Abstract
A 13-year-old female presented with diminution of vision in both eyes for 3 months following snakebite. Best-corrected visual acuities were hand movement in both eyes. Fundoscopy showed vitreous hemorrhage, and B-scan ultrasonography revealed an underlying tractional retinal detachment (TRD) involving the macula in both eyes. Patient underwent 25-gauge pars plana vitrectomy in conjunction with belt buckling, endolaser, and silicone oil tamponade in the left eye. At 6 weeks postoperatively, best-corrected visual acuity of the left eye was noted to be 20/200 with settled TRD and attached retina. Bilateral proliferative retinopathy with TRD is a hitherto unreported complication of snake bite.
Keywords: Snakebite, tractional retinal detachment, vitreous hemorrhage
India ranks first in the number of deaths resulting from snakebites, with an estimate of 83,000 bites and a death toll of 11,000/annum.[1] The nonpoisonous variety forms the majority of the 236 different species of snakes found in India. However, of the 13 notable poisonous species, these four in particular †” the common cobra (Naja naja), Russell's viper (Daboia russelii), saw-scaled viper (Echis carinatus), and the common krait (Bungarus caeruleus) †” account for most of the poisonous bites in India and are highly venomous.[1] Common ocular manifestations following a snakebite are predominantly neurologic including ptosis, ophthalmoplegia, accommodation paralysis, and optic neuritis or secondary to vasculotoxicity such as vitreous hemorrhage, macular infarction, and central retinal artery occlusion.[2,3,4,5]
We report a case of bilateral proliferative retinopathy with tractional retinal detachment (TRD) following snake bite.
Case Report
A 13-year-old female presented with gradual progressive painless diminution of vision in both eyes for 3 months. She gave a history of snakebite 3 months earlier, for which she received multiple doses of antivenom as well as hemodialysis. She was unable to identify the snake as the incident occurred at night, resulting in poor visibility. Best-corrected visual acuities were hand movements in both eyes. Anterior segment examination revealed clear cornea, quiet anterior chamber, and clear lens in both eyes. On fundoscopy, both eyes showed vitreous hemorrhage precluding any view of the retina. The patient was advised B-scan ultrasonography of both eyes, which revealed an underlying TRD involving the macula [Fig. 1a and b]. The patient was advised 25-gauge pars plana vitrectomy in conjunction with belt buckling, endolaser, and silicone oil tamponade under general anesthesia in both eyes under steroid cover. She was asked to undergo the same in the left eye first. Intraoperatively, left eye showed proliferative retinopathy with extensive TRD involving the posterior pole [Fig. 2]. At 6 weeks postoperatively, best-corrected visual acuity of the left eye was noted to be 20/200. Fundoscopy of the left eye showed settled TRD with an attached retina, peripheral laser marks, and silicone oil reflex [Fig. 3]. The patient was advised surgery in the right eye during the follow-up period of the left eye, but patient declined the same.
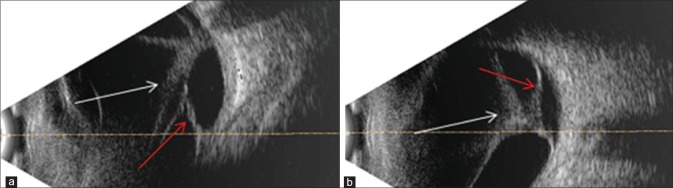
Figure 1.
B-scan ultrasonography of the right (a) and left (b) eyes showing incomplete posterior vitreous detachment with attachment at the posterior pole (white arrow) and a broad area of tractional retinal detachment involving the macula (red arrow)
Figure 2.
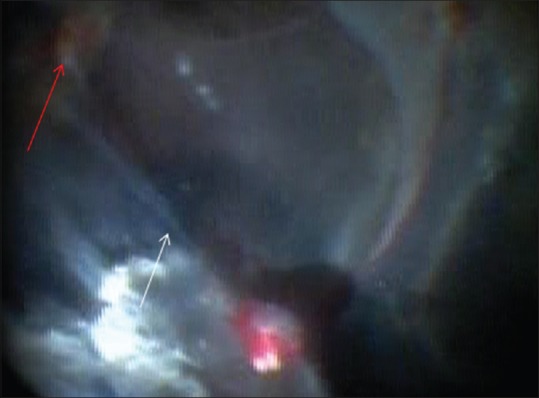
Intraoperative fundus photograph of the left eye showing proliferative retinopathy with extensive tractional retinal detachment (white arrow) involving the posterior pole. Red arrow shows the position of the optic nerve head
Figure 3.
