Abstract
Background and aims
Pathological gambling (PG) is an impulse control disorder. This study assessed the burden of co-occurring behavioral addictions and mental health disorders in treatment-seeking patients and estimated the likelihood of receiving care for these disorders by clinician specialty.
Methods
Study data were derived from the Massachusetts All-Payer Claims Database, a representative database, for the period 2009–2013. The sample included commercially insured adult residents of Massachusetts. Univariate and multivariate logistic regressions were used to estimate the likelihood of provision of care by clinician specialty adjusting for patient’s demographic characteristics and level of care. Bonferroni correction was applied to adjust for multiple testing.
Results
The study sample included 869 patients. Treatment-seeking patients who had a diagnosis of PG were mostly males (71%), aged 45–54 years (26.7%) and enrolled in a health maintenance organization (47%). The most prevalent co-occurring disorders among patients with PG as principal diagnosis were anxiety disorders (28%), mood disorders (26%), and substance use disorders (18%). PG was associated with a more than twofold likelihood of receiving care from social workers and psychologists (p < .05). Depressive disorders were associated with a three times greater likelihood of receiving care from primary care physicians (PCPs) (p < .05). Having three and four or more diagnosis was associated with a greater likelihood of receiving care from PCPs.
Discussion and conclusions
Psychiatric and substance use disorders are prevalent among treatment-seeking pathological gamblers. The likelihood of receiving care from specialty clinicians significantly varies by clinical diagnosis and patient clinical complexity.
Keywords: behavioral addictions, mental health disorders, treatment provision, clinician specialty, pathological gambling, All-Payer Claims Data
Introduction
Pathological gambling (PG) is an impulse control disorder characterized by a persistent and recurrent maladaptive behavior that disrupts personal, family, or vocational pursuits (American Psychiatric Association, 2000). In the United States (US), the lifetime prevalence rate of PG in the adult population ranges from 0.42% to 1.9% (Petry, Stinson, & Grant, 2005; Welte, Barnes, Wieczorek, Tidwell, & Parker, 2002).
PG is known to be associated with other psychiatric disorders (Dowling, Merkouris, & Lorains, 2016; Grant, Levine, Kim, & Potenza, 2005; Lorains, Cowlishaw, & Thomas, 2011; Suomi, Dowling, & Jackson, 2014). Mood disorders, including bipolar disorders and major depressive affective disorders, personality disorders and anxiety disorders are most often comorbid with PG (Chou & Afifi, 2011; Kim, Grant, Eckert, Faris, & Hartman, 2006). Substance use disorders are also concurrent with PG (Lorains et al., 2011; Petry et al., 2005). Alcohol abuse and dependence (Chou & Afifi, 2011; Suomi et al., 2014), tobacco dependence (Boothby, Kim, Romanow, Hodgins, & McGrath, 2017), and drug abuse (Johansson, Grant, Kim, Odlaug, & Götestam, 2009) are highly prevalent among pathological gamblers. A literature review of population-based surveys found that the highest mean prevalence for combined samples of problem and PG was for nicotine dependence (60.1%), followed by a substance use disorder (57.5%), alcohol use disorder (28.1%), and illicit drug abuse/dependence (17.2%). For mental health disorders, the highest mean prevalence was for any type of mood disorder (37.9%), any type of anxiety disorder (37.4%), and major depression (23.1%) (Lorains et al., 2011).
Prior studies have suggested that psychiatric disorders and alcohol and drug dependence and other non-dependent abuse of drugs typically predate the onset of disordered gambling (Kessler et al., 2008). Conversely, there is also evidence that disordered gambling precedes and predicts the onset of other mental health conditions, such as bipolar disorders, generalized anxiety disorders, and post-traumatic stress disorders (Chou & Afifi, 2011; Pilver, Libby, Hoff, & Potenza, 2013). Research has also suggested that disordered gambling is a risk factor for the development of alcohol, nicotine, and cannabis dependence and illicit drug use (Chou & Afifi, 2011; Pilver et al., 2013).
In 2011, Massachusetts (MA) enacted the Expanded Gaming Act legalizing commercial casino gambling. Scarcity of studies on treatment-seeking behaviors among pathological gamblers and associated treatment provision along with recent legislation provides the impetus to this study. This study assessed the sociodemographic characteristics of patients seeking treatment for PG and co-occurring substance use-related addictions and mental health disorders, analyzed the workforce composition and geographic distribution of treatment providers, and estimated the likelihood of patients receiving care by clinician specialty.
To the authors’ knowledge, this is the first study to assess the prevalence of co-occurring addictive behaviors and mental health disorders in pathological gamblers seeking treatment across all levels of care during a comprehensive period of time before casinos become operative in MA in 2018. Thus, this study has the potential to make a significant intellectual contribution to understanding the burden of psychiatric disorders and behavioral addictions and to inform clinicians’ workforce composition and future study projections to address patients’ treatment provision.
Methods
The Massachusetts All-Payer Claims Database (APCD) is a representative health claims database from public and private payers in MA. Study data were derived from all medical and pharmaceutical claims for MA residents covered by the 16 largest private commercial payers in MA with dates of service from January 1, 2009 through June 30, 2013. Study data included patient demographics (i.e., age, gender, and zip code), type of health insurance coverage (i.e., private and public insurance) and commercial insurance plan [i.e., health maintenance organization (HMO), preferred provider organization, point of service, and indemnity insurance], International Statistical Classification of Diseases and Related Health Problems codes (i.e., ICD-9-CM codes), health-care services and pharmaceuticals provided in all health-care settings in MA, service dates, provider zip code, and clinician specialty. Health-care services included physician/outpatient visits, inpatient and emergency department visits, and prescription drugs.
