Abstract
Background:
A frequently used method to determine the anatomic femoral fixation point in the operating room during medial patellofemoral ligament (MPFL) reconstruction is the radiographic method. However, the ability of this radiological method to establish an anatomic femoral attachment point might not be as accurate as expected.
Purpose:
(1) To evaluate the accuracy of the radiological method to locate the anatomic femoral fixation point in MPFL reconstruction surgery and (2) to determine the factors influencing the predictability of this method to obtain this objective.
Study Design:
Cohort study (diagnosis); Level of evidence, 2.
Methods:
A total of 100 consecutive 3-dimensional computed tomography (3D CT) knee examinations were performed at 0° of extension in 87 patients treated for chronic lateral patellar instability. For each knee, 2 virtual 7 mm–diameter femoral tunnels were created: 1 using the adductor tubercle as a landmark (anatomic tunnel) and the other according to the radiological method described by Schöttle et al (radiographic tunnel). We measured the percentage of overlap between both tunnels. Moreover, of the 100 included knees, 10 were randomly selected for a variability study.
Results:
Considering an overlap area greater than 50% as reasonable, the radiographic method achieved this in only 38 of the 100 knees. Intrarater and interrater reliability were excellent. There was a trend for female patients with severe trochlear dysplasia to have less overlap. This model accounted for 64.2% of the initial variability in the data.
Conclusion:
An exact anatomic femoral tunnel placement could not be achieved with the radiographic method. Radiography provided only an approximation and should not be the sole basis for the femoral attachment location. Moreover, in female patients with severe trochlear dysplasia, the radiographic method was less accurate in determining the anatomic femoral fixation point, although differences were not statistically significant.
Keywords: medial patellofemoral ligament, femoral attachment, MPFL anatomic reconstruction, 3D CT
Medial patellofemoral ligament (MPFL) reconstruction as a treatment for chronic lateral patellar instability is becoming more popular around the world.8 One of the key factors for the success of this surgical procedure is the correct choice of the femoral attachment point.8 The selected femoral attachment point is of utmost importance for MPFL graft length changes during knee flexion and relative graft length.11 Both factors influence the long-term success and failure rates of MPFL reconstruction surgery.11 Establishing an anatomic femoral fixation point during MPFL reconstruction is an easy and reproducible way to achieve an optimal change in the length pattern of the graft, correct isometry, an ideal graft length, and graft stress as well as good long-term clinical results.11 Proper femoral placement restores physiological kinematics and patellofemoral pressure postoperatively.11 To determine the anatomic femoral fixation point in the operating room, the radiographic method described by Schöttle et al12 in 2007 is frequently used. This radiographic method simplifies the operative procedure and allows for a very small skin incision at the femoral side of the knee. However, the precision of this radiological method to establish an anatomic femoral attachment point might not be as accurate as expected.
It has been shown that this radiographic method provides only an approximation and should not be the sole basis for the anatomic femoral attachment location.10 The main limitation of this previous study was that the number of patients in the series was relatively small.10 Another important limitation was the fact that all the different measurements were taken by the same radiologist, and therefore the reproducibility of the method used to determine the femoral attachment location was not evaluated, which could lead to important errors and biases.10
The objectives of this study were (1) to evaluate the radiographic method described by Schöttle et al12 regarding the accuracy of the anatomic location for the femoral fixation point of the MPFL and (2) to determine the factors influencing the predictability of this method to establish an anatomic femoral fixation point. Our main hypothesis was that in most patients with chronic lateral patellar instability, the Schöttle method would not ensure a precise fixation point from an anatomic standpoint in MPFL reconstruction surgery. Our secondary hypothesis was that in a group of female patients with severe dysplasia, which is more surgically demanding, the radiological method would have more failures.
