Abstract
Aim
Guided by the ALARA - “As Low As Reasonably Achievable” principle in radiation safety, a quality improvement project to optimise the bedside diagnostic imaging process to the best standards of care was conducted over a six month period. The goal was too reduce the radiation hazard opportunities in the neonatal intensive care unit by at least 75% from the existing level at Q2/2015, within 6 months.
Methods
The existing bedside imaging process was critically analysed and the following quality improvement initiatives were implemented namely, mandatory lead protective gear to healthcare staff, gonadal shield for neonates, guidelines for optimal collimation of X-ray beam and optimal positioning of neonates. Radiation dosimetry results, regular staff awareness sessions and strong collaboration between neonatologists, radiologists, radiographers and neonatal nurses helped to ensure compliance to the revised imaging process. Radiation hazard opportunities were measured by analysing all radiographs done during the period under baby exposure and healthcare staff exposure categories.
Summary of results
Radiation hazard opportunities were reduced by 100% to healthcare staff and 75% to neonates, and the overall reduction was 83%. The rate of discordance between radiograph request forms and images taken was measured as a surrogate marker for compliance to the project initiatives and it declined by 77%. Mandatory orientation of staff to the revised policy on the standardised diagnostic imaging process, regular radiation awareness talks and staff feedback sessions are among several measures taken to sustain the project.
Keywords: radiation safet, preterm infants, ALARA, radiation dosimetry, cumulative radiation exposure
Introduction
Radiation sensitivity is highest in the newborn period than at any other time in life, as high mitotic activity and small size make them particularly vulnerable.
While neonatal intensive care has advanced tremendously, an increasing number of survivors of high risk preterm births develop respiratory, gastrointestinal and neurodevelopmental morbidities that may require frequent diagnostic imaging examinations during early infancy and along their lifetime. The magnitude of diagnostic radiation exposure and its consequences in premature infants has thus been of increasing concern among neonatal care providers worldwide.
Problem
The Department of Neonatology and Developmental Medicine in Singapore General Hospital (SGH), a tertiary teaching institution, cares for sick newborn infants, including extremely low birthweight infants (<1000 g and <28 weeks’ gestation), with a focus on preserving their long-term neurodevelopmental health and well-being. An average of 900 bedside radiographs are performed annually on the babies admitted in the neonatal intensive care unit (NICU).
An annual audit of 859 radiographs performed in 174 infants was analysed as below (table 1).
Table 1.
Number of radiographs performed in different gestational age groups
| Radiograph | 23–28 weeks |
29–33 weeks |
34–36 weeks |
37–42 weeks |
| Chest X-ray | 126 | 93 | 37 | 61 |
| Abdominal X-ray | 15 | 18 | 1 | 0 |
| Combined X-ray | 192 | 188 | 40 | 23 |
| Other X-rays | 14 | 38 | 7 | 6 |
| Total | 347 | 337 | 85 | 90 |
The smaller the gestation the higher the number of radiographs performed during their inpatient stayand the majority of them happened during the first week of life.
Preterm infants weighing less than 750 g may be exposed to an average of 30 radiographs within the first 6 weeks of life. This trend is similar to what has been reported widely in the literature,1 2 with the smallest birthweight neonates receiving the greatest number of radiographs, related to their length of stay and the intensity of their treatments.
Bedside neonatal radiological examinations can be challenging assignments for the radiographers with varying levels of expertise, as the NICU environment makes it less than ideal for standard examination protocols to be adhered to. Neonates cannot cooperate, and very often monitoring devices, access lines or tubes may interfere with the image quality and positioning accuracy.
According to the audit, 42% of chest X-rays and 63% of abdominal X-rays were done as combined X-rays with liberal inclusion of anatomy adjacent to the region of interest. Although the very small size of patients in the NICU may be cited as a limitation for proper collimation, studies show that at least 50% reduction in unnecessary radiation exposure is feasible regardless of gestational age, birth weight or patient size with proper collimation technique alone.3
Extraneous adult fingers were frequently noted on the images. We observed that the NICU staff needs to be much closer than 1 m during radiation exposure to hold the neonate, often without lead protective gear and their hands may inadvertently fall within the primary beam. Previously published studies have shown4 that 15%–40% of NICU films had at least one adult finger visible in the images.