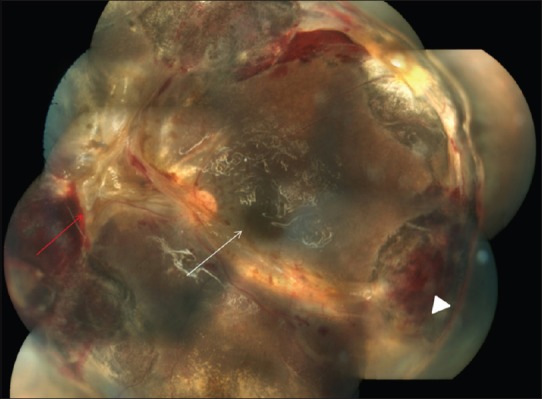
Color fundus montage of the left eye, 6 weeks postoperatively, showing settled tractional retinal detachment and attached retina (white arrow), peripheral laser marks (white arrowhead) and silicone oil reflex
Discussion
Ocular complications following snakebite are extremely rare. These include ptosis, external ophthalmoplegia,[2] conjunctival and corneal lacerations (following direct injury),[6] subconjunctival hemorrhages,[7] keratomalacia,[5] hyphema, anterior uveitis, and angle-closure glaucoma.[7] Neuro-ophthalmological manifestations such as occipital infarction and optic neuritis have been described.[8] Posterior segment manifestations, though very rare, have also been reported. They include macular infarction, central retinal arterial occlusion,[5] retinal and subhyaloid hemorrhage,[9] vitreous hemorrhage,[4] and exudative retinal detachment.[7]
The complications of snakebite are attributed mainly to the toxicity of its venom. Snake venom contains a toxic cocktail of proteins and enzymes with 90% of its dry weight primarily composed of protein. It mainly affects two systems; neurological and hematological. This is achieved by deranging the nerve synapses and the coagulation pathway, respectively. Venoms of Viperidae and some Elapidae and Colubridae contain serine proteases and other procoagulant enzymes. These enzymes stimulate blood clotting with the formation of fibrin in the bloodstream. Snake venom also contains phospholipase A2 (lecithinase). It damages mitochondria, red blood cells, leukocytes, platelets, peripheral nerve endings, skeletal muscle, and vascular endothelium. It also contains potent neurotoxins both pre- and post-synaptic. Postsynaptic neurotoxins include α-bungarotoxin and cobrotoxin. They bind to acetylcholine receptors at the motor endplate. Presynaptic neurotoxins include β-bungarotoxin, crotoxin, and taipoxin. These release acetylcholine at the nerve endings at neuromuscular junctions and then damage the endings thus preventing further release of transmitter. Toxicity of the venom is further potentiated by enzymes such as hyaluronidase, which promotes the spread of venom through tissues and proteolytic enzymes (metalloproteinases, endopeptidases, or hydrolases) and polypeptide cytotoxins which increase vascular permeability causing edema. They are also responsible for blistering, bruising, and necrosis at the site of the bite.[1]
The present case highlights bilateral TRD as a severe hitherto unreported complication of snakebite. It was not possible to identify the snake in the present case as the incident occurred in the dark. However, from the clinical history and need for hemodialysis, we can assume that the venom was hematotoxic in nature. Retinal hemorrhages, infarction, and exudative retinal detachment following snakebite have been reported.[5,7,9] However, the development of TRD adds a new dimension to the retinal toxicity of snake venom. Hematotoxic snake venoms are known to cause vasculitis.[5] We postulate in this case toxic vasculitis led to vascular occlusion and subsequently retinal ischemia. Retinal ischemia may have contributed to proliferative retinopathy thus leading to TRD. Prompt surgical management was helpful in restoring ambulatory vision to the patient.
Conclusion
This case highlights the need for close follow-up of patients with ocular complications following snakebite. Patients having retinal hemorrhages should be carefully examined to look for retinal neovascularization, and on clinical suspicion, fundus fluorescein angiography should be performed to detect neovascularization. Any neovascularization should be promptly treated with laser photocoagulation to prevent serious vision-threatening sequelae like TRD.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Warrell DA. WHO/SEARO guidelines for the clinical management of snakebite in the Southeast Asian region. Southeast Asian J Trop Med Public Health. 1999;30:1–85. [PubMed] [Google Scholar]
- 2.Takeshita T, Yamada K, Hanada M, Oda-Ueda N. Case report: Extraocular muscle paresis caused by snakebite. Kobe J Med Sci. 2003;49:11–5. [PubMed] [Google Scholar]
- 3.Menon V, Tandon R, Sharma T, Gupta A. Optic neuritis following snake bite. Indian J Ophthalmol. 1997;45:236–7. [PubMed] [Google Scholar]
- 4.Rao BM. A case of bilateral vitreous haemorrhage following snake bite. Indian J Ophthalmol. 1977;25:1–2. [PubMed] [Google Scholar]
- 5.Singh J, Singh P, Singh R, Vig VK. Macular infarction following viperine snake bite. Arch Ophthalmol. 2007;125:1430–1. doi: 10.1001/archopht.125.10.1430. [DOI] [PubMed] [Google Scholar]
- 6.Chen CC, Yang CM, Hu FR, Lee YC. Penetrating ocular injury caused by venomous snakebite. Am J Ophthalmol. 2005;140:544–6. doi: 10.1016/j.ajo.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Praveen Kumar KV, Praveen Kumar S, Kasturi N, Ahuja S. Ocular manifestations of venomous snake bite over a one-year period in a tertiary care hospital. Korean J Ophthalmol. 2015;29:256–62. doi: 10.3341/kjo.2015.29.4.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Merle H, Donnio A, Ayeboua L, Plumelle Y, Smadja D, Thomas L. Occipital infarction revealed by quadranopsia following snakebite by Bothrops lanceolatus. Am J Trop Med Hyg. 2005;73:583–5. [PubMed] [Google Scholar]
- 9.Bhandari V, Lohia M. An unusual case of bilateral vitreous haemorrhage following snake bite. Case Rep Med. 2013;2013:640582. doi: 10.1155/2013/640582. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]