Shockable Rhythm: asystole or pulseless electrical activity.
Two patients with missing Civil Registration Number.
AED, Automated External Defibrillator; AV, Audio Visual; ROSC, Return Of Spontaneous Circulation.
Also, when comparing AEDs providing metronome with AEDs without any feedback or metronome, we found no significant difference in ROSC or 30‐day survival; 43 (56%, 95% CI [44–67]) vs. 29 (51%, 95% CI [37–64]), P = 0.6 and 31 (41%, 95% CI [30–53]) vs. 22 (39%, 95% CI [27–53]), P = 1.
Shock waveforms, energy levels and converting rates
Initial shockable rhythm was detected in 94 (49%) OHCA cases and one or more shocks were delivered by the applied AED in 85 cases. In these cases, 54 (64%) AEDs used biphasic truncated exponential waveform and 31 (36%) used rectilinear biphasic waveform.
In patients where a biphasic truncated exponential waveform was used, 37 (69%, 95% CI [54–80]) obtained sinus rhythm compared with 22 (71%, 95% CI [52–86]) cases where a rectilinear biphasic waveform was used, (OR 0.9, 95% CI [0.3–2.3], P = 1) (Table 3).
Table 3.
Conversion rate in out‐of‐hospital cardiac arrest patients with initial shockable rhythm, receiving one or more shocks, according to AED shock waveforms
| Biphasic truncated exponential (n = 54) | Rectiliniear biphasic (n = 31) | P value | |
|---|---|---|---|
| Converted, n (%) | 37 (69%, 95% CI [54–80]) | 22 (71%, 95% CI [52–86]) | 1 |
Before conversion to a rhythm resembling sinus rhythm, 42 (71%) OHCA patients with an initial shockable rhythm were shocked one time, 11 (18.6%) patients two times, two (3.4%) patients three times, one (1.7%) patient four times and two (3.4%) patients were shocked five times respectively. In 57 (67%) cases, first shock was delivered with an energy level of 150 J or less, 19 (22%) used energy level above 150 J, and nine (11%) used impedance specific energy level. We found no significant difference in converting rates according to AED energy level, (Table 4).
Table 4.
Conversion‐rate in out‐of‐hospital cardiac arrest patients with initial shockable rhythm, receiving one or more shocks, according to AED shock energy level
| Energy level ≤ 150 J (n = 57) | Energy level > 150 J (n = 19) | Energy level impedance specific (n = 9) | P value | |
|---|---|---|---|---|
| Converted, n (%) | 38 (67%, 95% CI [53–79]) | 14 (74%, 95% CI [49–91]) | 7 (78%, 95% CI [40–97]) | 0.8 |
Discussion
The main finding of this study was that there was no difference in ROSC upon hospital arrival for OHCA patients in whom an AED with AV‐feedback was used compared with patients in whom an AED without AV‐feedback was used. Moreover, we found no difference in ROSC or 30‐day survival rates when comparing AEDs providing metronome with AEDs without any feedback mechanisms, and there were no differences in converting rates according to AED shock waveforms or energy levels.
A strength of this study is the study design, which allowed us to study OHCA in real‐life settings with evaluation of survival outcome measures (ROSC and 30‐day survival) according to bystanders use of AEDs with or without AV‐feedback. Most other investigations on AED AV‐feedback are mannequin studies focusing on surrogate measures, such as compression depth and frequency.24, 25
However, several limitations should be considered when interpreting our results. First, we assessed outcomes according to AED feedback mechanisms in The Capital Region of Denmark, a rather densely populated region with a relatively high number of OHCAs occurring in public locations, which might not be generalisable to either the rest of Denmark nor other countries or communities with other geographic characteristics, Public Access Defibrillation (PAD)‐programme structures and legislation.
We describe AED use in cardiac arrests occurring primarily in public places which might not be generalisable, as 70% of cardiac arrest occur in residential areas.26, 27 Cardiac arrests occurring in public might be more likely to be witnessed by persons who are trained in CPR and use of AED.
