Abstract
Background:
To determine the effects of knee taping in combination with exercise and medical treatment on functional outcome and pain of patients with knee osteoarthritis (OA).
Materials and Methods:
In a randomized single-blinded clinical trial, 36 patients with knee OA were randomly assigned to two study groups. Both groups received exercise and medical therapy for 6 weeks. In addition, the first group (20 patients) received taping in the first 3 weeks. Pain severity (assessed by visual analog scaling), weekly amount of analgesics consumption, timed get up and go test (TUG), and step tests were recorded at baseline, 3 and 6 weeks after the treatment and were further compared between two study groups.
Results:
There was no significant difference between two groups in pain severity score (P = 0.228), step test score (P = 0.771), TUG test score (P = 0.821) and weekly amount of analgesics consumption (P = 0.873) at baseline. After 3 weeks, weekly amount of analgesics consumption (P = 0.006), pain severity (P < 0.001) was significantly lower in taping group whereas step test score (P = 0.006) was significantly higher in the taping group. After 6 weeks, patients in taping group had significantly lower pain severity (P = 0.011) and higher step test score (P = 0.042). However, there was no significant difference in TUG test score (P = 0.443) and weekly amount of analgesics consumption (P = 0.270) between two groups.
Conclusion:
Therapeutic knee taping may be an effective method for short-term management of pain and disability in patients with knee OA.
Keywords: Knee taping, osteoarthritis, step test, timed get up and go test
Introduction
Osteoarthritis (OA) is the most common type of arthritis associated with high morbidity and disability especially in the elderly.[1] Because of the aging of populations and due to the obesity, a major risk factor is increasing in prevalence; the occurrence of OA is on the rise.[1] In the United States, OA prevalence will increase by 66–100% by 2020.[1] Knee OA is among the most common types of the diseases being associated with limitation of daily activity, severe pain, stiffness, swelling, and limitations of joint range of motion.[2] The goals of the treatment of OA are to alleviate pain and minimize loss of physical function. To the extent that pain and loss of function are consequences of inflammation, of weakness across the joint, and of laxity and instability, the treatment of OA involves addressing each of these impairments.[3] Comprehensive therapy consists of a multimodality approach including nonpharmacologic and pharmacologic elements.[3,4,5]
Knee OA involves different compartments that may result in modification of weight bearing of the knee leading to disturbing the weight and stress on the other compartments of the joint.[6] Involvement of patellofemoral compartment can cause severe pain especially within climbing stairs, squatting, or kneeling.[7,8] In addition, patellar misalignment led to improper distribution of forces on the lateral facet that can trigger these manifestations.[7,8] One of the treatments which is applied for management of knee OA and chronic knee pain is knee taping which is application of adhesive rigid strapping tape to the patella and/or associated soft tissue structures.[7,9,10,11,12,13] Taping of knee can reduce knee pain by improving patellofemoral alignment and lowering mechanical stress on soft tissues.[11,12] Various taping methods have been applied in different studies.[7,9,11,14,15,16] Since the inflamed soft tissue may be worsened with stretch, taping is used to reduce the load in infra-patellar fat pad or pesanserinus.[12] Taping can also enhance muscle performance and activity.[15] Taping also override the pain signals via stimulating sensory nerve endings of the skin (gate theory).[17] It is now hypothesized that taping of patella can improve patellar proprioceptive and sense of mechanical stability.[18] Recently, Ojaghi et al.[19] demonstrated that knee taping and elastic bondage is associated with improved patellofemoral pain along with improved dynamic postural control.
However, there are conflicting results in effectiveness of taping in reducing pain in patients with OA. According to these contradictory results and because this method is very safe, with few side effects and relatively inexpensive compared with other therapeutic methods, the need for further studies in this field are obvious. The present study was performed to determine the effects of knee taping in combination with exercise and medical treatment on the functional outcome of patients with knee OA.
