Abstract
Magnesium sulphate has been demonstrated to be an effective neuroprotectant for babies delivered prematurely (under 37 weeks’ gestational age). Antenatal administration reduces infant mortality and cerebral palsy (CP); however, uptake in the UK has been significantly lower than other countries. A quality improvement (QI) project (PReventing Cerebral palsy in Pre Term labour (PReCePT)) was carried out in the West of England, UK, to raise awareness of evidence and to improve the uptake of magnesium sulphate as neuroprotectant in preterm deliveries. Five National Health Service (NHS) Trusts and the West of England Academic Health Science Network participated in the QI project. The project was underpinned by a multifaceted QI approach that included: patient and clinical coproduction of resources; recruitment of clinical champions to support the local microsystems and create a stimulating/supporting environment for change; Plan, Do, Study, Act cycles; training for over 600 NHS staff and awareness raising and strategic influencing of key leaders. A baseline audit and regular measurement of the number of eligible women receiving magnesium sulphate was undertaken at each hospital site, and the overall programme was evaluated using data from an international benchmarking organisation for neonatal care outcomes—the Vermont Oxford Network. During the project 664 staff received magnesium sulphate training. The use of magnesium sulphate increased across the West of England from an average baseline of 21% over the 2 years preceding the project to 88% by the conclusion of the project. The project was also able to influence the development of a national data collection process for benchmarking the use of magnesium sulphate for neuroprotection in preterm deliveries in the U.K. PReCePT appears to have had a favourable effect on the uptake of magnesium sulphate across the West of England. The project has also provided learning about how to stimulate adoption and spread of evidence using a QI approach across a network.
Keywords: obstetrics and gynecology, quality improvement methodologies, shared decision making, team training, quality measurement
Problem
Cerebral palsy (CP) is a significant consequence of preterm birth.1 Within the West of England, approximately 500 infants are born weighing less than 1500 g each year.2 These babies are eligible for antenatal magnesium sulphate, which has been proven to reduce the rate of CP.1 Before the inception of this project, only between 8% and 66% of eligible infants were receiving this treatment across the five sites,2 potentially resulting in disability that could have been prevented. Significant variation in operational practice was identified both within and between the sites, and we discovered that even where a policy existed that highlighted the need to give antenatal magnesium sulphate, it was not consistently being administered, and a large number of staff and parents were unaware of the need to offer this treatment, often confusing it with the treatment for pre-eclampsia.
The West of England Academic Health Science Network is a membership organisation made up of NHS health and social care providers, clinical commissioning groups, universities and the South West Ambulance Service. It acts to coordinate projects across the member organisations to improve quality and patient safety and speed up the adoption of evidence into practice.
‘PReCePT’ was codesigned with a range of partners in response to a call asking for local examples of best practice that could be shared with our member organisations and which would benefit from a QI approach to implementation and spread.
Dr Karen Luyt, MBChB, PhD, FRCPCH (Consultant in Neonatal Medicine and Consultant Senior Lecturer Neonatal Neuroscience, University of Bristol), submitted a proposal to share the progress that had been made in University Hospitals Bristol NHS Foundation Trust in the use of magnesium sulphate for neuroprotection in preterm babies with the maternity unit at Gloucestershire Hospitals NHS Foundation Trust.
A panel of peers reviewed the proposal and felt that it should be supported as the project was specific, measureable and could be delivered within a relatively short timescale. The panel also felt that it could aid understanding of how best to support our member organisations put evidence into practice and deliver cultural change.
The ‘PReCePT’ project’s main aims were to:
focus on the needs of patients and the local population by increasing the numbers of eligible women offered and receiving treatment in the West of England to 60% within the project timeline
train core staff to understand the benefits of using magnesium sulphate for neuroprotection
support system change in the five NHS Trusts to embed this practice as ‘business as usual’
find a sustainable long-term measurement system to enable continuous improvement.
Other longitudinal aims, beyond the scope of the QI project were to:
improve the long-term neurodevelopmental outcomes of babies born at 30 weeks’ gestation or less and reduce the incidence of CP in the West of England.
We aimed to do this within a 6-month time period.
Background
Premature birth, where delivery occurs before 37 weeks’ gestation, is associated with reduced survival and increased rate of life-altering complications, including physical disability, blindness, deafness and cognitive impairment,5compared with full term birth. Progress in perinatal care over the past three decades has led to greater survival rates for infants born prematurely6; however the rate of disability in survivors remains high, with 14% of children delivered at less than 27 weeks’ completed gestation having CP in one nationwide UK study.7 In 2014, 10,781 babies born at less than 33 weeks’ completed gestation were admitted to neonatal units in England, Scotland and Wales.8 The incidence of CP in infants of these gestations is approximately 98.8 per 1000 live births in the UK,9 equating to an estimated 1065 new cases of CP secondary to prematurity per year.
While this figure is small, the human impact of CP is unquantifiable for individuals and families. CP can lead to significant life-long issues far in excess of the physical difficulties encountered.9 Financially, however, it is estimated that the lifetime cost per patient with CP, including healthcare, productivity and social costs, is in the region of €860 000 for men and €800 000 for women.3 In addition to this, there were 188 claims for CP/brain injury to the NHS litigation authority in 2015/2016 totalling £989.7 million,4 although this also includes babies born at full term and post-term.
