Abstract
Objective
Predictors of permanent disability among individuals with spinal dysraphism are not well established. We examined potential risk factors for self-reported permanent disability among adults with spinal dysraphism.
Methods
188 consecutive individuals followed in an adult spinal dysraphism clinic completed a standardized National Spina Bifida Patient Registry survey. Chi-square tests and logistic regression were used to assess bivariate relationships, while multivariate logistic regression was used to identify factors independently associated with self-identification as “permanently disabled.”
Results
A total of 106 (56.4%) adults with spina bifida identified themselves as permanently disabled. On multivariate analysis, relative to completion of primary and/or secondary school, completion of technical school (OR 0.01 95% CI 0-0.40 p=0.021), some college (OR 0.22 95% CI 0.08-0.53 p<0.001), a college degree (OR 0.06 95% CI 0.003-0.66 p=0.019), and an advanced degree (OR 0.12 95% CI 0.03-0.45 p=0.019) were negatively associated with permanent disability. Relative to open myelomeningocele, diagnosis of closed spinal dysraphism was also negatively associated with permanent disability (OR 0.20, 95% CI 0.04-0.90, p=0.036). Additionally, relative to no stool incontinence, stool incontinence occurring at least daily (OR 6.41, 95% CI 1.56-32.90, p=0009) or more than weekly (OR 3.43, 95% CI 1.10-11.89, p=0.033) were both positively associated with permanent disability. There was a suggestion of a dose-response relationship with respect to the influence of educational achievement and frequency of stool incontinence on likelihood of permanent disability.
Conclusions
Our findings suggest that level of education and degree of stool incontinence are the strongest predictors of “permanent disability” among adults with spinal dysraphism. These findings will be the basis of efforts to improve community engagement and to improve readiness for transition to adult care in a multidisciplinary pediatric spina bifida clinic.
Keywords: spinal dysraphism, employment, outcome assessment, adult
Introduction
Spinal dysraphism is the most common congenital abnormality of the spinal cord, and the most complex congenital condition with high rates of survival into adulthood.6 While 75% of these individuals can expect to reach adulthood,6,10 there is great variability in the range and degree of disability,21 and multiple medical and psychosocial limitations pose challenges to full community engagement.
Studies on the impact of medical factors on quality of life and employment status among adults with spina bifida are conflicting.2,8,10,31 Current data are frequently extrapolated from studies including patients with cerebral palsy.3,36
In this retrospective cohort study, we compared adults with spinal dysraphism who identify themselves as permanently disabled to adults that are either employed, seeking work, a current student, volunteer worker, or homemaker with respect to their continence status for both bladder and bowel, education status, race, functional level of lesion, and medical comorbidities. We hypothesize that both medical and psychosocial factors interact to influence employment status in adults with spina bifida. The purpose of this study is to better appreciate the relative importance of these factors on employment status in this population.
Methods
Patient Selection and Description of Adult Spinal Dyraphism Program
All individuals treated at the University of Alabama at Birmingham (UAB) Multidisciplinary Adult Spina Bifida Clinic between October 2010 and March 2016 were retrospectively identified in April 2016 from the computerized medical record. The Adult Spina Bifida Clinic is a multidisciplinary clinic including providers in the fields of neurosurgery, urology, physical medicine and rehabilitation, social work, physical therapy and occupational therapy. Adults attending this clinic carry a diagnosis of spinal dysraphism, including myelomeningocele, meningocele, split cord malformation, lipomyelomeningocele, dermal sinus tract, and “other”. Data included in this study are collected for all adults with spina bifida as part of data collection for the National Spina Bifida Patient Registry (NSBPR, http://www.cdc.gov/ncbddd/spinabifida/nsbprregistry.html) and during routine standard of care. Participants were asked to complete a standardized questionnaire at each clinic visit which included the variables under study. Sample size was determined by the number of participants for whom complete data points were available.
Data Collection
At each visit to the Multidisciplinary Adult Spina Bifida Clinic, an interview is conducted by the clinic coordinator. All NSBPR variables are recorded at that time and entered into the NSBPR electronic medical record (EMR).
As part of the NSBPR questionnaire, participants are first asked whether they are currently employed. If yes, they specified full-time or part-time employment. If no, they selected one of the following reasons why they were not currently employed: 1) seeking work, 2) occasional worker, 3) volunteer, 4) child, 5) student, 6) retired, 7) homemaker, or 8) permanently disabled. Therefore, the individuals who identify as permanently disabled are only those sho are not engaged in any of the other activities listed. The classification of “permanently disabled” is not a reflection of receipt of government disability benefits, as some individuals may receive these benefits, despite part time or volunteer employment. The primary outcome for this study was self-identified permanent disability. The above employment data were therefore classified dichotomously as either permanently disabled or not permanently disabled.
