Abstract
Background:
The Schöttle point is commonly used for anatomic femoral tunnel placement during medial patellofemoral ligament (MPFL) reconstruction. This technique has not been previously validated in the skeletally immature patient, in whom femoral tunnel placement may put the distal femoral physis at risk of iatrogenic injury.
Hypothesis:
Interobserver reliability for femoral tunnel placement will be higher in adult knees compared with pediatric knees.
Study Design:
Cross-sectional study (diagnosis); Level of evidence, 3.
Methods:
We selected 30 perfect lateral radiographs for this study: 20 from pediatric knees (mean patient age, 10 years; range, 8-11 years) and 10 from adult knees (mean patient age, 18.5 years; range, 18-23 years). Six observers with varying levels of clinical experience evaluated each radiograph and approximated the site of the MPFL femoral tunnel using the Schöttle technique. Intra- and interobserver reliabilities for femoral tunnel placement were evaluated. Statistical analysis was used to compare measurements.
Results:
During initial interobserver measurements, the diameter of the composite perfect circles averaged 9.0 and 6.8 mm in adult and pediatric knees, respectively (P = .004). At repeat measurement, circles averaged 9.8 and 7.3 mm in adult and pediatric knees, respectively (P = .0001). Femoral tunnel placement intraobserver variance averaged 2.9 mm in adult knees (range, 1.9-4.0 mm) and 2.3 mm in pediatric knees (range, 1.9-2.9 mm). This difference was not significant (P = .14).
Conclusion:
This study demonstrated that interobserver variance is actually greater in adult knees compared with pediatric knees, although interobserver variance was significantly different for both populations. Additionally, intraobserver variance is small on repeat measures, demonstrating that the Schöttle technique is reproducible for individual observers. Sources of this increased variance between observers are differences in agreement on the bony landmarks required for the Schöttle technique. Due to this variability in tunnel placement, we recommend caution when the Schöttle technique is used in pediatric knees to avoid iatrogenic injury to the distal femoral physis during femoral tunnel placement.
Keywords: medial patellofemoral ligament, patellar instability, radiographic, reconstruction, pediatric, skeletally immature
Recurrent patellofemoral instability is not uncommon.11 After an index patellar dislocation, the rate of recurrence of patellofemoral instability is estimated to be anywhere from 15% to 44%.2–4,12,14–18,31 Reconstruction of the medial patellofemoral ligament (MPFL) has become an option to address patients with recurrent patellofemoral instability. Biomechanical studies have shown the MPFL to be the most important soft tissue restraint to lateral displacement of the patella.5,7 In knees with incompetence of the MPFL following patellofemoral instability, anatomic MPFL reconstruction can successfully stabilize the patellofemoral articulation.6,13,23,24,26 Traditionally, patellofemoral instability in skeletally immature patients has been addressed with nonanatomic soft tissue and/or bony realignment procedures. However, anatomic reconstruction of the MPFL can be difficult in the pediatric population, as the MPFL femoral attachment lies in close proximity to the distal femoral physis.9,19–22 Nonanatomic reconstruction of the MPFL can result in altered patellofemoral contact pressures and recurrent patellofemoral instability. Specifically, malpositioning of the MPFL femoral attachment has been implicated as a major cause of graft failure and poor patient outcomes.27,28
To assist with anatomic placement of the MPFL at the femoral attachment site, Schöttle et al28 described a radiographic method for identification of the MPFL on lateral radiographic images of the knee. This radiographic landmark, known as the Schöttle point, has been extensively studied in the adult population.25 However, the Schöttle point has been less studied in the pediatric population. The importance of correctly identifying the Schöttle point is arguably more significant in the pediatric population given the relationship of the MPFL femoral attachment to the distal femoral physis.9,19,29,30 Iatrogenic injury to the distal femoral physis could potentially result in limb length discrepancy or angular deformity of the lower extremity.
The purpose of this study was to evaluate the interobserver and intraobserver reliability of the Schöttle point as a radiographic landmark for the femoral attachment of the MPFL in the pediatric population. We hypothesized that interobserver reliability would be higher in adult knees compared with pediatric knees.