Second, our data do not provide any information on whether the bystander using the AED was trained in CPR or not. This aspect would have been interesting as it has been demonstrated in a systematic review conducted by Yeung et al.18 that AV‐feedback might improve CPR skill acquisition during training. Moreover, Sainio et al.28, demonstrated a significantly higher rate of ROSC at hospital admission when an AED providing AV‐feedback was used, but AEDs were applied by physicians who could decide to activate the feedback mechanism or not. One possible drawback of AV‐feedback could be that voice prompts and visual indicators add noise and may distract the CPR provider, thereby prolonging time to defibrillation. Capucci et al.29 recently reported a beneficial effect on survival when laymen applied an AED in OHCA without performing any other CPR, thereby shortening time to first shock. Considering our results, it can be discussed whether the AV‐feedback can be omitted to avoid disturbing elements for CPR providers who are not professionals as the key issues are rapid CPR and defibrillation if the rhythm is shockable. In our study, we find no measurable impact on survival in favour of AV‐feedback, but further studies are needed to determine if these devices improve patient outcomes when applied in patients with cardiac arrest. Thirdly, we were only able to include OHCA patients where the AED data were downloaded and an AED is only applied in approximately 2–4% of all OHCAs.12, 26, 30 AEDs may have been applied without ECG data being retrieved if the AED was not brought to the EMDC after OHCA. Importantly, we did not find any difference in ROSC according to AV‐feedback, but we might have overlooked a clinically relevant difference as seen by the somewhat wide 95% CIs.
Overall ROSC and 30‐day survival was 54% and 40%, respectively, which is in accordance with previous studies reporting on bystander CPR and patients with shockable rhythm.12, 31, 32, 33, 34, 35 Unfortunately, an AED was only applied in 3.7% of all OHCAs. The survival benefit from use of AEDs by laymen prior to ambulance arrival in the context of low application rates enhances the importance of developing, implementing and optimising PAD programs.
In terms of AED models providing different shock waveforms, only few studies have been conducted with no evidence supporting on type of biphasic waveform instead of the other,36, 37, 38, 39 which is also supported by this study. Concerning AED energy levels ERC recommendations state that the initial biphasic shock energy should be at least 150 J for all waveforms. We found no difference in converting rates according to initial shock energy below or above 150 J, but our study was not powered to detect such a difference and further studies are needed.
Conclusion
In OHCA patients with an AED applied prior to ambulance arrival, we found no difference in survival according to AV‐feedback. In addition, we found no difference in converting rate in patients with initial shockable rhythm according to waveform and energy level.
Supporting information
Table S1. AED models registered within the Danish automated external defibrillator online network in The Capital Region of Denmark ultimo 2014.
Acknowledgements
Special thanks to Martin Fjordholdt for helping with data acquisition.
Agerskov M, Hansen MB, Nielsen AM, Møller TP, Wissenberg M, Rasmussen LS. Return of spontaneous circulation and long‐term survival according to feedback provided by automated external defibrillators. Acta Anaesthesiologica Scandinavica 2017.
Conflict of interest
No conflicts reported.
Funding
Lars Rasmussen and Anne Møller Nielsen have received grants from TrygFonden. TrygFonden has not taken any part in designing the study, analysing the data or any decision‐making regarding the manuscript.