Methods
Patients
Enrolled in this study were 87 patients (65 female, 22 male) treated for chronic lateral patellar instability with at least 2 documented patellar dislocations (Table 1). In 13 patients, the contralateral knee also underwent MPFL reconstruction because of chronic lateral patellar instability with at least 2 documented patellar dislocations. Therefore, the total number of knees analyzed was 100. All knees were preoperatively evaluated for patella alta (Caton-Deschamps index ≥1.2 on lateral knee radiography), tibial tuberosity–trochlear groove (TT-TG) distance on CT, and trochlear dysplasia according to the 4 types of the Dejour1,2 classification on CT. This study was approved by the hospital’s institutional review board (Hospital Universitario y Politécnico La Fe; No. 2013/0341 ). All patients gave their informed consent.
TABLE 1.
Patient Characteristicsa
| Age, mean (range), y | 24 (14-48) |
| Sex, n | |
| Male | 22 |
| Female | 65 |
| Patella alta, No. of knees | 45 |
| Pathological TT-TG distance (>20 mm), No. of knees | 39 |
| TT-TG distance, mean (range), mm | 19.12 (4-33) |
| Trochlear dysplasia, No. of knees | 77 |
| Type A | 12 |
| Type B | 11 |
| Type C | 19 |
| Type D | 35 |
aTT-TG, tibial tuberosity–trochlear groove.
Computed Tomography
A total of 100 consecutive 3-dimensional computed tomography (3D CT) knee examinations were performed. All the knees were imaged with a high–spatial resolution 256–detector row CT scanner (Brilliance iCT; Philips) at 0° of extension. The raw data sets were acquired under 64 × 0.625–mm collimation, rotation time of 0.5 seconds, slice reconstruction thickness of 0.9 mm, pitch of 0.45, 120 kV, and automated mAs control. All patients had the gonads shielded by the placement of a lead apron. Images were reconstructed and transmitted to a picture archiving and communication system (Impax; AGFA HealthCare). A 3D bone surface–rendering knee image was obtained in all of the cases.
Imaging Analysis
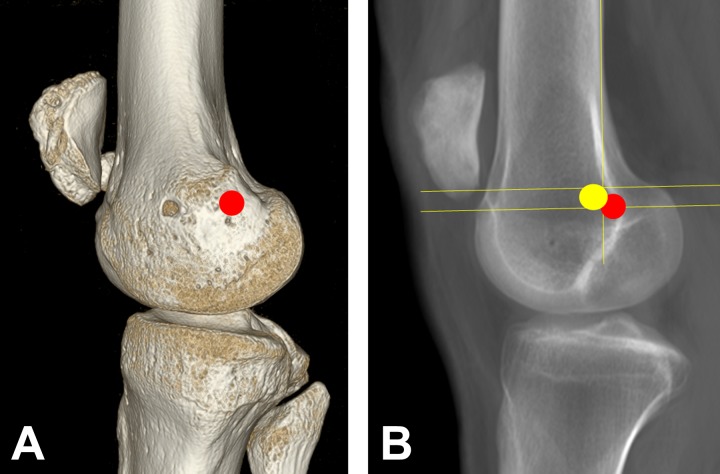
For each knee, 2 virtual 7 mm–diameter femoral tunnels were created “in silico” on the surface-rendering images. One of the tunnels was created using the adductor tubercle as a landmark because it is a well-defined anatomic point of reference and because the relationship between the adductor tubercle and the femoral insertion of the MPFL is constant (∼1 cm).4,15,17,18 This was considered as the anatomic tunnel (Figure 1A). The other was created according the radiological method described by Schöttle et al12 (Figure 1B). This was considered as the radiographic tunnel. We used 7 mm as a fixed standardized diameter because it is the tunnel width normally used in our daily surgical practice. The percentage of the anatomic tunnel covered by the tunnel created according to the Schöttle method was calculated. A simple spatial overlap index, termed the overlap coefficient, was set at 50% to define the minimum overlap to be considered as similar, as the value ranges from 0 (no spatial overlap between the 2 locations) to 1 (complete overlap). The 50% overlap was arbitrarily established to minimize spurious results and maximize clinical similarity in a similar way to the kappa statistic. To measure the percentage of overlap, open-access software (GeoGebra 4.4; https://www.geogebra.org/download) was used according to the technique described previously.10
Figure 1.