Also evident in the audit was the discrepancy between the radiograph requested and the image taken. Residents and nursing staff anecdotally recalled that the radiology request forms could be verbally modified to include a wider area of exposure for various reasons, for example, to check the position of a newly inserted oro-gastric feediing tube or an endotracheal tube.
An exaggerated fear of radiation injury was widely prevalent among the healthcare staff. Radiation safety concerns for the neonates in adjacent incubators were also raised by family members. Radiation dosimetry tudies including the one by Burrage et al,5 6 on scatter radiation doses using a ‘new born’ anthropomorphic phantom, have shown that environmental radiation levels are extremely low 1 m away from the radiation isocentre.
Project conception
The process of bedside imaging is a multidisciplinary team effort involving physicians, nursing staff and radiographers, and we hypothesised that standardising this process was essential to minimise variability and maximise patient safety. The wide spectrum of gestational maturity, birth weight and level of neonatal care creates a unique set of challenges for every exposure and hence ample opportunities for unnecessary and inadvertent radiation exposure to the neonates and the healthcare staff.
Uncertainty prevails regarding the dose–effect relationship between ionising radiation and biological damage, particularly in very low birthweight infants. At radiation doses below 100 mSv per year, the International Commission on Radiological Protection (ICRP)7 considers the linear no threshold model as a prudent basis for radiological protection against stochastic and heritable effects. Literature review reiterates the importance of adhering to well-defined technical protocols and protective measures for each radiographical examination in NICU, so that the lowest radiation doses are used to create the highest quality of X-ray images. This is the concept of ALARA (‘as low as reasonably achievable’) in diagnostic radio-imaging,8 which is endorsed by radiation protection organisations like ICRP and the Commission of the European Community.
Project Red RaIN (acronym for the goal statement) was conceived with the aim to investigate measure, standardise, educate and enhance radiation safety in the neonatal unit, guided by the ALARA principle.
Baseline measurements
A three-pronged strategy was adopted to quantify the existing radiation hazard opportunities in the unit.
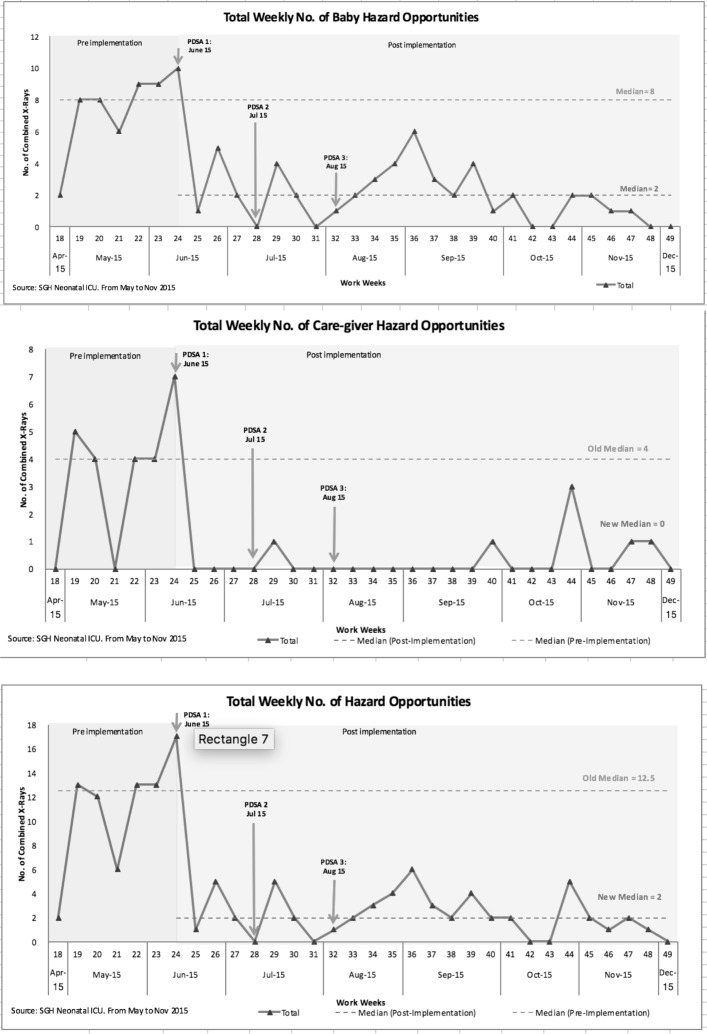
First, all radiographs done over a 4-week period were critiqued by the team, and the identified radiation hazard opportunities were categorised under two groups, namely baby hazards and caregiver hazards. Over-exposures (defined as exposure of at least one additional region apart from the region of interest) and babygrams (defined as exposure of at least two or more additional regions apart from the region of interest) constitute baby hazard opportunities, and the presence of extraneous adult fingers in images constitute caregiver hazard opportunities. The overall median was reported as 12.5 per week. The team aimed to reduce this by at least 75% within the project span of 6 months (figure 1).
