Abstract
One of the most unusual complications in cholethiasis is spontaneous cholecystocutaneous fistula, which has only been reported a few times in the literature. We report the case of a 76 year old man who presented with a right hypochondrium subcutaneous abscess, with pain evoked through palpation. No comorbidity in the patient’s medical history were noted. Confirmation of cholecystocutaneous fistula was made using the proper diagnostic process, which is computed tomography with contrast media, followed by hepatobiliary MRI. This confirmed the presence of a fistulous pathway between the gallbladder and the skin. The patient underwent cholecystectomy surgery and open laparotomy with en block aponeurotic muscle, skin and fistula orifice excision.
Keywords: Cholecystocutaneous, Fistula, cholethiasis, abdominal fistula, gallbladder stones, gallbladder cancer, Bile Ducts, Laparotomy
Introduction
Spontaneous cholecystocutaneous abscess or fistula is an extremely uncommon complication of gallbladder disease. Less than 100 cases have been described in the literature. The first descriptions of cholecystocutaneous fistula was made by Thelisus in 1670. Later Courvoisier reported 169 cases of biliary fistula in the 19th century 1. The natural history of the disease has changed from suppurative cholecystitis with spontaneous rupture to operative external drainage of an abscess 2. Early and effective medical and surgical management of biliary tract disease can prevent this rare condition. Stone obstruction of the biliary tree plays a crucial role in the pathophysiology of the development of this condition; intra-gallbladder pressure can increase dramatically due to the obstruction of the cystic duct. The unresolved obstruction of the bile outflow compromise gallbladder wall blood circulation, as well as lymphatic drainage, resulting in necrosis of the gallbladder wall with the fistula formation. Once pierced, the gallbladder may drain into the peritoneal cavity, causing peritoneal localized abscess or the abscess can lead into an external fistula due to its adherence to the abdominal wall 1– 3.
Case report
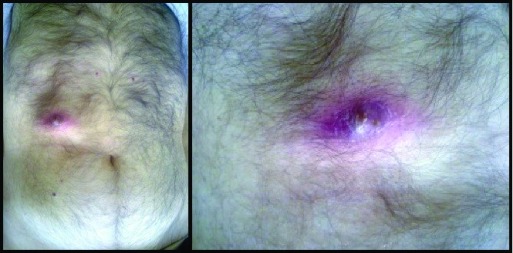
A 76 year old man was admitted to our University Hospital “Ospedale Vittorio Emenuele” and seen in our surgical department. He presented with a 3 cm tumefaction of the right hypochondrium, surrounded by an erythematous skin area, with small secretion of a yellowing-green material, attributable to a bile leaking ( Figure 1). The patient’s medical history was clear from previous medical disease and surgery; he only referred to previous upper right quadrant pain and nonspecific dyspeptic disorder.
Figure 1. Cholecystocutaneous fistula, macroscopic appearance.
An abdominal ultrasound examination revealed the presence of a lesion in the aponeurotic muscle wall, but the possible underlying pathology was unknown. No other signs of pathology were observed. Routine blood work was normal.
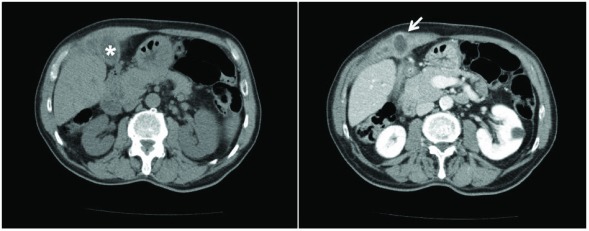
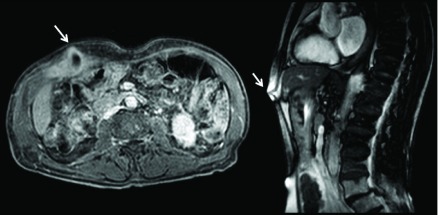
Abdominal computed tomography scan with contrast media showed the gallbladder walls had diffuse thickened and blurred edges, and the right and transverse abdominal muscles were almost covered and embedded with minute hypo-dense ailments compatible with relapsing phlogistic processes ( Figure 2). Hepatobiliary MRI detected that the gallbladder had anteriorly shifted and adhered to the right abdominal muscles. The side wall showed a break through with consensual purulent collection, which extruded through the thick abdominal wall ( Figure 3). Eventually, several different-sized stones were revealed inside the cholecyst. Consequently, a diagnosis of spontaneous cholecystocutaneous fistula was made.
