Abstract
Introduction
The autonomic nervous system (ANS) is involved in regulating social behavior; Autism Spectrum Disorder (ASD) is characterized by alterations in social behavior and reduced physiological response to threat. We hypothesized that adolescents with ASD would show reduced ANS response to social threat.
Methods
Eighteen males with ASD and thirteen males with typical development (TD), ages 12 to 17, completed a social threat paradigm while wearing an impedance cardiography apparatus. We calculated pre-ejection period (PEP) and tested for between-group differences in PEP response to social threat. We also conducted correlation analyses between PEP change scores and clinical symptom scales.
Results
There was an effect of diagnosis on change in PEP from baseline to the onset of social threat (F=7.60, p=0.01), with greater changes in PEP in TD compared to ASD. PEP change score and the Social Communication Questionnaire (r=0.634, p=0.005) and the ADHD Problems Subscale of the Child Behavior Checklist (r=0.568, p=0.014) were correlated.
Conclusions
These findings suggest reduced arousal in response to social threat in ASD, with preliminary evidence that reduced sympathetic activation is associated with increased social behavior symptoms.
Keywords: autism spectrum disorder, pre-ejection period, social evaluative threat, adolescence, social behavior
Background
The autonomic nervous system (ANS) facilitates adaptive social behavior by regulating the avoidance of and engagement with potential threat through the sympathetic branch (SNS, Sapolsky et al., 2000) and facilitating flexible engagement with social stimuli through the parasympathetic branch (PNS, Porges, 2001; 2007). Increased activity of the SNS facilitates arousal (Sapolsky et al., 2000) including through the regulation of heart rate via sympathetic trunk projections, primarily to the ventricles, resulting in the release of norepinephrine, which binds to beta-1 adrenergic receptors at the neuromuscular junction. SNS influence on cardiac rhythm can be indexed by pre-ejection period (PEP), which is defined as the interval from stimulation of the left heart ventricle to the opening of the aortic valve. A decrease in the time between heart contractions results in a decrease in PEP, which reflects an increase in sympathetic activation (Berntson et al., 1994).
A large body of literature has investigated individual differences in SNS reactivity through measurement of PEP in the context of social evaluation (Mills and Dimsdale, 2013). A commonly used experimental paradigm in this field is the Trier Social Stress Test (TSST), which requires individuals to give a speech in front of an audience and reliably activates physiological stress systems (Kirschbaum et al., 1993). A recent study used both high-threat and low-threat versions of the TSST in typically developing (TD) children and found that the low-threat version of the TSST was associated with longer PEP than the standard high-threat protocol, indicating reduced SNS engagement during low SET (Yim et al., 2015). In this context, SNS activation is likely adaptive (Quas et al., 2012) and has been associated with improved emotional regulation (Schuengel et al., 2009; Stifler et al., 2011). Thus, ANS measures of arousal in social contexts could serve as an important biomarker for psychiatric disorders associated with social impairments.
Autism Spectrum Disorder (ASD) is a neurodevelopmental disorder characterized by a primary deficit in social behavior and cognition (APA, 2013). Differences in regulatory systems that underlie social approach and avoidance behavior, including alterations in the ANS, could be related to observable differences in social behavior in ASD (Benevides and Lane, 2013). Impedance cardiography may be particularly beneficial in assessing ANS reactivity in ASD; it is non-invasive and can act as an objective measure of reactivity to a variety of stimuli (Schaaf, Benevides, Leiby, & Sendecki, 2015). Despite the benefits of impedance cardiography both methodologically and empirically, there have been few ASD studies that utilize PEP. One study found that children with ASD did not have significantly different changes in PEP compared to controls following a sensory challenge (Schaaf et al., 2015). In another study, which asked participants to interact with a novel adult and with a parent, children with ASD demonstrated disorganized ANS responses. Specifically, typically developing boys showed the expected decrease in SNS influence over heart rate when interacting with a familiar adult, while those with ASD showed similar SNS responses to both novel and familiar partners (Neuhaus, Bernier, & Beauchaine, 2016).
Studies of TD populations suggest pubertal effects on PEP (Allen & Matthews, 1997; Benevides & Lane, 2013). Studies employing the TSST in pre-pubertal children with ASD have found decreased physiological reactivity to SET (Lanni et al., 2012; Levine et al., 2012). Specifically Levine and colleagues (2012) found differences in the salivary cortisol response to the TSST in children with ASD compared to TD, by subtracting baseline cortisol from cortisol during the TSST to get a measure of cortisol response to the TSST; children with ASD showed a reduction in salivary cortisol during the TSST relative to baseline, and TD children showed an increase. However, this study also examined electrodermal activity (EDA), an indirect measure of SNS activity, and found no differences at baseline or during the TSST between groups. Lanni and colleagues (2012) similarly found reduced salivary cortisol response to the TSST in ASD; in this study, change scores calculated by subtracting baseline cortisol from cortisol response during the TSST found no difference from zero in ASD, but a significant response in the TD group. Interestingly, both studies did not find between-group differences in baseline physiology or in the maintenance of the stress response, but instead, differences between groups seem to be limited to the initial response to the onset of the TSST. This suggests that potential SNS functional differences in ASD may be characterized by a reduced response to the onset of SET. In contrast, one study of adults with ASD did not find differences in HPA axis reactivity in ASD versus TD groups when comparing cortisol response before, during, and after the TSST (Jansen et al., 2006). Because the finding of reduced SNS reactivity was not present in adults with ASD, this could suggest a possible developmental mechanism that occurs during the transition to adulthood. However, no PEP studies have been conducted in adolescents.
In the present study, adolescent participants with and without ASD completed the TSST. We used ambulatory impedance cardiography measures to collect PEP data throughout the TSST. We hypothesized that individuals with ASD would show reduced SNS reactivity to the TSST compared to TD adolescents (i.e., longer PEP) associated with the onset of TSST. We also hypothesized that PEP change in response to the TSST would be correlated with social behavior.