Figure 1.
Radiation hazard opportunities: pre and post project implementation. PDSA, Plan Do Study Act.
Second, a limited radiation dosimeter study was done for 10 X-ray exposures at various incubator positions within the unit. The entrance skin dose (ESD) to the neonate receiving the radiograph and scatter radiation to the environment was measured. The data were gathered with an intention to identify scope for improvement in radiation dose and to measure scatter radiation in the neonatal unit (Tables 2,3).
Table 2.
Measurement of neonate’s radiation dose during mobile chest X-ray
| Unfors patient skin dosimeter | Neonate’s skin dose during chest X-ray (mGy) | Source to image distance (cm) | Exposure factors (kV/mAs) |
| 1 | 0.069 | 95 | 52/2.2 |
| 2 | 0.064 | 95 | 52/2.2 |
| 3 | 0.054 | 95 | 50/2.2 |
| 4 | 0.057 | 95 | 50/2.2 |
| 5 | 0.052 | 95 | 50/2.2 |
| 6 | 0.057 | 95 | 51/2.5 |
| 7 | 0.047 | 95 | 49/2.5 |
| 8 | 0.072 | 95 | 53/2.5 |
| 9 | 0.040 | 95 | 45/2.0 |
| 10 | 0.044 | 95 | 45/2.5 |
| Average skin dose (mGy) | 0.056 | ||
Unfors patient skin dosimeter was placed at the anterior of the left shoulder to measure the radiation dose during chest X-ray examination.
Table 3.
Measurement of scattered radiation using a 4 cm thick PMMA to simulate a neonate
| Mobile X-ray unit, Fuji GO | kV | mAs | SID | PMMA phantom (18×24 cm) | FOV |
| Exposure factors | 50 | 2.5 | 95 cm | 4 cm thick | 15×15 cm |
FOV, Field of view; PMMA, polymethylmethacrylate; SID, Source to image distance.
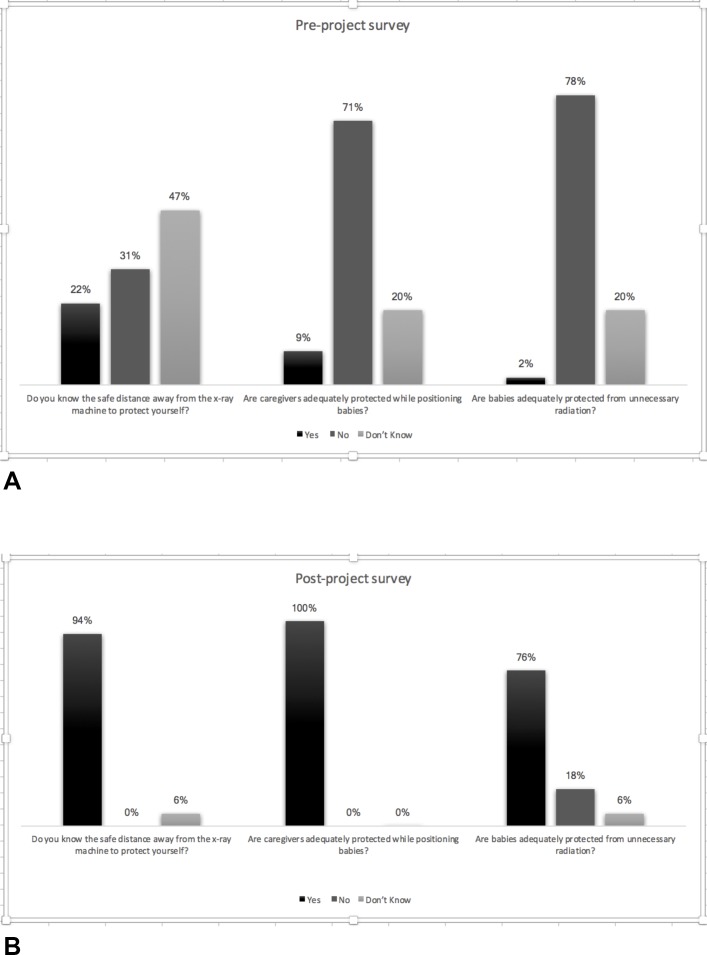
Third, a questionnaire on radiation safety concerns was given to a sample group of the healthcare team involved in the bedside imaging process. According to this survey, 78% of the participants agreed on the lack of adequate protection for the neonates and 71% on the lack of adequate protective gear for the nurses. Occupational hazard from radiation exposure was a great concern for 38% and some concern for 55% of those surveyed. Only 22% of the staff were aware of the recommended safe distance from the primary beam during exposure. An overwhelming 97% believed in the need to improve the bedside imaging process (figure 2A).