Figure 2. Abdominal computed tomography images.
Left image, * indicates the gallbladder; right image, the arrows indicates the fistula.
Figure 3. Hepatobiliary MRI.
The white arrows show the fistula. From left to right: coronal and sagittal fistula view.
The patient underwent cholecystectomy surgery 10 days after diagnosis, with an open laparotomy with en block aponeurotic muscle, skin and fistula orifice excision. In order to have a good abdominal wall reconstruction, a properly shaped Prolene Prosthesis was placed using fibrin glue 4– 7. The patient received broad-spectrum antibiotics after surgery (Piperacillin/Tazobactam 4.5 g, 3 times a day for 5 days via IV).
Considering the patient’s good general condition and good post-operative course, discharge was on the seventh day post-surgery. Surgical wound re-dressing was made one week after discharge in our facility, where the surgical stitches were removed. Scar appearance was good and without concern. No other dressing was needed and the scar was covered with a bandage. The first follow-up was scheduled 15 days after discharge, second one 60 days from discharge. For both follow-ups, routine blood work and surgical scar checking were performed, the results of which were normal and the scar was healing normally.
A histological examination confirmed the diagnosis of chronic cholecystitis with gallstones and cholecystocutaneous fistula.
Discussion
Thanks to the progress made with medical imaging and surgical techniques, biliary fistula is today a very rare pathology 8– 11. Fistulas often represent the result of post-surgical 12 or post-traumatic 15 complications that generally involve the duodenum (77%) and colon (15%) 16.
Spontaneous cholecystocutaneous fistula represents a truly exceptional event, as confirmed by the analysis of the literature, which revealed only 28 cases published over the last 10 years ( Table 1). This disease mainly affects female subjects over the age of 60. Etiology is generally due to an acute inflammatory process as a consequence of a cholecystitis or chronic gallstones disease 17– 20, although there are described cases of spontaneous cholecystocutaneous fistula in the absence of gallstones 21. Rarely does cholecystocutaneous fistula evolve into a neoplastic process. Instead, fistula can be a sign of gallbladder cancer 19, 20. According to Sibakoti, polyarteritis nodosa with gallbladder vasculitis and prolonged use of high dose steroids can be considered predisposing factors 21. Fistula primum movens is by cystic duct obstruction, which increases the pressure within the gallbladder, with wall distension and impaired vascularization, resulting in the formation of focal necrosis of the wall with perforation evolution and abscess formation to the surrounding area that will rupture in to the continuous structures. In the present case, the abscess drained through the abdominal wall and the fistulose pathway originated from the bottom of the gallbladder. This area is the most distant from the cystic artery and physiologically the least vascularized and therefore more susceptible to ischemia 17.
Table 1. Publications within the last 10 years concerning cholecystocutaneous fistula.
| Author(s) | Year
published |
Number
of cases |
Country | Age | Gender | Treatment
technique |
|---|---|---|---|---|---|---|
| Maynard et al. 35 | 2016 | 1 | United Kingdom | 68 | F | Open |
| Jayasinghe et al. 36 | 2016 | 1 | United Kingdom | >70 | F | Open |
| Guardado-B et al. 37 | 2015 | 1 | Mexico | 30 | F | Open |
| Álvarez et al. 38 | 2014 | 1 | Argentina | 79 | F | Open |
| Dixon et al. 39 | 2014 | 1 | United Kingdom | 94 | F | Open |
| Pripotnev and
Petrakos 40 |
2014 | 1 | Canada | 85 | F | Open |
| Kim et al. 41 | 2013 | 1 | Australia | Open | ||
| Jayant et al. 42 | 2013 | 1 | India | 42 | F | Open |
| Sodhi et al. 43 | 2012 | 1 | India | 66 | F | Open |
| Kapoor et al. 44 | 2013 | 1 | India | 45 | M | Open |
| Ozdemir et al. 45 | 2012 | 2 | India | 45 & 65 | M | Open |
| Ugalde Serrano et al. 46 | 2012 | 1 | Spain | 83 | M | Open |
| Andersen and
Friis-Andersen 24, 47 |
2012 | 1 | Denmark | 89 | F | Open |
| Ioamidis et al. 48 | 2012 | 1 | Greece | 71 | M | Open |
| Cheng et al. 49 | 2011 | 1 | China | Open | ||
| Gordon 50 | 2011 | 1 | U.S.A. | 83 | F | Open |
| Sayed et al. 51 | 2010 | 1 | United Kingdom | 85 | F | Open |
| Pezzilli et al. 52 | 2010 | 1 | Italy | 90 | F | Open |
| Metsemakers et al. 53 | 2010 | 1 | Belgium | 69 | M | Open |
| Tallón Aguilar et al. 54 | 2010 | 1 | Spain | 83 | F | Open |
| Kahn et al. 55 | 2010 | 1 | Ireland | 76 | M | Open |
| Hawari et al. 56 | 2010 | 1 | United Kingdom | 84 | M | Open |
| Murphy et al. 57 | 2008 | 1 | United Kingdom | 80 | M | Open |
| Ijaz et al. 58 | 2008 | 1 | United Kingdom | 80 | F | Open |
| Chatterjee et al. 59 | 2007 | 1 | India | 45 | F | Open |
| Malik et al. 60 | 2007 | 1 | United Kingdom | 76 | F | Laparoscopic |
The external fistular orifice is usually on the right upper quadrant, but other locations have been described, including the left hypocondrium, umbilical scar, right lumbar, and right iliac fossa, and rarely the right gluteus and breast region 19, 24, 47.