Methods
This study was approved by the Cleveland Clinic Institutional Review Board. We identified true lateral radiographic images from 20 pediatric and 10 adult patients for this study. Radiographic images were obtained at random by reviewing the electronic medical record for true lateral images in both adult and pediatric patients presenting for outpatient orthopaedic evaluation for knee complaints. Patients were included if lateral radiographs were in neutral rotation, defined by perfect supposition of the femoral condyles, and had open growth plates (for our pediatric cohort). Patients were excluded if the lateral radiographic images were inappropriately rotated or if there was radiographic evidence of either osseous deformity or prior surgery.
The lateral radiographic images were distributed to 6 observers of varying clinical experience to perform clinical measurements. These included 2 fellowship-trained sports medicine specialists (L.D.F., S.G.K.), 1 fellowship-trained pediatric sports medicine specialist (P.S.), 1 orthopaedic sports medicine fellow (K.L.H.), a second-year orthopaedic surgery resident (U.G.O.), and a second-year medical student with an interest in orthopaedic surgery (C.L.W.). The set of 30 radiographs were given to each individual in a random order. Each reviewer was also given the original article from Schöttle et al28 describing the technique for identifying the MPFL attachment site on lateral radiographic images. We requested each reviewer to draw all of the landmarks as described by Schöttle et al28 to determine the location of the MPFL femoral attachment site (Figure 1). Each reviewer then placed a mark at the estimated site of the MPFL femoral attachment sight (Figure 2). Each reviewer assessed and marked the same 30 radiographs approximately 1 month after completion of the initial measurements. The radiographs were distributed in a different order to promote further randomization. To determine interobserver reliability, we constructed an overlay of each reviewer’s estimated site of the MPFL femoral attachment. Once all points were displayed in a composite fashion, a true-fit circle was constructed to include all points as described by Schöttle et al28 (Figure 2). A true-fit circle implies that the smallest possible circle that included all points was used. The diameter of the true-fit circle was then measured to determine test-retest variability between observers. This was repeated for all 30 radiographic images. Intraobserver reliability was determined by measuring the distance between points made by each observer on repeat measures (Figure 3). We used a paired Student t test for all statistical analysis. The P value was set at a significance level of .05.
Figure 1.
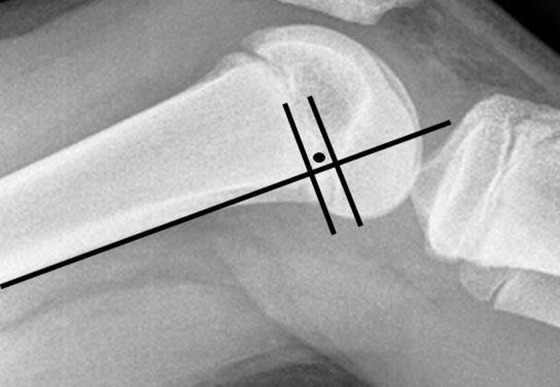
Example of the Schöttle technique.
Figure 2.
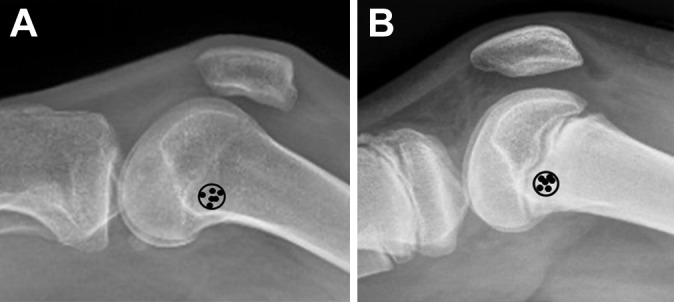
Example of interobserver evaluation using true-fit circle in (A) an adult knee and (B) a pediatric knee. All observer markings were placed in composite.
Figure 3.

Example of intraobserver measurements in (A) an adult knee and (B) a pediatric knee.