While antenatal steroids10 and surfactant therapy11 have contributed significantly to increased survival rates for preterm babies, fewer interventions have specifically improved neurodevelopmental outcome. In meta-analysis, magnesium sulphate given prenatally to women at risk of preterm birth significantly reduced the risk of CP in their child (relative risk 0.68; 95% CI 0.54 to 0.87; five trials; 6145 infants).1 Furthermore, the therapeutic number of women needed to be treated to prevent one case of CP is lower at earlier gestations, 46:1 (95% CI 26 to 187) at less than 30 weeks, increasing to 56:1(95% CI 34 to 164) before 32–34 weeks of gestation.12
Despite these results and international recommendation,13–15 uptake of magnesium sulphate for neuroprotection has been slow to develop in the UK. In 2012, only 9% of 1251 eligible UK deliveries (22–29+6 weeks’ gestation) recorded in the Vermont Oxford Network (VON) database received antenatal magnesium sulphate, with only 5% of infants delivered at 28 weeks receiving the treatment.2 In 2012, there were 8045 infants born at <1500 g in England and Wales.16 Extrapolating the data for VON to the national population, this results in a potential 159 preventable cases of CP in 1 year alone. In contrast, in 2012 across VON (1048 units, 70.8% within the USA) 45.8% of infants in the same category were treated with magnesium sulphate, including 44.9% of infants at 28 weeks.2 Uptake of magnesium sulphate in the UK has been increasing, with 24% of 1200 infants in VON receiving antenatal treatment in 2013.17 However, when the project was started in 2014, it was estimated if the rate of increase in uptake remained constant (15% per year) it would take at least a further 4 years to reach the target uptake of 90% where it stands for antenatal steroids. Furthermore, variability in practice between UK units is striking with the lowest quartile of units in the UK having 3.8% or lower uptake and the upper quartile of units having almost 10-fold higher rates.17
In order to expedite the uptake of magnesium sulphate and therefore improve neonatal outcomes, efforts are required to raise awareness of the body of evidence for practice change with clinicians (particularly midwives, obstetricians and neonatologists), parents, operational managers and chief executives.
‘PReCePT’ was designed to embed this evidence-based intervention into routine NHS obstetric practice to conclude the final stage of translational research.
‘PReCePT’ was carried out in five NHS Trusts in the West of England. This study evaluates the impact of this QI intervention in terms of uptake rates across participating Trusts.
The five Trusts were:
Gloucestershire Royal Hospital (Gloucester Hospital NHS Foundation Trust)
Royal United Hospital (Bath NHS Foundation Trust)
St Michael’s Hospital (University Hospitals Bristol NHS Foundation Trust)
Southmead Hospital (North Bristol Trust)
Swindon Hospital (Great Western Hospitals NHS Foundation Trust).
Baseline measurement
The baseline for this project was measured by the research midwives in two ways: through accessing the five NHS Trusts individual submissions to VON and from a local case note audit in each trust of the preceding 2 years of data (2012 and 2013). The five Trusts participating in ‘PReCePT’ are all members of VON.
In addition, a research midwife in each Trust undertook a thorough case note audit of the historical use of magnesium sulphate for babies delivered at 30 weeks or less, covering a 2-year period prior to the commencement of the project. The reason for using case notes was to see if there was any documentation about why magnesium sulphate was or was not given, as some contraindications for the treatment exist. The baseline therefore included how many babies had been delivered at 30 weeks by each Trust and of those how many mothers would have been eligible for antenatal magnesium sulphate infusions and to ascertain whether this treatment was:
offered and accepted
offered and refused
not offered
not offered because of documented contraindications.
The National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care West (NIHR CLAHRC West) study then obtained central permission from VON to use the data from each site. This allowed a deeper statistical analysis of relevant data from women admitted/babies delivered between 1 January 2012 and 31 December 2013 from the registry for analysis. This included gestational age, year of birth, use of magnesium sulphate, birth weight, multiple births and maternal data. All data (patients and sites) were anonymised in order to avoid identification of individual patients/sites.
The data were analysed to see if there were any discernible patterns to usage, for instance variation by clinician, between emergency presentation compared with planned birth or between Trust. The data were also cross-referenced to check that the numbers from the case notes aligned to the data submitted to VON, in order to check whether any data processing errors existed. The results of this quantitative data from NIHR CLAHRC West also allowed validation/cross-checking with the Badgernet data. The results from this study are in press.
The research midwife data showed significant variation in practice with one site administering to only 8% of women (below the 12% UK national average) with the best administering to 66% of women.
In addition to variation across the sites, we identified clear patterns in variation within sites between gestational age, singleton/multiple birth and diagnosis of hypertension in mother and also between emergency presentation compared with planned birth. Our working hypotheses were that:
that not all clinicians knew when to offer the treatment, and if it was appropriate in complex presentations: highlighting a knowledge mobilisation issue
that in emergency presentations there may not always been time to administer the full dose, and clinicians might not be aware of the benefits of administering the loading dose.
Design
Exploratory phase
The initial design of the project was codesigned by a core QI team comprised of obstetricians, neonatologists, midwives, QI coaches and parents (supported by the charity Bliss).18 This team included staff from the ‘originating’ team who had led the improvement in Bristol and the ‘adopting’ team from Gloucestershire.
The first task was to collect baseline information about current practice in the use of magnesium sulphate for neuroprotection. It was agreed that the most effective way to measure the success of this project was to use quantitative data that were already being routinely collected for VON, which included monthly uploads of data about premature births, including whether magnesium sulpate had been administered. Having found that the local data were well below the rates of equivalent Western health systems in the USA and Australia, the team then agreed that there was a strong need to work together to codesign a range of products that could be used to help train and raise awareness in health staff, inform parents and make the case for change.
These exploratory findings were shared with the West of England Academic Health Science Network’s Board, and several of the local hospitals’ chief executive officers agreed that the project should be supported and an executive sponsor of the project was selected.
The QI team’s initial vision was to design the programme to include three further phases.
design: to help understand and diagnose the current systems and processes, understand the current variation, model the likely impact of the intervention and articulate the case for change
testing: to test the ideas, concepts and products from the design phase in the complex setting of an NHS maternity unit
evaluation, dissemination and spread: to share results locally and nationally.