The diagnostic process always begins with upper abdomen ultrasound and ends with hepatobiliary MRI to visualize the biliary tree. Considering that 11% of cholecystitis have concomitant presence of gallstones in the main bile duct, it is advisable to perform endoscopic retrograde cholangiopancreatography (ERCP) 2– 29. In our case CT with CM and hepatobiliary MRI confirmed the fistula presence and it was not necessary to execute the ERCP before surgery. Although an intraoperative cholangiogram was performed to check that the bile ducts were clear from gallstones. Cholecystocutaneous fistula has always been treated by two different strategies. The first includes a two-step approach: percutaneous drainage and antibiotic therapy, and subsequently cholecystectomy. The second directly involves laparotomy cholecystectomy execution with en block aponeurotic muscles, as well as skin and fistula orifice excision.
The second strategy is the most commonly used since the two-step approach treatment is reserved for patients with sepsis and poor general condition 12, 15, 29.
In 1998, Kumar described the first case of gynecological fistula treated with laparoscopic technique, proposing to the scientific community the feasibility of this innovative approach 27, 30.
Conclusion
Rarity of this pathology confirms the great quality of progress made by early diagnostic techniques and medical treatment to prevent complication of cholethiasis. Although cholecystocutaneous spontaneous fistula is not common, it can lead to a serious condition. If not quickly treated, it can rapidly evolve into a generalized septic state with severe impairment prognosis. In our case, the patient was in good health arguably because the fistula was draining the most of the abscess outside the body and not in the peritoneum space. Surgical treatment was, however, essential to restore the physiologic bile flow and adequate broad-spectrum antibiotic prophylaxis lowed the risk of post-operative infections. Although laparoscopic approaches have been described since 1998, this pathology is, in most cases, continuing to be treated with open technique, most likely because it is easier and with fewer risks of post-surgical complications 31– 34.
Consent
Written informed consent was obtained from the patient for the publication of the patient’s clinical details and related images.
Funding Statement
The author(s) declared that no grants were involved in supporting this work.