Methods
Participants
The Vanderbilt University Institutional Review Board approved this study. Study participants were recruited from IRB-approved flyers posted at area schools, resource centers, and university clinics, as well as university-wide and local autism email listservs. Informed consent was obtained from the parents of participants prior to the study, and assent was obtained from participants. Research participants included 13 adolescent males with TD and 18 males with ASD between the ages of 12 and 17 (Table 1). Participants were matched for age and IQ as measured by the Wechsler Abbreviated Scale of Intelligence (WASI, Wechsler, 1999). For inclusion in the present study, all participants had a full-scale IQ > 70. All ASD participants had diagnosis confirmed by administration of the Autism Diagnostic Observation Schedule Version II module three (ADOS-2, Lord et al., 2012) by a research-reliable clinician. All ASD participants had ADOS total scores greater than seven. Completion of the Social Communication Questionnaire (SCQ, Rutter, 2003) and Social Responsiveness Scale (SRS-2, Constantino, 2012) to parents further supported diagnosis and confirmed that none of the TD participants demonstrated social-communication difficulties commensurate with a diagnosis. No TD participants had an SCQ >10. For the SRS, no TD participant had a total T-score greater than 50. Mean T-scores for the sub scales in the ASD group were as follows: Social Awareness: 69.95; Social Cognition: 68.75; Social Communication: 73.2; Social Motivation: 69.15; Restricted Repetitive Interests or Behaviors: 74.95.
Table 1. Sample Demographic Data.
| Group (N) | Age (SD) | PDS Score (SD) | VIQ (SD) | PIQ (SD) | FSIQ (SD) | SCQ Total Score (SD) | SRS Total Score (SD) | STAIC Trait Total Score (SD) | STAIC State Total Score (SD) |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| TD (13) | 14.77 | 2.80 | 118.15 | 112.92 | 117.69 | 2.23 | 42.08 | 30.92 | 31.92 |
| (1.70) | (0.60) | (14.44) | (9.33) | (11.63) | (2.09) | (3.12) | (5.96) | (3.58) | |
|
| |||||||||
| ASD (18) | 14.94 | 3.09 | 103.33 | 108.50 | 106.44 | 21.39 | 74.83 | 36.33 | 32.61 |
| (1.44) | (0.53) | (25.28) | (16.97) | (22.26) | (11.34) | (11.04) | (6.33) | (6.90) | |
|
| |||||||||
| t Statistic | -0.30 | -1.41 | 1.90 | 0.85 | 1.66 | -6.01 | -10.36 | -2.35 | -0.32 |
| (Cohen's d) | 0.11 | 0.52 | 0.70 | 0.32 | 0.62 | 2.61** | 4.44** | 0.89* | 0.12 |
PDS=Pubertal Development Scale, VIQ=Verbal IQ, PIQ=Performance IQ, SCQ=Social Communication Questionnaire, SRS= Social Responsiveness Scale, SD=Standard Deviation,
p<0.05,
p<0.0001
Procedures
The study involved two visits to the laboratory. During the first vist, participants completed the ADOS and WASI while parents completed the SCQ, SRS, the Pubertal Development Scale (PDS, Petersen, 1988) and Child Behavior Checklist (CBCL, Achenbach, 1991). The PDS asks parents to report on degree of development associated with puberty and shows moderate to good reliability between self-report and parent-report, with composite score interclass coefficients ranging from .238 to .441 (Carskadon and Acebo, 1993). All participants in this study had a mean PDS score of at least 2, indicating the onset of puberty. The CBCL is used to identify problem behaviors across multiple domains and is normed for ages 6-18. Parents rate the frequency of problem behaviors occurring in the last six months. Study of the CBCL in children with ASD indicates clinically significant scores in the Thought, Anxiety, Attention, Affective, and Social Problems domains the most commonly reported (Schroeder et al, 2011) as well as the ADHD, Anxiety, and Affective Problems Subscales (Kim et al., 2000). These subscores have good psychometric properties, with reliability scores ranging from .71 to .89 (Nakamura et al., 2009).
The second visit consisted of the TSST (Kirschbaum et al., 1993, Figure 1) and collection of autonomic data via electrocardiogram (ECG). ECG data were collected via a multichannel BioNex 8-slot chassis mobile ECG unit with a 4-channel biopotential amplifier provided by MindWare Technologies (Gahanna, OH). Sensors were placed on the participant's torso following standard seven-lead ECG protocols. The distance in centimeters between lead II and lead III was measured and recorded. Five minutes of baseline ECG data were acquired prior to the TSST protocol. Following baseline ECG acquisition, the participant was led to the TSST conference room, where they were greeted by two raters, one male and one female, wearing white lab coats. We modified the TSST to make it more salient for adolescents by replacing one of the adult raters with an age- and gender-matched peer. Following explanation of the task, the participant was told they would have five minutes to prepare to give a speech. This “preparation period” marks the beginning of the TSST task. During this period, participants remained in the same room where the baseline ECG data was acquired, where the same lab personnel who collected baseline ECG data joined them. Participants were instructed to quietly prepare for their speech. They were not allowed to take notes and all questions or verbalizations were ignored. For the speech and math portions of the TSST, the participant was led back to the conference room. Each of these periods was five minutes long. For the speech portion, the participant was prompted to describe why they would be a good candidate for a position in the lab. For the math portion, the participant was instructed to serial subtract by sevens from 758. Both raters were trained to maintain a neutral affect throughout the paradigm, and provided no supportive verbal or nonverbal feedback. For the debriefing period, the raters smiled, congratulated and praised the participant, and told them the entire task was “just pretend.” The participant was told they could ask questions if they liked, and the raters reassured them that they did a good job before saying goodbye. The participant then returned to the testing room with lab personnel to complete the State/Trait Anxiety Inventory for Children, a measure of state and trait anxiety (STAIC, Spielberger, 1973).
Figure 1.