Participants
Patients with a diagnosis of PG ascertained by ICD-9-CM code “31231” any time in the study period were included in the study. Co-occurring mental health and substance use disorders were classified into episodic mood disorders (ICD9-296) and neurotic personality disorders (ICD9-300–316). Neurotic personality disorders were classified as anxiety disorders (ICD9-300), adjustment reaction (ICD9-309) and depressive disorders (ICD9-311), disorders of impulsive control (ICD9-312), and psychoactive substance disorders (ICD9-303–305). Psychoactive substance disorders were broken down into alcohol dependence syndrome (ICD9-303), drug dependence (ICD9-304), and non-dependent abuse of drugs (ICD9-305). Non-dependent abuse of drugs included alcohol abuse (ICD9-305.0), tobacco use disorder (ICD9-305.1), cannabis abuse (ICD9-305.2), opioids abuse (ICD9-305.5), and cocaine abuse (ICD9-305.6).
Measures
We created categorical variables for co-occurring disorders to estimate the likelihood of receiving care by assessed clinician specialties associated with each diagnosis with respect to all other mental health and psychoactive substance diagnosis and with the number of prevalent co-occurring disorders as a bundle (i.e., one, two, three, and four or more diagnosis). Prevalence rates were reported as the percentage of patients with each specific co-occurring disorder divided by total number of patients with a diagnosis of PG, either as a principal or primary diagnosis in a given year.
Patients were excluded from the analytical sample if they were under the age of 18 years (n = 13 patients over the study period), lived in a zip code outside MA (n = 8) or received care from a provider in a zip code outside MA (n = 2) anytime during the study period. In addition, patients who only had public insurance coverage in all their claims (n = 62 patients over the study period) were excluded from the analysis. Patients who switched from public to private insurance or vice versa in a given year (n = 1) were kept in the analytical sample. Patients whose first claim appeared in the period of January–June 2013 (n = 27) were excluded from the analysis so as to have a minimum of 6-month time span for claims data processing.
Analysis of the provision of health-care services included all levels of care in all health-care settings across the Commonwealth of Massachusetts. Analysis of the likelihood of receiving care for mental health and substance use disorders by clinician specialty included therapeutic providers (e.g., counseling psychologists and clinical social workers) and prescribing providers (e.g., psychiatrists and general practice physicians). Analysis of the geographic distribution of providers and patients was performed by Massachusetts County.
Statistical analysis
Descriptive statistics were performed for main study variables by year and overall for the entire study period. Univariate and multivariate analyses, prevalence estimates, and 95% confidence intervals were performed to examine patient sociodemographic characteristics and prevalence of PG and co-occurring disorders. Multivariate logistic regression was conducted to estimate the likelihood of receiving care by assessed clinician specialties holding constant sociodemographic variables, type of health insurance coverage, and level of care. The following equation represents the model:
where i = 1,…, n individuals, ui the error term – errors are independent and identically distributed, N(0, σ2ν) – and F is the standard normal cumulative distribution function. Y represents the provider specialty, X1 represents a vector of patient’s sociodemographic characteristics, X2 represents type of health insurance coverage (i.e., HMO vs. other type of insurance), and X3 represents level of care. Odds ratio estimates indicate the probability of the outcome variable associated with the assessed explanatory variables. Bonferroni correction was applied to adjust for multiple testing. All study analyses were performed using STATA MP Software, version 14.0 (StataCorp 2014, Stat Statistical Software, Release 14, StataCorp LLC, College Station, TX, USA) and SAS 9.1 (SAS Institute Inc., Cary, NC, USA).
Ethics
This study used de-identified administrative claims data. The Massachusetts Department of Public Health and the UMass Institutional Review Board granted study approval.
Results
The study analytical sample included 869 MA residents with a clinical diagnosis of PG who sought care in the Commonwealth at some time during the study period. Overall, treatment-seeking patients who had a diagnosis of PG and co-occurring disorders were mostly males (71%), aged 45–54 years (26.7%), living in the Middlesex County (25%), and enrolled in a HMO (47%) (Table 1).
Table 1.
Sociodemographic characteristics of treatment-seeking patients
| 2009 | 2010 | 2011 | 2012 | 2009–2012 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age | ||||||||||
| 18–24 | 11 | 2.7% | 21 | 4.3% | 22 | 4.8% | 18 | 4.2% | 36 | 4% |
| 25–34 | 52 | 12.8% | 59 | 12.0% | 58 | 12.7% | 45 | 10.5% | 118 | 14% |
| 35–44 | 95 | 23.3% | 108 | 22.0% | 94 | 20.6% | 95 | 22.2% | 199 | 23% |
| 45–54 | 126 | 31.0% | 145 | 29.5% | 129 | 28.2% | 124 | 29.0% | 249 | 29% |
| 55–64 | 101 | 24.8% | 126 | 25.6% | 121 | 26.5% | 109 | 25.5% | 202 | 23% |
| 65+ | 22 | 5.4% | 33 | 6.7% | 33 | 7.2% | 37 | 8.6% | 65 | 7% |
| Gender | ||||||||||
| Female | 122 | 30.0% | 131 | 26.6% | 133 | 29.1% | 127 | 29.7% | 252 | 29% |
| Male | 285 | 70.0% | 361 | 73.4% | 324 | 70.9% | 301 | 70.3% | 617 | 71% |
| Commercial insurance plan | ||||||||||
| Health maintenance organization (HMO) | 197 | 56.6% | 250 | 60% | 224 | 58% | 202 | 57% | 321 | 47% |
| Preferred provider organization | 103 | 29.6% | 119 | 28% | 104 | 27% | 94 | 26% | 245 | 36% |
| Point of service | 32 | 9.2% | 36 | 9% | 36 | 9% | 34 | 10% | 85 | 13% |
| Exclusive provider organization | 14 | 4.0% | 15 | 4% | 14 | 4% | 17 | 5% | 29 | 4% |
| Indemnity insurance | 5 | 1.4% | 10 | 2% | 18 | 5% | 17 | 5% | 27 | 4% |
| Total patients with private health insurance | 348 | 86% | 419 | 85% | 386 | 84% | 355 | 83% | 678 | 78% |
| Patients by county | ||||||||||
| Barnstable | 6 | 1% | 9 | 2% | 9 | 2% | 7 | 2% | 13 | 1% |
| Berkshire | a | a | 10 | 2% | 9 | 2% | 11 | 3% | 13 | 1% |
| Bristol | 52 | 13% | 63 | 13% | 62 | 13% | 53 | 12% | 109 | 12% |
| Essex | 41 | 10% | 38 | 8% | 43 | 9% | 39 | 9% | 88 | 10% |
| Franklin | 8 | 2% | 7 | 1% | 8 | 2% | a | a | 10 | 1% |
| Hampden | 25 | 6% | 38 | 8% | 36 | 8% | 28 | 6% | 63 | 7% |
| Hampshire | 11 | 3% | 14 | 3% | 10 | 2% | 15 | 3% | 23 | 3% |
| Middlesex | 99 | 24% | 130 | 26% | 109 | 23% | 105 | 24% | 226 | 25% |
| Norfolk | 60 | 14% | 70 | 14% | 53 | 11% | 55 | 13% | 122 | 14% |
| Plymouth | 34 | 8% | 32 | 6% | 40 | 9% | 45 | 10% | 76 | 8% |
| Suffolk | 35 | 8% | 39 | 8% | 37 | 8% | 36 | 8% | 66 | 7% |
| Worcester | 40 | 10% | 52 | 10% | 51 | 11% | 40 | 9% | 87 | 10% |
| Total patients by county | 414 | 502 | 467 | 438 | 897 | |||||
| Total patients by analytical sample | 407 | 492 | 457 | 428 | 869 | |||||
Note. A patient may be in more than one county within a 1-year time period.