For each participant, the following data points were also retrieved from the NSBPR EMR: age, gender, body mass index (BMI, stratified as less than 30, between 30 and 40, and greater than 40), primary diagnosis (open myelomeningocele, lipomyelomeningocele, diastematomyelia, other), race (white, black, other), ethnicity (Hispanic or Latino versus not Hispanic or Latino), education level (primary/secondary, technical school, some college, college degree, advanced degree), insurance status (commercial insurance, Medicaid, Medicare, or “other”), indication of whether participant transitioned to adult spina bifida clinic from Children’s of Alabama pediatric spina bifida clinic or other hospital (yes versus no), current bowel management program (yes versus no), current bladder management program (yes versus no), frequency of stool incontinence (at least daily, less than daily but more than weekly, less than weekly but more than monthly, less than monthly, never, or unable to assess), frequency of urinary incontinence (at least daily, less than daily but more than weekly, less than weekly but more than monthly, less than monthly, never, or unable to assess), ambulation status (ambulates in the community, ambulates only within the home, ambulates only during organized therapy, or non-ambulatory), functional level of lesion (thoracic (no motor function in lower extremities), high-lumbar (knee extension present), mid-lumbar (knee extension present), low-lumbar (foot dorsiflexion present), sacral (foot plantarflexion present)), presence of a ventricular shunt (yes versus no), and number of ventricular shunt revisions. 156 out of 188 participants had BMI data available, and 180 out of 188 participants had insurance data available. Otherwise there were no missing data points.
Statistical Analysis
First, descriptive statistics were utilized to analyze univariate relationships between permanent disability and other variables. Logistic regression analysis for comparison of continuous variables and chi-square determination for comparison of proportions were applied to find significant associations between covariates and permanent disability. To test for independent association between permanent disability and the predictor variables, a multivariate logistic regression model was constructed, including those variables with a p value less than 0.2 on bivariate analysis. Insurance status was not included in the multivariate model as it is highly collinear with employment. A receiver operating characteristic curve was fit for permanent disability as a function of those variables which remained significantly associated with permanent disability on multivariate analysis.
Associations with P<0.05 were regarded as significant. JMP® 12 (SAS Institute, Cary, North Carolina, USA) was used for all statistical analyses. This study was approved by the institutional review board of the University of Alabama at Birmingham. The manuscript was prepared using the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) checklist for cohort studies.
Results
Study Population
A total of 188 adults with spina bifida were included. Age ranged from 19.1 to 74.6 years (median 28.5), and 119 (63.3%) were female (Table 1). Diagnoses included open myelomeningocele (163 participants, 86.7% of total), lipomyelomeningocele (17 participants, 9.0%), diastematomyelia (5 participants, 2.7%), and one each with meningocele, myelocystocele, and fibrolipoma of filum terminale (0.5% each). 109 participants (58.0%) had completed primary and/or secondary school, 2 (1%) had completed technical school, 50 (26.6%) had completed some college, 20 (10.6%) had a college degree, and 7 (3.7%) held an advanced degree. 106 participants (56.4%) reported they were not currently employed and identified themselves as permanently disabled. Of the remaining 82 participants, 33 (17.6%) were employed either full or part time, 26 (13.8%) were active students, and 23 (12.2%) were either volunteers, currently seeking work, occasional workers, retired, or working as a homemaker. Eighty-three participants (46.1%) utilized commercial insurance, 60 participants (33.3%) were on Medicaid, 31 participants (17.2%) were on Medicare, and 6 participants (3.3%) reported “other” for their insurance coverage. Forty-five participants (23.9%) reported having an active bowel management program, while 133 (70.3%) had an active bladder management program. 144 participants (60.6%) were non-ambulatory, 6 (3.2%) ambulated with assistance, 14 (7.5%) were ambulatory in the home, and 54 (28.7%) were independently ambulatory in the community. 136 participants (72.0%) had a ventricular shunt and 90 participants had at least 1 ventricular shunt revision. Frequency of stool incontinence, urinary incontinence, and functional lesion level is presented in Figure 1.