References
- 1. Berdowski J, Berg RA, Tijssen JGP, Koster RW. Global incidences of out‐of‐hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation 2010; 81: 1479–87. [DOI] [PubMed] [Google Scholar]
- 2. Atwood C, Eisenberg MS, Herlitz J, Rea TD. Incidence of EMS‐treated out‐of‐hospital cardiac arrest in Europe. Resuscitation 2005; 67: 75–80. [DOI] [PubMed] [Google Scholar]
- 3. Gräsner JT, Herlitz J, Koster RW, Rosell‐Ortiz F, Stamatakis L, Bossaert L. Quality management in resuscitation–towards a European cardiac arrest registry (EuReCa). Resuscitation 2011; 82: 989–94. [DOI] [PubMed] [Google Scholar]
- 4. Gräsner J‐T, Bossaert L. Epidemiology and management of cardiac arrest: what registries are revealing. Best Pract Res Clin Anaesthesiol 2013; 27: 293–306. [DOI] [PubMed] [Google Scholar]
- 5. Perkins GD, Handley AJ, Koster RW, Castrén M, Smyth MA, Olasveengen T, Monsieurs KG, Raffay V, Gräsner J‐T, Wenzel V, Ristagno G, Soar J. Adult basic life support and automated external defibrillation section Collaborators. European Resuscitation Council Guidelines for Resuscitation 2015: Section 2. Adult basic life support and automated external defibrillation. Resuscitation 2015; 95: 81–99. [DOI] [PubMed] [Google Scholar]
- 6. Blom MT, Beesems SG, Homma PCM, Zijlstra JA, Hulleman M, van Hoeijen DA, Bardai A, Tijssen JGP, Tan HL, Koster RW. Improved survival after out‐of‐hospital cardiac arrest and use of automated external defibrillators. Circulation 2014; 130: 1868–75. [DOI] [PubMed] [Google Scholar]
- 7. Berdowski J, Blom MT, Bardai A, Tan HL, Tijssen JGP, Koster RW. Impact of onsite or dispatched automated external defibrillator use on survival after out‐of‐hospital cardiac arrest. Circulation 2011; 124: 2225–32. [DOI] [PubMed] [Google Scholar]
- 8. Valenzuela T, Roe D, Nichol G, Clark L, Spaite D, Hardman R. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med 2000; 343: 1206–9. [DOI] [PubMed] [Google Scholar]
- 9. Nielsen AM, Folke F, Lippert FK, Rasmussen LS. Use and benefits of public access defibrillation in a nation‐wide network. Resuscitation 2013; 84: 430–4. [DOI] [PubMed] [Google Scholar]
- 10. Ringh M, Fredman D, Nordberg P, Stark T, Hollenberg J. Mobile phone technology identifies and recruits trained citizens to perform CPR on out‐of‐hospital cardiac arrest victims prior to ambulance arrival. Resuscitation 2011; 82: 1514–8. [DOI] [PubMed] [Google Scholar]
- 11. Hansen CM, Lippert FK, Wissenberg M, Weeke P, Zinckernagel L, Ruwald MH, Karlsson L, Gislason GH, Nielsen SL, Køber L, Torp‐Pedersen C, Folke F. Temporal trends in coverage of historical cardiac arrests using a volunteer‐based network of automated external defibrillators accessible to laypersons and emergency dispatch centers. Circulation 2014; 130: 1859–67. [DOI] [PubMed] [Google Scholar]
- 12. Agerskov M, Nielsen AM, Hansen CM, Hansen MB, Lippert FK, Wissenberg M, Folke F, Rasmussen LS. Public Access Defibrillation: great benefit and potential but infrequently used. Resuscitation 2015; 96: 53–8. [DOI] [PubMed] [Google Scholar]
- 13. Nielsen AM, Rasmussen LS. Data management in automated external defibrillators: a call for a standardised solution. Acta Anaesthesiol Scand 2011; 55: 708–12. [DOI] [PubMed] [Google Scholar]
- 14. Abella BS, Alvarado JP, Myklebust H, Edelson DP, Barry A, O'Hearn N, Vanden Hoek TL, Becker LB. Quality of cardiopulmonary resuscitation during in‐hospital cardiac arrest. JAMA 2005; 293: 305–10. [DOI] [PubMed] [Google Scholar]