Materials and Methods
Study population
This was a prospective randomized single-blind clinical trial being performed in a 4-month period from June to September 2014 in Al-Zahra Hospital, a tertiary health care center affiliated with Isfahan University of Medical Sciences. We included a total number of 44 patients who suffered from knee pain and diagnosed as knee OA with radiological Grade II to III (based on Kellgren–Lawrence grading scale) that referred to our center for management. All the patients were diagnosed to have OA according to the American Colleague of Rheumatology for diagnosis of knee OA.[20] We excluded those with allergic reaction to tape or any skin problem that prevents the tape (based on the history and clinical signs of dermatologic allergic reaction), presence of any inflammatory arthritis, history of any injection at knee or any surgical intervention in this part within the last 6-month, suspicion to other pathologies in the knee, severe obesity (body mass index >30 kg/m2), OA Grade IV, the instability of the knee joint (determined by physical examination and radiology), cardiovascular disorders (due to cardiovascular side-effect of celecoxib), trauma to the knee during the study, no following the treatment by patients, and performing physiotherapy within treatment schedule. The study protocol was approved by Institutional Review Board and Medical Ethics Committee of Isfahan University of Medical Sciences. All the patients provided their informed written consents before inclusion in the study. The study protocol is also registered with Iranian registry for clinical trials (www.irct.ir; IRCT2015041021673N1).
Randomization and intervention
After explaining the objectives and procedures of the study, the patients were randomly assigned by the computerized block randomization method to two treatment groups including taping group (n = 22) who received taping (in first 3 weeks) combined with exercise therapy (Paksaman® Standard Knee Tapes, Paksaman Corporations, Tehran, Iran) and medical therapy and control group (n = 22) who received only exercise and medical therapy. Taping was performed bilaterally. In our taping method, we used three tape straps: The first Y-shaped tape was placed from top to bottom of the knee, the second Y-shaped tape was placed from the lateral to the medial of the knee, and the third I-shaped tape was placed over the vastus medialis obliquus (VMO) [Figure 1].
Figure 1.

Knee taping method in the current study. Accordingly three tape straps were used: The first Y-shaped tape was placed from top to bottom of the knee, the second Y-shaped tape was placed from the lateral to the medial of the knee, and the third I-shaped tape was placed over the vastus medialis obliquus
Study protocol
Patients in two groups were equally received necessary training to reduce the pressure on the affected knee by recommendation to losing weight, refraining from kneeling, as well as training some especial exercises. These exercises were taught to all the participants in three consecutive sessions. These included stretching the hamstring and calf muscles (holding stretch for 30 s, repeating the stretch throughout the session at least 5 times, three sessions per day) and strengthening quadriceps muscles (holding contraction of muscle for 10 s, repeating it throughout the session at least 5 times, three sessions per day). The volume and frequency of the exercise was checked by self-reported diary. Drug therapy in both groups performed also equally including similar doses of celecoxib (100 mg, 1–3 capsules per day according to the pain severity that might be reduced by lowering the pain). Patients were prohibited taking other analgesics during treatment schedule. In addition to exercise therapy and medical therapy, the taping group received taping in three consecutive weeks. Tapes were replaced at each session and remained retained during the week. In case with the separation of the tape (which is very rare occurrence), the patient was referred to renew it. For all participants, pain severity was assessed using 100 mm visual analog scaling (VAS) method. To ensure that decrease in VAS score is not due to increase of analgesics, weekly amount of celecoxib capsules consumption was assessed. Furthermore, for measurement of taping effect on disability, timed get up and go test (TUG)[21] and step tests[22] were scheduled. These are validated and reliable functional test in knee OA.[23] In brief, the primary endpoint of the study was the pain intensity measured by VAS scale, results of TUG and step tests after 3 and 6 weeks of therapy. The secondary endpoints were the weekly amount of analgesic use after 3 and 6 weeks of therapy. All scores were assessed blindly by different physiatrist before the beginning of treatment as well as 3 and 6 weeks after the initial assessment. The patient and those applying the tapes were informed of the study group. Thus, it is a single-blinded study.
Statistical analysis
To have 85% power to detect 5% difference in mean VAS scores between two study groups, with the perception of α = 0.05, a total number of 18 patients were required for each study group. We included 44 patients to compensate for those who do not follow the study protocol to the end. Statistical package for social sciences (SPSS Inc., Chicago, IL, USA) version 20.0 was used for statistical analysis. Results are presented as mean ± standard deviation for quantitative variables and were summarized by frequency (percentage) for categorical variables. The nonparametric variables were compared between two study groups using Chi-square test. Parametric variables with normal distribution were compared using independent sample t-test. Repeated measure test was used to compare the trends in changes of pain intensity (VAS), step test, TUG and amount of analgesic consumption between groups. Paired t-test was used to compare the results within groups. All the comparing results are reported with 95% confidence interval (CI). A two-sided P value of <0.05 was considered statistically significant.