[version 1; referees: 3 approved]
References
- 1. Flora HS, Bhattacharya S: Spontaneous cholecystocutaneous fistula. HPB (Oxford). 2001;3(4):279–280. 10.1080/136518201753335584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gupta V, Benerjee S, Garg H, et al. : Spontaneous cholecysto-antral-cutaneous fistula: a consequence of neglected calculus cholecystitis. Singapore Med J. 2012;53(10):e201–3. [PubMed] [Google Scholar]
- 3. Mathew G, Bhimji SS: Fistula, Cholecystocutaneous.University of Pelita Harapan,2017. 28846261 [Google Scholar]
- 4. Zanghì G, Rinzivillo NM, Caponnetto AM, et al. : Sentinel lymph node biopsy in breast cancer New indications and our experience. Ann Ital Chir. 2015;86:508–12. [PubMed] [Google Scholar]
- 5. Biondi A, Tropea A, Monaco G, et al. : [Complications in the laparoscopic treatment of primary and secondary hernias of the abdominal wall]. Ann Ital Chir. 2010;81(3):193–198. [PubMed] [Google Scholar]
- 6. Zanghì G, Di Stefano G, Leanza V, et al. : Incisional hernia in day surgery: our personal experience. G Chir. 2012;33(6–7):218–220. [PubMed] [Google Scholar]
- 7. Leanza V, Zanghì G, Vecchio R, et al. : How to prevent mesh erosion in transobturator tension-free incontinence cystocoele treatment (TICT): a comparative survey. G Chir. 2015;36(1):21–25. [PMC free article] [PubMed] [Google Scholar]
- 8. Courvoisier L: Pathologie and Chirurgie derGallenwege. Leipzig, Germany: FCW Vogel;1890. [Google Scholar]
- 9. Naunyn B: Ulcerative affections of the biliary passage and fistula formation. In: A Treatise on Cholelithiasis. New Syndenham Society; (English version 1896). New Syndenham Society;1892;138–151. Reference Source [Google Scholar]
- 10. Bonnet: Fistule biliaire cutanee. Lyon Med. 1897;85. [Google Scholar]
- 11. Henry CL, Ort TG, Jr: Spontaneous external biliary fistulas. Surgery. 1949;26(4):641–646. [PubMed] [Google Scholar]
- 12. Czerniak A, Blumgart LH: External biliary fistula. (External Biliary Fistula, Surgery of the Liver and Biliary Tract).Churchill Livingstone; Edinburgh,1994;1. [Google Scholar]
- 13. Smith EE, Bowley N, Allison DJ: The management of post-traumatic intrahepatic cutaneous biliary fistulas. Br J Surg. 1982;69(6):317–318. 10.1002/bjs.1800690608 [DOI] [PubMed] [Google Scholar]
- 14. Glenn F, Reed C, Grafe WR: Biliary enteric fistula. Surg Gynecol Obstet. 1981;153(4):527–531. [PubMed] [Google Scholar]
- 15. Cruz RJ Jr, Nahas J, de Figueiredo LF: Spontaneous cholecystocutaneous fistula: a rare complication of gallbladder disease. Sao Paulo Med J. 2006;124(4):234–6. 10.1590/S1516-31802006000400012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Flora HS, Bhattacharya S: Spontaneous cholecystocutaneous fistula. HPB (Oxford). 2001;3(4):279–280. 10.1080/136518201753335584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ugalde Serrano P, Solar García L, Miyar de León A, et al. : [Cholecystocutaneous fistula as a first sign of presentation of a gallbladder adenocarcinoma]. Cir Esp. 2013;91(6):396–397. 10.1016/j.ciresp.2011.12.009 [DOI] [PubMed] [Google Scholar]
- 18. Zanghì G, Leanza V, Vecchio R, et al. : Neoplastic sigmoid-uterine fistula. An exceptional complication of large intestine cancer. G Chir. 2017;38(1):37–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kuo YC, Wu CS: Spontaneous cutaneous biliary fistula: a rare complication of cholangiocarcinoma. J Clin Gastroenterol. 1990;12(4):451–453. [DOI] [PubMed] [Google Scholar]
- 20. Birch BR, Cox SJ: Spontaneous external biliary fistula uncomplicated by gallstones. Postgrad Med J. 1991;67(786):391–2. 10.1136/pgmj.67.786.391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sibakoti YC, Basnet RB, Poudel R: Spontaneous Cholecystocutaneous Fistula: A Case Report. PMJM. 2012;12(1):51–54. Reference Source [Google Scholar]
- 22. Gibson TC, Howat JM: Cholecystocutaneous fistula. Br J Clin Pract. 1987;41(10):980–2. [PubMed] [Google Scholar]
