Abstract
Case series
Patient: Female, 50 • Male, 60
Final Diagnosis: Proximal femur fractures
Symptoms: Hip pain
Medication: —
Clinical Procedure: Internal fixation surgery
Specialty: Orthopedics and Traumatology
Objective:
Management of emergency care
Background:
Poliomyelitis is a neuromuscular disease which causes muscle atrophy, skeletal deformities, and disabilities. Treatment of hip fractures on polio-affect limbs is unique and difficult, since routine fixation methods like nailing may not be suitable due to abnormal skeletal structures.
Case Report:
We report one femoral neck fracture and one subtrochanteric fracture in polio survivors successfully treated with reverse less invasive stabilization system (LISS) plating technique. Both fractures were on polio-affected limbs with significant skeletal deformities and low bone density. A contralateral femoral LISS plate was applied upside down to the proximal femur as an internal fixator after indirect or direct reduction. Both patients had uneventful bone union and good functional recovery.
Conclusions:
Reverse LISS plating is a safe and effective technique to treat hip fractures with skeletal deformities caused by poliomyelitis.
MeSH Keywords: Bone Plates; Fracture Fixation, Internal; Hip Fractures; Poliomyelitis
Background
Poliomyelitis is a neuromuscular disease caused by viral infection. A large number of individuals who have survived this illness are alive today, especially in developing countries [1]. These patients are aging and reporting new complications, including high rates of falls and resultant fractures [2]. Polio-survivors are at high risk of hip fractures after simple falls and the patients may not return to their previous levels of function due to muscle atrophy, poor strength of the bone, and inadequate fixation. Treatment of such fractures are challenging because poliomyelitis may result in abnormal skeletal structures, such as significant coxa valga and excessive femoral anteversion, and regular implants may be contraindicated. Optimal treatment for hip fractures with significant skeletal deformities after poliomyelitis has never been discussed.
The reverse less invasive stabilization system (LISS) is an emerging technique to treat hip fractures. Recently, it has been proven to be a good alternative fixation method in the treatment of unstable proximal femur fractures as well as femoral neck non-unions [3–7]. In this case report, we successfully treated two hip fractures with poliomyelitis sequelae (one femoral neck fracture and one subtrochanteric fracture) by using the reverse LISS plating technique. Our case reports showed that hip fractures with significant skeletal deformities caused by poliomyelitis or other disease was a good indication for application of the reverse LISS plating technique.
Case Reports
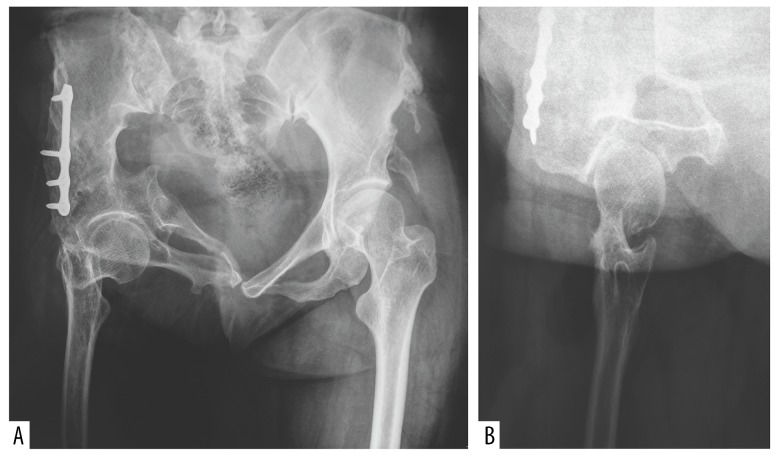
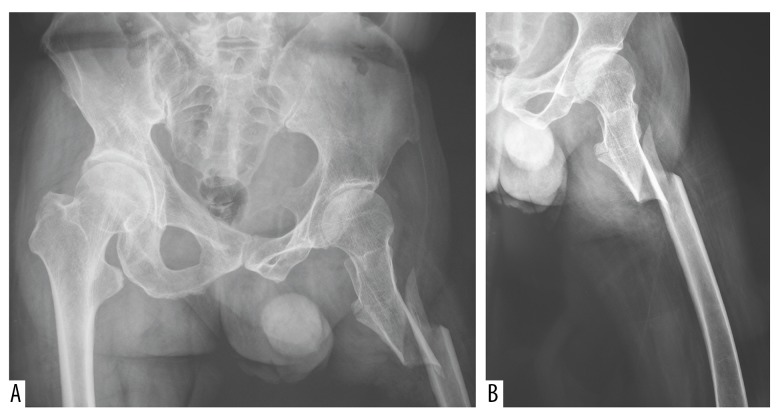
Case One was a 50-year-old female who had a femoral neck fracture after a simple fall. She had a history of paralytic poliomyelitis 15 months after birth. She underwent pelvic osteotomy surgery to correct pelvic deformity at the age of 22 years. Preoperative x-ray showed the femoral neck and shaft were significantly narrower than the normal side and deformities of the hip and pelvis were also notable (Figure 1A, 1B). Case Two was a 60-year male with left subtrochanteric femur fracture after a car accident. He had a history of poliomyelitis at the age of three years. X-ray showed a spiral intertrochanteric-subtrochanteric fracture with severe displacement (Figure 2A, 2B). Though both patients had significant muscle atrophy and shortening on the fractured limb, they could walk unaided and their daily living activities were unrestricted before injury. No other comorbidities or abnormal laboratory tests were reported in either case before surgery.
