Abstract
Objective. To assess the incidence of self-reported depression among pharmacy residents in Tennessee.
Methods. A 50-question survey was distributed to pharmacy residency program directors across Tennessee. Using questions modified from the Major Depression Inventory scale, subjects were asked to identify personal signs or symptoms of depression. The researcher observed trends of depression and offered mental health education to participating programs.
Results. Eighty-four residents were potentially exposed to the survey with 50 participants, yielding a 59% response rate. Of the 50 residents, 19 self-reported feeling depressed during residency. More concerning, 11 residents reported having suicidal thoughts. Additionally, 13 residents voiced they would benefit from mental health resources.
Conclusion. Self-reported depression among pharmacy residents is not uncommon. Defining mental health benefit resources at the beginning of residency would be beneficial.
Keywords: pharmacy, depression, resident
INTRODUCTION
Depression affects approximately 7% of the United States population, or about 14.8 million Americans.1 Mood disorders, such as depression, have become the third most common cause of hospitalization in the United States.2 Alarmingly, suicide is the 10th leading cause of death in the U.S. and the third leading cause of death for people 15 to 24 years old.3 More than 90% of those who die by suicide had one or more mental disorders, such as depression.2
Depression among health care professionals is well-documented. Medical residents have a higher incidence of depression when compared to the national average for the same age group, with a 30% versus 7% incidence rate respectively.4 This can lead to poor performance at work and increased risk of medication errors, increasing by as much as five times more than non-depressed peers.5 Perry and colleagues found that nearly 13% of surveyed nurses in Australia report a history of anxiety and depression.6 Unfortunately, addressing the issue of depression in the health care community is not commonly discussed.
Often the topic of depression in medically trained professionals arises after a negative event, such as suicide. In 2014, two resident physicians, within the same program in New York City, committed suicide. These two incidents sparked national recognition through multiple scholarly articles addressing the seriousness of depression within the medical community.4,7 In 2011, a pharmacy resident in Charleston, West Virginia also ended her life.8 Despite this, there have been no published studies to-date evaluating the incidence of depression among pharmacy residents. The lack of literature in this area is surprising considering pharmacists consistently rank among the top 10 professions with the highest suicide rates.9
The purpose of this study is to evaluate the incidence of self-reported signs and symptoms of depression in pharmacy residents in Tennessee, and those located within a three-hour radius of Nashville. The secondary purpose of this study is to determine if residents are aware of the availability of mental health benefit resources within their program.
METHODS
A 50-question survey was sent to residents asking them to self-report signs and symptoms of depression. The survey questions were adapted from the Major Depression Inventory (MDI) scale along with questions on how the residency environment could affect one’s overall self-perceived mental health. Lipscomb University’s Institutional Review Board approved the survey. The survey questions were uploaded to Research Electronic Data Capture, REDCap (Version 4.14.1, Vanderbilt University, Nashville, TN). This software created an anonymous external link that was not unique to the recipient. A list of residents’ email addresses was unavailable, so the investigator emailed the survey to pharmacy residency directors of ASHP-accredited pharmacy residencies in Tennessee, and to those located within a 3-hour radius of Nashville. The survey instrument was not pilot tested outside of the investigation prior to its use. All Tennessee residency programs (n=40) were eligible to be included in the study, and all directors received an email to participate. The email to the residency directors included a “read receipt.” This function allowed the investigator to quantify how many residents were exposed to the survey. The “read receipts” were used to track the survey response rate. Only one “read receipt” was received from any one email address. The investigator added the number of residents associated with each received “read receipt” to calculate the survey response rate. Potential participants were given seven weeks to respond to the survey with one mid-point reminder.