Table 1.
Demographics, functional status of cohorts, and association with permanent disability
| All patients (n=188) | Employed (n=82) | Permanent disability (n=106) | P-value† | |
|---|---|---|---|---|
|
| ||||
| Age in years, mean | 31.4 (range 19.1-74.6) | 31.9 (SD 12.2) | 31.1 (SD 7.76) | 0.538 |
|
| ||||
| Gender | 0.561 | |||
| Female | 119 (63.3%) | 50 (42.0%) | 69 (58.0%) | |
| Male | 69 (36.7%) | 32 (46.4%) | 37 (53.6%) | |
|
| ||||
| Primary diagnosis | <0.001 | |||
| Open myelomeningocele | 163 (86.7%) | 61 (37.4%) | 102 (62.6%) | |
| Lipomyelomeningocele | 17 (9.0%) | 14 (82.4%) | 3 (17.7%) | |
| Diastematomyelia | 5 (2.7%) | 5 (100%) | 0 (0%) | |
| Other | 3 (1.5%) | 2 (66.7%) | 1 (33.3%) | |
|
| ||||
| Transition from Children’s of Alabama | 0.754 | |||
| No | 117 (62.2%) | 50 (42.7%) | 67 (57.3%) | |
| Yes | 71 (37.8%) | 32 (45.1%) | 39 (54.9%) | |
|
| ||||
| Race | 0.199 | |||
| White | 155 (82.5%) | 72 (46.5%) | 83 (53.5%) | |
| Black | 31 (16.5%) | 9 (29.0%) | 22 (71.0%) | |
| Other | 2 (1.0%) | 1 (50.0%) | 1 (50.0%) | |
|
| ||||
| Ethnicity | 0.418 | |||
| Not Hispanic or Latino | 185 (98.4%) | 80 (43.2%) | 105 (56.8%) | |
| Hispanic or Latino | 3 (1.6%) | 2 (66.7%) | 1 (33.3%) | |
|
| ||||
| BMI* | 0.596 | |||
| <30 | 94 (60.3%) | 41 (43.6%) | 53 (56.4%) | |
| 30-40 | 40 (25.6%) | 17 (42.5%) | 23 (57.5%) | |
| >40 | 22 (14.1%) | 7 (31.8%) | 15 (68.2%) | |
|
| ||||
| Education level | <0.001 | |||
| Primary/secondary | 109 (58.0%) | 28 (25.7%) | 81 (74.3%) | |
| Technical school | 2 (1%) | 1 (50%) | 1 (50%) | |
| Some college | 50 (26.6%) | 33 (66.0%) | 17 (34.0%) | |
| College degree | 20 (10.6%) | 14 (70.0%) | 6 (30.0%) | |
| Advanced degree | 7 (3.7%) | 6 (85.7%) | 1 (14.3%) | |
|
| ||||
| Insurance status | <0.001) | |||
| Commercial insurance | 83 (46.1%) | 51 (61.5%) | 32 (38.5%) | |
| Medicaid | 60 (33.3%) | 13 (21.7%) | 47 (78.3%) | |
| Medicare | 31 (17.2%) | 13 (41.9%) | 18 (58.1%) | |
| Other | 6 (3.3%) | 2 (33.3%) | 4 (66.7) | |
|
| ||||
| Active bowel management program | 0.365 | |||
| No | 143 (76.1%) | 65 (45.5%) | 78 (54.5%) | |
| Yes | 45 (23.9%) | 17 (37.8%) | 28 (62.2%) | |
|
| ||||
| Active bladder management program (self-catheterization) | 0.749 | |||
| No | 55 (29.3%) | 23 (41.8%) | 32 (58.2%) | |
| Yes | 133 (70.3%) | 59 (44.4%) | 74 (55.6%) | |
|
| ||||
| Stool incontinence frequency, mean (SD) | 0.001 | |||
| At least daily | 25 (13.3%) | 4 (16.0%) | 21 (84.0%) | |
| Less than daily, more than weekly | 30 (15.9%) | 8 (26.7%) | 22 (73.3%) | |
| Less than weekly, more than monthly | 15 (8.0%) | 6 (40.0%) | 9 (60.0%) | |
| Less than monthly | 8 (4.2%) | 3 (37.5%) | 5 (62.5%) | |
| Never | 80 (42.6%) | 47 (58.8%) | 33 (41.2%) | |
| Cannot assess | 30 (15.9% | 14 (46.7%) | 16 (53.3%) | |
|
| ||||
| Urine incontinence frequency, mean (SD) | 0.037 | |||
| At least daily | 48 (25.5%) | 15 (31.3%) | 33 (68.8%) | |
| Less than daily, more than weekly | 11 (5.9%) | 4 (36.4%) | 7 (63.6%) | |
| Less than weekly, more than monthly | 13 (6.9%) | 5 (38.5%) | 8 (61.5%) | |
| Less than monthly | 4 (2.1%) | 0 (0%) | 4 (100%) | |
| Never | 83 (44.1%) | 45 (54.2%) | 38 (45.8%) | |
| Cannot assess | 29 (15.4%) | 13 (44.8%) | 16 (55.2%) | |
|
| ||||
| Functional lesion level | 0.206 | |||
| Thoracic (flaccid lower extremities) | 84 (44.7%) | 29 (34.5) | 55 (65.5%) | |
| High-lumbar (hip flexion present) | 18 (9.6%) | 9 (50.0) | 9 (50.0%) | |
| Mid-lumbar (knee extension present) | 38 (20.2%) | 20 (52.6) | 18 (47.4%) | |
| Low-lumbar (foot dorsiflexion present) | 16 (8.5%) | 8 (50.0) | 8 (50.0) | |
| Sacral (foot plantarflexion present) | 32 (17.0%) | 15 (46.9) | 17 (53.1%) | |
|
| ||||
| Independent ambulation | 0.021 | |||
| Community ambulation | 54 (28.7%) | 33 (61.1%) | 21 (38.9%) | |
| Household ambulation | 14 (7.5%) | 6 (42.9%) | 8 (57.1%) | |
| Therapeutic ambulation | 6 (3.2%) | 2 (33.3%) | 4 (66.7%) | |
| Non-ambulatory | 144 (60.6%) | 41 (36.0%) | 73 (64.0%) | |
|
| ||||
| Ventricular shunt | <0.001 | |||
| No | 52 (27.7%) | 34 (65.4%) | 18 (34.6%) | |
| Yes | 136 (72.3%) | 48 (35.3%) | 88 (64.7%) | |
|
| ||||
| Ventricular shunt revision | 0.010 | |||
| 0 | 98 (52.1%) | 53 (54.1%) | 45 (45.9%) | |
| 1-3 | 64 (34.0%) | 21 (32.8%) | 43 (67.2%) | |
| Greater than 3 | 26 (13.8)% | 8 (30.8% | 18 (69.2%) | |
Student’s t-test and logistic regression were used for comparison of means; Chi-square was used for comparison of proportions.
BMI data available for 156 patients. Complete data points available for all other patients.
Statistically significant at p<0.05
Figure 1.