Figure 1.
The graph shows a 50-year-old female with a Garden type-4 femoral neck fracture (Case One). (A) Preoperative pelvic anteroposterior view shows abnormal structure of pelvis, acetabulum, and proximal femur after poliomyelitis and implants of previous pelvic osteotomy. The femoral head was significantly displaced and the bone density of the fractured limb was much lower. (B) Preoperative lateral view showed post-translation of fracture and a narrow femoral neck.
Figure 2.
The pelvic anteroposterior (A) and lateral femur (B) x-rays show a 60-year-old male with a multi-fragmentary inter-subtrochanteric fracture (Case Two). A minor fracture line extends from the intertrochanteric to the subtrochanteric region. The bone density of left femur was lower than the opposite side.
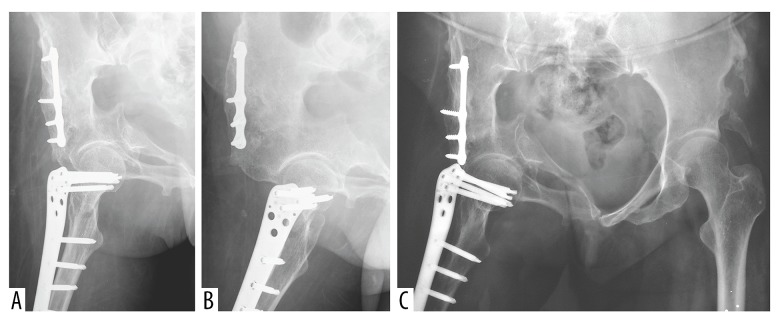
Surgery for Case One was performed the second day after injury. Regular closed reduction on traction table was done before prep and draping. The reduction was achieved by applying longitudinal traction to the fractured limb with 15° of abduction and internal rotation of the hip. Fracture alignment was corrected on both anteroposterior and lateral views and a hip valgus was noticed on fluoroscopy after reduction was achieved. A standard lateral approach was then used. The plate was slid down the submuscular plane of the lateral femur and was temporarily fixed at a central position on the lateral aspect by a reduction clamp. The normally distal tip of the plate was put slightly higher than the tip of greater trochanter and a guide wire was put through the Y hole. Fluoroscopy was checked to make sure that the guide wire was centered in the femoral neck on the lateral view. Two 2.0 mm K wires were used to temporarily fix the femoral head to the acetabulum to prevent loss of reduction during screw insertion. Four locking screws were then inserted into the proximal fragment and were checked by x-ray to make sure that they have enough purchase within the proximal fragment. Then five locking screws were inserted into the shaft holes and the K wires were removed. The final hardware placement was rechecked with x-ray imaging on both planes before irrigation and wound closing (Figure 3A, 3B).
Figure 3.
The postoperative x-ray of Case One. (A, B) X-ray on the first day after surgery showed that the fracture was reduced and stabilized with reverse LISS plating. The plate was put at a higher position bridging the fracture site. (C) X-ray at one year after surgery showed union of the fracture.