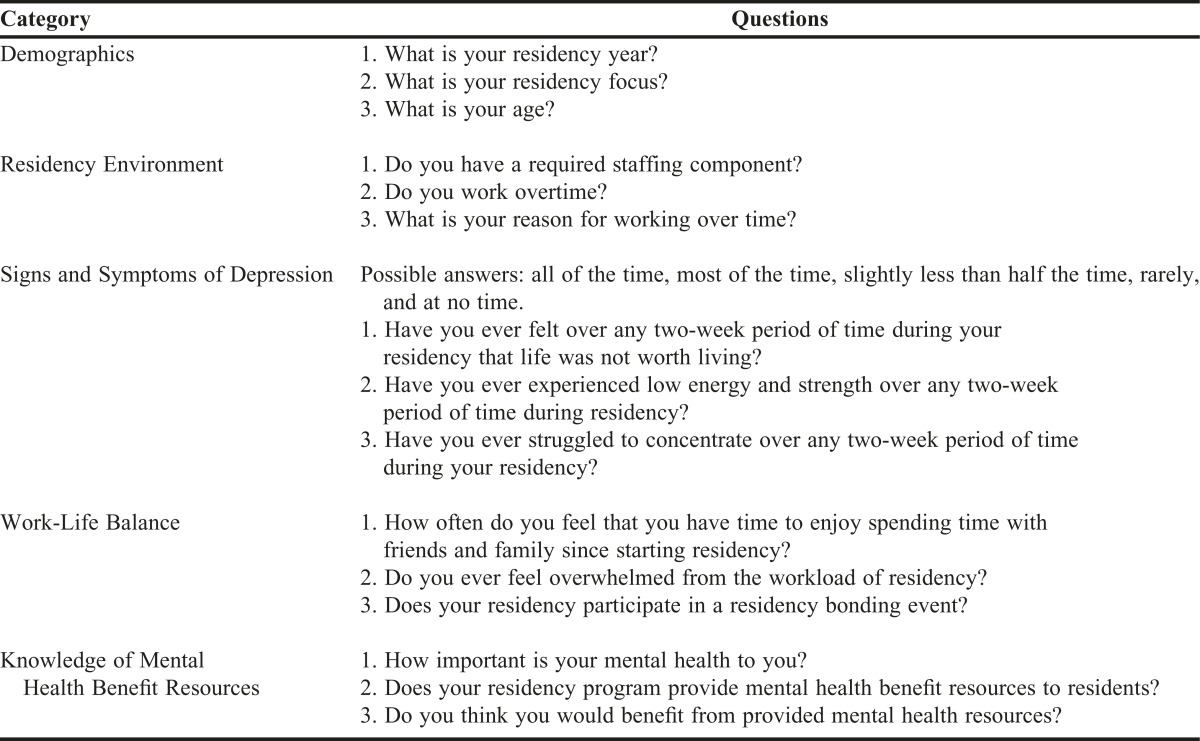
The survey questions covered the following areas: demographic data, self-reported signs and symptoms of depression, residency environment, work-life balance, and knowledge of mental health benefit resources. A partial list of questions from the survey can be found in Table 1. Questions regarding signs and symptoms of depression were modeled after the MDI scale and helped identify participants’ self-reporting depression symptoms. The MDI scale was chosen due to its internal and external validity of recognizing signs and symptoms of depression. The MDI scale correlates to the DSM-IV and ICD-10 algorithms and is comparable to the HAM-D scale.10 The MDI scale helps identify the severity of a patient’s signs and symptoms of depression using a concise number of questions and a simple sum to calculate the patient’s responses.11 This 10-question scale was utilized to help with survey fatigue and for its public domain access.
Table 1.
Partial List of Survey Questions Investigating Self-Reported Depression Among Pharmacy Residents
Questions about the residency environment included the presence of co-residents, staffing components, and overtime hours. Residents were also asked about work-life balance related to quality time with family and friends, adequate time for self or if they were overwhelmed from their residency workload. The final section of the survey asked the residents if they were aware of mental health benefit resources that their program offered. Residents were also asked if they would benefit from and utilize mental health resources if they were provided to them. Once the survey data was collected and analyzed, the investigator prepared and delivered a free online CE webinar. This webinar was offered to all residency programs within Tennessee and surrounding areas. The webinar addressed the results of the survey, treatment of depression, and available national resources.