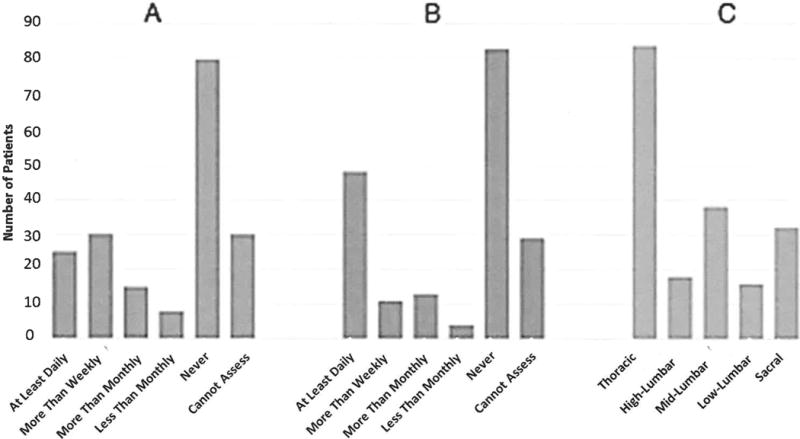
Frequency of stool incontinence, urinary incontinence, and functional lesion level of cohort
On bivariate analysis (Table 1), permanent disability was significantly associated with primary diagnosis (p<0.001), education level (p<0.001), insurance status (p<0.001), frequency of stool incontinence (p<0.001), frequency of urinary incontinence (p=0.037), ambulation status (0.021), and presence of a ventricular shunt (p<0.001). Number of ventricular shunt revisions was significantly associated with permanent disability (0, 1-3, versus >3 shunt revisions, p=0.010)
Multivariate analysis
On multivariate analysis (Table 2), education, diagnosis, and stool incontinence were independently associated with self-identification as permanently disabled. Relative to completion of primary and/or secondary school, completion of technical school (OR 0.01, 95% CI 0-0.40, p=0.021), some college (OR 0.22, 95% CI 0.08-0.53, p<0.001), college degree (OR 0.06, 95% CI 0.003-0.66, p=0.019), and holding an advanced degree (OR 0.12, 95% CI 0.03-0.45, p=0.002) were independently associated with lower likelihood of permanent disability. Due to the small number of patients with diastematomyelia and “other” spinal dysraphism, we collapsed the primary diagnosis variable into two categories for the multivariate analysis: 1) open myelomeningocele and 2) closed spinal dysraphism. Relative to open myelomeningocele, closed spinal dysraphism was independently associated with permanent disability status (OR 0.20, 95% CI 0.04-0.90, p=0.036).
Table 2.
Logistic regression models of permanent disability by covariates significantly associated on bivariate analysis
| Employment status
|
|||
|---|---|---|---|
| OR | 95% CI | P-value† | |
|
| |||
| Education | <0.001 | ||
| Primary/secondary | ref | ref | |
| Technical school | 0.01 | 0-0.40 | 0.021 |
| Some college | 0.22 | 0.08-0.53 | <0.001 |
| College degree | 0.06 | 0.003-0.66 | 0.019 |
| Advanced degree | 0.12 | 0.03-0.45 | 0.002 |
|
| |||
| Primary diagnosis | 0.036 | ||
| Open myelomeningocele | ref | ref | |
| Closed spinal dysraphism | 0.20 | 0.04-0.90 | 0.036 |
|
| |||
| Stool incontinence | 0.065 | ||
| Never | ref | ref | |
| At least daily | 6.41 | 1.56-32.90 | 0.009 |
| Less than daily, more than weekly | 3.43 | 1.10-11.89 | 0.033 |
| Less than weekly, more than monthly | 3.31 | 0.77-16.12 | 0.109 |
| Less than monthly | 0.97 | 0.16-6.77 | 0.974 |
| Cannot assess | 1.01 | 0.19-5.42 | 0.992 |
|
| |||
| Urinary incontinence | 0.151 | ||
| Never | ref | ref | |
| At least daily | 0.94 | 0.32-2.70 | 0.914 |
| Less than daily, more than weekly | 2.21 | 0.36-16.55 | 0.396 |
| Less than weekly, more than monthly | 1.55 | 0.38-6.84 | 0.543 |
| Less than monthly | ∞ | 4.35-∞ | 0.0059 |
| Cannot assess | 0.97 | 0.19-4.78 | 0.970 |
|
| |||
| Race | 0.235 | ||
| White | ref | ref | |
| Black | 2.68 | 0.86-9.04 | 0.089 |
| Other | 0.94 | 0.02-93.9 | 0.975 |
|
| |||
| Independent ambulation | 0.745 | ||
| Community ambulation | ref | ref | |
| Household ambulation | 1.89 | 0.38-10.13 | 0.440 |
| Therapeutic ambulation | 1.73 | 0.21-17.69 | 0.616 |
| Non-ambulatory | 1.71 | 0.64-4.64 | 0.285 |
|
| |||
| Ventricular shunt | 0.484 | ||
| No | ref | ref | |
| Yes | 1.55 | 0.46-5.47 | 0.484 |
|
| |||
| Ventricular shunt revision | 0.891 | ||
| 0 | ref | ref | 0.948 |
| 1-3 | 0.97 | 0.36-2.54 | |
| Greater than 3 | 1.27 | 0.39-4.33 | 0.695 |
Additionally, stool incontinence occurring at least daily (OR 6.41, 95% CI 1.56-32.90, p=0.009) or more than weekly (OR 3.43, 95% CI 1.10-11.89, p=0.033) were independently associated with increased odds of permanent disability. There was a suggestion of a dose-response relationship with respect to the influence of education achieved and frequency of stool incontinence on likelihood of permanent disability (Figure 2). Urinary incontinence, race, ambulation status, presence of a ventricular shunt, and number of ventricular shunt revisions did not correlate with permanent disability on multivariate analysis.