Using software analysis, the point calculated on 3-dimensional computed tomography was translated to a 2-dimensional fluoroscopy image. (A) Tunnel created using the adductor tubercle as a landmark (anatomic tunnel) (red circle). (B) Tunnel created according to the radiological method described by Schöttle et al12 (yellow circle).
Recent studies have shown that the femoral insertion of the MPFL is located distal to the adductor tubercle at the midpoint between the medial femoral epicondyle and the adductor tubercle.5,7,15–18 According to Fujino et al,4 the femoral attachment of the MPFL is distal to the apex of the adductor tubercle and parallel to the long axis of the femur; the mean linear distance between the 2 points was 10.6 mm, and the position of the insertion site was consistent in all knees. The great variability in the location of the adductor tubercle explains the variability in the location of the femoral insertion of the MPFL. Therefore, the MPFL must be considered unique for every person. That is, the optimal femoral position is patient specific and must be precisely defined before surgery. Volumetric 3D CT provides the opportunity to locate the adductor tubercle and therefore the location of the femoral attachment point of the MPFL based on the location of the adductor tubercle. According to Schöttle et al,12 the radiographic site of the anatomic MPFL femoral attachment is located, on a true lateral radiograph, 1.3 mm anterior to the tangent line to the posterior femoral cortex, 2.5 mm distal to the perpendicular line drawn through the top of the medial femoral condyle, and proximal to the perpendicular line drawn through the most posterior part of the Blumensaat line. In our study, 3D CT was used to define the Schöttle area by determining the Blumensaat line in the distal femur’s surface-rendering 3D reconstruction after eliminating the contralateral condyle in the image.
Of the 100 included knees, 10 were randomly selected for the variability study. Two radiologists with more than 5 years of experience in musculoskeletal radiology (C.R.-F. and I.E.) performed the measurements. Both radiologists independently measured all 10 of the knees 5 times with a time interval of at least 1 week between each measurement. Both observers were blinded to any additional data. Before performing the measurements, the 2 observers agreed on the precise definitions of the landmarks to be used, according to the anatomic method described by Fujino et al4 and the radiological method described by Schöttle et al.12
Statistical Analysis
All values were expressed as the mean ± SD. A P value of <.05 was considered significant. Interclass and intraclass correlation coefficients (ICCs) were obtained in the 10 randomly chosen knees in the variablilty study. The chi-square test was used to analyze the relationships between an overlap greater than 50% and the major factors of instability (trochlear dysplasia, TT-TG distance >20 mm, and patella alta). Moreover, a multivariate statistical technique (correspondence analysis) was used to analyze the relationship between the categories of variables. To compare the 3 qualitative variables (percentage of overlap, trochlear dysplasia, and sex), contrasts of proportions were used. All statistical analyses were performed using SPSS software version 17 (IBM).
Results
The mean percentage of the overlap area of the femoral tunnel using the radiographic method and the anatomic landmarks was 38.97% ± 23.58% (range, 0%-93%). Considering an overlap area greater than 50% as reasonable, the radiographic method achieved it in only 38 of the 100 knees (38%). The point identified with the radiographic method was located in 92% of the knees anterior and proximal to the point that we considered as anatomic.
The mean percentage of overlap obtained by the 2 observers was 47.1% ± 26.9% and 47.2% ± 31.1%, respectively. The intrarater reliability for the measurement of the percentage of the anatomic tunnel area covered by the femoral tunnel created using the radiographic method was similar for both radiologists: observer 1 ICC = 0.866 (95% CI, 0.716-0.959); observer 2 ICC = 0.862 (95% CI, 0.709-0.957) (Figure 2). With regard to interrater reliability, the ICC was 0.943 (95% CI, 0.800-0.985) (Figure 3).
Figure 2.