Results
Two patients from taping group (one due to allergic reaction to tape and other due to trauma to knee) and six patients from control groups (one patient due to physiotherapy during scheduled period, another patient due to knee effusion and 4 patients withdrew to seek treatment) excluded from study and finally 20 patients remained in the taping group and 16 patients in control group [Figure 2]. As shown is Table 1, the baseline characteristic was comparable between two study group. Both study groups had also comparable pain intensity measured by VAS (P = 0.228), step test (P = 0.771), TUG (P = 0.821), and weekly amount of analgesic use (P = 0.873) before the study.
Figure 2.
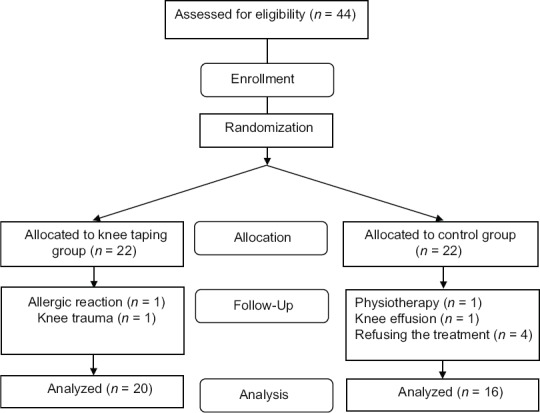
CONSORT flow diagram of the study
Table 1.
Baseline characteristics of 36 patients with knee osteoarthritis undergoing knee taping and medical therapy (n=20) or medical therapy alone (n=16)
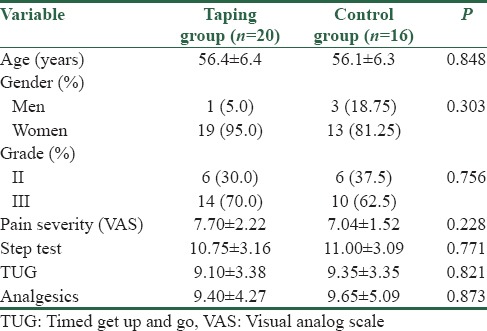
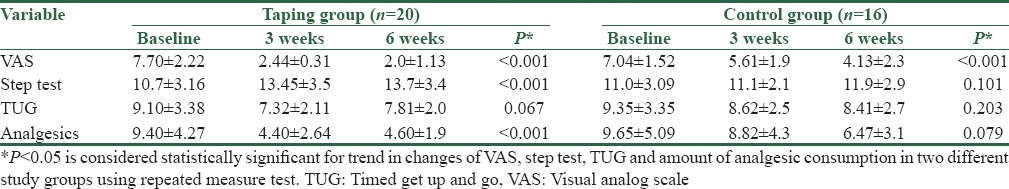
Table 2 summarizes the trends in changes of VAS, step test, TUG, and weekly amount of analgesic use in two study groups. We found that the pain intensity decreased significantly in both study groups after 6 weeks of intervention. Although the step test increased significantly in taping group (P < 0.001; CI 95%: 0.349 [−3.4–−2.1]), it remained steady in control group (P = 0.101; CI 95%: 0.53 [−2.1–0.193]) after 6 weeks of therapy. The TUG test did not decrease significantly in both study groups. However, the weekly amount of analgesics consumption decreased significantly in taping group (P < 0.001; CI 95%: 0.96 [2.78–6.18]) while it did not change in control group (P = 0.079; CI 95%: 1.69 [−0.41–6.76]) after 6 weeks of intervention [Table 2].
Table 2.