- 23. Nicholson T, Born MW, Garber E: Spontaneous cholecystocutaneous fistula presenting in the gluteal region. J Clin Gastroenterol. 1999;28(3):276–7. 10.1097/00004836-199904000-00024 [DOI] [PubMed] [Google Scholar]
- 24. Andersen P, Friis-Andersen H: [Spontaneous cholecystocutaneous fistula presenting in the right breast]. Ugeskr Laeger. 2012;174(18):1235–1236. [PubMed] [Google Scholar]
- 25. Costi R, Gnocchi A, Di Mario F, et al. : Diagnosis and management of choledocholithiasis in the golden age of imaging, endoscopy and laparoscopy. World J Gastroenterol. 2014;20(37):13382–13401. 10.3748/wjg.v20.i37.13382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cacopardo C, Pinzone M, Berretta S, et al. : Localized and systemic bacterial infections in necrotizing pancreatitis submitted to surgical necrosectomy or percutaneous drainage of necrotic secretions. BMC Surg. 2013;13(Suppl 2):S50. 10.1186/1471-2482-13-S2-S50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bentivegna F, Cortese V, Bentivegna S, et al. : Treatment of the pancreatic stump after DCP. Eur Rev Med Pharmacol Sci. 2014;18(Suppl 2):36–39. [PubMed] [Google Scholar]
- 28. Zanghì G, Leanza V, Rinzivillo NM, et al. : Radio-guided surgery in breast cancer. Euromediterranean Biomedical Journal. 2016;11(13):101–106. 10.3269/1970-5492.2016.11.13 [DOI] [Google Scholar]
- 29. Vasanth A, Siddiqui A, O’Donnell K: Spontaneous cholecystocutaneous fistula. South Med J. 2004;97(2):183–5. 10.1097/01.SMJ.0000051150.63130.E8 [DOI] [PubMed] [Google Scholar]
- 30. Kumar SS: Laparoscopic management of a cholecystocutaneous abscess. Am Surg. 1998;64(12):1192–4. [PubMed] [Google Scholar]
- 31. Leanza V, Zanghì G, Leanza G, et al. : A specific application of two psychological measures on pelvic organ prolapse patients. Giornale Italiano di Ostetricia e Ginecologia. 2015;37(2):82–86. Reference Source [Google Scholar]
- 32. Zanghì G, Leanza V, Vecchio R, et al. : Single-Incision Laparoscopic Cholecystectomy: our experience and review of literature. G Chir. 2015;36(6):243–246. 10.11138/gchir/2015.36.6.243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Vecchio R, Marchese S, Famoso S, et al. : Colorectal cancer in aged patients. Toward the routine treatment through laparoscopic surgical approach. G Chir. 2015;36(1):9–14. 10.11138/gchir/2015.36.1.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zanghì G, Di Stefano G, Caponnetto A, et al. : Breast cancer and sentinel lymph node micrometastases: indications for lymphadenectomy and literature review. G Chir. 2014;35(11–12):260–65. [PMC free article] [PubMed] [Google Scholar]
- 35. Maynard W, McGlone ER, Deguara J: Unusual aetiology of abdominal wall abscess: cholecystocutaneous fistula presenting 20 years after open subtotal cholecystectomy. BMJ Case Rep. 2016;2016: pii: bcr2015213326. 10.1136/bcr-2015-213326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jayasinghe G, Adam J, Abdul-Aal Y: Unusual presentation of gallbladder perforation. Int J Surg Case Rep. 2016;18:42–44. 10.1016/j.ijscr.2015.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Guardado-Bermúdez F, Aguilar-Jaimes A, Ardisson-Zamora FJ, et al. : [Spontaneous cholecystocutaneous fistula]. Cir Cir.(English Edition).2015;83(1):61–64. 10.1016/j.circir.2015.04.026 [DOI] [PubMed] [Google Scholar]
- 38. Álvarez Florencia, Meraldi A, Emery NC, et al. : [Spontaneous cholecystocutaneous fistula in an elderly woman]. Rev Med Chil. 2014;142(8):1076–7. 10.4067/S0034-98872014000800017 [DOI] [PubMed] [Google Scholar]
- 39. Dixon S, Sharma M, Holtham S: Cholecystocutaneous fistula: an unusual complication of a para-umbilical hernia repair. BMJ Case Rep. 2014;2014: pii: bcr2013202417. 10.1136/bcr-2013-202417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Pripotnev S, Petrakos A: Cholecystocutaneous fistula after percutaneous gallbladder drainage. Case Rep Gastroenterol. 2014;8(1):119–22. 10.1159/000362360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kim M, Beenen E, Fergusson J: Spontaneous cholecystocutaneous fistula by gallstone erosion into abdominal wall. ANZ J Surg. 2014;84(11):888–89. 10.1111/ans.12359 [DOI] [PubMed] [Google Scholar]