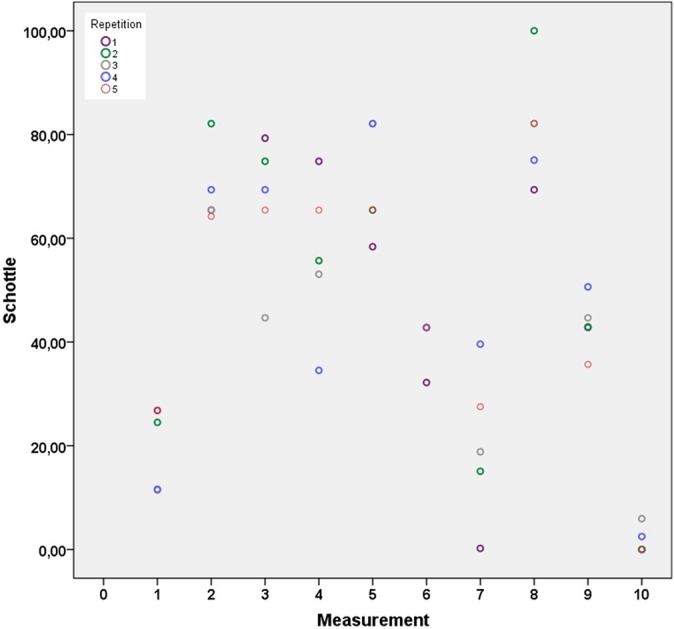
Bland-Altman plot of intrarater reliability.
Figure 3.
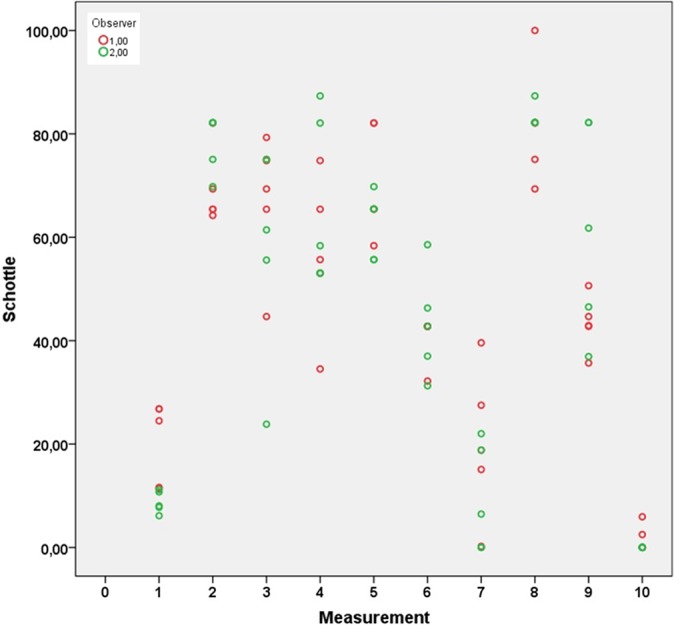
Bland-Altman plot of interrater reliability.
Evaluating the influence of dysplasia on the results, 37% of knees with dysplasia had an overlap area greater than 50% compared with 39% of knees without dysplasia, with the differences being nonsignificant (χ2 = 0.016, P = .898). The percentage was lower (31%) in knees with severe trochlear dysplasia compared with 47% of knees that did not have severe dysplasia. However, these differences were also not statistically significant (χ2 = 2.608, P = .1063).
The influence of patient sex was also statistically nonsignificant. The overlap area was greater than 50% in 44% of male patients compared with 36% of female patients (χ2 = 0.652, P = .419). The area of overlap was greater than 50% in 36% of knees with patella alta compared with 40% of knees that did not have patella alta. However, the differences were not statistically significant (χ2 = 0.126, P = .723).
An area of overlap greater than 50% was observed in only 33% of knees with an increased TT-TG distance (>20 mm) compared with 41% of knees that did not present a pathological TT-TG distance. These differences were also not significant (χ2 = 0.591, P = .442).
Finally, an overlap of more than 50% of the anatomic femoral tunnel was obtained using the radiographic method in only 30% (12/40) of female patients with severe trochlear dysplasia (type C and D) compared with 67% (7/12) of male patients without severe trochlear dysplasia (Z = –1.774, P = .076). The differences were not statistically significant, but a tendency toward significance could be observed (Table 2).