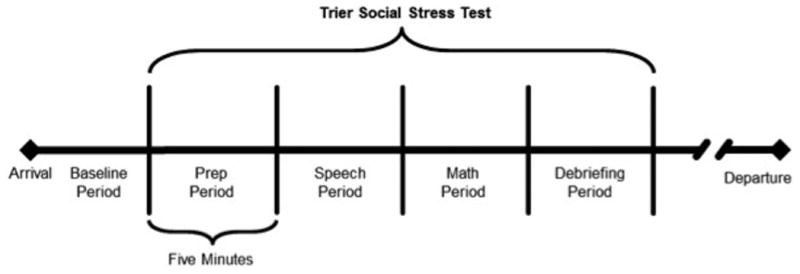
Schematic of Trier Social Stress Test behavioral paradigm
PEP Data Analyses and Processing
PEP data were calculated minute by minute from each participant's ECG using the Biolab 3.1 Heart Rate Variability Impedance Analysis Suite provided by MindWare. This software automatically recognizes the QRS complex and the B point on each trace. We calculated the B Point as the point of the maximum slope of the derivative of the mean impedance waveform before the peak. The QRS complex was confirmed by a trained rater (BLINDED). PEP was defined as the distance between the B point and the Q point on each trace. Average PEP was calculated for each participant at baseline and each portion of the TSST (Figure 1).
Statistical Analysis
We performed all analyses with SPSS Version 22.0 (IBM Corp, 2013). We used independent samples t-tests to test for between-group differences in age, pubertal status, IQ, and STAIC scores. Effect sizes are reported as Cohen's d for independent samples t-test, with values of d=0.2, d=0.5, and d=0.8 considered small, medium, and large effect sizes, respectively. We used Levene's Test for Homogeneity of Variance to test for significant effects of diagnosis on within-group variance in PEP at all points. To test for SNS reactivity to the onset of the TSST and to be consistent with previous literature (Lanni et al, 2012), we computed a PEP change score by subtracting mean PEP during baseline from PEP during the first portion of the TSST (i.e., the preparation period). We performed Univariate ANOVA to test for between-group differences in change scores. To determine if there were between-group differences in PEP throughout the TSST, we performed a repeated measures ANOVA, with mean PEP at each time point (Baseline, Preparation, Speech, Math, and Debriefing) as the dependent variables and diagnosis as the independent variable. We calculated partial η2 for all ANOVA analyses and considered values of .01, .09, and .25 to be small, medium, and large effect sizes, respectively. To see if there was any relationship between SNS response to the TSST and self-reported anxiety following the TSST, we performed Pearson's bivariate correlation analyses between STAIC total scores and PEP change scores for ASD group only. To determine if there were correlations between ASD symptom severity and PEP, we conducted Pearson's bivariate correlation analyses between SCQ and SRS and PEP change scores in the ASD group only because of limited variance in clinical scores in the TD group. Finally, to test for possible relationships between PEP response to the TSST and additional symptoms, we performed Pearson's bivariate correlations analyses between CBCL subscales (Attention, Social, Anxiety, Affective, and Thought Problems), in the ASD group only, due to limited variability in clinical scales in the TD group. Results were considered significant at p=0.008 (0.05/6).
Results
There were no significant between-group differences in age, pubertal development, verbal, performance, or full scale IQ, all p values >.10 (see Table 1). There were, as expected, higher scores in the ASD group for the SCQ, t(29)=-6.01, p<0.0001, Cohen's d=2.61 and the SRS total scores, t(29)=-10.36, p<0.0001, Cohen's d=4.44, indicating a large effect. There was also greater self-reported trait, but not state anxiety as indexed by the STAIC in the ASD group than in the TD group, t(28)=-2.35, p=0.026, Cohen's d=0.89 and t(28)=-0.32, p=0.751, Cohen's d=0.12, respectively.
Levene's test for homogeneity of variance demonstrated that there was significantly greater PEP variance in the ASD group than TD group during preparation for the TSST, F(1, 29)=12.44, p=0.001. There were no between-group differences in variance during baseline, F(1, 29)=0.26, p=0.615, speech, F(1, 29)=2.46, p=0.127, math, F(1, 29)=2.83, p=0.103 or debriefing, F(1, 29)=2.31, p=0.139 periods. Because there was a difference in the equality of variance across time, we used Greenhouse-Geisser correction to conservatively adjust the degrees of freedom for remaining parametric testing (Abdi, 2010).
Univariate ANOVA revealed an effect of diagnosis on change in PEP from baseline to the preparation period of the TSST, F(1, 31)=7.60, p=0.01, partial η2= .15 with significantly greater changes in PEP in the TD group compared to the ASD group (Figure 2).
Figure 2.
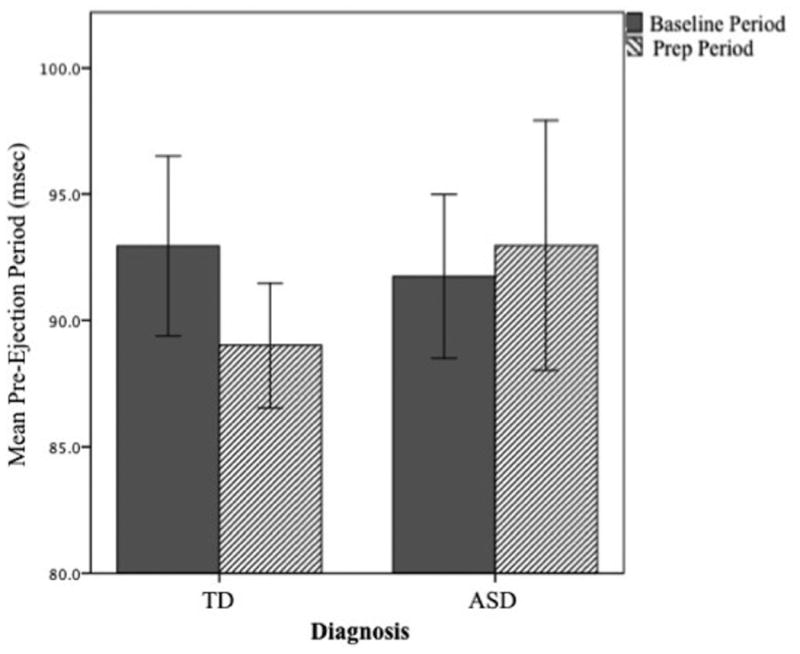
Between group differences in pre-ejection period response to the onset of the Trier Social Stress Test. TD=typically developing, ASD=autism spectrum disorder
Repeated measures ANOVA with the five phases of the TSST (Baseline, Preparation, Speech, Math, and Debriefing) as the within subjects factor and group as the between subjects factor showed no main effects of diagnosis, F(1, 29)=0.19, p=0.663, partial η2 =.007, time, F(2.465)=1.91, p=0.147, partial η2 =.062 or their interaction, F(2.465)=1.10, p=0.349, partial η2 =.036 (Figure 3).
