Abstract
OBJECTIVE
Differences in sleep results due to the placement of actigraphy devices (non-dominant vs. dominant wrist) are yet to be determined.
METHODS
65 nights of data from 13 adult participants was collected while participants wore two actigraphy devices, one on each wrist. Sleep indices including total sleep time (TST), total time in bed (TTB), sleep efficiency (SE%), sleep latency (SL), wake after sleep onset (WASO), sleep onset time (SOT) and wake time (WT) were assessed between the two devices.
RESULTS
There were no significant differences between devices for any of the measured sleep variables (p>0.05). SE%, SL and WASO resulted in high correlations between devices (0.89, 0.89 and 0.76, respectively), with all other sleep variables resulting in very high correlations (>0.90) between devices.
CONCLUSIONS
Based on our results, it does not seem critical which wrist the actigraphy device is worn on for measuring key sleep variables.
Keywords: Polysomnography, Actigraphy, Validity of Tests, Technology
INTRODUCTION
The quantification and measurement of sleep amongst various interventional and population research studies and clinical settings is of increasing importance. Sleep monitoring has also become a substantial consumer industry, with a rising rate of commercial companies producing various wearable sleep monitoring devices1. Although considered the 'gold standard' method of sleep measurement, polysomnography (PSG) requires a somewhat intrusive and expensive assessment of sleep indices. Wrist actigraphy is a non-intrusive, cost-effective tool used to estimate sleep quantity and quality which has been compared to PSG, showing an accuracy of up to 93% in healthy adults for total sleep time and sleep efficiency2,3 and as such is widely used in the sleep literature4.
Actigraphy involves the use of a device housed in a wristwatch that contains a small accelerometer capable of sensing movement along any one of three axes4. The accelerometer is sampled multiple times per second and the actigraph is downloaded and either manually or automatically scored for sleep indices. While actigraphy has become commonplace in both the research and consumer setting, the optimal placement of the actigraph itself is relatively unknown.
Traditionally, the majority of research studies recommend that the actigraphy device should be worn on the non-dominant wrist4, however some studies have suggested that it may be more suitable to wear the actigraph on the dominant wrist5, and others do not specify what wrist it should be worn on6. Furthermore, the new emerging technology over the past decade has seen improved automatic scoring actigraphy devices, reducing the need for sleep technicians.
Given the increasing use of actigraphy for monitoring sleep, the new and emerging technology for automatic scoring of devices and the disparate recommendations in the literature, this is an important area that needs further clarification. Therefore, the aim of the current case study was to determine if differences exist between wearing automatic-scoring actigraphy devices on the non-dominant and dominant wrists in healthy adults.
METHODS
Participants
A total of 13 healthy adults (8 male / 5 female, mean ± SD, age: 26±7) volunteered to take part in the study. All participants were free of any diagnosed sleep disorders. Ethical approval for the study was obtained through the institutions Human Research Ethics Committee.
Study Design
Participants were required to wear a wrist actigraphy device (Readiband, Fatigue Science, Vancouver) on each wrist (dominant and non-dominant) over a period of 5 nights. Participants were instructed to maintain their usual sleep habits and general daily activity patterns during the monitoring period, and were instructed to leave the devices on at all times. The Readiband has been validated against PSG, with accuracy levels of 93% being reported7 and research from our laboratory has also shown that the Readiband results in acceptable levels of inter-device reliability (ICC = >0.90)8.
At the conclusion of each recording period, actigraphy data were wirelessly downloaded to a computer using a Nordic 2.4 GHz ANT transceiver, which was then analysed using Fatigue Science software (16Hz sampling rate: ReadibandT, Fatigue Science, Vancouver). The raw activity scores were translated to sleep-wake scores based on computerized scoring algorithms. Sleep indices including total sleep time (TST), sleep efficiency (SE%), total time in bed (TTB), sleep latency (SL), wake after sleep onset (WASO), sleep onset time (SOT) and wake time (WT) were used for comparison between devices.