TABLE 2.
Severe Trochlear Dysplasia by Sex
| Tunnel Overlap >50%, % | ||
|---|---|---|
| No | Yes | |
| No | ||
| Male | 41.67 | 58.33 |
| Female | 57.58 | 42.42 |
| Yes | ||
| Male | 66.67 | 33.33 |
| Female | 70.00 | 30.00 |
In the multivariate statistical analysis, none of the analyzed factors (patella alta, TT-TG distance >20 mm, or trochlear dysplasia) had a significant effect on the percentage of overlap greater than 50% of the anatomic femoral tunnel using the radiographic method. Only severe trochlear dysplasia might predict nonoverlapping, although the association was not statistically significant (P = .069). Only severe trochlear dysplasia correlated with no overlaps greater than 50%. This regression model used to analyze the relationship between categories of variables predicting accurate (overlapping) tunnels accounted for 64.2% of the initial variability in the data.
Discussion
Our study confirms that the radiographic method described by Schöttle et al12 did not ensure a precise location, from an anatomic standpoint, of the femoral fixation point in MPFL reconstruction surgery in patients with chronic lateral patellar instability. In most cases, 2-dimensional (2D) radiological methods do not allow for a proper anatomic femoral placement.10 Compared with that study,10 our current investigation has important strengths. First, the number of evaluated knees is larger (30 vs 100, respectively), with the results being more generalizable. Also, an analysis of the interobserver and intraobserver variability of the 2 methods used to identify the femoral fixation point of the MPFL was performed to validate previous results.
Interobserver and intraobserver variability could affect the reliability of the volumetric 3D CT scan analysis to assess the femoral attachment location. Accuracy and reproducibility in radiological results are important because many crucial surgical decisions are often based on the assumption that they represent the truth. Radiologist-dependent factors, among others, might contribute to measurement inconsistencies. In our series, high intraobserver and interobserver consistency was shown. Our findings validate previous results.10 Moreover, our study is in agreement with that of Ziegler et al,19 who demonstrated that even using a pure lateral radiological view as recommended by Schöttle et al,12 the radiological method is not a precise method to determine the anatomic femoral fixation point of the MPFL. In our study, we also used a strict lateral view. In this ideal situation, the authors found a mean distance of 4.1 mm from the anatomic MPFL attachment.19 If the lateral radiograph is not strictly lateral, the error is even greater. Just a small 5° rotation will have a significant effect in determining the anatomic femoral fixation point (7.5-9.2 mm).19
Our study has clinical implications in MPFL reconstruction surgery. The 2D method will frequently produce a nonanatomic femoral tunnel placement. A malpositioned femoral tunnel occurs in between 31% and 64% of MPFL reconstructions.6,13 The determination of the femoral attachment point location in MPFL reconstruction surgery is of major importance because it determines the length change behavior of the graft and therefore the graft tension and patellofemoral compression force at different angles of knee flexion.11 Mistakes in the femoral attachment point have resulted in increased patellofemoral contact pressure, increased rates of MPFL reconstruction failure, and loss of graft isometry.3,9 In the present study, it was observed that certain patients may have had more errors with the 2D method (female patients with trochlear dysplasia), but this was not a significant finding. The clinical relevance of this finding lies in the fact that lateral patellar instability is more frequent in female patients with severe trochlear dysplasia. Moreover, this is the most surgically demanding group and therefore requires a more precise anatomic technique. The reason is simple: the MPFL graft must compensate for the harmful effects of the associated anatomic factors that favor patellar instability.
Fluoroscopy is an ingenious real-time radiographic method that can be most helpful for surgeons who perform this type of surgery very occasionally to avoid gross failures at the time of determining the femoral attachment point in MPFL reconstruction surgery. Although fluoroscopy is extremely variable and prone to errors, it seems to work to some extent when combined with isometry testing. Without advanced 3D imaging, the only accurate way to be sure of an anatomic femoral placement of the graft and to perform accurate MPFL reconstruction is to make a large enough incision to unequivocally identify the most important anatomic landmark: the adductor tubercle.