Descriptive statistics are reported for all sample characteristics. The investigator used intent-to-treat when completing statistical analyses and reporting results. Intent-to-treat was used to allow participants to refrain from answering any given question. Nominal measures were reported as counts and percentages. Statistical software JMP Statistical Discovery from SAS (Version 12.2, SAS Institute, Cary, NC) was used to conduct a Student t-test to compare the survey response means.
RESULTS
Based on the “read receipt,” 84 residents potentially received the survey. A total of 50 residents responded to the survey resulting in a 59% response rate. A majority (n=40, 80%) of the residents were PGY-1 residents. There were 13 (74%) female and 37 (26%) male residents and most (n=43, 86%) were between 24-29 years of age.
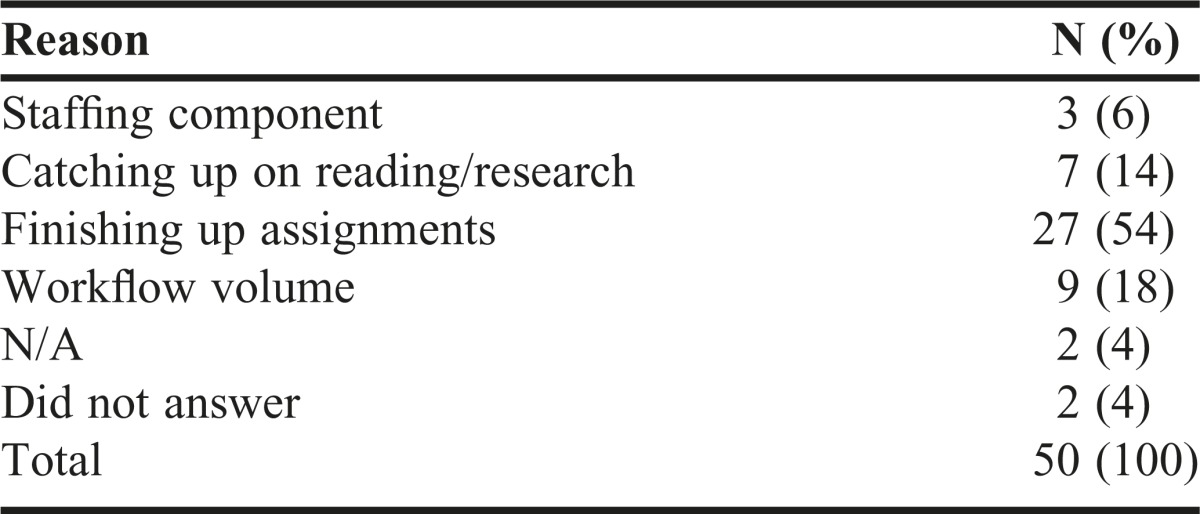
A majority of the residents (n=39, 78%) reported working 8-10 hours a day during their residency and six (12%) reported working 10-12 hours in a single shift. In regards to overtime, 34% (n=17) reported working 1-2 hours over their required shift for 5 or more days of the week. Table 2 provides a summary of the residents’ reasons for staying past their assigned work shift. A majority of the residents (n=41, 82%) also reported a required staffing component for their residency.
Table 2.