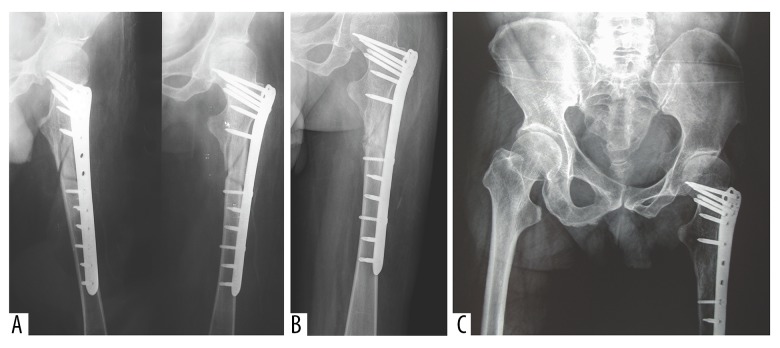
Surgery for Case Two was performed two days after injury and was done with the patient lying supine on a regular table. A direct lateral approach to the proximal femur was used. Reduction of the lateral femoral cortex was performed under traction with the help of reduction forceps. The butterfly fragment was managed to the shaft and temporarily fixed with K wires. The measured shaft-neck angle was 150° intraoperatively, and reverse LISS plating was used instead of a regular 130° intramedullary nail. A 9-hole contralateral LISS plate was first attached to the lateral femur at a central position and one guide wire was passed through a proximal wire hole and into the center of the neck as a visual cue for the placement of screws. The plate was then fixed to the shaft by one cortical screw and five proximal locking screws. The butterfly fragment was also stabilized by one screw through the plate before the rest of the distal holes were screwed in. The final hardware placement was rechecked with x-ray imaging on both planes before irrigation and wound closing (Figure 4A).
Figure 4.
The postoperative x-ray of Case Two. (A) X-ray on the first day after surgery showed alignment of fragments was restored by reverse LISS plating. The valgus deformity of hip was observed on the x-ray. (B) X-ray at 16 weeks after surgery shows ongoing union of the fracture. (C) X-ray at one year after surgery shows union of the fracture.
Blood transfusion was not necessary in either case. For both patients, range of motion (ROM) on bed was encouraged the second day after surgery and a toe-touch weight bearing was encouraged six weeks after operation. Full weight bearing was carried out 16 weeks after surgery when there were clear signs of healing on x-ray imaging. Both patients were restored to fully daily activities six months after operation and hip functions were both recovered to the pre-injury level. The patient in Case Two had normal hip ROM after surgery. In Case One, the patient had limited ROM of the hip (extension-flexion 0–110°, abduction 25°, adduction 30°, internal rotation 20° and external rotation 30°) postoperatively. Minor impingement was detected when the hip was passively abducted 25 ° or internally-rotated 20°. Since the patient also had limited ROM of the right hip before injury due to previous pelvic surgery, and she had no pain nor limitations on daily living activities, no further treatment was needed. Final union was confirmed at one year after operation for both cases (Figures 3C, 4B, 4C).
Discussion
Falls with resultant injuries are significant issues for polio survivors. Approximately 61% of polio survivors have falls for which they received medical attention, including 35% who had at least one fracture [8]. Weakness and disuse are the main reasons for the high risk of fracture on poliomyelitis-affected limbs [9]. Existent skeletal deformities like coxa valga, increase pelvic tilt and excessive femoral anteversion, as shown in these two cases, make it difficult to estimate the actual shaft-neck angle and degree of femoral anteversion during surgery planning. Therefore, regular neck-shaft angle devices may not be a suitable choice. Routine fixations also become less stable due to the low bone quality, which is another common comorbidity in the aging post-polio population [10].
For distal femur fractures, LISS has been proven to have advantages of high union rate and good maintenance of fixation, especially in osteoporotic bones and multi-fragmentary fractures [11–13]. The reverse LISS plating technique was first reported in treatment of proximal femur fracture in a poly-trauma patient [14]. This technique has now been successfully applied in some unstable proximal femoral fractures [6,15,16]. Similar to its use in distal femur fracture, the reverse LISS plating has the advantages of good angular stability and biological fixation with limited damage to the local blood supply when applied in proximal femur fractures. Ma et al. showed reverse LISS plate fixation led to complete union of unstable proximal femoral fractures without additional procedures [4]. They concluded that it was a simple and safe technique and recommended reverse LISS plating in cases that are unsuitable for nailing. When compared to nailing in the treatment of proximal femur fractures, reverse LISS more effectively avoided coxa vara and may be indicated for patients with very severe osteoporosis [6,7,16]. Our group has also shown successful application of reverse LISS in a series of femoral neck nonunion revision surgeries [3]. In this current case report, this technique was also proven to be a good alternative solution to treat hip fractures in polio survivors with significant hip deformities and low bone quality.