Figure 2.
Pre project and post-project survey.
Design
The task force with representatives from the radiology and the neonatal departments facilitated a safe platform for open and honest discussions about the existing radiation safety practices and the unique challenges faced in this high-intensity patient care unit. Thus the group was able to list out the numerous contributing factors that may influence the process outcome.
Guided by the Pareto principle, our efforts to optimise radiation safety in the unit consisted of four main aspects: staff protection, gonadal shielding for the neonates, scripting a standard protocol for the bedside radiological examination process, and enhancing staff awareness and education. Critical analysis of the existing process map and brainstorming for ideas helped to crystallise the effective solutions.
Staff protection
Immediate provision for a set of lead protective gear (lead apron, thyroid shield) for the nursing personnel, who may need to hold the neonate during the exposure, was made. This was well-received by the nursing staff and compliance was monitored by the team members present in the unit. Personal radiation protection gear empowered the nursing staff to position the neonates better. As our NICU has an open layout with incubators spaced from each other at variable distances, a portable lead wall was made available to protect adjacent incubators from the primary beam of lateral shoot through radiographs. It also facilitates the uninterrupted care for neonates undergoing procedures in close vicinity to the X-ray machine in time-sensitive situations.
Gonadal shielding for neonates
Gonadal shielding9 10 is a well-studied dose-reducing strategy among radiosensitive population groups. As this practice has never been explored in NICUs across Singapore, sourcing for a commercial product implied time and resource consumption beyond the scope of this project. To circumvent the hurdle, we designed an improvised version of a gonad shield by cutting a thin rubberised lead sheet into a rectangular piece that can be placed to cover the pelvis and lower limbs of the neonate for all radiographs except abdominal views. The nurses and radiographers were educated on the gender-appropriate method of usage of the gonad shield. It is to be placed inside a new plastic bag for each use in order to comply with the stringent infection control policy of the hospital.
Optimal collimation and positioning
The anatomical landmarks of collimation for the routinely ordered radiographs and guidelines on optimal positioning of the neonate were scripted down as a standard protocol for bedside imaging. Nurses and radiographers were encouraged to remind each other of the appropriate X-ray beam collimation and optimal positioning of the neonate for every imaging process. Visual reminders of the revised process map were placed at strategic places to raise awareness of the new quality requirements.
The practice of amending X-ray orders verbally to include a wider anatomy or get combined X-rays (a single chest/abdomen exposure) was strongly discouraged. The practitioners thus became part of the dose reduction effort by justifying every order for combined X-rays. There are numerous references in the literature to combined X-rays11 12 as reducing the radiation dose by a factor of 1.7 compared with performing separate chest and abdomen exposures. However, we insist that every combined X-ray request should be justified based on clinical necessity and not overused.
We believed in the need for a standardised policy for the bedside imaging process. A policy was scripted that explains the revised process map and provides clear instructions on all the key initiatives introduced by the project. It was uploaded in the ‘Intranet’, a hospital-wide electronic repository of policies for quick reference and user-based learning.
Staff awareness and education
We believed that empowering the nursing staff with adequate lead protective gear and radiation safety awareness will translate into increased adherence to the standard protocol in bedside imaging process and thereby ensure utmost patient safety.