- 15. Wik L, Kramer‐Johansen J, Myklebust H, Sørebø H, Svensson L, Fellows B, Steen PA. Quality of cardiopulmonary resuscitation during out‐of‐hospital cardiac arrest. JAMA 2005; 293: 299–304. [DOI] [PubMed] [Google Scholar]
- 16. Van Hoeyweghen RJ, Bossaert LL, Mullie A, Calle P, Martens P, Buylaert WA, Delooz H. Quality and efficiency of bystander CPR. Belgian Cerebral Resuscitation Study Group. Resuscitation 1993; 26: 47–52. [DOI] [PubMed] [Google Scholar]
- 17. Valenzuela TD, Kern KB, Clark LL, Berg RA, Berg MD, Berg DD, Hilwig RW, Otto CW, Newburn D, Ewy GA. Interruptions of chest compressions during emergency medical systems resuscitation. Circulation 2005; 112: 1259–65. [DOI] [PubMed] [Google Scholar]
- 18. Yeung J, Meeks R, Edelson D, Gao F, Soar J, Perkins GD. The use of CPR feedback/prompt devices during training and CPR performance: a systematic review. Resuscitation 2009; 80: 743–51. [DOI] [PubMed] [Google Scholar]
- 19. Kirkbright S, Finn J, Tohira H, Bremner A, Jacobs I, Celenza A. Audiovisual feedback device use by health care professionals during CPR: a systematic review and meta‐analysis of randomised and non‐randomised trials. Resuscitation 2014; 85: 460–71. [DOI] [PubMed] [Google Scholar]
- 20. Dansk Hjertestopregister . Årsrapport 2005. Hjertestopbehandling udenfor hospital i Danmark. Available at: https://www.sundhed.dk/content/cms/67/1867_aarsrapport-2005-hjertestopregister.pdf (accessed 5 January 2017).
- 21. Hansen MB, Lippert FK, Rasmussen LS, Nielsen AM. Systematic downloading and analysis of data from automated external defibrillators used in out‐of‐hospital cardiac arrest. Resuscitation 2014; 85: 1681–5. [DOI] [PubMed] [Google Scholar]
- 22. Pedersen CB. The danish civil registration system. Scand J Public Health 2011; 39: 22–5. [DOI] [PubMed] [Google Scholar]
- 23. Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D, Bossaert LL, Brett SJ, Chamberlain D, de Caen AR, Deakin CD, Finn JC, Gräsner J‐T, Hazinski MF, Iwami T, Koster RW, Lim SH, Ma MH‐M, McNally BF, Morley PT, Morrison LJ, Monsieurs KG, Montgomery W, Nichol G, Okada K, Ong MEH, Travers AH, Nolan JP. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out‐of‐hospital cardiac arrest. Resuscitation 2015;96:328–40. [DOI] [PubMed] [Google Scholar]
- 24. Peberdy MA, Silver A, Ornato JP. Effect of caregiver gender, age, and feedback prompts on chest compression rate and depth. Resuscitation 2009; 80: 1169–74. [DOI] [PubMed] [Google Scholar]
- 25. Fischer H, Gruber J, Neuhold S, Frantal S, Hochbrugger E, Herkner H, Schöchl H, Steinlechner B, Greif R. Effects and limitations of an AED with audiovisual feedback for cardiopulmonary resuscitation: a randomized manikin study. Resuscitation 2011; 82: 902–7. [DOI] [PubMed] [Google Scholar]
- 26. Wissenberg M, Lippert FK, Folke F, Weeke P, Hansen CM, Christensen EF, Jans H, Hansen PA, Lang‐Jensen T, Olesen JB, Lindhardsen J, Fosbol EL, Nielsen SL, Gislason GH, Kober L, Torp‐Pedersen C. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out‐of‐hospital cardiac arrest. JAMA 2013; 310: 1377–84. [DOI] [PubMed] [Google Scholar]