Statistical Analysis
Simple group statistics are shown as means ± standard deviations unless stated otherwise. An independent-samples T-test was used to compare dominant and non-dominant wrist measures using the Statistical Package for Social Science (V. 22.0, SPSS Inc., Chicago, IL), with statistical significance set at p<0.05. Inter-device agreements for dominant and non-dominant wrists were examined using Pearson's correlation coefficients (r) with 95% confidence intervals (95% CI) and interpreted as 0.90-1.00 = very high correlation, 0.70-0.89 = high correlation, 0.50-0.69 = moderate correlation, 0.26-0.49 = low correlation and 0.00-0.25 = little, if any correlation9. Between-device typical error of estimates (TEE) was determined using an excel spreadsheet10 and are presented as a coefficient of variation percentage (CV%) and as absolute values. Similar to Werner et al.11, we defined an apriori difference between the 2 devices of = 30 min satisfactory for TST, with a difference < 5% for SE satisfactory.
RESULTS
There were no significant differences between devices for any of the measured sleep variables (p>0.05).
Mean differences of 6 mins and 2 min between non-dominant and dominant wrists for TST and TTB were associated with CV% scores of 4.6 and 3.8%, respectively (Table 1).
Table 1.
Mean ± SD values for the measured sleep variables between non-dominant and dominant wrist-actigraphy devices. Comparison between devices are reported using mean bias, Pearson correlations (r), typical error of estimates (TEE) and coefficient of variation % with 95% confidence intervals.
| Non-Dominant | Dominant | Mean bias | Pearson's r | TEE | CV% | |
|---|---|---|---|---|---|---|
| Total Sleep Time (mins) | 436±72 | 442±80 | 6±19 | 0.97 (0.95 - 0.98) | 18 (15 -22) | 4.6 (3.8 - 4.7) |
| Total Time in Bed (mins) | 552±85 | 554±83 | 2±20 | 0.97 (0.95 - 0.98) | 20 (17 - 25) | 3.8 (3.1 - 4.7) |
| Sleep Efficiency (%) | 81±9 | 82±6 | 1±4 | 0.89 (0.81 - 0.94) | 4 (3 - 5) | 5.3 (4.4 - 6.6) |
| Sleep Latency (mins) | 29±34 | 28±31 | -1±15 | 0.89 (0.82 - 0.94) | 15 (13 - 19) | 102.4 (80.2 - 140.7) |
| Wake After Sleep Onset (mins) | 53±38 | 52±43 | -1±28 | 0.76 (0.61 - 0.86) | 25 (21 - 32) | 60.5 (47.7 - 82.5) |
| Sleep Onset Time (time of day) | 23:25±1:32 | 23:24±1:33 | -1±11 | 0.99 (0.99 - 0.99) | 12 (11 - 15) | 0.8 (0.7 - 1.0) |
| Wake Time (time of day) | 7:30±1:21 | 7:31±1:21 | 1±11 | 1.00 (1.00 - 1.00) | 11 (9 - 14) | 2.5 (2.1 - 3.1) |
TST, TTB, SOT and WT all resulted in very high correlations (>0.90), with SE%, SL and WASO resulting in high correlations between devices (0.89, 0.89 and 0.76, respectively).
DISCUSSION
The main finding in the current study was that there were no significant differences between non-dominant and dominant wrist actigraphy for monitoring sleep in healthy adults. The non-significant differences between devices were associated with high to very high correlations for all sleep measures and relatively low (~5%) CV's for the key sleep variables of total sleep time, total time in bed and sleep efficiency. The typical error of estimate for total sleep time and total time in bed was ~20 minutes and the mean bias was ~5 minutes, suggesting that there is little difference in what wrist the actigraph is worn on.