Resident Reason For Working Overtime
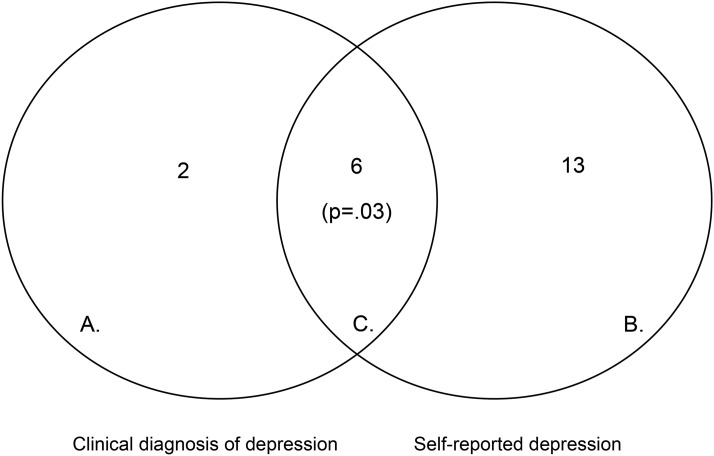
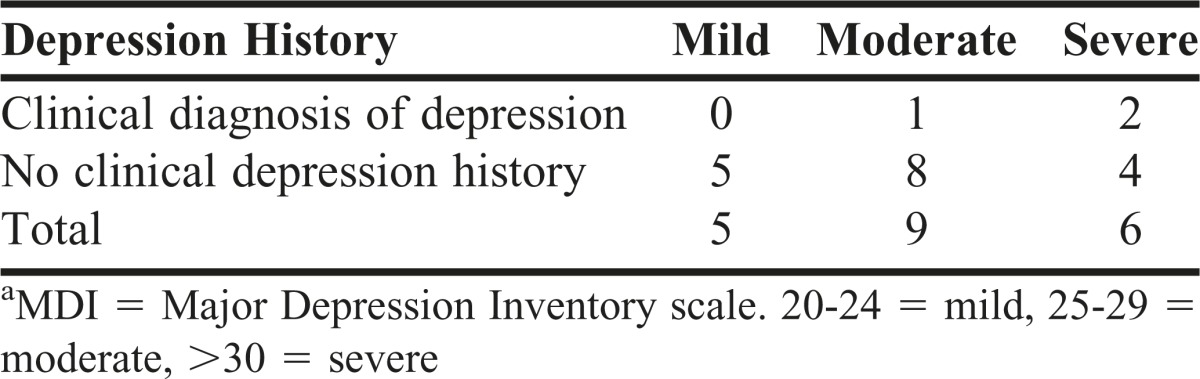
Forty-one (82%) of residents reported having experienced an episode of depressed mood at least once during residency. This was indicated by answering “yes” to the question, “During your residency, have you ever considered yourself depressed?” Simultaneously, 36 (72%) have experienced losing interest in pleasurable activities, while 43 (86%) reported a period of feeling less confident at least once during residency. Eleven (22%) residents reported that during their residency, they experienced an episode of suicidal ideation. Of these 11 residents, eight reported that the suicidal ideation occurred “rarely,” one reported that the suicidal ideation occurred “less than half of the time,” and two reported that the suicidal ideation occurred “more than half of the time” during a specific two-week period of time. Using questions modified from the MDI scale, the investigator added up the scores of each resident’s responses and discovered the following: five residents reported mild symptoms of depression, nine residents reported moderate symptoms of depression, and six residents reported severe symptoms of depression. Of those residents that fell into the severe category, only two reported a previous clinical diagnosis of depression (Figure 1, Table 3).
Figure 1.
Clinical Diagnosis of Depression (A) and Self-reported Depression (B) Among Pharmacy Residents with Overlap (C)
Table 3.
Resident MDIa Score Compared to Past History of Depression
Eighteen (36%) residents reported having poor work-life balance during residency. Twenty-one (42%) residents reported that they “rarely” have time to spend with family and friends since starting residency and 17 (34%) reported “rarely” having time to enjoy hobbies. Thirty-one (62%) residents reported feeling overwhelmed from the workload of residency.
Thirty-five (70%) residents believe that their mental well-being is “very important” and 13 (26%) believe that they would benefit from receiving mental health benefit resources. A majority (n=27, 54%) do not know if their program provides mental health benefit resources.