Design phase
The design phase aimed to:
articulate and communicate the project’s aim and build a shared purpose
understand the patient population’s needs from patient and clinical perspectives and by learning from the lived experience of public contributors
agree the target patient group and subgroups
understand the current systems and processes in place in each of the five maternity units
identify the professional groups whose behaviour we were seeking to influence
understand the current demand for this treatment and model the likely impact of our intervention in terms of clinical effectiveness, patient experience and cost.
We originally thought this phase would take 3 months.
Testing phase
The original intention was to support Gloucestershire Hospitals NHS Trust to use the Institute of Healthcare Improvement (IHI) model to undertake Plan, Do, Study, Act (PDSA) cycles to test and refine the ideas, concepts and products from the design phase with the aim of fully embedding a practice change.
We originally anticipated that this might take several PDSA cycle ramps to complete, including:
communication of shared purpose
staff knowledge mobilisation
patient knowledge mobilisation
behaviour change
measurement
system change.
We anticipated this would take 3–6 months to complete.
Evaluation, dissemination and spread
The group anticipated that once this process had been designed and tested in Gloucestershire and we had made a case for sustainable change, we would then be able to share the resources that had been developed locally to the other three maternity units in the area. Any learning from this group process could then be shared via clinical networks and nationally.
The group felt that the overall design of the programme would be an effective way of spreading best practice from one hospital site to another as it would allow scrutiny of what had worked well and what could have been improved, supporting the iterative process of adoption in other sites.
Strategy
The project drew on the following quality improvement (QI) methodologies:
The Model for Improvement (Institute of Healthcare Improvement)19
Coproduction and Experienced-Based Co-Design20
microsystems 5Ps approach (purpose, patients, people, process and patterns)21
Design phase
The QI team began the design phase in Spring 2014. Using a coproduction approach22 with parents with lived experience of preterm birth, the neonatal charity ‘Bliss’, professionals and other key stakeholders, the team began to articulate and communicate the project’s aim and build a shared purpose. The team used elements of the Experience-Based Co-Design toolkit20 and through iterative design cycles produced several draft products ready for testing.
These included:
- Clinical tools and prompts:
- a clinical care pathway with standardised auditable checklist
- a proforma for patient notes to make recording as easy as possible.
- Clinical and patient information:
- communication materials to outline the case for practice change, designed by clinicians for clinicians
- a patient information leaflet designed by parents with lived experience of preterm birth in conjunction with the charity ‘Bliss’ to explain the need for the treatment, the potential positive outcomes and the likely side effects for mothers while in labour when the magnesium sulphate is given.
- an infographic outlining the case for change nationally (UK) and in our local area (West of England)
- a recognisable name and brand for the programme
- a range of promotional collateral to help market the project (pens, magnets for booking-in boards, lanyards with the key pathway steps on them).
- Training approach:
- clinicians designed a training pack that could be adapted to suit each site and for different clinical audiences
- a ‘train the trainer’ programme was devised to cascade the training.
- digital tablet devices were procured to enable ‘agile’ training opportunities.
- QI approaches:
- a detailed implementation plan
- a measurement strategy
- an evaluation strategy.
- Operational delivery mechanisms:
- contracts to provide financial support to the Trusts to allow research midwives to be released to lead the project, undertake a baseline assessment, deliver the training and promote the project emerged from this codesign process
- governance structures
- executive sponsorship
- regular programme meetings with research midwives were established.
We originally thought this phase would take 3 months; in reality, it took 4 months to complete as the number of Trusts that wanted to take part in the programme increased. At the end of the design phase, the QI team had originally planned to hold a learning event for key clinicians, operational managers and patients from Gloucestershire and then work with Gloucester Hospital NHS Foundation Trust to help develop a series of PDSA cycles to test and refine the products. However, an unexpected opportunity allowed us to present the case for change and the draft products in front of a wider clinical audience at the South West Obstetrics Network (SWON).
This event inspired all five maternity units in the West of England to work together and try to adopt the practice in parallel, rather than wait to test in one location first. All the units could see the benefit of the approach and could not see any advantage in waiting to be included in the project. The scope of the project therefore expanded from two to five maternity units. While staff from the original cohort had been fully involved in the codesigned development phase, the three other units were recruited at speed, and local adaptations to the products were then completed and procured rapidly within a 6-week time frame.
In order to speed up adoption, we found funding to ring-fence some time for research midwives to become the ‘clinical champions’ for the project. We calculated that to complete the baseline audit, roll out training, act as an ambassador for the project and measure the ongoing uptake of magnesium sulphate, we would require 90 hours of time. To support this, we engaged with chief executives of all the hospitals and asked for their active leadership to help facilitate the programme. This senior leadership support was vital for the success and speed of the project.
Following baseline assessment from VON data and case note audit two phases of PDSA cycles were completed.
Testing phase
The testing phase of the project was split into two tranches, commencing on 1 August 2014 and 1 October 2014, respectively. The end of this phase was scheduled on 31 March 2015 for both tranches. The research midwives formed a temporary regional QI team and met regularly together through this period. They were very experienced practitioners with a keen interest in evidence and data and a track record of being involved in research. On a personal level, they were articulate and skilful communicators, passionate about making a difference for patients and understood their local microsystems in detail. For some, it was the first time they had used formal QI methodologies and so training on the IHI Model of Improvement19 was given and QI coaching was provided throughout.
Implementation phase 1
The ‘PReCePT’ care bundle was introduced across all sites using the codesigned materials.