Figure 2.
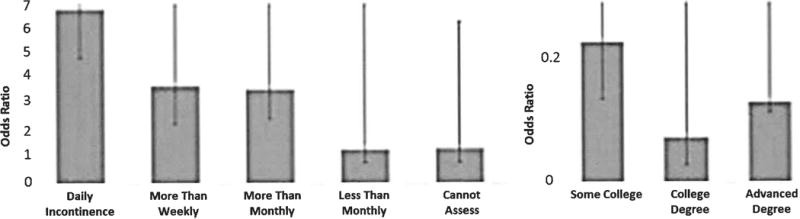
Odds of permanent disability in multivariate logistic regression as a function of a) stool continence and b) education status
A receiver operating characteristic curve was additionally fit for permanent disability as a function of those variables which remained significantly associated with permanent disability on multivariate analysis, with an area under the curve of 0.82 (Figure 3).
Figure 3.
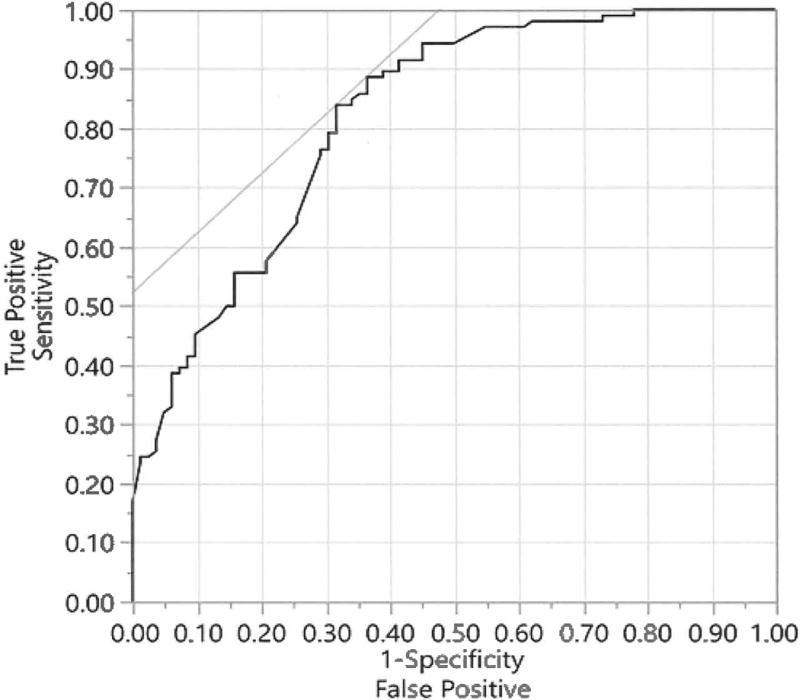
Receiver Operating Characteristic curve for permanent disability as a function of those variables significantly associated with permanent disability on multivariate analysis
Discussion
In this study of 188 adults with spina bifida, we found education level, stool incontinence, and diagnosis (open versus closed spinal dysraphism) to be independent predictors of self-reported permanent disability, which can be viewed as a surrogate for functional community participation. These findings provide a more granular description of the relationship between the various factors influencing community engagement in adults with spina bifida. We additionally observed a subjective dose-response effect on permanent disability by both frequency of stool incontinence and level of education.
Stool continence and employment
Stool incontinence carried a marked impact on permanent disability in our multivariate model, with participants experiencing daily incontinence carrying an over 6-fold likelihood of permanent disability relative to participants with less than monthly or no incontinence. Bowel dysfunction carries both physical and psychological consequences, impairing psychosocial development and self-esteem,32 and greatly impacting quality of life.7,16,28 In one study, 66% of adults with spina bifida reported stool incontinence to be a significant barrier to attending school, maintaining relationships, and obtaining employment.14
Conservative bowel management programs include dietary changes, stool softeners and bulking agents, suppositories, retrograde colonic enemas, and digital evacuation.11 Continence rates with these methods range from 67-80%, and positively impact quality of life.39 Anterograde colonic enema through a surgical ostomy may also be recommended for select individuals, with resultant continence rates exceeding 80% and reduced need for medication or rectal maneuvers.15 Despite the availability of effective regimens, only 24% of our population reported having an active bowel regimen program. Reluctance to address bowel incontinence due to stigma, or lack of awareness of treatment options, is common in adults with spina bifida.20 Our findings underscore the importance of addressing bowel continence, with significant potential impact on social functioning and employment.
van Mechelen et al found stool or urine incontinence to be predictive of employment status in a Danish population on bivariate but not multivariate analysis.38 Separating stool and urine incontinence and distinguishing frequency of incontinence may explain the difference observed in our population. Consistent with prior studies, our study showed stool incontinence to be a significant predictor in the multivariate model, while urinary incontinence did not have a meaningful effect on reported permanent disability in this population.4,38
Education and employment
Multiple studies have been reported on predictors of employment status in cerebral palsy, but data on adults with spina bifida in the United States are limited and frequently conflicting. IQ scores have been positively correlated with employment rates in these individuals,1,29 while level of education may also be a proxy for intelligence, motivation, perseverance or other positively adaptive behaviors. Among adults with cerebral palsy without cognitive impairment in the Netherlands, college education is associated with higher rates of employment.23 In both Sweden and the Netherlands, higher education did increase work participation in adults with spina bifida.37,38 The generalizability of their findings to a US-based population is uncertain however, as significant wage subsidies facilitate employment for individuals with disabilities in both countries.36 While college education does appear to improve employment rates in the United States for people with a range of disabilities in their 20s and 30s, significant employment loss occurs in the later decades.24 While age was not associated with perceived disability in the present study, only eight individuals at least fifty years of age were included. Aging with congenital disabilities is relatively unexplored, and whether a similar relationship holds true for individuals with spina bifida remains unclear.