Suppressed data.
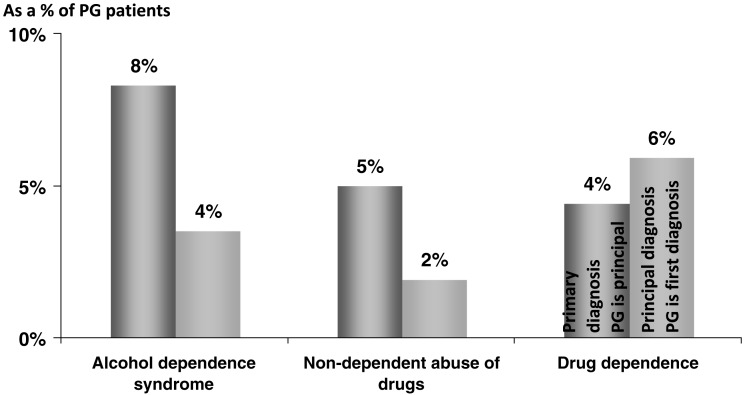
In the period from January 1, 2009 through December 31, 2012, 447 (51.4%) and 373 (42.9%) of treatment-seeking patients had PG as a principal and primary diagnosis, respectively. The most prevalent primary diagnoses, in patients who had PG as a principal diagnosis, were anxiety, dissociative and somatoform disorders (27.8%), episodic mood disorders (25.6%), and depressive disorders (13.3%) (Table 2). Adjustment reaction prevalence (9.4%) included adjustment disorder with predominant disturbance of other emotions and post-traumatic stress disorders. Prevalence of disorders of impulse control, not elsewhere classified (9%) included unspecified impulse control disorders and PG. Psychoactive substance disorders (17.8%) including alcohol dependence (8.3%), drug dependence (i.e., opioid-, anxiolytic-, cocaine-, and cannabis dependence) (4.4%), and non-dependent abuse of drugs (i.e., alcohol abuse, tobacco use disorders, and cannabis-, opioid-, and cocaine abuse) (5.0%) were also prevalent conditions among patients with PG as a principal diagnosis (Figure 1).
Table 2.
Prevalence rates for primary diagnosis among patients with pathological gambling as principal diagnosis, ICD-9-CM codes
| 2009 | 2010 | 2011 | 2012 | 2009–2012 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Episodic mood disorders (296) | 19 | 25.7% | 23 | 23.2% | 21 | 22.1% | 16 | 18.8% | 46 | 25.6% |
| Neurotic disorders, personality disorders, and other non-psychotic mental disorders (300–316) | ||||||||||
| Anxiety, dissociative, and somatoform disorders (300.0–300.9) | 20 | 27.0% | 26 | 26.3% | 27 | 28.4% | 22 | 25.9% | 50 | 27.8% |
| Psychoactive substance (303–305) | 15 | 20.3% | 17 | 17.2% | 15 | 15.8% | 14 | 16.5% | 32 | 17.8% |
| Adjustment reaction (309.0–309.9) | 9 | 12.2% | 7 | 7.1% | 9 | 9.5% | 7 | 8.2% | 17 | 9.4% |
| Depressive disorder, not elsewhere classified (311) | 12 | 16.2% | 13 | 13.1% | 13 | 13.7% | 10 | 11.8% | 24 | 13.3% |
| Disorders of impulse control, not elsewhere classified (312.3) | 7 | 9.5% | 6 | 6.1% | 8 | 8.4% | 9 | 10.6% | 17 | 9.4% |
| Patients with principal diagnosis when PG is principal diagnosis | 204 | 50.1% | 247 | 50.2% | 229 | 50.1% | 204 | 47.7% | 447 | 51.4% |
| Patients with first diagnosis when PG is principal diagnosis | 74 | 36.3% | 99 | 40.1% | 95 | 41.5% | 85 | 41.7% | 180 | 40.3% |
Figure 1.