Figure 3.
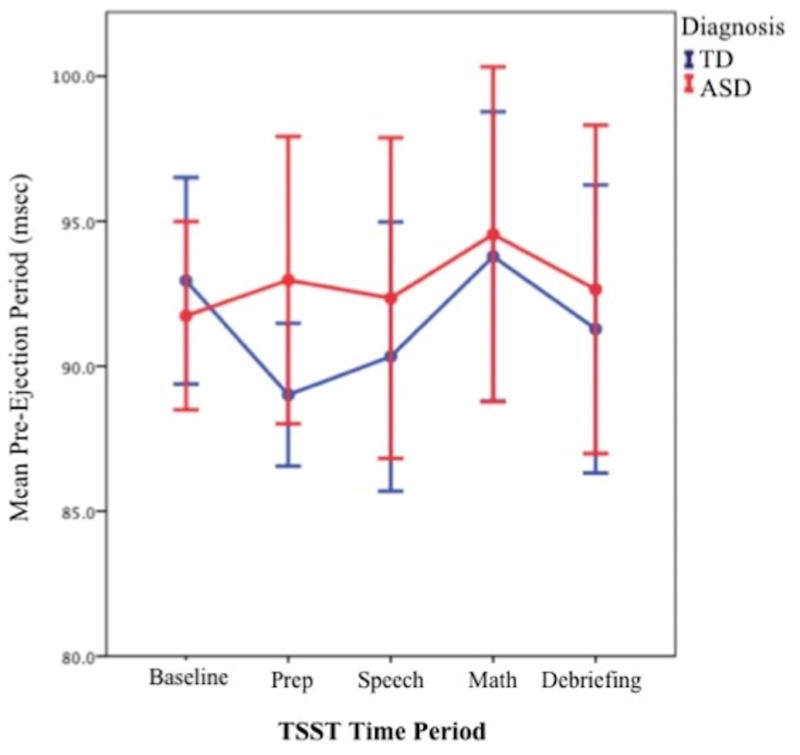
Mean pre-ejection period at baseline and during the Trier Social Stress Test. Error bars depict +2 SE. TSST=Trier Social Stress Test, TD=typically developing, ASD=autism spectrum disorder
In the ASD group, there was a significant correlation between PEP change (i.e., PEP during the Preparation period minus PEP at Baseline) and SCQ scores, r(16)=.63, p=0.005 (Figure 4) and SRS total scores, r(16)=.48, p=0.046. There were also no significant correlations between PEP change scores (defined as PEP values during the Preparation period, minus Baseline) and state, r(18)=-.043, p=0.865 or trait, r(18)=.192, p=0.446 anxiety, as assessed by the STAIC.
Figure 4.
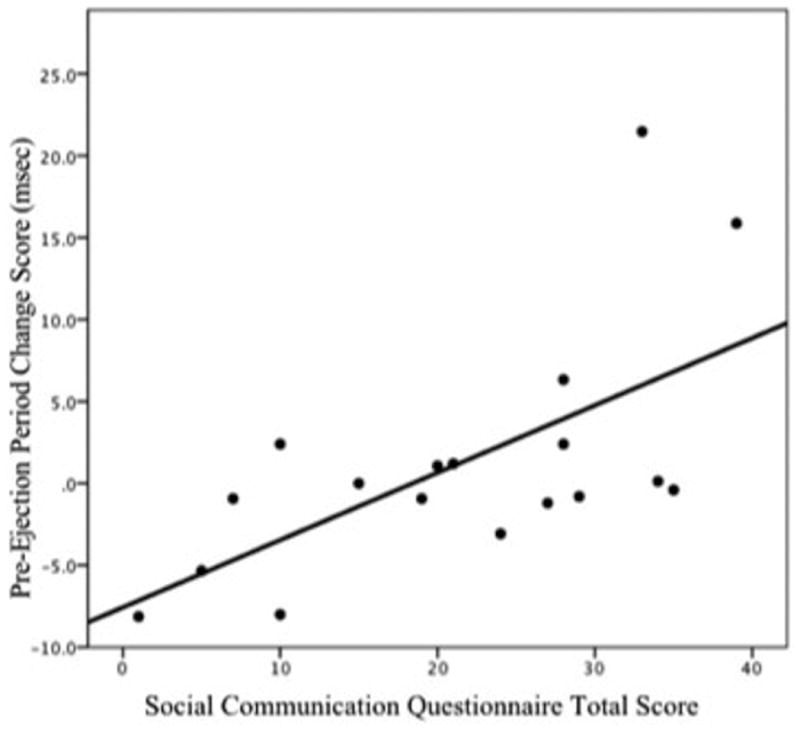
Significant correlation between Social Communication Questionnaire Total T-score and Pre-Ejection Period change score in the autism spectrum disorder group only.
To explore relationships between co-occurring psychiatric symptoms and PEP change in the ASD group, we conducted preliminary post hoc Pearson's bivariate correlations between PEP change scores and the most-commonly reported subscales of the CBCL in ASD (Kim et al., 2000; Schroeder et al., 2011). There was a significant correlation between PEP change scores and the ADHD Symptoms, r(16)=.57, p=0.014 (Figure 5). However, this finding did not meet criteria for significance following Bonfferoni correction for multiple comparison (0.05/6=0.008). There were no significant correlations between the Attention Problems domain, r(16)=.15, p=0.551, or the Social, r(16)=.24, p=0.340, Anxiety, r(16)=-.10, p=0.704, Affective, r(16)=-.17, p=0.498, or Thought Problems subscales, r(16)=.11, p=0.662 (Table 2).
Figure 5.