We have observed that patients who achieve a higher level of education are less likely to consider themselves permanently disabled. Furthermore, increasing levels of education correlate with lower likelihood of perceived disability. Technical school remains an outlier, with technical school completion associated with the lowest risk of permanent disability status. However, the observed effect may have been skewed by the very small number of patients completing technical school in our population. Nevertheless, vocational schools may represent an attainable goal for many individuals, adding purpose and improving quality of life in this population.
Medical factors influencing community participation
In one study, 85% of people with spina bifida are attending or have graduated from high school and/or college, and a similar percentage have social bladder continence.6 However, community participation in these individuals is historically low, with only 30% involved in weekly organized community activities.5 It is generally accepted that multidisciplinary teams provide superior care for this population.13 Overall physical health has been shown to correlate with employment status,8 and previous reports have found ventricular shunt revision to be a negative predictor of long term achievement.12 While ventricular shunting and number of ventricular shunt revisions was associated with permanent disability in our univariate analysis, these were not significant predictors on multivariate analysis. While ventricular shunt infections have been negatively correlated with cognitive function, ventricular shunt revisions in the absence of infection have not been associated with declines in IQ scores.9,27
Our results differ from prior studies by inclusion of continence and level of education, functional metrics which we find to be the best predictors of permanent disability. Furthermore, while previous work has shown a link between the level of neurological function and survival and need for care in adulthood, we find no correlation between functional level or ambulation status and employment/disability.25,26 Seemingly minor barriers such as transportation difficulties can also hinder work participation in patents with motor disabilities.19
Finally, even in the multivariate model, individuals with closed spinal dysraphism continued to report permanent disability far less frequently than individuals with open myleomeningocele. Since ambulation status, continence, and ventricular shunting were included in the multivariate model, we must consider other potential explanations such as cognitive function for the difference between these groups. Nevertheless, this finding is encouraging for the prospect of long-term success among patients with closed spinal dysraphism.
School-to-work and pediatric-to-adult care transitions
For pediatric patients with chronic medical conditions, transitioning to adult care presents a formidable challenge.33,34 Patients and families are often reluctant to leave the familiar pediatric center and sometimes perceive a lack of interest among adult providers. Studies on transition to adult care have suggested that successful transitions are associated with adequate pre-transition patient preparation, flexible timing of transition, early introduction to the adult clinic, and invested and coordinated adult providers3,30 Similarly, school-to-work transitions require professional support, social support, consideration of transportation needs, and assistance coping with medical comorbidities, stigma, learning disabilities and executive dysfunction.17,18
To build a successful transition program for children with spina bifida, engagement of the patient and family, as well as a range of medical and social teams are essential.22,35 The results from the present study suggest that highlighting the impact of stool continence and education in the pediatric clinic may be a high-yield transitional education topic, and is worthy of further study.
Limitations
There are several limitations of our observational study design. Data were retrospectively reviewed, with potential for underreporting or inaccuracies in data reporting and coding. This study was nonrandomized, and our findings may have been confounded by unmeasured factors for which we were unable to adjust. It is also unclear whether these findings are generalizable to adults with spine bifida treated at other institutions. Additionally, we used patient self-reported permanent disability, rather than receipt of governmental disability benefits, due to lack of sensitivity and specificity of that metric. Some participants may consider themselves permanently disabled but not receive disability benefits, while other participants may receive governmental disability benefits yet still engage in volunteer or part-time work. In a related issue, we elected not to include insurance status in our multivariate model, in that insurance status is reflective of disability status, without necessarily representing a confounding variable. It is unsurprising that a high percentage of individuals identifying themselves as permanently disabled are on Medicaid, and equally unsurprising that a high percentage of people with commercial insurance do not identify themselves as permanently disabled. Given the constraints of our study design, we were unable to rigorously evaluate the independent effect of insurance status on permanent disability in this population. Finally, while community engagement influences health-related quality of life (HRQoL), it is important to note that we did not utilize validated HRQoL metrics in this study. Future work would be valuable to determine whether the same factors which influence permanent disability have a similar effect on HRQoL. Despite these limitations, we feel our findings yield important insights. A strength of the current approach was the use of multivariate techniques to adjust for potential confounding variables. The interplay of medical, psychosocial, and socioeconomic factors in adults with spina bifida is highly complex, and the independent effect of each can be difficult to ascertain.
Conclusions
Adults with spina bifida face numerous barriers to fulfilling participation in society. Our findings suggest both medical and psychosocial factors contribute in limiting these individuals in obtaining employment. Further studies are indicated to determine whether targeted medical or social service interventions can have an outsized impact on employment status in this at-risk population. This study indicates that greater emphasis should be placed on bowel management in the pediatric years to establish a working bowel program prior to reaching adulthood. Furthermore, our study supports a need for counseling adults with spina bifida and family members about the impact of advanced education in this population.