Regular staff awareness and feedback sessions were held to address their concerns and achieve maximum compliance to the newly implemented quality improvement measures. Appropriate use of gonad shields and the optimal positioning of neonates were demonstrated with the help of manikins. Practical difficulties were voiced in restraining the hands of term neonates away from the primary X-ray beam while imaging. This contributed to a lingering presence of overexposure in chest radiographs, the most commonly done radiograph in NICU. Sand bags and physical restrainers were suggested to restrain the limbs away from the primary beam. The sand bag may also be used to maintain the head in the neutral midline position without the need for a staff to hold the baby.
Another issue that surfaced was the rotational posting of radiographers to the neonatal unit, who being oblivious to the newly implemented protocol may get into professional misunderstanding. Hence, orientation to the new standardised policy was made mandatory to every new staff (doctors, nurses and radiographers), thereby minimising operator-dependent deviations to the bedside imaging process.
The team members from the Department of Radiology presented the results of the radiation dosimetry to the entire healthcare team. The average background radiation in the neonatal unit was 0.33 µSv/hour, similar to natural background radiation in the environment. The scatter radiation doses at different distances from the isocentre as compared with the background radiation was explained with schematic diagrams. The average ESD in premature neonates was 56 μGy per chest radiograph,13 14 which is in par with international reference standards (tables 2, 3 and 4).
Table 4.
Scattered radiation measured at various distances using Unfors Xi Survey Meter
| Distance from centre of PMMA (cm) | Scattered radiation measured in μGy | Equivalent hours of background radiation (using natural background radiation of 3 mSv/year) |
| 30 | 0.227 | 0.663 |
| 50 | 0.106 | 0.309 |
| 100 | 0.029 | 0.085 |
| 200 | 0.007 | 0.020 |
PMMA, polymethylmethacrylate.
Knowledge of these objective measures of radiation safety and safe distance from secondary radiation exposure made a tremendous impact on staff morale and adherence to the revised standards of bedside imaging.
Results
The benefits of the project initiatives extend beyond the scope of objective measurements. The targets achieved are highlighted using the same methods used to quantify the existing problem.
The radiographs done throughout the 6 months’ period were analysed for baby and caregiver hazard opportunities as discussed earlier. By 6 months, the median for the total number of baby hazard opportunities decreased from 8 to 2, and the median for the total number of caregiver hazard opportunities decreased from 4 to 0, thereby reaching an overall reduction of 84% (figure 1).
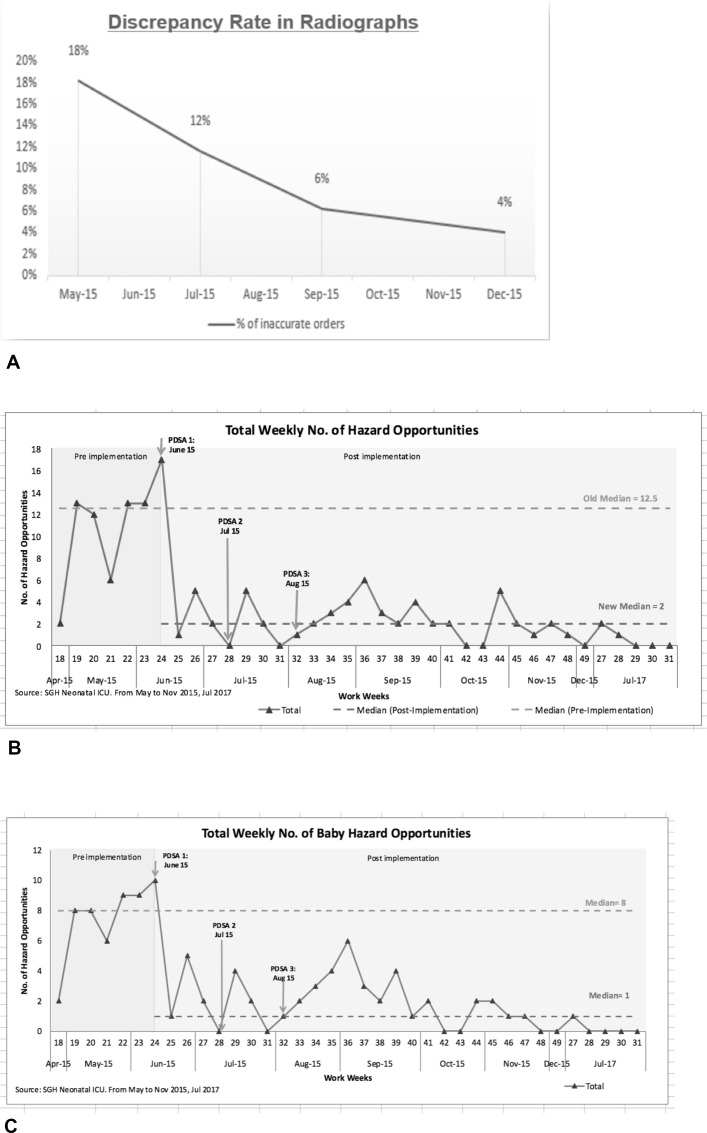
By means of increasing awareness and ensuring compliance to the newly implemented QI measures, we believed to see a decrease in the number of radiographs with discordance between the request form and the image. The rate of discordance decreased by 77% (18%–4%) within the 6-month period and stands as a surrogate marker for compliance to the project initiatives (figure 3A).