The femoral insertion of the MPFL is located between the adductor tubercle and the medial epicondyle. It has been observed that the distance between the adductor tubercle and the femoral insertion of the MPFL has lower variations than that between the medial femoral epicondyle and the femoral insertion of the MPFL.17 That is the reason why some authors advocate the use of the adductor tubercle as a landmark for MPFL reconstruction instead of the medial femoral epicondyle.17 Moreover, the adductor tubercle is a well-defined anatomic landmark and therefore easier to identify than the medial femoral epicondyle.17 According to Viste et al,17 the relationship between the adductor tubercle and the femoral insertion of the MPFL is constant (10 mm below). Smirk and Morris15 also found that the femoral insertion of the MPFL is most frequently located 1 cm distal to the adductor tubercle. According to Wijdicks et al,18 the attachment of the MPFL is 8.9 ± 2.0 mm from the adductor tubercle. These findings are in accordance with those observed by Fujino et al,4 who found that the anatomic MPFL femoral attachment point is located 10.6 mm distal to the apex of the adductor tubercle and was also consistent between knees. These are the reasons why the adductor tubercle has been considered the landmark to identify the femoral fixation point of the MPFL in our study.
Fujino et al4 used the adductor tubercle as a landmark to identify the femoral fixation point of the MPFL. Yet, these authors used 3D CT reconstructions of the distal femur. The bone surface anatomy of the medial side of the distal femur is easily detected with 3D CT–reconstructed images. As small-incision surgery is preferred by patients over large-incision surgery, an attractive option would be to use 3D CT technology to locate the anatomic femoral attachment point. With the 3D CT method, we can determine exactly where the adductor tubercle is. 3D CT provides an image similar to what we would find with a surgical dissection of that anatomic area.
As previously mentioned, there is consensus among studies regarding the fact that the distance between the adductor tubercle and the MPFL femoral fixation point, estimated at 1 cm, is constant and uniform between different knees.4,15,17,18 Based on this finding, 3D CT allows us to determine the femoral fixation point of the MPFL for each specific knee. 3D CT allows one to locate the femoral attachment point of the MPFL based on the location of the adductor tubercle. This point that can be exactly determined on 3D CT can be easily extrapolated, through specific software, to a 2D image (see Figure 1). It would be a similar image to what we can obtain with fluoroscopy in the operating room. Therefore, using radioscopy in the operating room, with a strict lateral view, we can identify this fixation point that the radiologist has extrapolated into a 2D image. We would not need a large incision to identify the femoral insertion point; a 1- to 1.5-cm incision would be enough for femoral fixation of the graft. This surgical technique would practically be a percutaneous technique. Thus, 3D CT allows us to perform tailor-made surgery, determining the femoral attachment point location based on anatomy. Our findings are in accordance with those of Siebold and Borbon,14 who recommended individualizing the femoral fixation site, as it varies in each patient.
One limitation of our study is that the test used of contrasts of proportions is only applicable to large sample sizes (n > 30), and the sample size of male patients without severe dysplasia was smaller (n = 12). Therefore, the number of patients, especially male patients without severe dysplasia, should be increased, although the difficulty is that the prevalence of the disease in this group of patients is low.
Conclusion
An exact anatomic femoral tunnel placement could not be achieved with the Schöttle method. Radiographic 2D identification of the femoral graft placement site only provided an approximation and should not be the sole basis for the femoral attachment location. The femoral attachment point must be determined during surgical exposure based on knowledge of the anatomy, and 3D imaging may aid in identifying the appropriate location.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from the Instituto de Investigación Sanitaria La Fe (registration No. 2013/0341).