Acknowledgments
Dr. Davis completed this work as a Women’s Leadership Council Clinical Scholar in the Department of Neurosurgery at the University of Alabama at Birmingham, supported by the Kaul Foundation. Dr. Rocque is supported by NIH Grant 1KL2TR001419, and by the Kaul Pediatric Research Institute of Children’s of Alabama.
Footnotes
Disclosure: The authors have no relevant conflicts to report.
References
- 1.Barf HA, Post MWM, Verhoef M, Jennekens-Schinkel A, Gooskens RHJM, Prevo AJH. Restrictions in social participation of young adults with spina bifida. Disabil Rehabil. 2009;31:921–927. doi: 10.1080/09638280802358282. [DOI] [PubMed] [Google Scholar]
- 2.Bellin MH, Zabel TA, Dicianno BE, Levey E, Garver K, Linroth R, et al. Correlates of depressive and anxiety symptoms in young adults with spina bifida. J Pediatr Psychol. 2010;35:778–789. doi: 10.1093/jpepsy/jsp094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Binks JA, Barden WS, Burke TA, Young NL. What do we really know about the transition to adult-centered health care? A focus on cerebral palsy and spina bifida. Arch Phys Med Rehabil. 2007;88:1064–1073. doi: 10.1016/j.apmr.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 4.Bomalaski MD, Teague JL, Brooks B. The long-term impact of urological management on the quality of life of children with spina bifida. J Urol. 1995;154:778–781. doi: 10.1097/00005392-199508000-00120. [DOI] [PubMed] [Google Scholar]
- 5.Boudos RM, Mukherjee S. Barriers to community participation: Teens and young adults with spina bifida. J Pediatr Rehabil Med. 2008;1:303–310. [PubMed] [Google Scholar]
- 6.Bowman RM, McLone DG, Grant JA, Tomita T, Ito JA. Spina bifida outcome: a 25-year prospective. Pediatr Neurosurg. 2001;34:114–120. doi: 10.1159/000056005. [DOI] [PubMed] [Google Scholar]
- 7.Choi EK, Im YJ, Han SW. Bowel Management and Quality of Life in Children With Spina Bifida in South Korea. Gastroenterol Nurs. 2015 doi: 10.1097/SGA.0000000000000135. [DOI] [PubMed] [Google Scholar]
- 8.Cox A, Breau L, Connor L, McNeely PD, Anderson PA, MacLellan DL. Transition of care to an adult spina bifida clinic: patient perspectives and medical outcomes. J Urol. 2011;186:1590–1594. doi: 10.1016/j.juro.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 9.Del Bigio MR. Neuropathological changes caused by hydrocephalus. Acta Neuropathol. 1993;85:573–585. doi: 10.1007/BF00334666. [DOI] [PubMed] [Google Scholar]
- 10.Dicianno BE, Kurowski BG, Yang JMJ, Chancellor MB, Bejjani GK, Fairman AD, et al. Rehabilitation and medical management of the adult with spina bifida. Am J Phys Med Rehabil. 2008;87:1027–1050. doi: 10.1097/PHM.0b013e31818de070. [DOI] [PubMed] [Google Scholar]
- 11.Eire PF, Cives RV, Gago MC. Faecal incontinence in children with spina bifida: the best conservative treatment. Spinal Cord. 1998;36:774–776. doi: 10.1038/sj.sc.3100694. [DOI] [PubMed] [Google Scholar]
- 12.Hunt GM, Oakeshott P, Kerry S. Link between the CSF shunt and achievement in adults with spina bifida. J Neurol Neurosurg Psychiatr. 1999;67:591–595. doi: 10.1136/jnnp.67.5.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kennedy A, Sloman F, Douglass JA, Sawyer SM. Young people with chronic illness: the approach to transition. Intern Med J. 2007;37:555–560. doi: 10.1111/j.1445-5994.2007.01440.x. [DOI] [PubMed] [Google Scholar]
- 14.Krogh K, Lie HR, Bilenberg N, Laurberg S. Bowel function in Danish children with myelomeningocele. APMIS Suppl. 2003:81–85. [PubMed] [Google Scholar]
- 15.Lemelle JL, Guillemin F, Aubert D, Guys JM, Lottmann H, Lortat-Jacob S, et al. A multicentre study of the management of disorders of defecation in patients with spina bifida. Neurogastroenterol Motil. 2006;18:123–128. doi: 10.1111/j.1365-2982.2005.00737.x. [DOI] [PubMed] [Google Scholar]
- 16.Lemelle JL, Guillemin F, Aubert D, Guys JM, Lottmann H, Lortat-Jacob S, et al. Quality of life and continence in patients with spina bifida. Qual Life Res. 2006;15:1481–1492. doi: 10.1007/s11136-006-0032-x. [DOI] [PubMed] [Google Scholar]
- 17.Lindsay S, McPherson AC, Maxwell J. Perspectives of school-work transitions among youth with spina bifida, their parents and health care providers. Disabil Rehabil. 2016:1–12. doi: 10.3109/09638288.2016.1153161. [DOI] [PubMed] [Google Scholar]
- 18.Liptak GS, Garver K, Dosa NP. Spina bifida grown up. J Dev Behav Pediatr. 2013;34:206–215. doi: 10.1097/DBP.0b013e31828c5f88. [DOI] [PubMed] [Google Scholar]
- 19.Magill-Evans J, Galambos N, Darrah J, Nickerson C. Predictors of employment for young adults with developmental motor disabilities. Work. 2008;31:433–442. [PubMed] [Google Scholar]