- 27. Folke F, Gislason GH, Lippert FK, Nielsen SL, Weeke P, Hansen ML, Fosbøl EL, Andersen SS, Rasmussen S, Schramm TK, Køber L, Torp‐Pedersen C. Differences between out‐of‐hospital cardiac arrest in residential and public locations and implications for public‐access defibrillation. Circulation 2010; 122: 623–30. [DOI] [PubMed] [Google Scholar]
- 28. Sainio M, Kämäräinen A, Huhtala H, Aaltonen P, Tenhunen J, Olkkola KT, Hoppu S. Real‐time audiovisual feedback system in a physician‐staffed helicopter emergency medical service in Finland: the quality results and barriers to implementation. Scand J Trauma Resusc Emerg Med 2013; 1: 21–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Capucci A, Aschieri D, Guerra F, Pelizzoni V, Nani S, Villani GQ, Bardy GH. Community‐based automated external defibrillator only resuscitation for out‐of‐hospital cardiac arrest patients. Am Heart J 2016; 172: 192–200. [DOI] [PubMed] [Google Scholar]
- 30. Rea T, Blackwood J, Damon S, Phelps R, Eisenberg M. A link between emergency dispatch and public access AEDs: potential implications for early defibrillation. Resuscitation 2011; 82: 995–8. [DOI] [PubMed] [Google Scholar]
- 31. Kitamura T, Iwami T, Kawamura T, Nagao K, Tanaka H, Hiraide A. Nationwide public‐access defibrillation in Japan. N Engl J Med 2010; 362: 994–1004. [DOI] [PubMed] [Google Scholar]
- 32. Caffrey SL, Willoughby PJ, Pepe PE, Becker LB. Public use of automated external defibrillators. N Engl J Med 2002; 347: 1242–7. [DOI] [PubMed] [Google Scholar]
- 33. Sasaki M, Iwami T, Kitamura T, Nomoto S, Nishiyama C, Sakai T, Tanigawa K, Kajino K, Irisawa T, Nishiuchi T, Hayashida S, Hiraide A, Kawamura T. Incidence and outcome of out‐of‐hospital cardiac arrest with public‐access defibrillation. A descriptive epidemiological study in a large urban community. Circ J 2011; 75: 2821–6. [DOI] [PubMed] [Google Scholar]
- 34. Steinmetz J, Barnung S, Nielsen SL, Risom M, Rasmussen LS. Improved survival after an out‐of‐hospital cardiac arrest using new guidelines. Acta Anaesthesiol Scand 2008; 52: 908–13. [DOI] [PubMed] [Google Scholar]
- 35. Reinikainen M, Oksanen T, Leppänen P, Torppa T, Niskanen M, Kurola J. Finnish Intensive Care Consortium. Mortality in out‐of‐hospital cardiac arrest patients has decreased in the era of therapeutic hypothermia. Acta Anaesthesiol Scand 2012; 56: 110–5. [DOI] [PubMed] [Google Scholar]
- 36. van Alem AP, Chapman FW, Lank P, Hart AAM, Koster RW. A prospective, randomised and blinded comparison of first shock success of monophasic and biphasic waveforms in out‐of‐hospital cardiac arrest. Resuscitation 2003; 58: 17–24. [DOI] [PubMed] [Google Scholar]
- 37. Martens PR, Russell JK, Wolcke B, Paschen H, Kuisma M, Gliner BE, Weaver WD, Bossaert L, Chamberlain D, Schneider T. Optimal Response to Cardiac Arrest study: defibrillation waveform effects. Resuscitation 2001; 49: 233–43. [DOI] [PubMed] [Google Scholar]
- 38. Carpenter J, Rea TD, Murray JA, Kudenchuk PJ, Eisenberg MS. Defibrillation waveform and post‐shock rhythm in out‐of‐hospital ventricular fibrillation cardiac arrest. Resuscitation 2003; 59: 189–96. [DOI] [PubMed] [Google Scholar]
- 39. Morrison LJ, Henry RM, Ku V, Nolan JP, Morley P, Deakin CD. Single‐shock defibrillation success in adult cardiac arrest: a systematic review. Resuscitation 2013; 84: 1480–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. AED models registered within the Danish automated external defibrillator online network in The Capital Region of Denmark ultimo 2014.