In Case One, screws of the conventional triple-screw or DHS fixation may easily break or penetrate the cortex of the femoral neck due to an extremely narrow femoral neck and coxa valga. Thus, reverse LISS plating avoided these risks by bridging the fracture zone instead of directly placing all the screws across the fracture line within the femoral neck. Regular fixation methods may also be less stable because of the low bone mass of the proximal femur. Multiple locking screws provided enough purchase and stability to the osteoporotic fragments.
Case Two was a case of an unstable multi-fragmentary subtrochanteric fracture. The optimal device for stabilization of subtrochanteric fractures is controversial and no consensus has been reached on the ideal choice of implants, so far. Similar to Case One, coxa valga contraindicated the use of a regular 130° intramedullary nail. We successfully restored the alignment of fragments and maintained the integrity of lateral cortex by using open reduction and reverse LISS plating. The locking screws offered satisfactory anti-rotational, anti-angulation, and anti-pullout stability in osteoporotic bone.
Implant failure and loss of fixation have been reported in proximal femur fractures treated with plating [17]. In our case report, both cases healed uneventfully. Some previous studies concluded that low patient compliance was an influential factor for implant failure since the weight bearing was usually delayed and thus should be monitored by x-ray imaging during follow-up [18]. Though weight bearing was not as early as intramedullary nailing, both patients in this study reported satisfactory functional recovery.
Currently, there is no agreement reached on the proper indications of reverse LISS plating. Some authors recommend nailing over reverse LISS for intertrochanteric fractures because of delayed weight bearing with reverse LISS technique [17]. Complications of reverse LISS plating such as broken implant and screw cutting out have also been reported [6,19]. Though some studies suggested that this technique could be a useful alternative in certain cases in which nailing is not suitable due to abnormal structure of the proximal femur [20], more illustrated cases are needed to further address this. Our report directly supported the aforementioned point and we suggest that unique hip fractures not suitable for routine fixations, such as fractures with abnormal structure of the proximal femur, are a good indication for application of reverse LISS plating.
Conclusions
Reverse LISS plating is an effective treatment for proximal femur fractures with hip deformities caused by poliomyelitis. It is a versatile and biological fixation method and can be used with either direct or indirect reduction. This technique may also be a useful alternative to treat other unique proximal femoral cases when routine methods are not applicable.
Footnotes
Conflict of interest
None.
References:
- 1.Trojan DA, Cashman NR. Post-poliomyelitis syndrome. Muscle Nerve. 2005;31(1):6–19. doi: 10.1002/mus.20259. [DOI] [PubMed] [Google Scholar]
- 2.Hill KD, Stinson AT. A pilot study of falls, fear of falling, activity levels and fall prevention actions in older people with polio. Aging Clin Exp Res. 2004;16(2):126–31. doi: 10.1007/BF03324541. [DOI] [PubMed] [Google Scholar]
- 3.Lin S, Zhang CQ, Jin DX. Combination of modified free vascularized fibular grafting and reverse Less Invasive Stabilization System (LISS) for the management of femoral neck nonunion in patients thirty years of age or younger. Injury. 2015;46(8):1551–56. doi: 10.1016/j.injury.2015.04.018. [DOI] [PubMed] [Google Scholar]
- 4.Ma CH, Tu YK, Yu SW, et al. Reverse LISS plates for unstable proximal femoral fractures. Injury. 2010;41(8):827–33. doi: 10.1016/j.injury.2010.03.028. [DOI] [PubMed] [Google Scholar]
- 5.Papanna MC, Al-Hadithy NL. Letter to Editor regarding: “Ma C-H, Tu Y-K, Yu S-W, Yen C-Y, Yeh J-H, Wu C-H. Reverse LISS plates for unstable proximal femoral fractures [Injury, 2010; 41(8): 827–33].”. Injury. 2012;43(3):392. doi: 10.1016/j.injury.2010.11.026. [DOI] [PubMed] [Google Scholar]