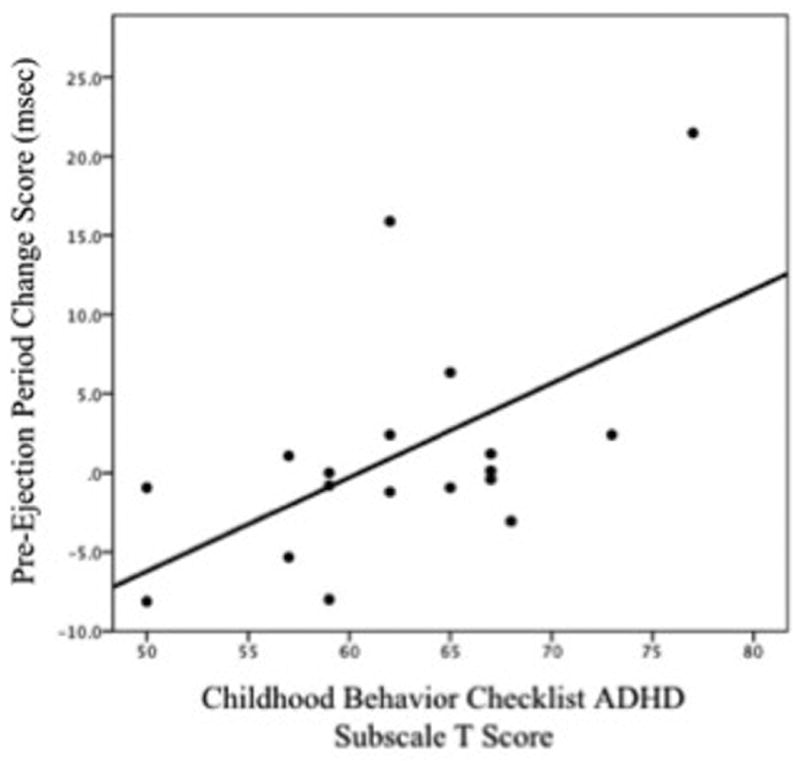
Significant correlation between the ADHD subscale of the Child Behavior Checklist and pre-ejection period change score in the autism spectrum disorder group only.
Table 2. Pearson Bivariate Correlations Between PEP Change Score (Preparation Period-Baseline) and CBCL Subscales in ASD.
| CBCL ADHD Symptoms | CBCL Attention Problems | CBCL Social Problems | CBCL Anxiety Problems | CBCL Affective Problems | CBCL Thought Problems | |
|---|---|---|---|---|---|---|
| PEP Change Score | .568* | .151 | .239 | -.096 | -.171 | .111 |
PEP= Pre-ejection Period, CBCL=Child Behavior Checklist,
=p<0.05
Discussion
In this sample of adolescent males, we found reduced SNS activation in ASD relative to TD males, suggesting that the onset of SET is less stressful for adolescent males with ASD.
Although no study to date has used the TSST, a classic SET paradigm, to study PEP reactivity in ASD, previous work has indicated reduced arousal in response to SET in ASD. This includes studies using salivary cortisol (Jansen et al., 2000; Jansen et al., 2003; Lanni et al., 2012; Levine et al., 2012; Edmiston et al., 2016) as well as a study showing reduced parasympathetic regulatory capacity in response to the TSST in adolescents with ASD (Edmiston et al., 2016) and a study that showed that reduced cortisol and parasympathetic response were related to anxiety symptoms in ASD (Hollocks et al., 2014). In contrast, studies using social play paradigms have indicated increased physiological arousal in children with ASD during interaction with peers (Corbett et al., 2012; O'Haire et al., 2015). The contradictory findings of heightened stress response to seemingly benign social interactions, coupled with blunted physiological response to SET, could indicate deficits in autonomic adaptation in ASD (Shahrestani et al., 2015). In line with the present findings, previous studies have indicated a reduced SNS response, measured via salivary cortisol, to the TSST in pre-pubertal children with ASD (Lanni et al., 2012; Levine et al., 2012). Interestingly, the only study to date to assess for SNS responsivity in adults with ASD, also via salivary cortisol, found no differences in the SNS response to the TSST between ASD and TD groups (Jansen et al., 2006). Taken together, these findings suggest a developmental mechanism in SNS reactivity to SET in ASD. Our findings extend this literature to include adolescents, indicating that alterations in physiological arousal present in childhood persist during puberty. Furthermore, the Levine and colleagues (2012) study found reduced SNS response using salivary cortisol measures, but no differences at baseline or during the TSST using electrodermal activity (EDA), a measure of SNS activity. The authors interpret their findings to suggest that differences may be present in the neuroendocrine system in ASD but not in the ANS. We also did not find significant differences in SNS activity in our overall analysis of the TSST using repeated measures ANOVA of the five time points (Baseline, Preparation, Speech, Math, and Debriefing periods); differences between the TD and ASD groups in this study were only found in the mounting of the SNS response at the onset of the TSST. It could be that this difference in analytic approach accounts for our findings. Differences may also be due to different methodological approach (PEP vs EDA) or subject characteristics, as the Levine and colleagues study was of pre-pubertal children and the present study was of pubertal adolescents.
We did not identify significant PEP differences during the TSST or time by group interaction effects on PEP. This could be due to a sample size that limits our statistical power. It is also possible that the initial PEP response to a stimulus best distinguishes ASD from TD adolescents, as our TD group showed a large response to the introduction of the TSST paradigm, but no significant differences from the ASD group as the TSST paradigm continued. More studies are needed with larger sample sizes to best determine the relationship between ASD diagnosis and physiological response and recovery to SET. PEP changes scores with the onset of the TSST was correlated with ASD symptom severity as indexed by the SCQ. Our findings indicate that more prominent social impairments in ASD are associated with blunted physiological response to SET. SNS activation in the context of social interaction supports adaptive behavioral responses (Henry, 1982; Porges et al., 2001; Worthham, 2009). Our findings could indicate reduced salience of social cues in ASD. There is a large body of literature suggesting reduced attention to social stimuli in ASD using eye tracking (for review see, Chita-Tegmark, 2016), as well as pupillometry literature suggesting reduced arousal during exposure to social stimuli (Nuske et al., 2014a and b; Krach et al., 2015). This literature suggests a possible developmental cascade of reduced arousal in response to social cues that may reduce attention to social stimuli, thereby leading to altered social behaviors (Dawson et al., 2005). Studies that combine measures of arousal with eye tracking during SET could ascertain the relationship between SNS reactivity, social salience and attention, and behavior.