Figure 3.
Radiograph discrepancy rate. PDSA, Plan Do Study Act.
Follow-up survey results showed a remarkable change in the awareness and attitude of healthcare staff towards complying with the best standards of radiation safety. Nursing staff (100%) felt very confident and satisfied with the enhanced radiation safety practices and worried less (6%) about occupational radiation exposure or radiation to the vulnerable infants (18%), when they were resurveyed 2 months after the project was completed (figure 2B).
The intangible benefits are several.
The neonatal caregivers are better informed about the radiation safety measures and hence impart their valuable knowledge to the anxious parents.
The optimal positioning of neonate is given adequate importance by the radiographers and nurses, thereby maintaining good comparability between images.
The lead barrier wall allows the medical team to continue with the ongoing procedures in the intensive care unit, even when a neonate in the neighbouring cot requires a radiograph.
The parents feel reassured and confident in the care provided to their infants.
Lessons learnt
Overexposure was defined as inclusion of at least one adjacent body part apart from the region of interest in the primary radiation beam. This is a very stringent criterion to avoid in extremely small preterm infants (birth weight <750 g). The observed outliers were those done in such critically ill neonates receiving higher levels of intensive care. Neonates can be precariously labile and severely compromised by life-threatening conditions when they require frequent diagnostic imaging. And in such circumstances, radiographs done with minimal handling of infants to avoid further compromise in their clinical status is a fine balance within the ALARA principle.
Sustainability
The policy on bedside diagnostic imaging in neonates and the revised workfoware uploaded in the SGH electronic web portal to serve as a valuable resource material for all newly posted staff in the departments of neonatology and diagnostic radiology.
Regular monitoring of the imaging process and analysing the images taken, staff appreciation and feedback are part of a continuum to sustain the quality improvement in radiation safety practices.
Sustainability data was measured for a period of 4 weeks in 2017, 18 months after project completion. The median for total radiation hazard opportunities is well sustained and the median for baby hazard opportunities has reduced further from 2 to 1 (figure 3B,C).
Conclusions
‘Not everything that can be counted counts. Not everything that counts can be counted.’
Albert Einstein
Although the risk of radiation harm from any single radiograph is extremely low, it is worth remembering that many preterm infants may need computed tomography and fluoroscopy imaging within early infancy, the radiation dose of such maybe 1000 times a chest radiograph. The vulnerability to radiation harm may add to the long-term morbidities of prematurity and raise the risk of radiation-induced cancer over their lifetime. Hence judicious use of radiographic examinations in accordance with the ALARA principle is essential for ensuring utmost patient safety.
Acknowledgments
The team acknowledges the support extended by the Heads of the Department of Neonatology and Diagnostic Radiology, Singapore General Hospital, and the nursing department for their support and cooperation. The team is thankful to Service Operations, SGH for supporting the project.