Most prevalent psychoactive substance diagnosis among treatment-seeking patients, 2009–2012. Note. Non-dependent abuse of drugs includes alcohol abuse, tobacco use disorder, cannabis abuse, opioid abuse, and cocaine abuse. Drug dependence includes opioid-type dependence and anxiolytic-, cocaine-, and cannabis dependence. Chart includes treatment-seeking patients with primary diagnosis (n = 180) out of 447 patients who had pathological gambling as principal diagnosis and patients with a principal diagnosis when pathological gambling was primary diagnosis (n = 373) out of 869 patients in the analytical sample who had a principal diagnosis
The most prevalent principal diagnoses, in patients who had PG as a primary diagnosis, were episodic mood disorders (34.7%), anxiety, dissociative and somatoform disorders (17%), and depressive disorders (7.5%) (Table 3). Psychoactive substance disorders (9.3%) including alcohol dependence (3.5%), drug dependence (5.9%), and non-dependent abuse of drugs (2.0%) were also prevalent principal diagnoses among patients with PG as a primary diagnosis (Figure 1). In the study period, PG was the hospital admitting diagnosis for 3%–5% of the treatment-seeking patients in the analytical sample.
Table 3.
Prevalence rates for principal diagnosis among patients with pathological gambling as primary diagnosis, ICD-9-CM codes
| 2009 | 2010 | 2011 | 2012 | 2009–2012 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Episodic mood disorders (296) | 77 | 48.1% | 74 | 38.3% | 72 | 39.1% | 78 | 41.5% | 157 | 42.1% |
| Neurotic disorders, personality disorders, and other non-psychotic mental disorders (300–316) | ||||||||||
| Anxiety, dissociative, and somatoform disorders (300.0–300.9) | 28 | 17.5% | 41 | 21.2% | 36 | 19.6% | 40 | 21.3% | 77 | 20.6% |
| Psychoactive substance (303–305) | 26 | 16.3% | 25 | 13.0% | 25 | 13.6% | 32 | 17.0% | 42 | 11.3% |
| Adjustment reaction (309.0–309.9) | 10 | 6.3% | 20 | 10.4% | 20 | 10.9% | 46 | 24.5% | 33 | 8.8% |
| Depressive disorder, not elsewhere classified (311) | 14 | 8.8% | 16 | 8.3% | 15 | 8.2% | 8 | 4.3% | 34 | 9.1% |
| Disorders of impulse control, not elsewhere classified (312.3) | 9 | 5.6% | 9 | 4.7% | 9 | 4.9% | 10 | 5.3% | 23 | 6.2% |
| Patients with principal diagnosis when PG is first diagnosis | 179 | 89.4% | 218 | 88.5% | 206 | 89.3% | 213 | 88.3% | 452 | 82.5% |
| Patients with PG as first diagnosis | 160 | 39.3% | 193 | 39.2% | 184 | 40.3% | 188 | 43.9% | 373 | 42.9% |
Note. Non-dependent abuse of drugs (ICD9-305.0–305.9) includes alcohol abuse (ICD9-305.0), tobacco use disorder (ICD9-305.1), cannabis abuse (ICD9-305.2), opioid abuse (ICD9-305.5), and cocaine abuse (ICD9-305.6). Drug dependence (ICD9-304) includes opioid-type dependence (ICD9-304.0) and anxiolytic, cocaine, and cannabis dependence (ICD9-304.1–304.9).
Adjustment reaction (ICD9-309.0–309.9) includes adjustment disorder with predominant disturbance of other emotions (ICD9-309.0–309.9) and post-traumatic stress disorder (ICD9-309.81). Disorders of impulse control, not elsewhere classified (ICD9-312.3), include impulse control disorder, unspecified (ICD9-312.30), and pathological gambling (ICD9-312.31).
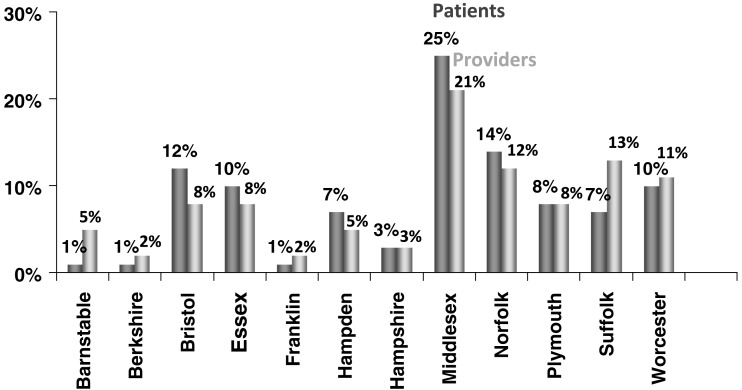
The geographic location of treatment-seeking patients with a diagnosis of PG who received care across settings in the Commonwealth and their health-care provider practice offices/settings were not evenly distributed (Figure 2). Prevalence of PG and concurrent psychiatric and substance use disorders were higher than the county population in Middlesex (25% and 23%, respectively), Norfolk (14% and 10%, respectively), and Bristol Counties (12% and 8%, respectively) (U.S. Census Bureau, 2010). In addition, the percentage of treatment-seeking patients with a diagnosis of PG and concurrent disorders was greater than the percentage of assessed clinicians providing treatment services in Middlesex (25% and 21%, respectively) and Norfolk (14% and 12%, respectively) Counties. Conversely, 7% of patients lived in the Suffolk County where 13% of the clinicians provided care.
Figure 2.
Treatment-seeking patients and health-care providers by Massachusetts County, 2009–2012. Note. Data for Nantucket and Dukes County were suppressed
Adjusting for patient’s demographic characteristics, type of health insurance plan and level of care, the likelihood of receiving care by specialty of clinicians significantly varied by patient’s diagnosis and number of co-occurring disorders. PG as a principal diagnosis was associated with almost a three times greater probability of receiving care from psychologists (2.8, p < .01) and social workers (2.6, p < .01) and a lower probability of receiving care from primary care physicians (PCPs) and psychiatrists (0.4; p < .01) (Table 4). Conversely, compared with other concurrent mental health diagnosis, depressive disorder diagnosis was associated with greater than three times likelihood of receiving care from PCPs (3.5; p < .01).
Table 4.