Results
The mean age of our participants was 10 years for those with pediatric knees and 18.5 years for those with adult knees. When we evaluated the true-fit circles for interobserver reliability, the diameter of our true-fit circles averaged 6.8 mm in the pediatric knees and 9.0 mm in adult knees, indicating greater variability between observers in adult knees (Table 1). This was a significant difference (P = .004). With repeat measurement, true-fit circle diameter averaged 7.3 mm and 9.8 mm in pediatric and adult knees, respectively (P = .0001) (Table 1). With respect to intraobserver reliability, femoral tunnel placement variance on repeat measures averaged 2.3 mm in pediatric knees (range, 1.9-2.9 mm) (Table 2) and 2.9 mm in adult knees (range, 1.9-4.0 mm) (Table 3). This difference was not significant (P = .14).
TABLE 1.
Interobserver Measures of True-Fit Circles (in mm)a
| Initial Measure | Repeat Measure | |||
|---|---|---|---|---|
| Image No. | Adult | Pediatric | Adult | Pediatric |
| 1 | 7.083 | 5.508 | 6.85 | 7.603 |
| 2 | 8.406 | 6.035 | 7.286 | 6.611 |
| 3 | 6.972 | 8.884 | 10.557 | 8.234 |
| 4 | 7.888 | 6.606 | 8.891 | 7.242 |
| 5 | 8.526 | 5.962 | 12.329 | 6.978 |
| 6 | 12.802 | 6.17 | 12.158 | 6.238 |
| 7 | 9.69 | 5.827 | 10.202 | 7.403 |
| 8 | 7.391 | 7.087 | 7.753 | 6.816 |
| 9 | 7.407 | 5.588 | 7.694 | 6.428 |
| 10 | 13.878 | 6.106 | 14.522 | 6.583 |
| 11 | 7.789 | 7.792 | ||
| 12 | 7.477 | 8.121 | ||
| 13 | 5.819 | 7.014 | ||
| 14 | 6.526 | 6.667 | ||
| 15 | 6.667 | 6.88 | ||
| 16 | 8.634 | 8.483 | ||
| 17 | 7.955 | 8.386 | ||
| 18 | 4.96 | 5.055 | ||
| 19 | 6.408 | 7.978 | ||
| 20 | 10.701 | 9.878 | ||
| Mean | 9.0043 | 6.83545 | 9.8242 | 7.3195 |
| SD | 2.43708 | 1.38858 | 2.57027 | 1.03835 |
aThe diameter of the true-fit circle encompassing all 6 observer markings was measured for 10 adult and 20 pediatric images.
TABLE 2.
Intraobserver Measurement Variance (in mm) for Pediatric Kneesa
| Image No. | SMS1 | MS | Fellow | SMS2 | OSMR | PSMS |
|---|---|---|---|---|---|---|
| 1P | 0.0 | 4.5 | 2.4 | 1.5 | 1.6 | 2.1 |
| 2P | 3.9 | 4.1 | 2.7 | 2.8 | 4.5 | 2.8 |
| 3P | 3.2 | 2.1 | 0.9 | 0.7 | 1.9 | 2.5 |
| 4P | 3.4 | 0.0 | 1.9 | 2.3 | 1.5 | 0.8 |
| 5P | 0.0 | 1.6 | 0.0 | 1.8 | 4.9 | 1.7 |
| 6P | 2.8 | 1.8 | 2.0 | 2.5 | 1.8 | 1.7 |
| 7P | 4.5 | 3.0 | 2.3 | 2.3 | 3.1 | 1.7 |
| 8P | 3.2 | 2.7 | 1.5 | 2.6 | 1.9 | 1.6 |
| 9P | 2.8 | 3.1 | 2.7 | 0.9 | 0.9 | 1.0 |
| 10P | 3.9 | 2.7 | 2.5 | 2.6 | 1.9 | 2.6 |
| 11P | 2.6 | 4.7 | 3.0 | 1.8 | 1.5 | 3.3 |
| 12P | 1.5 | 2.5 | 3.0 | 3.6 | 4.3 | 2.4 |
| 13P | 0.0 | 2.1 | 2.7 | 4.3 | 1.8 | 1.1 |
| 14P | 2.2 | 1.9 | 2.0 | 2.5 | 1.1 | 2.5 |
| 15P | 3.1 | 2.5 | 2.0 | 3.3 | 2.4 | 2.6 |
| 16P | 3.7 | 2.0 | 5.1 | 1.5 | 2.0 | 0.7 |
| 17P | 2.1 | 2.3 | 2.3 | 4.0 | 1.6 | 2.2 |
| 18P | 3.7 | 1.5 | 2.3 | 0.0 | 0.9 | 1.8 |
| 19P | 3.5 | 3.6 | 0.7 | 1.4 | 3.8 | 1.5 |
| 20P | 7.4 | 1.2 | 0.0 | 1.8 | 2.6 | 1.2 |
| Mean | 2.9 | 2.5 | 2.1 | 2.2 | 2.3 | 1.9 |
| SD | 1.7066 | 1.13577 | 1.14064 | 1.0901 | 1.19824 | 0.71884 |
aMS, medical student; OSMR, orthopaedic sports medicine resident; PSMS, pediatric sports medicine specialist; SMS, sports medicine specialist.