Footnotes
Contributors: The authors were in the six-member QIP team involved hence in the design, study, brainstorming and implementation of the proposed initiatives. PE: project lead, involved in concept, design, data analysis, conducting radiation awareness sessions to the multidisciplinary team and scripted the department policy on bedside radiography in neonates and writing the manuscript. PSC: involved in data analysis, providing orientation of the QIP to nursing staff, monitoring compliance and conducting preproject and postproject survey, contributed to the run charts, and final approval of the manuscript. VAS: mentored the QIP and contributed to administrative details of the project and revised the critical content of the manuscript. SKS: provided expertise and literature search on radiation studies in neonatal units, and contributed to the radiation dosimetry study and relevant sections of the manuscript. GHT and LNL: conceptualised and conducted the radiation dosimetry study in the neonatal unit and played a role in enlisting the radiographers’ commitment to the QIP, compiled the dosimetry results and revised relevant sections in the manuscript.
Disclaimer: All the views expressed in this paper are reflective of the project team and are not the official statement of the institution.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Vachharajani A, Vachharajani NA, Najaf T. Neonatal radiation exposure. Neoreviews 2013;14:e190–e197. doi:10.1542/neo.14-4-e190 [Google Scholar]
- 2. Iyer NP, Baumann A, Rzeszotarski MS, et al. . Radiation exposure in extremely low birth weight infants during their neonatal intensive care unit stay. World J Pediatr 2013;9:175–8. doi:10.1007/s12519-013-0417-1 [DOI] [PubMed] [Google Scholar]
- 3. Datz H, Ben-Shlomo A, Bader D, et al. . The additional dose to radiosensitive organs caused by using under-collimated X-ray beams in neonatal intensive care radiography. Radiat Prot Dosimetry 2008;130:518–24. doi:10.1093/rpd/ncn090 [DOI] [PubMed] [Google Scholar]
- 4. Russell J, Burbridge BE, Duncan MD, et al. . Adult fingers visualized on neonatal intensive care unit chest radiographs: what you don’t see. Can Assoc Radiol J 2013;64:236–9. doi:10.1016/j.carj.2012.04.004 [DOI] [PubMed] [Google Scholar]
- 5. Duetting T, Foerste B, Knoch T, et al. . Radiation exposure during chest X-ray examinations in a premature intensive care unit: phantom studies. Pediatr Radiol 1999;29:158–62. doi:10.1007/s002470050562 [DOI] [PubMed] [Google Scholar]
- 6. Burrage JW, Rampant PL, Beeson BP. Scatter and transmission doses from several pediatric X-ray examinations in a nursery. Pediatr Radiol 2003;33:704–8. doi:10.1007/s00247-003-0999-1 [DOI] [PubMed] [Google Scholar]
- 7. The 2007 recommendations of the international commission on radiological protection. ICRP publication no. 103. Ann ICRP 2007;37:1–332. [DOI] [PubMed] [Google Scholar]
- 8. European guidelines on quality criteria for diagnostic radiography images in paediatrics. Report EUR 16261EN. Luxembourg. ftp://ftp.cordis.lu/pub/fp5-euratom/docs/eur16261.pdf (accessed 22 Jun 2017).
- 9. Haines GA, Hendry JH, Daniel CP, et al. . Germ cell and dose-dependent DNA damage measured by the comet assay in murine spermatozoaa after testicular X-irradiation. Biol Reprod 2002;67:854–61. doi:10.1095/biolreprod.102.004382 [DOI] [PubMed] [Google Scholar]
- 10. Barcham N, Egan I, Dowd SB. Gonadal protection methods in neonatal chest radiography. Radiol Technol 1997;69:157–61. [PubMed] [Google Scholar]
- 11. Yu CC. Radiation safety in the neonatal intensive care unit: too little or too much concern? Pediatr Neonatol 2010;51:311–9. doi:10.1016/S1875-9572(10)60061-7 [DOI] [PubMed] [Google Scholar]
- 12. Bahreyni Toossi MT, Malekzadeh M. Radiation dose to newborns in neonatal intensive care units. Iran J Radiol 2012;9:145–9. doi:10.5812/iranjradiol.8065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Malone J, Guleria R, Craven C, et al. . Justification of diagnostic medical exposures: some practical issues. Report of an international atomic energy agency consultation. Br J Radiol 2012;85:523–38. doi:10.1259/bjr/42893576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ono K, Akahane K, Aota T, et al. . Neonatal doses from X ray examinations by birth weight in a neonatal intensive care unit. Radiat Prot Dosimetry 2003;103:155–62. doi:10.1093/oxfordjournals.rpd.a006127 [DOI] [PubMed] [Google Scholar]