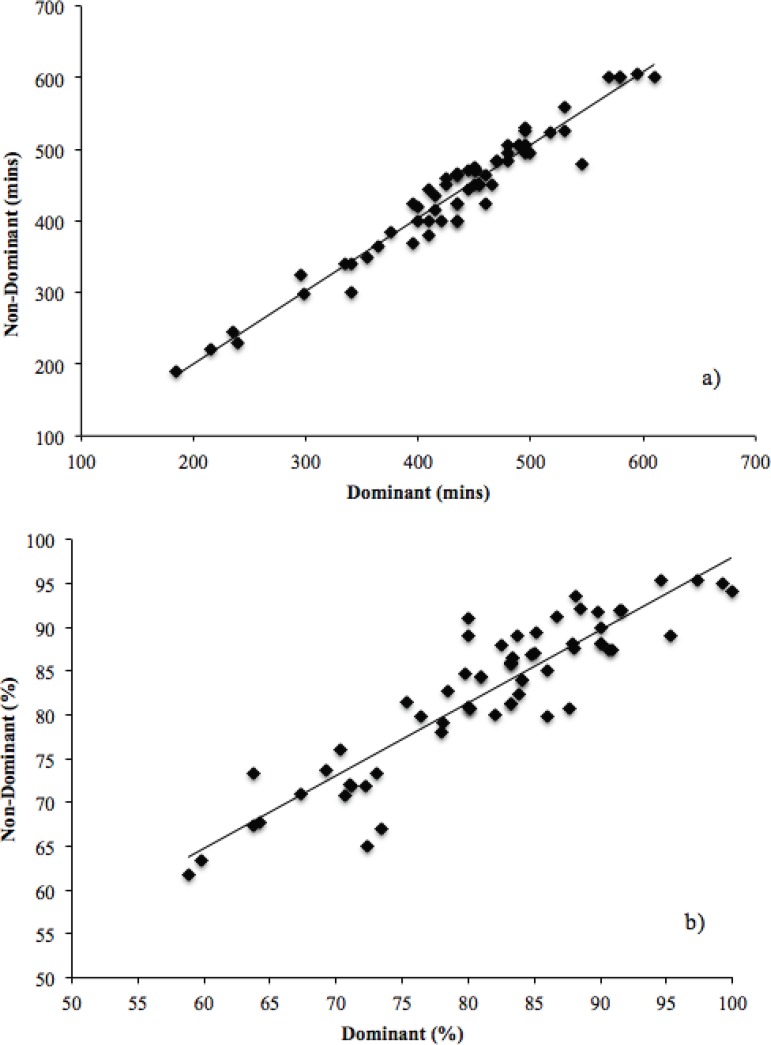
Figure 1.
Correlation plots between non-dominant and dominant wrist actigraphy data for: a) total sleep time (mins), and b) sleep efficiency (%).
The use of wrist-actigraphy for monitoring sleep is becoming increasingly popular in numerous research fields, including athletic12, clinical13, adolescent14 and pediatric15 populations. However, while traditionally it was suggested that actigraphy devices should be worn on the dominant wrist of participants16, there is a lack of evidence to show whether or not any differences actually exist. Furthermore, the ever-evolving technology of sleep monitoring via actigraphy has introduced automatic-scoring devices8, further identifying the need to investigate differences in the placement of devices.
As previously suggested6,17, care should be taken when interpreting results for WASO and SL when measured via wrist actigraphy, as the accuracy of these measures when compared to PSG is questionable. The current study would support this, as these were the most variable sleep indices between the two devices, with typical error of estimates and CV% of ~25 minutes and ~60% for WASO and ~15 minutes and ~100% for SL, respectively.
Results from the current study would suggest that the placement of the actigraphy device (dominant vs. non-dominant wrist) is not critical for accurate sleep measurement of key sleep measures including total sleep time, total time in bed, sleep onset and wake time. Given this, the authors would recommend that individuals wearing actigraphy devices, either as general consumers or research participants, should opt to wear their actigraphy device on whatever wrist feels the most comfortable. Indeed, if the device feels uncomfortable, it is more likely to influence adherence to wearing the monitor and overall sleep results.