TABLE 3.
Intraobserver Measurement Variance (in mm) for Adult Kneesa
| Image No. | SMS1 | MS | Fellow | SMS2 | OSMR | PSMS |
|---|---|---|---|---|---|---|
| 1A | 0.0 | 1.3 | 3.5 | 2.4 | 3.7 | 2.7 |
| 2A | 0.0 | 2.7 | 1.9 | 2.0 | 3.0 | 1.4 |
| 3A | 0.0 | 3.0 | 2.5 | 2.8 | 3.9 | 1.8 |
| 4A | 0.0 | 2.1 | 3.5 | 2.2 | 3.9 | 2.9 |
| 5A | 2.5 | 6.4 | 2.8 | 2.9 | 2.4 | 1.7 |
| 6A | 3.4 | 1.4 | 1.8 | 0.0 | 2.0 | 0.0 |
| 7A | 2.0 | 9.2 | 1.8 | 2.7 | 3.5 | 7.0 |
| 8A | 2.0 | 0.0 | 3.5 | 2.9 | 3.0 | 2.8 |
| 9A | 4.0 | 3.6 | 3.7 | 1.7 | 2.3 | 3.4 |
| 10A | 5.4 | 10.7 | 5.1 | 2.7 | 6.5 | 2.1 |
| Mean | 1.9 | 4.0 | 3.0 | 2.2 | 3.4 | 2.6 |
| SD | 1.9 | 3.6 | 1.1 | 0.9 | 1.3 | 1.8 |
aMS, medical student; OSMR, orthopaedic sports medicine resident; PSMS, pediatric sports medicine specialist; SMS, sports medicine specialist.
Discussion
Recurrent patellar dislocations can become a significant issue for patients who cannot tolerate symptomatic instability. In patients with relatively normal bony anatomic structure and alignment, reconstruction of the medial patellofemoral ligament has become a popular option to restore patellofemoral stability. The importance of the MPFL is its function as a checkrein during the first 30° to 40° of knee flexion to guide the patella into the trochlear groove.1,8 Injury of this ligament has been implicated in recurrent patellofemoral instability.23 Successful anatomic reconstruction of the MPFL requires accurate identification of the native MPFL attachment sights. The MPFL femoral attachment lies along a bony ridge that is situated on the medial aspect of the distal femur between the adductor tubercle and the medial epicondyle.9 The femoral attachment of the MPFL also has an intimate relationship with the distal femoral physis.9,29,30 Farrow et al9 demonstrated that the MPFL femoral attachment is situated just distal to the medial aspect of the distal femoral physis. Due to its close association to the distal femoral physis, the growth plate is at risk during placement of the femoral tunnel during MPFL reconstruction in the pediatric patient. To add to the difficulty of safe anatomic femoral tunnel placement, the distal femoral physis has an undulating pattern, making interpretation of this structure difficult when lateral radiographic images are viewed.