Trends in the changes of pain intensity visual analog scale, step test, timed get up and go and amount of analgesic consumption in 36 patients with knee osteoarthritis undergoing knee taping and medical therapy (n=20) or medical therapy alone (n=16)
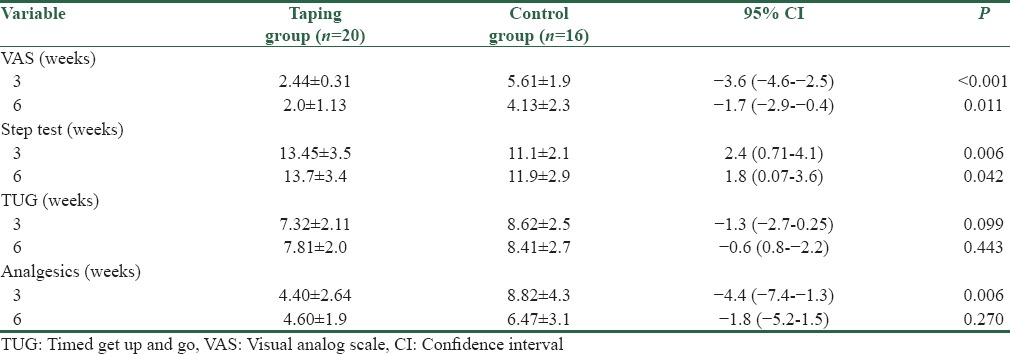
We found that those who received knee taping had significantly lower VAS after 3 (P < 0.001) and 6 (P = 0.011) weeks of therapy when compared to control group. In the same way, the step test was significantly higher after 3 (P = 0.006) and 6 (P = 0.042) weeks of therapy in taping group when compared to control group. The weekly amount of analgesic use was also lower in taping group after 3 weeks of intervention (P = 0.006). There was no significant difference between two study groups regarding the weekly amount of analgesic use after 6 weeks of therapy (P = 0.270); in addition, the TUG results were comparable between two study groups during the follow-up. Just 1 (5.0%) patient in knee taping group experienced tap separation that referred for renewing it. These results are summarized in Table 3.
Table 3.
Comparing the pain intensity, step test, timed get up and go and amount of analgesic consumption in 36 patients with knee osteoarthritis undergoing knee taping and medical therapy (n=20) or medical therapy alone (n=16)
Discussion
Treatment of OA is certainly based on a combination of treatment protocols including physical therapy, medical therapy, exercise-based therapy and even psychological counseling[4,5] Although the position of all pointed treatment in improvement of knee function and pain relief has been clearly identified, but the role of taping in relieving disease symptoms remains uncertain. A systematic review claimed that there is no strong evidence for the effectiveness of taping in knee OA.[24] But another one, emphasize that knee taping effectively relieves knee pain.[25] Arora et al. studied immediate effect of taping in patients with knee OA and concluded significant pain relief and improvement in disability.[26] Hinman et al. had also shown that therapeutic tape reduces pain and disability (assessed by SF-36) in people with OA of knee 3–6 weeks after taping.[11]
In our study, we showed that the use of taping concurrently with other protocols not only can relieve knee pain even 3 weeks after tape removal but also can significantly improve knee function in a mid-time period. One advantage of our study was that we concurrently measured amount of analgesics consumption to be sure that change in VAS score is not caused by increasing amount of analgesic consumption. Another advantage was measurement of disability with two validated tests (step test and TUG). Arora et al. studied effect of taping in disability by functional test, just immediately after taping.[26] However, we measured it during 6 weeks (3 weeks with tape and 3 weeks after tape removal). Hinman et al.,[11] had also shown that therapeutic tape reduces disability by self-reported questionnaires (SF-36). However, we used performance base functional tests, and our study confirmed their result. In applying taping method, it should be considered that despite beneficial effects of this technique it has negligible side effects (only one case showed mild allergic reaction to tape) and low cost. Especially in old patients, diabetic and renal insufficient patients with knee OA, that have limitations in analgesics consumption, taping is a safe and effective methods for pain relief.
Based on previous research,[17] applying McConnell taping and elastic bandage can reduce pain in patients with patellofemoral pain. Another study presented criteria for successful taping and standard bandage which was pain reduction on VAS scale. Therefore, increased reach distances after taping might occur due to the following reasons: (1) Pain reduction, (2) VMO muscle activity enhancement. It has been previously shown that in healthy subjects, vastus medialis activation is associated with anterior direction excursions.[27] It has also been reported that knee taping is associated with improved onset of VMO activity.[28] This revealed that VMO insufficiency might have caused functional deficits in anterior directions in patients with patellofemoral pain. Consequently, dynamic postural control improvement, especially in anterior and anterolateral reach distances, has been due to VMO facilitation. (3) Knee joint stability improvement. It is possible that medial and lateral stabilities are the most sensitive measures of postural control.[29,30] Therefore, improvement in lateral and medial excursions following taping and standard bandage respectively can be attributed to magnitude enhancement of VMO activation.