- 42. Jayant M, Kaushik R, Attri AK: Spontaneous cholecystocutaneous abscess. Indian J Gastroenterol. 2014;33(5):498. 10.1007/s12664-013-0401-7 [DOI] [PubMed] [Google Scholar]
- 43. Sodhi K, Athar M, Kumar V, et al. : Spontaneous cholecysto-cutaneous fistula complicating carcinoma of the gall bladder: a case report. Indian J Surg. 2012;74(2):191–93. 10.1007/s12262-011-0280-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kapoor Y, Singh G, Khokhar M: Spontaneous cholecystocutaneous fistula-not an old time story. Indian J Surg. 2013;75(Suppl 1):188–91. 10.1007/s12262-012-0560-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ozdemir Y, Yucel E, Sucullu I, et al. : Spontaneous cholecystocutaneous fistula as a rare complication of gallstones. Bratisl Lek Listy. 2012;113(7):445–47. 10.4149/BLL_2012_099 [DOI] [PubMed] [Google Scholar]
- 46. Ugalde Serrano P, Solar García L, Miyar de León A, et al. : [Cholecystocutaneous fistula as a first sign of presentation of a gallbladder adenocarcinoma]. Cir Esp. 2013;91(6):396–97. 10.1016/j.ciresp.2011.12.009 [DOI] [PubMed] [Google Scholar]
- 47. Andersen P, Friis-Andersen H: [Spontaneous cholecystocutaneous fistula presenting in the right breast]. Ugeskr Laeger. 2012;174(18):1235–36. [PubMed] [Google Scholar]
- 48. Ioannidis O, Paraskevas G, Kotronis A, et al. : Spontaneous cholecystocutaneous fistula draining from an abdominal scar from previous surgical drainage. Ann Ital Chir. 2012;83(1):67–69. [PubMed] [Google Scholar]
- 49. Cheng HT, Wu CI, Hsu YC: Spontaneous cholecystocutaneous fistula managed with percutaneous transhepatic gallbladder drainage. Am Surg. 2011;77(12):E285–286. [PubMed] [Google Scholar]
- 50. Gordon PE, Miller DL, Rattner DW, et al. : Image of the Month—Quiz Case. Arch Surg. 2011;146(4):487–8. 10.1001/archsurg.2011.66-a [DOI] [PubMed] [Google Scholar]
- 51. Sayed L, Sangal S, Finch G: Spontaneous cholecystocutaneous fistula: a rare presentation of gallstones. J Surg Case Rep. 2010;2010(5):5. 10.1093/jscr/2010.5.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Pezzilli R, Barakat B, Corinaldesi R, et al. : Spontaneous Cholecystocutaneous Fistula. Case Rep Gastroenterol. 2010;4(3):356–60. 10.1159/000320687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Metsemakers WJ, Quanten I, Vanhoenacker F, et al. : Spontaneous Cholecystocutaneous Abscess. JBR-BTR. 2010;93(4):198–200. 10.5334/jbr-btr.289 [DOI] [PubMed] [Google Scholar]
- 54. Tallón Aguilar L, López Porras M, Molina García D, et al. : Fístula colecistocutánea. Una rara complicación de la colelitiasis. Gastroenterol Hepatol. 2010;33(7):553–54. 10.1016/j.gastrohep.2010.02.012 [DOI] [PubMed] [Google Scholar]
- 55. Khan AA, Azhar MZ, Khan AA, et al. : Spontaneous Cholecystocutaneous Fistula. J Coll Physicians Surg Pak. 2005;15(11):726–27. [PubMed] [Google Scholar]
- 56. Hawari M, Wemyss-Holden S, Parry GW: Recurrent Chest Wall Abscesses Overlying a Pneumonectomy Scar: An Unusual Presentation of a Cholecystocutaneous Fistula. Interact Cardiovasc Thorac Surg. 2010;10(5):828–29. 10.1510/icvts.2009.221085 [DOI] [PubMed] [Google Scholar]
- 57. Murphy JA, Vimalachandran CD, Howes N, et al. : Anterior abdominal wall abscess secondary to subcutaneous gallstones. Case Rep Gastroenterol. 2008;2(2):219–23. 10.1159/000137375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Ijaz S, Lidder S, Mohamid W, et al. : Cholecystocutaneous fistula secondary to chronic calculous cholecystitis. Case Rep Gastroenterol. 2008;2(1):71–75. 10.1159/000118831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Chatterjee S, Choudhuri T, Ghosh G, et al. : Spontaneous Cholecystocutaneous Fistula in a Case of Chronic Colculous Cholecystitis--a Case Report. J Indian Med Assoc. 2007;105(11):644, 646, 656. [PubMed] [Google Scholar]
- 60. Malik AH, Nadeem M, Ockrim J: Complete laparoscopic management of cholecystocutaneous fistula. Ulster Med J. 2007;76(3):166–7. [PMC free article] [PubMed] [Google Scholar]