We also found that reduced SNS response to the TSST was associated with more prominent ADHD symptoms. One explanation for the pathophysiology of ADHD posits that ADHD symptomatology may stem from sensation seeking in the context of understimulation. According to this hypothesis, hyperactivity associated with ADHD is an auto-regulation strategy for individuals who have reduced SNS activity both at baseline and in response to threat or reward (Beauchaine et al., 2007; Geissler et al., 2014). When reduced SNS activity is coupled with blunted parasympathetic capacity, there is a net increase in behavioral activation, impulsivity, and mood lability (Rash and Aguierre-Camacho, 2012). Our preliminary results provide support for these theoretical explanations of arousal in ADHD symptoms; however, few studies have addressed PEP in ADHD. Some studies have reported no difference in PEP compared to control groups (Beauchaine et al., 2001; Musser et al., 2011), while others have reported differences in PEP that are related to social behavior subtypes in ADHD (Musser et al., 2013; Karalunas et al., 2014). We did not formally assess for co-occurring ADHD, and are limited to parental reports of symptoms without a clinical diagnosis. ADHD is among the most common co-occurring diagnoses in ASD (Leyfer et al., 2006) and symptoms are linked to more prominent behavioral problems in ASD (Yerys et al., 2009). There is a need for more study of the physiological and behavioral correlates of ADHD in adolescents with and without ASD.
We are limited by a relatively small sample size; this is the first study to evaluate PEP in adolescents with ASD, larger studies will clarify the role of the SNS in ASD across pubertal development. This study only included male participants without intellectual impairment, limiting the generalizability of our findings. Studies designed to recruit adolescent girls with ASD are needed. Future research should focus on adaptation of social paradigms for use in participants with IQ<70. Finally, our sample was characterized as pubertal via parental report. Although the PDS allows for reliable characterization of puberty, it does not allow for the assessment of specific hormonal effects on physiological responses. Although potential pubertal hormone effects are unlikely to underlie our reported group differences findings in PEP change scores, longitudinal studies that assess for bioavailable hormone levels and their effects on responses to social stimuli are important.
Conclusions
This study offers preliminary evidence for differences in SNS response to SET in adolescents with ASD. Our findings indicate that the onset of SET is less salient or stressful for adolescents with ASD, and that this difference is associated with social communication symptoms in ASD. Findings also indicate there may be relationships between ADHD symptoms and physiological response to social stimuli. This is the first study to examine PEP reactivity in adolescents with ASD. Our findings corroborate a growing body of literature suggesting altered ANS function in ASD, while also extending this literature to include PEP during puberty. As people diagnosed in early childhood enter adolescence, a better understanding of the physiological correlates of stress is critical for clinicians, educators, and caregivers to support and advocate for the needs of adolescents as they transition to adult social relationships.
Highlights.
Adolescent males with autism show less sympathetic response to social threat
Physiological response to threat was correlated with ADHD symptoms
Physiological response to threat was also correlated with social communication symptoms
Acknowledgments
The authors would like to thank the research participants and their families for contributing to the study. This study was funded by NIMH R01 MH085717.
Footnotes
Competing Interests: The authors have no competing interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abdi H. The Greenhouse-Geisser correction. In: Salkind Neil., editor. Encyclopedia of Research Design. Thousand Oaks, CA: Sage Press; 2010. [Google Scholar]
- Achenbach TM, Howell CT, Quay HC, Conners CK. National survey of problems and competencies among four- to sixteen-year-olds: parents' reports for normative and clinical samples. Monogr Soc Res Child Dev. 1991;56(1):1–131. [PubMed] [Google Scholar]
- Allen MT, Matthews KA. Hemodynamic responses to laboratory stressors in children and adolescents: the influences of age, race, and gender. Psychophysiology. 1997;34(3):329–339. doi: 10.1111/j.1469-8986.1997.tb02403.x. [DOI] [PubMed] [Google Scholar]
- Ames CS, White SJ. Are ADHD traits dissociable from the autistic profile? Links between cognition and behavior. J Autism Dev Disord. 2011;41(3):357–363. doi: 10.1007/s10803-010-1049-0. [DOI] [PubMed] [Google Scholar]
- APA. Diagnostic and statistical manual of mental disorders, Fifth Edition (DSM-V) Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- Beauchaine TP, Katkin ES, Strassberg Z, Snarr J. Disinhibitory psychopathology in male adolescents: discriminating conduct disorder from attention-deficit/hyperactivity disorder through concurrent assessment of multiple autonomic states. J Abnorm Psychol. 2001;110(4):610–624. doi: 10.1037//0021-843x.110.4.610. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Gatze-Kopp L, Mead HK. Polyvagal Theory and developmental psychopatholoy: emotion dysreguation and conduct problems from preschool to adolescence. Biol Psychol. 2007;74(2):174–184. doi: 10.1016/j.biopsycho.2005.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benevides TW, Lane SJ. A review of cardiac autonomic measures: considerations for examination of physiological response in children with autism spectrum disorder. J Autism Dev Disord. 2013;45(2):560–575. doi: 10.1007/s10803-013-1971-z. [DOI] [PubMed] [Google Scholar]