We note some limitation to our study. First, the number of patients included in the current study was less than that of calculated as a sample size in control group. We required 18 patients in each group while the control group had 16 (due to the exclusion of the patients during the study). Thus, the study might be underpowered to detect significant differences between corresponding variables. However, final power calculation revealed 80% power for this study. The other limitation is that the follow-up period was just 6 weeks which can be less than expected. Thus, longer follow-up periods are required for the next studies to determine the long-term effects of knee taping on knee OA. The other limitation was that the exercise protocol was focused on strengthening the hamstring and calf muscles, and we did not focus on hip muscles and VMO strengthening. Overall this is among the first studies determining the effects of knee taping on disability and pain of the patients with knee OA.
Conclusion
We demonstrate more lowering knee pain, more improvement in knee function, and also less need for medication following use of taping in combination with other common treatment techniques such as exercise and anti-inflammatory medication in patients with knee OA.
Financial support and sponsorship
Isfahan University of medical sciences
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to acknowledge all the patients and their families who participated in the study. We would also like to acknowledge the editorial assistant of Dr. Fariborz Ghaffarpasand during preparation and revision of the manuscript.
References
- 1.Glyn-Jones S, Palmer AJ, Agricola R, Price AJ, Vincent TL, Weinans H, et al. Osteoarthritis. Lancet. 2015;386:376–87. doi: 10.1016/S0140-6736(14)60802-3. [DOI] [PubMed] [Google Scholar]
- 2.Chu CR, Millis MB, Olson SA. Osteoarthritis: From palliation to prevention: AOA critical issues. J Bone Joint Surg Am. 2014;96:e130. doi: 10.2106/JBJS.M.01209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fibel KH, Hillstrom HJ, Halpern BC. State-of-the-art management of knee osteoarthritis. World J Clin Cases. 2015;3:89–101. doi: 10.12998/wjcc.v3.i2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, et al. American college of rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2012;64:465–74. doi: 10.1002/acr.21596. [DOI] [PubMed] [Google Scholar]
- 5.Nelson AE, Allen KD, Golightly YM, Goode AP, Jordan JM. A systematic review of recommendations and guidelines for the management of osteoarthritis: The chronic osteoarthritis management initiative of the U.S. bone and joint initiative. Semin Arthritis Rheum. 2014;43:701–12. doi: 10.1016/j.semarthrit.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 6.Blalock D, Miller A, Tilley M, Wang J. Joint instability and osteoarthritis. Clin Med Insights Arthritis Musculoskelet Disord. 2015;8:15–23. doi: 10.4137/CMAMD.S22147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cushnaghan J, McCarthy C, Dieppe P. Taping the patella medially: A new treatment for osteoarthritis of the knee joint? BMJ. 1994;308:753–5. doi: 10.1136/bmj.308.6931.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Richmond SA, Fukuchi RK, Ezzat A, Schneider K, Schneider G, Emery CA. Are joint injury, sport activity, physical activity, obesity, or occupational activities predictors for osteoarthritis. A systematic review? J Orthop Sports Phys Ther. 2013;43:515–19. doi: 10.2519/jospt.2013.4796. [DOI] [PubMed] [Google Scholar]
- 9.Anandkumar S, Sudarshan S, Nagpal P. Efficacy of kinesio taping on isokinetic quadriceps torque in knee osteoarthritis: A double blinded randomized controlled study. Physiother Theory Pract. 2014;30:375–83. doi: 10.3109/09593985.2014.896963. [DOI] [PubMed] [Google Scholar]
- 10.Crossley K, Cowan SM, Bennell KL, McConnell J. Patellar taping: Is clinical success supported by scientific evidence? Man Ther. 2000;5:142–50. doi: 10.1054/math.2000.0354. [DOI] [PubMed] [Google Scholar]