Maximum likelihood estimates for treatment-seeking patients by clinician specialty, 2009–2012
| Adjusted odds ratios; (p values); [95% confidence intervals – CI] | ||||||||
|---|---|---|---|---|---|---|---|---|
| PCP | Psychiatrist | Psychologist | Social worker | PCP | Psychiatrist | Psychologist | Social worker | |
| Male (ref: female) | 1.063 | 1.072 | 1.214 | 0.747 | 0.988 | 1.340 | (omitted) | 0.796 |
| (0.822) | (0.813) | (0.505) | (0.329) | (0.965) | (0.324) | (0.433) | ||
| [0.63–1.81] | [0.60–1.91] | [0.69–2.15] | [0.42–1.34] | [0.59–1.66] | [0.75–2.40] | [0.45–1.41] | ||
| Age (ref: 18–24) | ||||||||
| 25–34 | 1.306 | 0.216* | 1.863 | 2.027 | 1.263 | 0.294 | 1.522 | 1.817 |
| (0.697) | (0.038) | (0.443) | (0.420) | (0.730) | (0.113) | (0.612) | (0.500) | |
| [0.34–5.02] | [0.05–0.92] | [0.38–9.13] | [0.36–11.27] | [0.34–4.74] | [0.06–1.34] | [0.30–7.73] | [0.32–10.30] | |
| 35–44 | 1.052 | 0.321 | 2.461 | 1.502 | 0.927 | 0.416 | 2.443 | 1.354 |
| (0.939) | (0.107) | (0.245) | (0.632) | (0.907) | (0.240) | (0.257) | (0.723) | |
| [0.29–3.84] | [0.08–1.28] | [0.54–11.22] | [0.28–7.92] | [0.26–3.31] | [0.10–1.80] | [0.52–11.45] | [0.25–7.24] | |
| 45–54 | 1.472 | 0.515 | 1.842 | 0.843 | 1.208 | 0.591 | 2.007 | 0.862 |
| (0.547) | (0.305) | (0.427) | (0.840) | (0.766) | (0.444) | (0.372) | (0.862) | |
| [0.42–5.19] | [0.14–1.83] | [0.41–8.31] | [0.16–4.44] | [0.35–4.18] | [0.15–2.27] | [0.43–9.27] | [0.16–4.64] | |
| 55–64 | 1.307 | 0.282 | 1.445 | 2.030 | 0.989 | 0.362 | 1.484 | 2.208 |
| (0.684) | (0.077) | (0.641) | (0.397) | (0.986) | (0.170) | (0.623) | (0.351) | |
| [0.36–4.75] | [0.07–1.14] | [0.31–6.81] | [0.39–10.44] | [0.28–3.54] | [0.08–1.55] | [0.31–7.14] | [0.42–11.68] | |
| 65+ and older | 0.803 | 0.468 | 2.914 | 1.269 | 0.640 | 0.563 | 3.186 | 1.312 |
| (0.781) | (0.391) | (0.243) | (0.818) | (0.580) | (0.550) | (0.243) | (0.796) | |
| [0.17–3.77] | [0.08–2.66] | [0.48–17.56] | [0.17–9.69] | [0.13–3.12] | [0.09–3.69] | [0.45–22.32] | [0.17–10.28] | |
| Outpatient (ref: other level of care) | 0.744 | 0.694 | 1.363 | 1.726 | 0.727 | 0.757 | 1.138 | 1.735 |
| (0.392) | (0.379) | (0.405) | (0.161) | (0.380) | (0.498) | (0.723) | (0.156) | |
| [0.38–1.46] | [0.31–1.57] | [0.66–2.82] | [0.80–3.70] | [0.36–1.48] | [0.34–1.69] | [0.56–2.33] | [0.81–3.72] | |
| HMO (ref: other insurance) | 2.912*** | 0.394*** | 0.714 | 0.692 | 3.059*** | 0.350*** | 0.742 | 0.684 |
| (0.000) | (0.001) | (0.213) | (0.208) | (0.000) | (0.000) | (0.279) | (0.195) | |
| [1.83–4.64] | [0.23–0.67] | [0.42–1.21] | [0.39–1.23] | [1.89–4.95] | [0.20–0.61] | [0.43–1.27] | [0.39–1.21] | |
| Patient and provider same city zip code (ref: different zip code) | 0.986 | 0.665 | 1.474 | 0.944 | 0.855 | 0.669 | 1.633 | 1.085 |
| (0.966) | (0.326) | (0.260) | (0.878) | (0.650) | (0.338) | (0.181) | (0.829) | |
| [0.51–1.92] | [0.30–1.50] | [0.75–2.90] | [0.45–1.96] | [0.43–1.68] | [0.29–1.52] | [0.80–3.34] | [0.52–2.27] | |
| Number of diagnosis (ref: one) | ||||||||
| Two diagnosis | 1.457 | 1.914 | 0.641 | 0.673 | ||||
| (0.242) | (0.145) | (0.154) | (0.258) | |||||
| [0.78–2.74] | [0.80–4.58] | [0.35–1.18] | [0.34–1.34] | |||||
| Three diagnosis | 2.860** | 4.708** | 0.0936*** | 0.431* | ||||
| (0.004) | (0.002) | (0.000) | (0.050) | |||||
| [1.41–5.81] | [1.81–12.25] | [0.03–0.31] | [0.19–1.00] | |||||
| Four or more diagnosis | 5.655*** | 1.761 | 0.268*** | 0.177*** | ||||
| (0.000) | (0.227) | (0.001) | (0.001) | |||||
| [2.86–11.17] | [0.70–4.41] | [0.13–0.57] | [0.07–0.47] | |||||
| Pathological gambling (31231) as principal (ref: other mental health diagnosis) | 0.404** | 0.378** | 2.774** | 2.582** | ||||
| (0.002) | (0.009) | (0.002) | (0.002) | |||||
| [0.23–0.71] | [0.18–0.78] | [1.47–5.24] | [1.42–4.69] | |||||
| Depressive disorder (311) in any position (ref: other mental health diagnosis) | 3.547** | 0.163* | 0.718 | 0.584 | ||||
| (0.001) | (0.012) | (0.494) | (0.310) | |||||
| [1.67–7.55] | [0.04–0.67] | [0.28–1.85] | [0.21–1.65] | |||||
| Adjustment reaction (309) in any position (ref: other mental health diagnosis) | 0.642 | 0.576 | 1.915 | 1.655 | ||||
| (0.295) | (0.277) | (0.164) | (0.253) | |||||
| [0.28–1.47] | [0.21–1.56] | [0.77–4.79] | [0.70–3.93] | |||||
| Episodic mood (296) in any position (ref: other mental health diagnosis) | 1.126 | 1.514 | 0.390* | |||||
| (0.695) | (0.193) | (0.019) | (omitted) | |||||
| [0.62–2.03] | [0.81–2.83] | [0.18–0.86] | ||||||
| Anxiety (300) in any position (ref: other mental health diagnosis) | 0.686 | 0.836 | 1.193 | 1.828 | ||||
| (0.213) | (0.590) | (0.599) | (0.07) | |||||
| [0.38–1.24] | [0.44–1.61] | [0.62–2.30] | [0.95–3.51] | |||||
| Observations | 370 | 370 | 370 | 370 | 370 | 370 | 370 | 370 |
| Log likelihood | −220.7 | −165.9 | −176.4 | −165.0 | −222.9 | −160.7 | −176.2 | −166.6 |
| χ2 | 50.59 | 25.48 | 29.34 | 27.99 | 50.15 | 39.25 | 33.28 | 27.00 |
| Pseudo R2 | 0.115 | 0.0903 | 0.0928 | 0.0804 | 0.106 | 0.118 | 0.0938 | 0.0717 |
Note. Bonferroni correction applied. Omitted refers to variables excluded from the regression model due to multicollinearity. PCP: primary care physicians; HMO: health maintenance organization.