Each of the five maternity units undertook to collect outcome data and some process measures in the same way using a shared measurement system. Each was provided with the initial draft resources developed by the design group and asked to undertake a rapid series of PDSA ramps to test their usefulness in practice.
This included a draft:
clinical proforma
patient leaflet
training materials
outline training method
infographic outlining the case for change
a visual way of displaying improvement over time
ideas on implementation methods.
This was followed by email, face-to-face and telephone QI coaching and two reflective meetings with the research midwives to share their learning about what had worked and what had not suited their local microsystem.
Implementation phase two and onwards
The ‘PReCePT’ care bundle was adapted for local conditions.
Inevitably, some of the products in the design phase needed to be adapted to meet local conditions. We found that what emerged during the testing phase was a model that supported each unit to align to a common set of measures, metrics and aims but which allowed each site to create bespoke approach to fit the needs of their local microsystem. Each research midwife then designed and tested changes to ensure the care bundle met the needs of their local system. In addition to changes to the initial design, some of the midwives innovated new products, services or processes, which were then tested for effectiveness. Table 1 gives examples of some of the key local PDSA tests of change in the individual units and the three overarching themes that emerged.
Table 1.
Local PReCePT PDSA cycles
| Theme | What situation was observed? | What change was tested? | Was this change successful, and was it evidenced? |
| Awareness raising and promotion | Midwives on the unit were not routinely aware of which mothers were eligible for the intervention. | A set of stickers depicting the project logo were developed and attached to relevant sets of notes on admission. | Each mother with the sticker on the notes received the intervention. It also had the unintended consequence of making notes easier to find for the purpose of continually monitoring uptake and providing performance feedback to unit staff. |
| Awareness raising and promotion | Based on previous experience on the unit, it was known that simple and accessible protocols aided uptake of new practice and promoted consistency in administration. | The lead midwife asked the intended audience what they would find helpful as an aide memoire. As a result, credit card-sized cards depicting the clinical protocol were designed to be attached to identification lanyards already worn by clinical staff. | During project implementation, staff were observed referring to the cards on a daily basis. When the test batch was depleted, unit staff requested additional stock and suggested amendments and improvements for subsequent iterations. This was the most successful of all the materials in promoting awareness among staff in this unit. |
| Awareness raising and promotion | The original PReCePT patient leaflets were tested and found to be suitable for those women who were expected to encounter a preterm birth and could be given them in advance. However, the leaflets were found to be too long for use by mothers in a stressful emergency premature labour. | The unit lead developed an A5 leaflet containing just the key points for mothers in emergency labour. | Direct feedback from patients in this unit was not evaluated in real time, as the leaflet was used at a highly stressful moment in labour. However, unit staff requested more leaflets when the initial stock was depleted, indicating the countermeasure was valued by staff through use and feedback from women after birthsaid they had valued it. |
| Equipment and environment | The clinical supplies needed to support administration were stored in separate locations and required additional time to collate in a time-critical situation. | A brightly coloured and clearly marked ‘PReCePT’ box was created containing all necessary materials and stored in a prominent position behind the nurses’ station. | Unit staff were observed to use the box and request that other staff do so when admitting patients. Also, unit staff commented directly to the project lead on its ease of use and visibility. |
| Training and knowledge mobilisation | Difficulties were noted in accessing some staff groups for training either due to time constraints or because of rostering conflicts (particularly night staff). | The training presentation was sent out to staff by email, with the request for automatic confirmation of the email being opened and understood by the recipient being included. | Numbers of staff opening the email was tracked, with 52 staff members in a single unit using the automated response function. Furthermore, the unit’s project lead did not note any variation in uptake between day and night shifts. In another unit the research midwife spent several night shifts educating staff through a ’micro-training' approach. |
| Training and knowledge mobilisation | Difficulties were noted in accessing some staff groups for training through traditional mechanisms (such as large scale training sessions). | The project midwife adapted the first iteration of the training presentation to suit a 7-inch tablet screen. This was then used to support opportunistic ‘micro training’ sessions (with as few as a single participant) that could be completed to suit the ebb and flow of clinical demands on the ward. | The rate of numbers trained increased following the introduction of a ‘micro training’ approach. This approach was used in addition to existing, larger scale training opportunities. It also helped to train people on night shifts, when traditional training sessions are not available. |
| Training and knowledge mobilisation | The numbers of staff initially targeted for phase 1 of the training was too large to be manageable within the constraints of the project. | A review of the staff group was undertaken to find those most able to influence uptake. Efforts were then directed to ensuring that these key staff received the relevant training and could cascade. | The trend of missed opportunities for giving the intervention was towards zero during the project timeframe, and there were no missed opportunities during the whole of 2015/2016 (after the conclusion of the project). |
PDSA, Plan, Do, Study, Act; PReCePT, PReventing Cerebral palsy in Pre Term labour.
By the end of the testing phase, the data confirmed that some of the products that had been created in the design phase were being used by all five units with no change, some had needed further refinement to meet the individual units’ needs and, in addition, new change ideas had generated helpful innovations that it was then possible to spread from one site to another (table 1).
At the end of the testing phase, a final ‘lessons learnt’ meeting captured what had gone well and what they would have done differently with hindsight. Overall, the research midwives felt that they had achieved the aim to have embedded the project as ‘business as usual’ in each maternity unit’s operational system and to have trained enough staff to change the custom and practice of the use of magnesium sulphate. The main challenge identified by the research midwives had been the 3-month time frame that had been particularly challenging for those units that had volunteered to join the project after the SWON event. In hindsight it would have been better to have given these teams more time to prepare.
Measurement systems had been embedded that would allow ongoing monitoring and a continuous QI process, which the West of England Academic Health Science Network agreed to continue to monitor for 2 years after the project formally finished.