- 11.Hinman RS, Crossley KM, McConnell J, Bennell KL. Efficacy of knee tape in the management of osteoarthritis of the knee: Blinded randomised controlled trial. BMJ. 2003;327:135. doi: 10.1136/bmj.327.7407.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krustev E, Reid A, McDougall JJ. Tapping into the endocannabinoid system to ameliorate acute inflammatory flares and associated pain in mouse knee joints. Arthritis Res Ther. 2014;16:437. doi: 10.1186/s13075-014-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Warden SJ, Hinman RS, Watson MA, Jr, Avin KG, Bialocerkowski AE, Crossley KM. Patellar taping and bracing for the treatment of chronic knee pain: A systematic review and meta-analysis. Arthritis Rheum. 2008;59:73–83. doi: 10.1002/art.23242. [DOI] [PubMed] [Google Scholar]
- 14.Hinman RS, Bennell KL, Crossley KM, McConnell J. Immediate effects of adhesive tape on pain and disability in individuals with knee osteoarthritis. Rheumatology (Oxford) 2003;42:865–9. doi: 10.1093/rheumatology/keg233. [DOI] [PubMed] [Google Scholar]
- 15.Hanafy AF, Abdallah AA. Quadriceps strength, knee pain and functional performance with patellar taping in knee osteoarthritis. Journal of Musculoskeletal Research. 2014;17:1450014. [Google Scholar]
- 16.Serra MV, Vieira ER, Brunt D, Goethel MF, Gonçalves M, Quemelo PR. Kinesio taping effects on knee extension force among soccer players. Braz J Phys Ther. 2015;19:152–8. doi: 10.1590/bjpt-rbf.2014.0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bockrath K, Wooden C, Worrell T, Ingersoll CD, Farr J. Effects of patella taping on patella position and perceived pain. Med Sci Sports Exerc. 1993;25:989–92. [PubMed] [Google Scholar]
- 18.Ernst GP, Kawaguchi J, Saliba E. Effect of patellar taping on knee kinetics of patients with patellofemoral pain syndrome. J Orthop Sports Phys Ther. 1999;29:661–7. doi: 10.2519/jospt.1999.29.11.661. [DOI] [PubMed] [Google Scholar]
- 19.Ojaghi SM, Kamali F, Ghanbari A, Ebrahimi S, Nematollahi AR. Effects of taping and elastic bandage on postural control in athletes with patellofemoral pain: A randomized control trial. Galen Med J. 2015;4:82–9. [Google Scholar]
- 20.Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29:1039–49. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 21.Podsiadlo D, Richardson S. The timed “Up and Go”: A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–8. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 22.Hill KD. A new test of dynamic standing balance for stroke patients: Reliability, validity and comparison with healthy elderly. Physiother Can. 1996;48:257–62. [Google Scholar]
- 23.Bennell KL, Hinman RS, Crossley KM, Metcalf BR, Buchbinder R, Green S, et al. Is the human activity profile a useful measure in people with knee osteoarthritis? J Rehabil Res Dev. 2004;41:621–30. doi: 10.1682/jrrd.2003.07.0103. [DOI] [PubMed] [Google Scholar]
- 24.Richette P, Sautreuil P, Coudeyre E, Chevalier X, Revel M, Rannou F. Usefulness of taping in lower limb osteoarthritis. French clinical practice guidelines. Joint Bone Spine. 2008;75:475–8. doi: 10.1016/j.jbspin.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 25.Crossley KM, Marino GP, Macilquham MD, Schache AG, Hinman RS. Can patellar tape reduce the patellar malalignment and pain associated with patellofemoral osteoarthritis? Arthritis Rheum. 2009;61:1719–25. doi: 10.1002/art.24872. [DOI] [PubMed] [Google Scholar]
- 26.Arora P, Arya S, Yardi S. A study of immediate effects of taping in patients with knee osteo-arthritis. Indian J Physiother Occup Ther. 2012;6:196–201. [Google Scholar]
- 27.Aminaka N, Gribble PA. A systematic review of the effects of therapeutic taping on patellofemoral pain syndrome. J Athl Train. 2005;40:341–51. [PMC free article] [PubMed] [Google Scholar]
- 28.Powers CM, Landel R, Sosnick T, Kirby J, Mengel K, Cheney A, et al. The effects of patellar taping on stride characteristics and joint motion in subjects with patellofemoral pain. J Orthop Sports Phys Ther. 1997;26:286–91. doi: 10.2519/jospt.1997.26.6.286. [DOI] [PubMed] [Google Scholar]
- 29.Fridén T, Zätterström R, Lindstrand A, Moritz U. A stabilometric technique for evaluation of lower limb instabilities. Am J Sports Med. 1989;17:118–22. doi: 10.1177/036354658901700120. [DOI] [PubMed] [Google Scholar]
- 30.Goldie PA, Bach TM, Evans OM. Force platform measures for evaluating postural control: Reliability and validity. Arch Phys Med Rehabil. 1989;70:510–7. [PubMed] [Google Scholar]