*p < .05. **p < .01. ***p < .001.
Furthermore, the likelihood of receiving care by clinician specialty was significantly associated with number of co-occurring psychiatric disorders. Treatment-seeking patients with three diagnoses had a 2.9 and 4.7 times greater likelihood of receiving care from PCPs and psychiatrists, respectively (p < .01) and a lower likelihood of receiving care from psychologists (p < .001) and social workers (p < .05) compared with treatment-seeking patients with one clinical diagnosis. Likewise, patients with four or more co-occurring disorders had almost six times (p < .001) greater likelihood of receiving care from a PCP.
Discussion
Despite the wealth of literature on the association between psychiatric and addictive disorders and gambling disorders (Dowling et al., 2015; Kessler et al., 2008), there are still very little data about pathological gamblers seeking treatment (Winters & Kushner, 2003). Prior research assessed self-reported comorbidity prevalence of psychiatric disorders in pathological gamblers seeking treatment in outpatient settings (Ibanez et al., 2001; Kausch, 2003; Specker, Carlson, Edmonson, Johnson, & Marcotte, 1996). To the best of our knowledge, this is the only study that has been conducted using a representative sample of pathological gamblers seeking treatment across all levels of care. In addition, this study is the most comprehensive examination of comorbid psychiatric and psychoactive substance use disorders among treatment-seeking pathological gamblers and assessment of treatment provision by clinician specialty conducted to date.
Study results show that anxiety disorders, episodic mood disorders, depressive disorders, and psychoactive substance disorders are prevalent co-occurring conditions among pathological gamblers seeking treatment for mental health and substance use disorders. This study found that one in four treatment-seeking patients with a principal diagnosis of PG had a concurrent diagnosis of anxiety disorders and mood disorders. In addition, one in five patients with a principal diagnosis of PG had a concurrent diagnosis of substance use disorders. In a prior study, Ibanez et al. (2001) assessed frequency of psychiatric comorbidity among a convenient sample of 69 pathological gamblers who applied to a specialized outpatient treatment program. A little over two in five pathological gamblers self-reported having a concurrent personality disorder and one in three self-reported having an alcohol abuse or dependence disorder (Ibanez et al., 2001).
Overall, prevalence rates of psychiatric and substance use disorders found in this study are lower than in previous studies, which may be related with some important methodological differences. First, this study focused on the most severe form of disordered gambling (i.e., PG as opposed to problem gambling). Second, this study included treatment-seeking patients with a clinical diagnosis of PG based on ICD-9 codes rather than DSM-IV Axis I disorders. Third, study findings have to be interpreted within the context of the US health-care system. Most previous studies assessing prevalence of co-occurring conditions among disordered gamblers seeking treatment were conducted in countries with universal health insurance coverage where patients have access to a broad range of publicly funded health-care services and treatment providers.
In 2015, two thirds of the population in MA had health-care coverage through private commercial plans and 4 in 10 commercially insured residents were enrolled in an HMO. HMOs offer a broad range of health-care services through a closed network of preferred providers and a PCP referral is required for HMO enrollees to access specialists. In line with state health insurance figures, this study found that almost two thirds of patients seeking care in the Commonwealth for PG and co-occurring disorders were enrolled in a HMO. Furthermore, study findings show that, compared with any other type of health insurance plan, having health insurance coverage through an HMO was significantly associated with a three times greater likelihood of receiving care from a PCP.
Little is known about the workforce composition and specialty of clinicians providing care for pathological gamblers with concurrent mental health and substance use disorders. Notably, this study found an unbalanced distribution of health-care providers across MA Counties and a shortage of mental health professionals in counties disproportionally affected by the burden of the disease.
Prior research has suggested that disordered gambling is common in primary care settings (Cowlishaw, Merkouris, Chapman, & Radermacher, 2014; Dowling et al., 2014; Pasternak & Fleming, 1999). Nevertheless, clinicians rarely screen for gambling disorders and disordered gamblers seek care for their comorbid conditions rather than their gambling problems (Drebing et al., 2001; Lorains et al., 2011; Sullivan, Arroll, Coster, Abbott, & Adams, 2000; Winters & Kushner, 2003). Kessler et al. (2008) found that almost half of the respondents with a lifetime PG self-reported receiving treatment for psychiatric or substance use problems in their life; whereas, none of them self-reported receiving treatment for gambling problems. Hence, gambling disorders often remain undiagnosed until psychiatric and substance use disorders become overt.