Evaluation, dissemination and spread
The West of England Academic Health Science Network commissioned an external qualitative evaluation of the project to consider how the local maternity teams felt about the effectiveness of the QI project, with a particular emphasis on how to capture any lessons learnt with regards to the project’s design, implementation and potential future replication in other Trusts.
This qualitative evaluation was undertaken using a realistic evaluation framework that used mixed method qualitative focus groups, surveys and quantitative data capture. The aim of the evaluation was to consider the experiences of staff across all five hospitals in which the project was conducted in order to better understand effectiveness and learn lessons to improve the quality of the project. Frequent evaluation at key points in the project’s lifecycle is a key component of QI science as it allows the project team to learn lessons, make any changes that are needed to the project plan and then run further PDSA cycles using the Model for Improvement. The evaluation report looked particularly at the following areas:
communication regarding the project
delivery of training
the use of midwives for project delivery
perceived impact on level of knowledge around magnesium sulphate for neuroprotection
the quality of the materials from the design phase.
Once the evaluation was completed, the project results were disseminated across the five maternity units and reported into their local governance structures. In addition, the results were shared at SWON and at national and international conferences.
The project highlighted the need to update the UK’s national audit tool (Badgernet, http://www.clevermed.com/badgernet/badgernet-neonatal/) to include the use of magnesium sulphate for neuroprotection in preterm birth to allow a UK audit of practice. This change has now been implemented, and the intervention has also been included in recent National Institute for Health and Care Excellence guidance.23
Results
The first aim of the ‘PReCePT’ project was to focus on the needs of patients and the local population by increasing the numbers of eligible women offered and receiving magnesium sulphate in preterm labour in the West of England to 60% within the project timeline.
Each of the five sites improved the rate at which magnesium sulphate was administered for preterm birth during the project timeline. A total of 82 eligible preterm deliveries occurred within the project timeline and of these 72 eligible births received the magnesium sulphate intervention, equating to 88% of eligible births. There was variation across the five sites, with some sites ensuring that every eligible woman was given the dose, but all units overachieved against the original ambition of 60% (table 2 and table 3).
Table 2.
Cumulative percentages of eligible women receiving magnesium sulphate (November 2014–February 2015)
| Nov 14 | Dec 14 | Jan 15 | Feb15 | Cumulative Total | |
| Unit A | 100 | 100 | 100 | 100 | 100 |
| Unit B | 75 | 80 | 80 | 81 | 81 |
| Unit C | 100 | 92 | 94 | 91 | 91 |
| Unit D | 100 | 100 | 100 | 89 | 89 |
| Unit E | 100 | 100 | 100 | 90 | 90 |
Table 3.
Cumulative percentages of eligible women receiving magnesium sulphate (November 2014 –February 2015): eligible and received
| November 14 | December 14 | January 15 | February 15 | Totals | |||||||||||
| Eligible | Received | % | Eligible | Received | % | Eligible | Received | % | Eligible | Received | % | Eligible | Received | % | |
| Unit A | 3 | 3 | 100 | 0 | 0 | N/A | 1 | 1 | 100 | 0 | 0 | N/A | 6 | 100 | |
| Unit B | 4 | 3 | 75 | 1 | 1 | 100 | 5 | 4 | 80 | 1 | 1 | 100 | 16 | 12 | 75 |
| Unit C | 6 | 6 | 100 | 7 | 6 | 86 | 4 | 4 | 100 | 6 | 5 | 83 | 37 | 34 | 92 |
| Unit D | 1 | 1 | 100 | 2 | 2 | 100 | 3 | 3 | 100 | 3 | 2 | 66 | 12 | 10 | 83 |
| Unit E | 2 | 2 | 100 | 5 | 5 | 100 | 2 | 2 | 100 | 2 | 1 | 50 | 11 | 10 | 91 |
Overall, of the 82 eligible births since the commencement of the project, 72 have received the recommended intervention, an overall compliance of 88%.
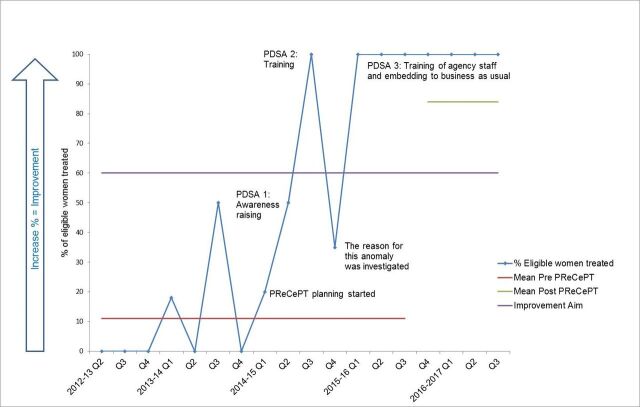
For example in one site, the run chart (figure 1) shows how the team started PDSA 1 with awareness training about the ‘PReCePT’ care bundle and marketing, followed by training permanent staff and then identifying a need to ensure locum, student and agency staff also knew what to do. They also found ways to embed this work into policy and practice and we can see from longitudinal data and subsequent submissions to the national Badgernet database (tables 2 and 3) that this has been maintained over time.
Figure 1.
An example of local data collection to support Plan, Do, Study, Act (PDSA) cycles from one of the PReCePT sites. % of eligible women treated by PReCePT.
Measurement of the outcomes is subject to considerable monthly variation because of the low numbers of preterm births in smaller units. The local run charts in each of the five sites enabled the teams to identify when a dose had not been administered and then find out why. Some common themes about missed doses emerged across the five units. These included:
emergency presentation preventing time for loading dose
confusion among untrained staff about who should give the loading dose and when
human error.