To assist with anatomic reconstruction of the MPFL, Schöttle et al28 described a technique for identifying the femoral attachment site of the MPFL on a lateral radiographic image. The Schöttle technique has been widely used in the adult population; however, use of this technique is more difficult in the pediatric patient. The aim of the present study was to evaluate the Schöttle technique of locating the distal femoral attachment in the pediatric population and comparing that with an adult control group.
The principal findings of our study demonstrate that the interobserver reliabilities for both pediatric and adult groups were significantly different at both time points. The intraobserver reliability showed no significant difference. We hypothesized that interobserver reliability would be better when the Schöttle technique was used in skeletally mature individuals. We believed that the presence of the distal femoral physis on the lateral radiographic image would influence where markings were made when the Schöttle technique was used. Furthermore, the osseous landmarks in the pediatric knee are not always as distinct as those found in the adult patient. Specifically, the point where the Blumensaat line intersects the posterior femoral cortex is sometimes less distinct in pediatric knees than in adult knees. In addition, the point where the posterior femoral condyle meets the posterior femoral cortex is often not distinct, as this is near the posterior aspect of the distal femoral physis on a lateral radiographic image. These radiographic landmarks are integral when the Schöttle technique is used. Based on the results of our study, presence of the distal femoral physis may actually assist with lesser variability in femoral tunnel placement between observers when using the Schöttle technique. Due to recent descriptions of the relationship of the MPFL femoral attachment to the distal femoral physis, observers may be more likely to err toward more consistent placement of the MPFL femoral tunnel, as it is understood that this point is always distal to the physis.9,29,30
Conversely, variability was much less for each observer when using the Schöttle technique. It can be assumed that one generally uses the same landmarks from measurement to measurement and thus the intraobserver reliability is less susceptible to retest variability. The variation in our interobserver measurements can be associated with how each individual interprets the landmarks needed to identify the Schöttle point. For example, the anterior and posterior variance of femoral tunnel placement is related to the posterior cortical line. We did not standardize the amount of the femoral shaft that was included in the radiographs. The different radii of curvature for each individual femur, especially in the mature participants, could have affected where the individual observers measured their posterior cortical line and thus have affected their measurements. Small deviations in angulation of this posterior cortical line could certainly alter placement of the femoral tunnel in the anterior-posterior direction (Figure 4).
Figure 4.
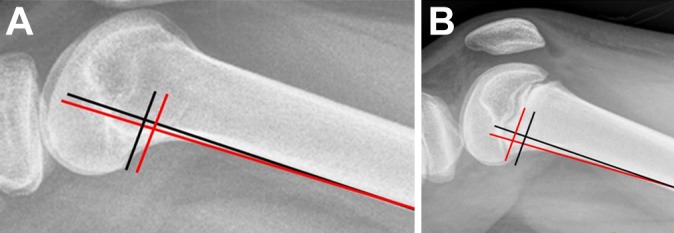
Example of landmark variability between observers in (A) an adult and (B) a pediatric knee. Horizontal line variability (as determined by perceived location of the posterior aspect of the condyle) in placement can result in anterior-posterior variability in tunnel placement. Vertical line variability (determined by perceived location of the posterior cortex) in placement can result in proximal-distal variability in tunnel placement.
Proximal-to-distal orientation is related to where the femoral condyle meets the posterior cortex of the femur. This can be affected by rotation of the radiograph if a nonperfect lateral image is used. We tried to eliminate this variable by using only perfect radiographs. Each observer may interpret differently the location of the transition point between the posterior condyle and the posterior femoral cortex, which might certainly have accounted for the interobserver differences and the intraobserver consistency (Figure 4). Additionally, the posterior-most extent of the Blumensaat line is used to confirm proximal-distal placement of the femoral tunnel. The morphological appearance of this area has been shown by Farrow et al10 to differ on lateral radiographic images. These authors showed that the Blumensaat line can have an indistinct appearance in certain individuals. This could also have accounted for the variations in inter- and intraobserver reliability.