This study found that the probability of receiving care from psychologists, mental health and substance abuse social workers, psychiatrists, and PCPs was significantly associated with patients’ diagnosis and clinical complexity, proxied by the number of concurrent disorders. Furthermore, study findings suggest that treatment-seeking patients did not seek care from family physicians for their gambling problems as their main clinical condition but as a bundle involving multiple disorders and conditions. Hence, study findings suggest the important role of primary care practitioners routinely screening for disordered gambling symptoms and co-occurring addictive behaviors and holistically addressing such behaviors. Therefore, strategies raising awareness among family practitioners may provide a unique opportunity for surveillance, more effective prevention interventions and comprehensive health-care treatment provision.
Finally, study findings suggest that health-care services provision and counseling may be fragmented into therapeutic interventions, such as cognitive behavioral therapy, cognitive therapy, and motivational interventions, typically provided by psychologists, mental health and substance abuse social workers, and mental health counselors and pharmacological treatment typically provided by psychiatrists and PCPs. While the US Food and Drug Administration has not approved a prescription drug for gambling disorders, opioid antagonists, antidepressants, mood stabilizers, and atypical antipsychotics are often prescribed off-label for disordered gamblers seeking treatment. Given the prevalence of co-occurrent mental health and substance use disorders in treatment-seeking patients with diagnosis of PG, prescribers should carefully assess the risk of prescription drug misuse and abuse. Thus, comprehensive and coordinated behavioral therapy and treatment provision remains a requisite for cost-effective care.
Limitations
This study has some limitations common in administrative claims-based studies including coding accuracy and data completeness. Claims data are dependent on professional ICD coding. Diagnoses were based on ICD-9-CM codes recorded in clinical encounters and no chart review was performed. We could not determine whether the medical encounter was for a new or established patient. There is also the possibility of residual confounding due to variables not included in the claims database. For example, payers typically do not capture race and ethnicity information that may influence treatment-seeking behaviors.
This study focused on psychiatrists, non-psychiatrists, mental health and substance use specialists (i.e., psychologists and social workers), and primary care doctors. Efforts were made to identify provider specialty classified as unknown. Provider entity codes and level of care data elements were reviewed as needed. When determination of provider specialty was not possible, the provider specialty was classified as unknown. No imputation approaches were performed.
In 2015, 61% of MA residents had a commercial insurance plan through an employer [Center for Health Information and Analysis (CHIA), 2016]. In addition, 16% and 19% of MA residents received their health insurance coverage through Medicare and Medicaid (i.e., MassHealth), respectively. The MA APCD includes residents with primary health-care coverage through the top 16 commercial payers in the Commonwealth. In 2013, the MA APCD medical and pharmaceutical claims data represented 89.5% and 83.8% of health-care expenditures, respectively (CHIA, 2016). This study focused on the commercially insured population seeking care in MA. This limits the generalizability of study findings to uninsured or non-commercially insured populations or other jurisdictions.
Study results show that PG is comorbid with mental health and substance use disorders. The cross-sectional nature of this study precludes a temporal association between these disorders. It may be that some mental health and substance use disorders are risk factors for PG; whereas, others might be a consequence of a PG disorder. Similarly, we cannot unequivocally determine whether patients sought care for their gambling problems or the underlying co-occurring mental health and substance use disorders. In spite of these limitations, administrative claims data are real-world valuable and a relatively inexpensive data source.
Conclusions
Study results show both the clinical complexity and the wide range of comorbid psychiatric and behavioral addictions among pathological gamblers seeking treatment and suggest the need for a more integrated and comprehensive provision of care. The likelihood of receiving care for PG and co-occurrent psychiatric and substance use disorders significantly varies by clinical diagnosis and number of comorbid conditions. Mental health and substance use providers may play a key role in identifying and addressing disordered gambling and co-occurring addictive behaviors. Study findings have the potential to illuminate public policies and interventions on more effective treatment provision and future projections about requisite workforce composition.
Acknowledgements
The authors would like to thank the Massachusetts Center for Health Information and Analysis (CHIA), and specially thank Adam Tapply and Sylvia Hobbs for their help through the All-Payer Claim Data application process.
Funding Statement
Funding sources: This research was partially funded by the Massachusetts Gaming Commission in Boston, MA. The Massachusetts Gaming Commission did not participate in any aspects of the research process, drafting, or editing of the manuscript. The findings, interpretations, and conclusions expressed in this manuscript are entirely those of the authors and do not represent the views of the Massachusetts Gaming Commission.
Authors’ contribution
RR-M conceived and designed the study, conducted analysis, and drafted the manuscript. ME participated in the study design, analysis, and contributed to the manuscript revision. ME worked under RR-M supervision. RV contributed to interpretation of results and revised the manuscript. All authors read and approved final manuscript.
Conflict of interest
All authors declare no conflict of interest.