Patient choice
The continuous improvement approach allowed each team to learn from a missed dose and try new tests of change to improve system reliability, moving to measurement systems that noted the days between a missed dose. The impact of the programme therefore went beyond its end date and the majority of teams continued to improve outcomes.
The second aim of the project was to train core staff to understand the benefits of using magnesium sulphate for neuroprotection. The five sites identified 584 core staff that needed to be trained and overachieved, training 664 people between September 2014 and March 2015. A survey of 76 of the clinicians attending the training demonstrated that 96% found the training to have been of a high quality, stating it was clear and concise, easy to understand and contained a good range of information that was easy to remember. Four per cent said that it could have been improved by having more detail on how the magnesium sulphate worked and would have liked more time spent discussing the background evidence. Following the training, 89% reported that they would feel highly confident at putting the learning into practice and now had the skills to implement the required changes. Eight per cent felt they needed more support, and three per cent did not respond to this question.
The evaluation focus groups highlighted that different staff groups appeared to want a slightly different emphasis in the training. The medics reported that they liked an emphasis on the evidence base, whereas the midwives reported that they liked to know about the practical elements of the intervention, for example, when the loading dose should be given and by whom. All staff groups reported that they found it very powerful to hear the training message about why magnesium sulphate was given as a neuroprotectant and the impact that a change in their practice could have on a child and their family. The focus groups also revealed that finding the time to do such widespread training had been difficult. Many of the innovations the research midwives led concentrated on how to deliver the training as quickly and efficiently as possible. The teams also all learnt to incentivise the training and find ways to make it visible within the microsystem that someone had completed their training (eg, by giving out a badge, lanyard or pen to those that completed it). All sites emphasised how important it had been to have local champions to spread this training and described how the research midwives’ passion for the project was ‘infectious’ and helped to spread the learning.
The third aim was to support system change in the five NHS Trusts to embed this practice as ‘business as usual’. All sites stated they had achieved this, and the ongoing measurement of the numbers of eligible women suggests that this is the case. Some of the participating Trusts that had not achieved system reliability with 100% of eligible women being offered this intervention during the project period have continued to improve and have now achieved this ambition.
The fourth aim was to find a sustainable long-term measurement system to enable continuous improvement. This has been achieved through influencing the addition of the use of magnesium sulphate to the UK’s national audit tool.24
Lessons and limitations
The five maternity units that took part in the programme overachieved against the original target in a very challenging time scale and in the complex, fast paced and resource stretched environment of UK NHS hospital Trusts.
Based on the collective findings across the five organisations, the main lessons and limitations were:
The flexible approach to training and implementation allowed adaptation of the project to suit each hospital, while keeping a consistent strategic approach to the primary aim to increase uptake of magnesium sulphate and the use of standard measures across the community of practice to measure progress. The flexibility of this local ‘bottom-up’ approach to development was perceived to increase ‘ownership’ of the project and helped with staff engagement and ‘buy-in’.
All felt that the use of infographics, posters and marketing collateral was key to raising the awareness of the project; the time invested during the design phase to develop these had actively helped to create a collective vision about the case for change.
The involvement of people with lived experience of preterm birth in the codesign of the project was extremely beneficial. A coproduction approach was used throughout and parents helped to articulate the need for change, cocreate the materials in the design phase, hold the quality teams to account for progress, help to design the programme and present and disseminate the results.
A visual data management system is helpful when giving feedback to the teams on the progress of the project. This could take the form of a ‘5Ps’ poster,21 the use of a ‘big room’25 or by having a site-specific ‘PReCePT’ poster showing the baseline, the current achievement level and the ambition of the project.
It was critically important that people felt that they could improve on the products created in the design phase and optimise them for their particular microsystem. The encouragement of an experimental culture led to many sites innovating new approaches and taking the project forward in ways that could not have been anticipated at the onset of the work. A good example of this was the development of the ‘PReCePT’ box, where all the required information and resources were readied ahead of time, so that in the rush of an unexpected preterm delivery, where the administration of the magnesium sulphate was time critical, valuable minutes were not lost searching for all the separate components for care. This was felt to have increased the likelihood of the intervention being given.
The patient leaflet was well received for those mothers who had a history of preterm birth or who were identified as at high risk of preterm delivery but who were not in active labour. However, testing revealed that the leaflet was too long for those women who presented in active labour. One site took the core messages from the original leaflet and made a shorter, more concise version detailing the benefits and side effects of magnesium sulphate.
A range of training packages and methods of training delivery were used. Some sites took a formal classroom-based approach, whereas others used digital solutions. The training materials were also adapted to suit the specific learning needs of differing staff (such as doctors, midwives and supporting staff). It was proposed it might be best to identify two training leads (one for the night and one for the day shift). Using the local knowledge of the research midwives about what would work and fit into the local culture was key to the success of the training.
A lead-in time of at least 3 months to allow for sufficient planning and preparation was suggested, as the sites that opted to join the project ahead of schedule experienced significant time pressure in meeting project requirements and releasing midwife capacity to support the project. This meant that some did not get the protected time that had been planned for and instead had to continue to deliver ‘PReCePT’ as well as existing duties. Ideally, there should be adequate time for recruiting and training of key staff prior to implementation.
Careful thought should be given to the skills, knowledge and capabilities required to be a ‘PReCePT’ ‘clinical champion’. Core skills included: being able to deliver training, communicate to a range of staff groups, lead change, organise and collect data, run PDSA cycles, help innovate new ideas and know how to embed and sustain systems to support continuous QI. The focus groups also showed just how important the research midwives’ personal qualities and leadership skills were to the success of the project, using their enthusiasm to drive forward change and to remind staff why they were making this change by keeping the longer term impact of their immediate actions on a child’s life alive in the team’s mind. The infographics and photos also helped to get this message across.