- Berntson GG, Cacioppo JT, Binkley PF, Uchino BN, Quigley KS, Fieldstone A. Autonomic cardiac control III psychological stress and cardiac response in autonomic space as revealed by pharmacological blockades. Psychophysiology. 1994;31(6):599–608. doi: 10.1111/j.1469-8986.1994.tb02352.x. [DOI] [PubMed] [Google Scholar]
- Carskadon MA, Acebo C. A self-administered rating scale for pubertal development. J Adol Health. 1993;14(1):190–195. doi: 10.1016/1054-139x(93)90004-9. [DOI] [PubMed] [Google Scholar]
- Charman T, Baird G, Simonoff E, Loucas T, Chandler S, Meldrum D, Pickles A. Efficacy of three screening instruments in the identification of autistic-spectrum disorders. Br J Psychiatry. 2007;191(12):554–559. doi: 10.1192/bjp.bp.107.040196. [DOI] [PubMed] [Google Scholar]
- Chita-Tegmark M. Social attention in ASD: a review and meta-analysis of eye-tracking studies. Res Dev Disab. 2016;48(1):79–93. doi: 10.1016/j.ridd.2015.10.011. [DOI] [PubMed] [Google Scholar]
- Constantino JN, Gruber CP. Social Responsiveness Scale. Los Angeles: Western Psychological Services; 2012. [Google Scholar]
- Corbett BA, Schupp CW, Simon D, Ryan N, Mendoza S. Elevated cortisol during play is associated with age and social engagement in children with autism. Mol Autism. 2010;1(1):13. doi: 10.1186/2040-2392-1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbett BA, Schupp CW, Lanni KE. Comparing biobehavioral profiles across two social stress paradigms in children with and without autism spectrum disorders. Mol Autism. 2012;3(1):13. doi: 10.1186/2040-2392-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson G, Webb SJ, McParland J. Understanding the nature of face processing impairment in autism: insights from behavioral and electrophysioogical studies. Devel Neuropsychol. 2005;27(3):403–424. doi: 10.1207/s15326942dn2703_6. [DOI] [PubMed] [Google Scholar]
- Edmiston EK, Jones RM, Corbett BA. Physiological response to social evaluative threat in adolescents with autism spectrum disorder. J Autism Dev Disord. 2016;46(9):2992–3005. doi: 10.1007/s10803-016-2842-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry JP. The relation of social to biological processes in disease. Soc Sci Med. 1982;16(4):369–380. doi: 10.1016/0277-9536(82)90047-8. [DOI] [PubMed] [Google Scholar]
- Hollocks MJ, Howlin P, Papadopoulos AS, Khondoker M, Simonoff E. Differences in HPA-axis and heart rate responsiveness to psychosocial stress in children with autism spectrum disorders with and without co-morbid anxiety. Psychoneuroendocrinology. 2014;46(1):32–45. doi: 10.1016/j.psyneuen.2014.04.004. [DOI] [PubMed] [Google Scholar]
- Geissir J, Romanos M, Hegerl U, Hensch T. Hyperactivity and sensation seeking as autoregulatory attempts to stabilize brain arousal in ADHD and mania? Atten Defic Hyperact Disord. 2014;6(3):159–173. doi: 10.1007/s12402-014-0144-z. [DOI] [PubMed] [Google Scholar]
- Jansen LM, Gispen-de Wied CC, Van der Gaag RJ, ten Hove F, Willemsen-Swinkels SW, Harteveld E, et al. Unresponsiveness to psychosocial stress in a subgroup of autistic-like children, multiple complex developmental disorder. Psychoneuroendocrinology. 2000;25(1):753–764. doi: 10.1016/s0306-4530(00)00020-2. [DOI] [PubMed] [Google Scholar]
- Jansen LM, Gispen-de Wied CC, van der Gaag RJ, van Engeland H. Differentiation between autism and multiple complex developmental disorder in response to psychosocial stress. Neuropsychopharmacology. 2003;28(1):582–590. doi: 10.1038/sj.npp.1300046. [DOI] [PubMed] [Google Scholar]
- Jansen LM, Gispen-de Wied CC, Wiegant VM, Westenberg HG, Lahuis BE, van Engeland H. Autonomic and neuroendocrine responses to a psychosocial stressor in adults with autistic spectrum disorder. J Autism Dev Disord. 2006;36(1):891–899. doi: 10.1007/s10803-006-0124-z. [DOI] [PubMed] [Google Scholar]
- Karalunas SL, Fair D, Musser ED, Aykes K, Iyes SP, Nigg JT. Subtyping attention-deficit/hyperactivity disorder using temperament dimensions: toward biologically based nosologic criteria. JAMA Psychiatry. 2014;71(9):1015–1024. doi: 10.1001/jamapsychiatry.2014.763. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Kim JA, Szatmari P, Bryson SE, Streiner DL, Wilson FJ. The prevalence of anxiety and mood problems among children with autism and Asperger syndrome. Autism. 2000;4(2):117–132. [Google Scholar]
- Kirisci L, Clark DB. Reliability and validity of the State-Trait Anxiety Inventory for Children in an adolescent sample: confirmatory factor analysis and item response theory. American Educational Research Association Annual Meeting; New York, NY. April 8-12.1996. [Google Scholar]
- Kirschbaum C, Pirke KM, Hellhammer DH. The ‘Trier Social Stress Test’-- a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology. 1993;28(1-2):76–81. doi: 10.1159/000119004. [DOI] [PubMed] [Google Scholar]
- Krach S, Kamp-Becker I, Einhauser W, Sommer J, Frassle S, Jansen A, et al. Evidence from pupillometry and fMRI indicates reduced neural response during vicarious social pain but not physical pain in autism. Hum Brain Mapp. 2015;36(11):4730–4744. doi: 10.1002/hbm.22949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanni KE, Schupp CW, Simon D, Corbett BA. Verbal ability, social stress, and anxiety in children with autistic disorder. Autism. 2012;16(1):123–138. doi: 10.1177/1362361311425916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine TP, Sheinkopf SJ, Pescosolido M, Rodino A, Elia G, Lester B. Physiologic arousal to social stress in children with autism spectrum disorders: a pilot study. Res Autism Spectr Disord. 2012;6(1):177–183. doi: 10.1016/j.rasd.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyfer OT, Folstein SE, Bacalman S, Davis NO, Dinh E, Morgan J, et al. Comorbid psychiatric disorders in children with autism: interview development and rates of disorders. J Autism Devel Disord. 2006;36(1):849–861. doi: 10.1007/s10803-006-0123-0. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord. 1994;24(1):659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, Risi S. Autism Diagnostic Observation Schedule. Los Angeles: Western Psychological Services; 2001. [Google Scholar]