References
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (DSM-IV-TR, 4th ed., text rev.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Boothby C. A., Kim H. S., Romanow N. K., Hodgins D. C., McGrath D. S. (2017). Assessing the role of impulsivity in smoking & non-smoking disordered gamblers. Addictive Behaviors, 70, 35–41. doi:10.1016/j.addbeh.2017.02.002 [DOI] [PubMed] [Google Scholar]
- Center for Health Information and Analysis [CHIA]. (2016). MA APCD, Supplemental payer data. September, 2015. Enrollment trends CHIA. Retrieved from http://archives.lib.state.ma.us/bitstream/handle/2452/422858/ocn956459428-2016-02.pdf?sequence=1&isAllowed=y
- Chou K. L., Afifi T. O. (2011). Disordered (pathologic or problem) gambling and axis I psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. American Journal of Epidemiology, 173(11), 1289–1297. doi:10.1093/aje/kwr017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowlishaw S., Merkouris S., Chapman A., Radermacher H. (2014). Pathological and problem gambling in substance use treatment: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 46(2), 98–105. doi:10.1016/j.jsat.2013.08.019 [DOI] [PubMed] [Google Scholar]
- Dowling N. A., Cowlishaw S., Jackson A. C., Merkouris S. S., Francis K. L., Christensen D. R. (2015). Prevalence of psychiatric co-morbidity in treatment-seeking problem gamblers: A systematic review and meta-analysis. The Australian and New Zealand Journal of Psychiatry, 49(6), 519–539. doi:10.1177/0004867415575774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowling N. A., Jackson A. C., Suomi A., Lavis T., Thomas S. A., Patford J., Harvey P., Battersby M., Koziol-McLain J., Abbott M., Bellringer M. E. (2014). Problem gambling and family violence: Prevalence and patterns in treatment-seekers. Addictive Behaviors, 39(12), 1713–1717. doi:10.1016/j.addbeh.2014.07.006 [DOI] [PubMed] [Google Scholar]
- Dowling N. A., Merkouris S. S., Lorains F. K. (2016). Interventions for comorbid problem gambling and psychiatric disorders: Advancing a developing field of research. Addictive Behaviors, 58, 21–30. doi:10.1016/j.addbeh.2016.02.012 [DOI] [PubMed] [Google Scholar]
- Drebing C. E., Mello A., Penk W., Krebs C., Van Ormer E., Peterson R. L., Federman E. J. (2001). Clinical care of gambling disorders: Training, experience, and competence among VHA psychologists. Journal of Gambling Studies, 17(2), 117–136. doi:10.1023/A:1016668429311 [DOI] [PubMed] [Google Scholar]
- Grant J. E., Levine L., Kim D., Potenza M. N. (2005). Impulse control disorders in adult psychiatric inpatients. American Journal of Psychiatry, 162(11), 2184–2188. doi:10.1176/appi.ajp.162.11.2184 [DOI] [PubMed] [Google Scholar]
- Ibanez A., Blanco C., Donahue E., Lesieur H. R., Perez de Castro I., Fernandez-Piqueras J. (2001). Psychiatric comorbidity in pathological gamblers seeking treatment. American Journal of Psychiatry, 158(10), 1733–1735. doi:10.1176/ajp.158.10.1733 [DOI] [PubMed] [Google Scholar]
- Johansson A., Grant J. E., Kim S. W., Odlaug B. L., Götestam K. G. (2009). Risk factors for problematic gambling: A critical literature review. Journal of Gambling Studies, 25(1), 67–92. doi:10.1007/s10899-008-9088-6 [DOI] [PubMed] [Google Scholar]
- Kausch O. (2003). Patterns of substance abuse among treatment-seeking pathological gamblers. Journal of Substance Abuse Treatment, 25(4), 263–270. doi:10.1016/S0740-5472(03)00117-X [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Hwang I., LaBrie R., Petukhova M., Sampson N. A., Winters K. C., Shaffer H. J. (2008). DSM-IV pathological gambling in the National Comorbidity Survey Replication. Psychological Medicine, 38(9), 1351–1360. doi:10.1017/S0033291708002900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S. W., Grant J. E., Eckert E. D., Faris P. L., Hartman B. K. (2006). Pathological gambling and mood disorders: Clinical associations and treatment implications. Journal of Affective Disorders, 92(1), 109–116. doi:10.1016/j.jad.2005.12.040 [DOI] [PubMed] [Google Scholar]
- Lorains F. K., Cowlishaw S., Thomas S. A. (2011). Prevalence of comorbid disorders in problem and pathological gambling: Systematic review and meta-analysis of population surveys. Addiction, 106(3), 490–498. doi:10.1111/j.1360-0443.2010.03300.x [DOI] [PubMed] [Google Scholar]
- Pasternak A. V., Fleming M. F. (1999). Prevalence of gambling disorders in a primary care setting. Archives of Family Medicine, 8(6), 515–520. doi:10.1001/archfami.8.6.515 [DOI] [PubMed] [Google Scholar]
- Petry N. M., Stinson F. S., Grant B. F. (2005). Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry, 66(5), 564–574. doi:10.4088/JCP.v66n0504 [DOI] [PubMed] [Google Scholar]
- Pilver C. E., Libby D. J., Hoff R. A., Potenza M. N. (2013). Problem gambling severity and the incidence of Axis I psychopathology among older adults in the general population. Journal of Psychiatric Research, 47(4), 534–541. doi:10.1016/j.jpsychires.2012.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Specker S. M., Carlson G. A., Edmonson K. M., Johnson P. E., Marcotte M. (1996). Psychopathology in pathological gamblers seeking treatment. Journal of Gambling Studies, 12(1), 67–81. doi:10.1007/BF01533190 [DOI] [PubMed] [Google Scholar]
- Sullivan S., Arroll B., Coster G., Abbott M., Adams P. (2000). Problem gamblers: Do GPs want to intervene? New Zealand Medical Journal, 113, 204–207. [PubMed] [Google Scholar]
- Suomi A., Dowling N. A., Jackson A. C. (2014). Problem gambling subtypes based on psychological distress, alcohol abuse and impulsivity. Addictive Behaviors, 39(12), 1741–1745. doi:10.1016/j.addbeh.2014.07.023 [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2010). Census. Geography-Massachusetts: Population, Housing Units, Area, and Density: 2010 – State – County. Retrieved from http://www.census.gov (April 8, 2017).
- Welte J. W., Barnes G. M., Wieczorek W. F., Tidwell M. C., Parker J. (2002). Gambling participation in the U.S.—Results from a national survey. Journal of Gambling Studies, 18(4), 313–337. doi:10.1023/A:1021019915591 [DOI] [PubMed] [Google Scholar]
- Winters K. C., Kushner M. G. (2003). Treatment issues pertaining to pathological gamblers with a comorbid disorder. Journal of Gambling Studies, 19(3), 261–277. doi:10.1023/A:1024203403982 [DOI] [PubMed] [Google Scholar]