Consistent guidance is required for each site to determine which staff can give magnesium sulphate to prevent delays and confusion.
Greater clarity at each site about when to begin the loading and full dose of magnesium sulphate and a better explanation about potential side effects for women in labour and the evidence base would improve staff knowledge.
Consideration should be given to strategies for training staff that have limited time available to help guide project leads delivering training. This could include guidance on cascade training or encouraging use of project champions. The use of digital technology such as tablet computers to allow on site and ‘tea trolley’ training was found to be very helpful across all five sites.
PReCePT is a clear example of how at a regional level in England an Academic Health Science Network can enable cross-system working and support different organisations to work together to deliver against a common vision for improvement to get evidence into practice. In addition, the 15 Academic Health Science Networks across England have the collective capability and capacity to act as vehicles for national adoption and spread of local improvement work to help improve patient outcomes and increase the cost-effectiveness of the initial design process.
The limitations of the project include the small number of participating sites (n=5), the 6-month duration of the QI project and relatively low numbers of births (n=89).
Conclusion
The evidence suggests that the ‘PReCePT’ project had a positive effect on both knowledge mobilisation and practice within the five maternity unitss. For midwives in particular, there was an improved awareness of the reasons for using magnesium sulphate in births at 30 weeks or less to help reduce the rate of CP in children. While some of the consultants and registrars may have already been armed with this knowledge prior to the project, it appears that the proactive nature of the campaign had greatly increased the incidence of administration of the drug. This project highlights the key role that midwives play in implementing evidence-based perinatal interventions.
Our background research identified that the problem with low rates of magnesium sulphate provision in anticipated preterm delivery is pervasive throughout the UK and internationally. The need for additional resources to expedite use into routine antenatal care has been recognised; however, little has been published on what this should involve or how to implement it. A binational, centrally funded QI programme is ongoing in Australia and New Zealand,26 providing educational materials and prompts to maternity hospitals in order to increase awareness of the national magnesium sulphate guideline. This has shown an increase in the rate of uptake of magnesium sulphate since the inception of the project,27 and the main findings are expected soon. Work from this group has identified that ‘knowledge and skills’ are enablers to uptake, as were reminders, prompts and influential colleagues,28 as seen in our project. The universal and international nature of the magnesium sulphate recommendation makes our project generalisable, and the persistently elevated rate of uptake in all units implies that our project is sustainable. The lessons learnt from our PDSA cycles, and the improvements to the materials produced, are applicable to units throughout the UK and beyond, and we suggest could be replicated in other healthcare settings for different health conditions.
Having a project lead at each site ensured that training reached as many staff as possible and that the message was spread to core staff and to those who may come into contact with patients who might benefit from magnesium sulphate. Use of training aids and visual prompts helped promote interest in the project and improve knowledge and understanding around the key messages. The flexibility for each site to run the project in a way that suited their hospital appeared to be important in developing a sense of ownership of the project by each lead midwife and allowed for changes to be made to suit the differing needs of staff and patients.
The helpful partnership with NIHR CLAHRC West has allowed a robust independent evaluation and statistical analysis of the quantitative data, cross-checking the VON and Badgernet submissions (data in press).
The five sites identified 584 core staff that needed to be trained and overachieved, training 664 people between September 2014 and March 2015. All of the sites dramatically improved the rate at which magnesium sulphate was administered for preterm births achieving an average of 88% of eligible births in only 6 months. This level of uptake is comparable with current uptake of antenatal steroids for preterm births in the UK, an intervention that required more than 20 years from the establishment of the evidence base to become routinely embedded in perinatal practice at this level of adoption.
Acknowledgments
The PReCePT project was funded by the West of England Academic Health Science Network and NHS England. It has been supported by the South West Obstetric Network, National Institute of Health Research Collaboration for Leadership in Applied Health Research and Care West, Bliss, People in Health West of England, University of Bristol, University of West of England, PROMPT and the Academic Health Science Network of Networks. Executive leadership and support for the project has been given thanks to University Hospitals Bristol NHS Foundation Trust, North Bristol NHS Trust, The Royal United Hospital, Bath, Gloucestershire Hospitals NHS Foundation Trust and Great Western Hospitals NHS Foundation Trust. We would like to thank patient leaders (Monica Bridge and Ellie Salisbury) for their expertise, obstetric consultants (Emma Treloar and Tim Draycot) and neonatal consultants (David Odd, Bala Thayagarajan, Miles Wagstaff, Sarah Bates and Steve Jones) for their clinical advice and the project midwives (Polly Alford, Rachel Howard, Hannah Harding, Hannah Bailey, Sharon Jordan, Ruth Davies and Maxine Sleath) for leading as clinical champions. Most important of all, we would like to thank all the clinicians, mothers and families who made this change possible and gave their support, time, ideas and discretionary effort to make a real difference to babies' lives. In addition, we would like to thank the many patients who helped to coproduce this work.
Footnotes
Contributors: This work is the result of a collaboration of staff from five NHS maternity units (KL, CL, HB, RD, HH, RH and SJ) and staff from the West of England Academic Health Science Network (AB, SR, NM, SW and KP) who all contributed to the planning and delivery of PreCePT and the data collection and reporting of the work described in the article. AB and Dr KL contributed to the literature search, data analysis and writing and are responsible for the overall content as guarantor(s).
Competing interests: None declared.