- Lord C, Petkova E, Hus V, Gan W, Lu F, Martin DM, et al. A multisite study of the clinical diagnosis of different autism spectrum disorders. Arch Gen Psychiatry. 2012;69(1):306–313. doi: 10.1001/archgenpsychiatry.2011.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills PJ, Dimsdale JE. Sympathetic nervous system responses to psychosocial stressors. In: Turner JR, Sherwood A, Light KC, editors. Individual differences in cardiovascular response to stress. New York: Springer; 2013. pp. 3–32. [Google Scholar]
- Musser ED, Backs RW, Schmitt CF, Ablow JC, Measelle JR, Nigg JT. Emotion regulation via the autonomic nervous system in children with attention-deficit/hyperactivity disorder (ADHD) J Abnorm Child Psychol. 2011;39(6):841–852. doi: 10.1007/s10802-011-9499-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musser ED, Galloway-Long HS, Frick PJ, Nigg JT. Emotion regulation and heterogeneity in attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2013;52(2):163–171. doi: 10.1016/j.jaac.2012.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura BJ, Ebesutani C, Bernstein A, Chorpita BF. A psychometric analysis of the child behavior checklist DSM-oriented scales. J Psychopathol Behav Assess. 2009;31(1):178–189. doi: 10.1007/s10862-009-9174-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuhaus E, Bernier RA, Beauchaine TP. Children with autism show altered autonomic adaptation to novel and familiar social partners. Autism Res. 2016 doi: 10.1002/aur.1543. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Nuske HJ, Vivanti G, Hudry K, Dissanayake C. Pupillometry reveals reduced unconscious emotional reactivity in autism. Biol Psychol. 2014a;10(1):24–35. doi: 10.1016/j.biopsycho.2014.07.003. [DOI] [PubMed] [Google Scholar]
- Nuske HJ, Vivanti G, Dissanayake C. Reactivity to fearful expression of familiar and unfamiliar people in children with autism: an eye-tracking pupillometry study. J Neurodev Disord. 2014b;6(1):14. doi: 10.1186/1866-1955-6-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Haire ME, McKenzie SJ, Beck AM, Slaughter V. Animals may act as social buffers: skin conductance arousal in children with autism spectrum disorder in a social context. Dev Psychobiol. 2015;57(5):584–595. doi: 10.1002/dev.21310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen AC, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: reliability, validity, and initial norms. J Youth Adolesc. 1988;17(1):117–133. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- Porges S. The polyvagal theory: phylogenetic substrates of a social nervous system. Int J Psychophysiol. 2001;42(2):123–146. doi: 10.1016/s0167-8760(01)00162-3. [DOI] [PubMed] [Google Scholar]
- Porges S. The polyvagal perspective. Biol Psychol. 2007;4(2):116–143. doi: 10.1016/j.biopsycho.2006.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quas JA, Yim IS, Rush E, Sumaroka M. Hypothalamic pituitary adrenal axis and sympathetic activation: joint predictors of memory in children, adolescents, and adults. Biol Psychol. 2012;89(2):335–341. doi: 10.1016/j.biopsycho.2011.11.006. [DOI] [PubMed] [Google Scholar]
- Rash JA, Aguirre-Camacho A. Attention-deficit hyperactivity disorder and cardiac vagal control: a systematic review. Atten Defic Hyperact Disord. 2012;4(4):167–177. doi: 10.1007/s12402-012-0087-1. [DOI] [PubMed] [Google Scholar]
- Rutter M. Categories, dimensions, and the mental health of children and adolescents. Ann N Y Acad Sci. 2003;1008(1):11–21. doi: 10.1196/annals.1301.002. [DOI] [PubMed] [Google Scholar]
- Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocrine Reviews. 2000;21(1):55–89. doi: 10.1210/edrv.21.1.0389. [DOI] [PubMed] [Google Scholar]
- Schaaf RC, Benevides TW, Leiby BE, Sendecki JA. Autonomic dysregulation during sensory stimulation in children with autism spectrum disorder. J Autism Dev Disord. 2015;45(2):461–472. doi: 10.1007/s10803-013-1924-6. [DOI] [PubMed] [Google Scholar]
- Schroeder J, Weiss J, Bebko J. CBCL profiles of children and adolescents with Asperger syndrome: a review and pilot study. J Dev Disabilities. 2011;17(1):26–37. [Google Scholar]
- Schuengel C, Sterkenburg PS, Jeczynski P, Janssen CG, Jongbloed G. Supporting affect regulation in children with multiple disabilities during psychotherapy: a multiple case design study of therapeutic attachment. J Consult Clin Psychol. 2009;77(2):291–301. doi: 10.1037/a0014274. [DOI] [PubMed] [Google Scholar]
- Shahrestani S, Stewart EM, Quintana DS, Hickie IB, Guastella AJ. Heart rate variability during adolescent and adult social interactions: a meta-analysis. Biol Psychol. 2015;105(1):43–50. doi: 10.1016/j.biopsycho.2014.12.012. [DOI] [PubMed] [Google Scholar]
- Spielberger CD. Manual for the State-Trait Anxiety Inventory for Children. Palo Alto, CA: Consulting Psychologists Press; 1973. [Google Scholar]
- Stifter CA, Dollar JM, Cipriano EA. Temperament and emotion regulation: the role of autonomic nervous system reactivity. Dev Psychobiol. 2011;53(3):266–279. doi: 10.1002/dev.20519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Abbreviated Scale of Intelligence. San Antonio, TX: Psychological Corporation; 1999. [Google Scholar]
- Worthman CM. Habits of the heart: life history and the developmental neuroendocrinology of emotion. Am J Hum Biol. 2009;21(6):772–781. doi: 10.1002/ajhb.20966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeryes BE, Wallace GL, Sokoloff JL, Shook DA, James JD, Kenworthy L. Attention deficit/hyperactivity disorder symptoms moderate cognition and behavior in children with autism spectrum disorders. Autism Res. 2009;2(6):322–333. doi: 10.1002/aur.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yim IS, Quas JA, Rush EB, Granger DA, Skoluda N. Experimental manipulation of the Trier Social Stress Test-Modified (TSST-M) to vary arousal across development. Psychoneuroendocrinology. 2015;57(1):61–71. doi: 10.1016/j.psyneuen.2015.03.021. [DOI] [PubMed] [Google Scholar]