References
- 1. Dejour D, Le Coultre B. Osteotomies in patellofemoral instabilities. Sports Med Arthrosc. 2007;15:39–46. [DOI] [PubMed] [Google Scholar]
- 2. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. [DOI] [PubMed] [Google Scholar]
- 3. Elias JJ, Cosgarea AJ. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med. 2006;34(9):1478–1485. [DOI] [PubMed] [Google Scholar]
- 4. Fujino K, Tajima G, Yan J, et al. Morphology of the femoral insertion site of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2015;23(4):998–1003. [DOI] [PubMed] [Google Scholar]
- 5. LaPrade MD, Kennedy MI, Wijdicks CA, LaPrade RF. Anatomy and biomechanics of the medial side of the knee and their surgical implications. Sports Med Arthrosc. 2015;23(2):63–70. [DOI] [PubMed] [Google Scholar]
- 6. McCarthy M, Ridley TJ, Bollier M, Wolf B, Albright J, Amendola A. Femoral tunnel placement in medial patellofemoral ligament reconstruction. Iowa Orthop J. 2013;33:58–63. [PMC free article] [PubMed] [Google Scholar]
- 7. Nomura E, Horiuchi Y, Kihara M. Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction. Knee. 2000;7(2):121–127. [DOI] [PubMed] [Google Scholar]
- 8. Sanchis-Alfonso V. Guidelines for medial patellofemoral ligament reconstruction in chronic lateral patellar instability. J Am Acad Orthop Surg. 2014;22:175–182. [DOI] [PubMed] [Google Scholar]
- 9. Sanchis-Alfonso V, Montesinos-Berry E, Ramirez-Fuentes C, Leal-Blanquet J, Gelber PE, Monllau JC. Failed medial patellofemoral ligament reconstruction: causes and surgical strategies. World J Orthop. 2017;8(2):115–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sanchis-Alfonso V, Ramirez-Fuentes C, Montesinos-Berry E, Aparisi-Rodriguez F, Martí-Bonmatí L. Does radiographic location ensure precise location of the femoral fixation site in medial patellofemoral ligament surgery? Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2838–2844. [DOI] [PubMed] [Google Scholar]
- 11. Sanchis-Alfonso V, Ramirez-Fuentes C, Montesinos-Berry E, Domenech J, Martí-Bonmati L. Femoral insertion site of the graft used to replace the medial patellofemoral ligament influences the ligament dynamic changes during knee flexion and the clinical outcome. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2433–2441. [DOI] [PubMed] [Google Scholar]
- 12. Schöttle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801–804. [DOI] [PubMed] [Google Scholar]
- 13. Servien E, Fritsch B, Lustig S, et al. In vivo positioning analysis of medial patellofemoral ligament reconstruction. Am J Sports Med. 2011;39(1):134–139. [DOI] [PubMed] [Google Scholar]
- 14. Siebold R, Borbon CA. Arthroscopic extraarticular reconstruction of the medial patellofemoral ligament with gracilis tendon autograft: surgical technique. Knee Surg Sports Traumatol Arthrosc. 2012;20(7):1245–1251. [DOI] [PubMed] [Google Scholar]
- 15. Smirk C, Morris H. The anatomy and reconstruction of the medial patellofemoral ligament. Knee. 2003;10(3):221–227. [DOI] [PubMed] [Google Scholar]
- 16. Steensen RN, Dopirak RM, McDonald WG., 3rd The anatomy and isometry of the medial patellofemoral ligament: implications for reconstruction. Am J Sports Med. 2004;32(6):1509–1513. [DOI] [PubMed] [Google Scholar]
- 17. Viste A, Chatelet F, Desmarchelier R, Fessy MH. Anatomical study of the medial patello-femoral ligament: landmarks for its surgical reconstruction. Surg Radiol Anat. 2014;36(8):733–739. [DOI] [PubMed] [Google Scholar]
- 18. Wijdicks CA, Griffith CJ, LaPrade RF, et al. Radiographic identification of the primary medial knee structures. J Bone Joint Surg Am. 2009;91(3):521–529. [DOI] [PubMed] [Google Scholar]
- 19. Ziegler CG, Fulkerson JP, Edgar C. Radiographic reference points are inaccurate with and without a true lateral radiograph: the importance of anatomy in medial patellofemoral ligament reconstruction. Am J Sports Med. 2016;44(1):133–142. [DOI] [PubMed] [Google Scholar]