Our study has several weaknesses. Because this was a pure radiographic study, we could not reference accuracy as it relates to the anatomic footprint of the native MPFL, but this was not the intention of this study. Our purpose was to evaluate the reproducibility of the Schöttle technique in pediatric versus adult knees. We also did not assess the relationship between tunnel location and the distal femoral physis, as we did not want the presence of the physis to influence where each reviewer placed the mark for the femoral tunnel. Last, we did not determine inter- and intraobserver reliabilities for the lines used to determine tunnel position. No standardized method exists for line placement with respect to the length of the lines or the angle at which the lines are placed. As such, it would have been difficult to accurately analyze test-retest reliability when there are so many variables (ie, linear distance and line angulation).
In conclusion, the Schöttle point is a reasonable technique to identify the correct placement of the femoral tunnel for MPFL reconstruction. This technique is reproducible in the adult population both within the same observer and between different observers. This is the first study evaluating the inter- and intraobserver reliabilities of the Schöttle technique in the pediatric population. Care should be taken when using the Schöttle technique for placement of the MPFL femoral tunnel in pediatric patients to avoid iatrogenic injury to the distal femoral physis. The Schöttle technique can be a useful tool for approximation of femoral tunnel placement in the pediatric knee. However, fluoroscopy in both the anteroposterior and lateral planes should be used as another check to confirm that the femoral tunnel is appropriately placed so as to prevent injury to the distal femoral physis.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was waived by the Cleveland Clinic Institutional Review Board.
References
- 1. Carrillon Y, Abidi H, Dejour D, Fantino O, Moyen B, Tran-Minh VA. Patellar instability: assessment on MR images by measuring the lateral trochlear inclination-initial experience. Radiology. 2000;216(2):582–585. [DOI] [PubMed] [Google Scholar]
- 2. Cash JD, Hughston JC. Treatment of acute patellar dislocation. Am J Sports Med. 1988;16(3):244–249. [DOI] [PubMed] [Google Scholar]
- 3. Christiansen SE, Jakobsen BW, Lund B, Lind M. Isolated repair of the medial patellofemoral ligament in primary dislocation of the patella: a prospective randomized study. Arthroscopy. 2008;24(8):881–887. [DOI] [PubMed] [Google Scholar]
- 4. Cofield RH, Bryan RS. Acute dislocation of the patella: results of conservative treatment. J Trauma. 1977;17(7):526–531. [DOI] [PubMed] [Google Scholar]
- 5. Conlan T, Garth WP, Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75(5):682–693. [DOI] [PubMed] [Google Scholar]
- 6. Davis DK, Fithian DC. Techniques of medial retinacular repair and reconstruction. Clin Orthop Relat Res. 2002;(402):38–52. [DOI] [PubMed] [Google Scholar]
- 7. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59–65. [DOI] [PubMed] [Google Scholar]
- 8. Farahmand F, Senavongse W, Amis AA. Quantitative study of the quadriceps muscles and trochlear groove geometry related to instability of the patellofemoral joint. J Orthop Res. 1998;16(1):136–143. [DOI] [PubMed] [Google Scholar]
- 9. Farrow LD, Alentado VJ, Abdulnabi Z, Gilmore A, Liu RW. The relationship of the medial patellofemoral ligament attachment to the distal femoral physis. Am J Sports Med. 2014;42(9):2214–2218. [DOI] [PubMed] [Google Scholar]
- 10. Farrow LD, Chen MR, Cooperman DR, Goodfellow DB, Robbin MS. Radiographic classification of the femoral intercondylar notch posterolateral rim. Arthroscopy. 2008;24(10):1109–1114. [DOI] [PubMed] [Google Scholar]
- 11. Fithian DC, Paxton EW, Cohen AB. Indications in the treatment of patellar instability. J Knee Surg. 2004;17(1):47–56. [DOI] [PubMed] [Google Scholar]