REFERENCES
- 1.Ko PR, Kientz JA, Choe EK, Kay M, Landis CA, Watson NF. Consumer Sleep Technologies: A Review of the Landscape. J Clin Sleep Med. 2015;11(12):1455–1461. doi: 10.5664/jcsm.5288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kushida CA, Chang A, Gadkary C, Guilleminault C, Carrillo O, Dement WC. Comparison of actigraphic, polysomnographic, and subjective assessment of sleep parameters in sleep-disordered patients. Sleep Med. 2001;2(5):389–396. doi: 10.1016/s1389-9457(00)00098-8. [DOI] [PubMed] [Google Scholar]
- 3.Babin L, Lee S, Halko S, Boudreau A, George C. Determining sleep-wake activity using actiwatch. Sleep Res. 1997;26:640–640. [Google Scholar]
- 4.Sadeh A. The role and validity of actigraphy in sleep medicine: an update. Sleep Med Rev. 2011;15(4):259–267. doi: 10.1016/j.smrv.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 5.Jean-Louis G, Mendlowicz MV, Von Gizycki H, Zizi F, Nunes J. Assessment of physical activity and sleep by actigraphy: examination of gender differences. J Womens Health Gend Based Med. 1999;8(8):1113–1117. doi: 10.1089/jwh.1.1999.8.1113. [DOI] [PubMed] [Google Scholar]
- 6.Marino M, Li Y, Rueschman MN, Winkelman JW, Ellenbogen JM, Solet JM, et al. Measuring sleep: accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep. 2013;36(11):1747–1755. doi: 10.5665/sleep.3142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Russell CA, Caldwell JA, Arand D, Myers LJ, Wubbels P, Downs H. Validation of the Fatigue Science ReadibandTM Actigraph and Associated Sleep/WakeClassification Algorithms. 2011. [2017 Aug 23]. Available from: https://www.fatiguescience.com/wp-content/uploads/2016/09/Readiband-Validation-Accuracy.pdf. [Google Scholar]
- 8.Driller M, McQuillan J, O'Donnell S. Inter-device reliability of an automatic-scoring actigraph for measuring sleep in healthy adults. Sleep Sci. 2016;9(3):198–201. doi: 10.1016/j.slsci.2016.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Munro BH. Statistical methods for health care research. Philadelphia: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 10.Hopkins W. Analysis of reliability with a spreadsheet. A New View of Statistics, Internet Society for Sport Science. 2010. [2017 Aug 22]. Available from: http://sportsci.org/resource/stats/xrely.xls. [Google Scholar]
- 11.Werner H, Molinari L, Guyer C, Jenni OG. Agreement rates between actigraphy, diary, and questionnaire for children's sleep patterns. Arch Pediatr Adolesc Med. 2008;162(4):350–358. doi: 10.1001/archpedi.162.4.350. [DOI] [PubMed] [Google Scholar]
- 12.O’Donnell S, Driller MW. Sleep-hygiene Education improves Sleep Indices in Elite Female Athletes. Int J Exerc Sci. 2017;10:522–530. [PMC free article] [PubMed] [Google Scholar]
- 13.Briscoe S, Hardy E, Pengo MF, Kosky C, Williams AJ, Hart N, et al. Comparison of 7 versus 14 days wrist actigraphy monitoring in a sleep disorders clinic population. Chronobiol Int. 2014;31(3):356–362. doi: 10.3109/07420528.2013.858163. [DOI] [PubMed] [Google Scholar]
- 14.Short MA, Gradisar M, Lack LC, Wright HR, Chatburn A. Estimating adolescent sleep patterns: parent reports versus adolescent self-report surveys, sleep diaries, and actigraphy. Nat Sci Sleep. 2013;5:23–26. doi: 10.2147/NSS.S38369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Conrad N, Karlik J, Lewandowski Holley A, Wilson AC, Koh J. A Narrative Review: Actigraphy as an Objective Assessment of Perioperative Sleep and Activity in Pediatric Patients. Children (Basel) 2017;4(4) doi: 10.3390/children4040026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sadeh A, Sharkey KM, Carskadon MA. Activity-based sleep-wake identification: an empirical test of methodological issues. Sleep. 1994;17(3):201–207. doi: 10.1093/sleep/17.3.201. [DOI] [PubMed] [Google Scholar]
- 17.Zinkhan M, Berger K, Hense S, Nagel M, Obst A, Koch B, et al. Agreement of different methods for assessing sleep characteristics: a comparison of two actigraphs, wrist and hip placement, and self-report with polysomnography. Sleep Med. 2014;15(9):1107–1114. doi: 10.1016/j.sleep.2014.04.015. [DOI] [PubMed] [Google Scholar]