Ethics approval: The project was subject to and meets the requirements of the NHS Research and Development Committee processes and ethical standards for service evaluation.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1. Doyle LW, Crowther CA, Middleton P, et al. Magnesium sulphate for women at risk of preterm birth for neuroprotection of the fetus. Cochrane Database Syst Rev 2009:CD004661. 10.1002/14651858.CD004661.pub3 [DOI] [PubMed] [Google Scholar]
- 2. Nightingale Internet Reporting System. Vermont oxford network database of very low birth weight infants born in 2012. Burlington, VT: Vermont Oxford Network. (accessed 4 Oct 2016). [Google Scholar]
- 3. Bliss. Neonatal Care in the UK: Facts and Statistics. (accessed Aug 2016).
- 4. Odding E, Roebroeck ME, Stam HJ. The epidemiology of cerebral palsy: incidence, impairments and risk factors. Disabil Rehabil 2006;28:183–91. 10.1080/09638280500158422 [DOI] [PubMed] [Google Scholar]
- 5. Kruse M, Michelsen SI, Flachs EM, et al. Lifetime costs of cerebral palsy. Dev Med Child Neurol 2009;51:622–8. 10.1111/j.1469-8749.2008.03190.x [DOI] [PubMed] [Google Scholar]
- 6. NHS Litigation Authority. Annual report and accounts. http://www.nhsla.com/AboutUs/Documents/NHS_Litigation_Authority_Annual_Report_Accounts_2015-2016.pdf
- 7. Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet 2008;371:261–9. 10.1016/S0140-6736(08)60136-1 [DOI] [PubMed] [Google Scholar]
- 8. Costeloe KL, Hennessy EM, Haider S, et al. Short term outcomes after extreme preterm birth in England: comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). BMJ 2012;345:e7976. 10.1136/bmj.e7976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Moore T, Hennessy EM, Myles J, et al. Neurological and developmental outcome in extremely preterm children born in England in 1995 and 2006: the EPICure studies. BMJ 2012;345:e7961. 10.1136/bmj.e7961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev 2006:CD004454. 10.1002/14651858.CD004454.pub2 [DOI] [PubMed] [Google Scholar]
- 11. Polin RA, Carlo WA. Committee on Fetus and Newborn American Academy of Pediatrics. Surfactant replacement therapy for preterm and term neonates with respiratory distress. Pediatrics 2014;133:156–63. 10.1542/peds.2013-3443 [DOI] [PubMed] [Google Scholar]
- 12. Costantine MM, Weiner SJ. Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Effects of antenatal exposure to magnesium sulfate on neuroprotection and mortality in preterm infants: a meta-analysis. Obstet Gynecol 2009;114:354–64. 10.1097/AOG.0b013e3181ae98c2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Royal College of Obstetricians and Gynaecologists. Magnesium sulphate to prevent cerebral palsy following preterm birth: Scientific impact paper no. 29, 2011. [Google Scholar]
- 14. American College of Obstetricians and Gynecologists Committee on Obstetric Practice Society for Maternal-Fetal Medicine. Committee Opinion No. 455: Magnesium sulfate before anticipated preterm birth for neuroprotection. Obstet Gynecol 2010;115:669–71. 10.1097/AOG.0b013e3181d4ffa5 [DOI] [PubMed] [Google Scholar]
- 15. The University of Adelaide. Antenatal magnesium sulphate prior to preterm birth for neuroprotection of the fetus, infant and child: National clinical practice guidelines, 2010. [Google Scholar]
- 16. Office of National Statistics. Characteristics of birth 1, 2012. [Google Scholar]
- 17. Nightingale Internet Reporting System. Vermont oxford Nntwork database of very low birth weight infants born in 2013. Burlington, VT: Vermont Oxford Network, 2013. (accessed on 4 Oct 2016). [Google Scholar]
- 18. Bliss for babies born premature or sick. http://www.bliss.org.uk
- 19. Langley G, Moen R, Nolan KM, et al. ; The improvement guide: a practical approach to enhancing organizational performance. 2nd edition. San Francisco, California, USA: Jossey-Bass Publishers, 2009. [Google Scholar]
- 20. Bate SP, Robert G. Bringing user experience to healthcare improvement: the concepts methods and practices of experience-based design: Oxford Radcliffe Publishing, 2007. [Google Scholar]
- 21. Godfrey M, Nelson E, Batalden P, et al. Clinical microsystem action guide: improving health care by improving your microsystem: Dartmouth College, 2004. [Google Scholar]
- 22. Löffler E. Why co-production is an important topic for local government. 2013. http://www.govint.org/fileadmin/user_upload/publications/coproduction_why_it_is_important.pdf
- 23. Preterm labour and birth: nice.org.uk/guidance/ng25: NICE guideline, 2015. [Google Scholar]
- 24. The Royal College of Paediatrics and Child Health. NNAP 2016 dataset audit measures. audit measures.v.1.pdf2016 http://www.rcpch.ac.uk/system/files/protected/page/2016
- 25. Info Queue. Lean project management using "Oobeya". https://www.infoq.com/articles/lean-project-management-oobeya
- 26. Crowther CA, Middleton PF, Bain E, et al. Working to improve survival and health for babies born very preterm: the WISH project protocol. BMC Pregnancy Childbirth 2013;13:7. 10.1186/1471-2393-13-239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Siwicki K, Bain E, Bubner T, et al. Nonreceipt of antenatal magnesium sulphate for fetal neuroprotection at the Women’s and Children’s Hospital, Adelaide 2010-2013. Aust N Z J Obstet Gynaecol 2015;55:233–8. 10.1111/ajo.12334 [DOI] [PubMed] [Google Scholar]
- 28. Bain E, Bubner T, Ashwood P, et al. Barriers and enablers to implementing antenatal magnesium sulphate for fetal neuroprotection guidelines: a study using the theoretical domains framework. BMC Pregnancy Childbirth 2015;15:11. 10.1186/s12884-015-0618-9 [DOI] [PMC free article] [PubMed] [Google Scholar]