- 12. Garth WP, Jr, Pomphrey M, Jr, Merrill K. Functional treatment of patellar dislocation in an athletic population. Am J Sports Med. 1996;24(6):785–791. [DOI] [PubMed] [Google Scholar]
- 13. Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM. Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res. 1998;(349):174–182. [DOI] [PubMed] [Google Scholar]
- 14. Hawkins RJ, Bell RH, Anisette G. Acute patellar dislocations: the natural history. Am J Sports Med. 1986;14(2):117–120. [DOI] [PubMed] [Google Scholar]
- 15. Larsen E, Lauridsen F. Conservative treatment of patellar dislocations: influence of evident factors on the tendency to redislocation and the therapeutic result. Clin Orthop Relat Res. 1982;(171):131–136. [PubMed] [Google Scholar]
- 16. Maenpaa H, Huhtala H, Lehto MU. Recurrence after patellar dislocation: redislocation in 37/75 patients followed for 6-24 years. Acta Orthop Scand. 1997;68(5):424–426. [DOI] [PubMed] [Google Scholar]
- 17. Maenpaa H, Lehto MU. Patellar dislocation: the long-term results of nonoperative management in 100 patients. Am J Sports Med. 1997;25(2):213–217. [DOI] [PubMed] [Google Scholar]
- 18. McManus F, Rang M, Heslin DJ. Acute dislocation of the patella in children: the natural history. Clin Orthop Relat Res. 1979;(139):88–91. [PubMed] [Google Scholar]
- 19. Nelitz M, Dornacher D, Dreyhaupt J, Reichel H, Lippacher S. The relation of the distal femoral physis and the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2011;19(12):2067–2071. [DOI] [PubMed] [Google Scholar]
- 20. Nelitz M, Dreyhaupt J, Reichel H, Woelfle J, Lippacher S. Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents with open growth plates: surgical technique and clinical outcome. Am J Sports Med. 2013;41(1):58–63. [DOI] [PubMed] [Google Scholar]
- 21. Nelitz M, Reichel H, Dornacher D, Lippacher S. Anatomical reconstruction of the medial patellofemoral ligament in children with open growth-plates. Arch Orthop Trauma Surg. 2012;132(11):1647–1651. [DOI] [PubMed] [Google Scholar]
- 22. Nguyen CV, Farrow LD, Liu RW, Gilmore A. Safe drilling paths in the distal femoral epiphysis for pediatric medial patellofemoral ligament reconstruction. Am J Sports Med. 2017;45(5):1085–1089. [DOI] [PubMed] [Google Scholar]
- 23. Nomura E. Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop. 1999;23(5):260–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nomura E, Horiuchi Y, Kihara M. A mid-term follow-up of medial patellofemoral ligament reconstruction using an artificial ligament for recurrent patellar dislocation. Knee. 2000;7(4):211–215. [DOI] [PubMed] [Google Scholar]
- 25. Redfern J, Kamath G, Burks R. Anatomical confirmation of the use of radiographic landmarks in medial patellofemoral ligament reconstruction. Am J Sports Med. 2010;38(2):293–297. [DOI] [PubMed] [Google Scholar]
- 26. Sandmeier RH, Burks RT, Bachus KN, Billings A. The effect of reconstruction of the medial patellofemoral ligament on patellar tracking. Am J Sports Med. 2000;28(3):345–349. [DOI] [PubMed] [Google Scholar]
- 27. Schöttle PB, Fucentese SF, Romero J. Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):516–521. [DOI] [PubMed] [Google Scholar]
- 28. Schöttle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801–804. [DOI] [PubMed] [Google Scholar]
- 29. Shea KG, Grimm NL, Belzer J, Burks RT, Pfeiffer R. The relation of the femoral physis and the medial patellofemoral ligament. Arthroscopy. 2010;26(8):1083–1087. [DOI] [PubMed] [Google Scholar]
- 30. Shea KG, Styhl AC, Jacobs JC, Jr, et al. The relationship of the femoral physis and the medial patellofemoral ligament in children: a cadaveric study. Am J Sports Med. 2016;44(11):2833–2837. [DOI] [PubMed] [Google Scholar]
- 31. Sillanpaa PJ, Mattila VM, Maenpaa H, Kiuru M, Visuri T, Pihlajamaki H. Treatment with and without initial stabilizing surgery for primary traumatic patellar dislocation: a prospective randomized study. J Bone Joint Surg Am. 2009;91(2):263–273. [DOI] [PubMed] [Google Scholar]