- 20.Mattsson S, Gladh G. Tap-water enema for children with myelomeningocele and neurogenic bowel dysfunction. Acta Paediatr. 2006;95:369–374. doi: 10.1080/08035250500437507. [DOI] [PubMed] [Google Scholar]
- 21.McDonnell GV, McCann JP. Issues of medical management in adults with spina bifida. Childs Nerv Syst. 2000;16:222–227. doi: 10.1007/s003810050502. [DOI] [PubMed] [Google Scholar]
- 22.Mennito SH, Clark JK. Transition medicine: a review of current theory and practice. South Med J. 2010;103:339–342. doi: 10.1097/SMJ.0b013e3181d32356. [DOI] [PubMed] [Google Scholar]
- 23.Michelsen SI, Uldall P, Kejs AMT, Madsen M. Education and employment prospects in cerebral palsy. Dev Med Child Neurol. 2005;47:511–517. doi: 10.1017/s0012162205001015. [DOI] [PubMed] [Google Scholar]
- 24.Mitchell JM, Adkins RH, Kemp BJ. The Effects of Aging on Employment of People with and without Disabilities. J Rehab Couns Bull. 2006;49(3):157–165. [Google Scholar]
- 25.Oakeshott P, Hunt GM, Poulton A, Reid F. Expectation of life and unexpected death in open spina bifida: a 40-year complete, non-selective, longitudinal cohort study. Dev Med Child Neurol. 2010;52:749–753. doi: 10.1111/j.1469-8749.2009.03543.x. [DOI] [PubMed] [Google Scholar]
- 26.Oakeshott P, Hunt GM, Poulton A, Reid F. Open spina bifida: birth findings predict long-term outcome. Arch Dis Child. 2012;97:474–476. doi: 10.1136/archdischild-2011-300624. [DOI] [PubMed] [Google Scholar]
- 27.Ralph K, Moylan P, Canady A, Simmons S. The effects of multiple shunt revisions on neuropsychological functioning and memory. Neurol Res. 2000;22:131–136. doi: 10.1080/01616412.2000.11741049. [DOI] [PubMed] [Google Scholar]
- 28.Rendeli C, Ausili E, Tabacco F, Caliandro P, Aprile I, Tonali P, et al. Assessment of health status in children with spina bifida. Spinal Cord. 2005;43:230–235. doi: 10.1038/sj.sc.3101707. [DOI] [PubMed] [Google Scholar]
- 29.Roach JW, Short BF, Saltzman HM. Adult consequences of spina bifida: a cohort study. Clin Orthop Relat Res. 2011;469:1246–1252. doi: 10.1007/s11999-010-1594-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rutishauser C, Akré C, Surìs J-C. Transition from pediatric to adult health care: expectations of adolescents with chronic disorders and their parents. Eur J Pediatr. 2011;170:865–871. doi: 10.1007/s00431-010-1364-7. [DOI] [PubMed] [Google Scholar]
- 31.Sawin KJ, Bellin MH. Quality of life in individuals with spina bifida: a research update. Dev Disabil Res Rev. 2010;16:47–59. doi: 10.1002/ddrr.96. [DOI] [PubMed] [Google Scholar]
- 32.Sawin KJ, Thompson NM. The experience of finding an effective bowel management program for children with spina bifida: the parent’s perspective. J Pediatr Nurs. 2009;24:280–291. doi: 10.1016/j.pedn.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 33.Scal P, Evans T, Blozis S, Okinow N, Blum R. Trends in transition from pediatric to adult health care services for young adults with chronic conditions. J Adolesc Health. 1999;24:259–264. doi: 10.1016/s1054-139x(98)00127-x. [DOI] [PubMed] [Google Scholar]
- 34.Steinbeck KS, Brodie L, Towns SJ. Transition in chronic illness: Who is going where? J Paediatr Child Health. 2008;44:478–482. doi: 10.1111/j.1440-1754.2008.01321.x. [DOI] [PubMed] [Google Scholar]
- 35.Stellman-Ward G, Bannister CM, Lewis M. Assessing the needs of the adult with spina bifida. Eur J Pediatr Surg. 1993;3(Suppl 1):14–16. doi: 10.1055/s-2008-1066054. [DOI] [PubMed] [Google Scholar]
- 36.Törnbom M, Jonsson U, Sunnerhagen KS. Work participation among middle-aged persons with cerebral palsy or spina bifida–a longitudinal study. Disabil Health J. 2014;7:251–255. doi: 10.1016/j.dhjo.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 37.Valtonen K, Karlsson A-K, Alaranta H, Viikari-Juntura E. Work participation among persons with traumatic spinal cord injury and meningomyelocele1. J Rehabil Med. 2006;38:192–200. doi: 10.1080/16501970500522739. [DOI] [PubMed] [Google Scholar]
- 38.van Mechelen MC, Verhoef M, van Asbeck FWA, Post MWM. Work participation among young adults with spina bifida in the Netherlands. Dev Med Child Neurol. 2008;50:772–777. doi: 10.1111/j.1469-8749.2008.03020.x. [DOI] [PubMed] [Google Scholar]
- 39.Velde SV, Biervliet SV, Bruyne RD, Winckel MV. A systematic review on bowel management and the success rate of the various treatment modalities in spina bifida patients. Spinal Cord. 2013;51:873–881. doi: 10.1038/sc.2013.123. [DOI] [PubMed] [Google Scholar]