- 6.Yao C, Zhang CQ, Jin DX, Chen YF. Early results of reverse less invasive stabilization system plating in treating elderly intertrochanteric fractures: A prospective study compared to proximal femoral nail. Chin Med J (Engl) 2011;124(14):2150–57. [PubMed] [Google Scholar]
- 7.Zhang CQ, Sun Y, Jin DX, et al. Reverse LISS plating for intertrochanteric hip fractures in elderly patients. BMC Musculoskelet Disord. 2010;11:166. doi: 10.1186/1471-2474-11-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silver JK, Aiello DD. Polio survivors: Falls and subsequent injuries. Am J Phys Med Rehabil. 2002;81(8):567–70. doi: 10.1097/00002060-200208000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Goerss JB, Atkinson EJ, Windebank AJ, et al. Fractures in an aging population of poliomyelitis survivors: A community-based study in Olmsted County, Minnesota. Mayo Clin Proc. 1994;69(4):333–39. doi: 10.1016/s0025-6196(12)62217-4. [DOI] [PubMed] [Google Scholar]
- 10.Mohammad AF, Khan KA, Galvin L, et al. High incidence of osteoporosis and fractures in an aging post-polio population. Eur Neurol. 2009;62(6):369–74. doi: 10.1159/000242444. [DOI] [PubMed] [Google Scholar]
- 11.Kregor PJ, Stannard JA, Zlowodzki M, Cole PA. Treatment of distal femur fractures using the less invasive stabilization system: Surgical experience and early clinical results in 103 fractures. J Orthop Trauma. 2004;18(8):509–20. doi: 10.1097/00005131-200409000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Markmiller M, Konrad G, Sudkamp N. Femur-LISS and distal femoral nail for fixation of distal femoral fractures: Are there differences in outcome and complications? Clin Orthop Relat Res. 2004;426:252–57. doi: 10.1097/01.blo.0000141935.86481.ba. [DOI] [PubMed] [Google Scholar]
- 13.Wong MK, Leung F, Chow SP. Treatment of distal femoral fractures in the elderly using a less-invasive plating technique. Int Orthop. 2005;29(2):117–20. doi: 10.1007/s00264-004-0609-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pryce Lewis JR, Ashcroft GP. Reverse LISS plating for proximal segmental femoral fractures in the polytrauma patient: A case report. Injury. 2007;38(2):235–39. doi: 10.1016/j.injury.2006.08.052. [DOI] [PubMed] [Google Scholar]
- 15.Ozkaya U, Bilgili F, Kilic A, et al. Minimally invasive management of unstable proximal femoral extracapsular fractures using reverse LISS femoral locking plates. Hip Int. 2009;19(2):141–47. doi: 10.1177/112070000901900211. [DOI] [PubMed] [Google Scholar]
- 16.Han N, Sun GX, Li ZC, et al. Comparison of proximal femoral nail antirotation blade and reverse less invasive stabilization system-distal femur systems in the treatment of proximal femoral fractures. Orthop Surg. 2011;3(1):7–13. doi: 10.1111/j.1757-7861.2010.00118.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tao R, Lu Y, Xu H, et al. Internal fixation of intertrochanteric hip fractures: A clinical comparison of two implant designs. ScientificWorldJournal. 2013;2013:834825. doi: 10.1155/2013/834825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.El-Desouky II, Mohamed MM, Kandil AE. Clinical outcome of conventional versus biological fixation of subtrochanteric fractures by proximal femoral locked plate. Injury. 2016;47(6):1309–17. doi: 10.1016/j.injury.2016.03.016. [DOI] [PubMed] [Google Scholar]
- 19.Lin SJ, Huang KC, Chuang PY, et al. The outcome of unstable proximal femoral fracture treated with reverse LISS plates. Injury. 2016;47(10):2161–68. doi: 10.1016/j.injury.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 20.Jiang X, Wang Y, Ma X, et al. Proximal femoral nail antirotation versus reverse less invasive stabilization system-distal femur for treating proximal femoral fractures: A meta-analysis. Medicine. 2016;95(14):e3168. doi: 10.1097/MD.0000000000003168. [DOI] [PMC free article] [PubMed] [Google Scholar]