DISCUSSION
Although depression among medical residents is a well-documented problem,4,7 to the investigator’s knowledge, this is the first survey looking specifically at pharmacy residents and the self-reported incidence of depression during residency. While, the incidence of self-reported depression is relatively high (40%) among this sample, it is comparable to the 30% reported incidence among medical residents.4 In comparison, the self-reported incidence of depression coincides with the number of participants reporting mild, moderate and severe symptoms of depression, showing consistency. Out of the six residents who reported experiencing severe symptoms of depression, only two reported having a documented history of clinical depression. This should be concerning to program directors because residents are experiencing periods of depression that warrant professional psychiatric care. Absence of treatment may be due to the lack of education in recognizing depression, the stigma attached to mental illness, lack of resources, or fear of losing clinical privileges. Three residents who have a history of clinical depression reported symptoms of “moderate” or “severe” depression (Table 3). The authors recognize that lower self-reported depression scores may be attributed to the clinically depressed residents being adequately treated with medications, which was not accessed in this study.
The most concerning result from the study were the residents who expressed suicidal ideation, whether it be passive or active, at least once during their residency year. When a resident commits suicide, questions such as is this an outlier, or is this a common occurrence arise. The results of the study show that suicidal ideation is not rare, and there is a need for more literature regarding this topic in this particular population. These outcomes should shed a much needed light on the area of mental health in pharmacy residents and should encourage residency program directors to establish new policies and procedures for their residency practice sites.
A survey conducted in 2015 showed that 64.5% of pharmacists reported that their stress levels have increased over the previous year.12 This was mainly attributed to an increased workload.12 Workload stress and the residency environment could be a contributing factor to increased reports of depression in pharmacy residents. Possible causative factors could be the added components of staffing, being on-call, all combined with lack of sleep.6 Many residents reported that their sleep habits changed since they began their residency. Also, some residents reported feeling overwhelmed from the workload of residency and having to work overtime, defined as working over their typical work day hours specific to their site, extra days worked per week or working from home after the workday is completed, in order to complete project assignments. Reported “poor work-life balance” may also play a role in depression.
The response rate of the study was moderate. This could be due to the fact that distressed residents may have viewed the survey as an outlet to talk about their depression. The response rate could have been larger had the residents received the survey directly, instead of through their residency director. This method of distribution did not ensure that all residents had the opportunity to participate in the survey. Additionally, the link provided to the residents was not unique, which could result in one participant taking the survey multiple times.
There were additional limitations to this study. While the study would meet power when comparing the rate of depression among the study participants and the general population (β=.99), the study did not meet power when comparing this sample to the incidence of depression among medical residents (β=.23). One way to meet power in this study would be to expand it geographically to achieve a sample size of 278 participants. Additionally, the study relied on self-reported results, which could lend to reporting bias. To overcome this, formal clinical evaluations in addition to collateral information would help validate the design of the study. Location and convenience sample bias may inflate the incidence of self-reported depression as Tennessee has a slightly higher incidence of depression among people 18 years old and older, with 7.9% versus 6.8% nationally.13 However, the survey did not assess permanent residency of the participants of the survey. Expanding the survey to all ASHP-accredited residency programs would help eliminate these biases. Other methodological study flaws existed and would need to be corrected in any future studies. These include the use of a non-validated survey tool, no baseline survey results for comparative purposes, and the lack of assessment of pharmacologic and non-pharmacologic treatment.
The purpose of this study was to raise awareness of depression among pharmacy residents. The results of the study were used to provide, and show the importance of providing, mental health resources and education to residency programs (Table 4). Depression may adversely affect the concentration and confidence of pharmacy residents, lowering the quality of care they provide to patients.5 With 27% of health care professionals suffering from depression,14 residency program directors should be concerned and vigilant about the mental wellness of their residents. Apart from offering educational materials, training programs should include interventions that promote resident well-being. One approach may be to incorporate weekly meetings that allow residents to reflect upon areas of discontent, which already has promising data in helping to improve resident well-being.15,16 Another strategy is for medical residents to enroll in a volunteer tracking program for depression and anxiety in which residents who score in the “moderate and severe” categories would be contacted by a mental health provider. This program could be modified to fit into pharmacy residency programs.17
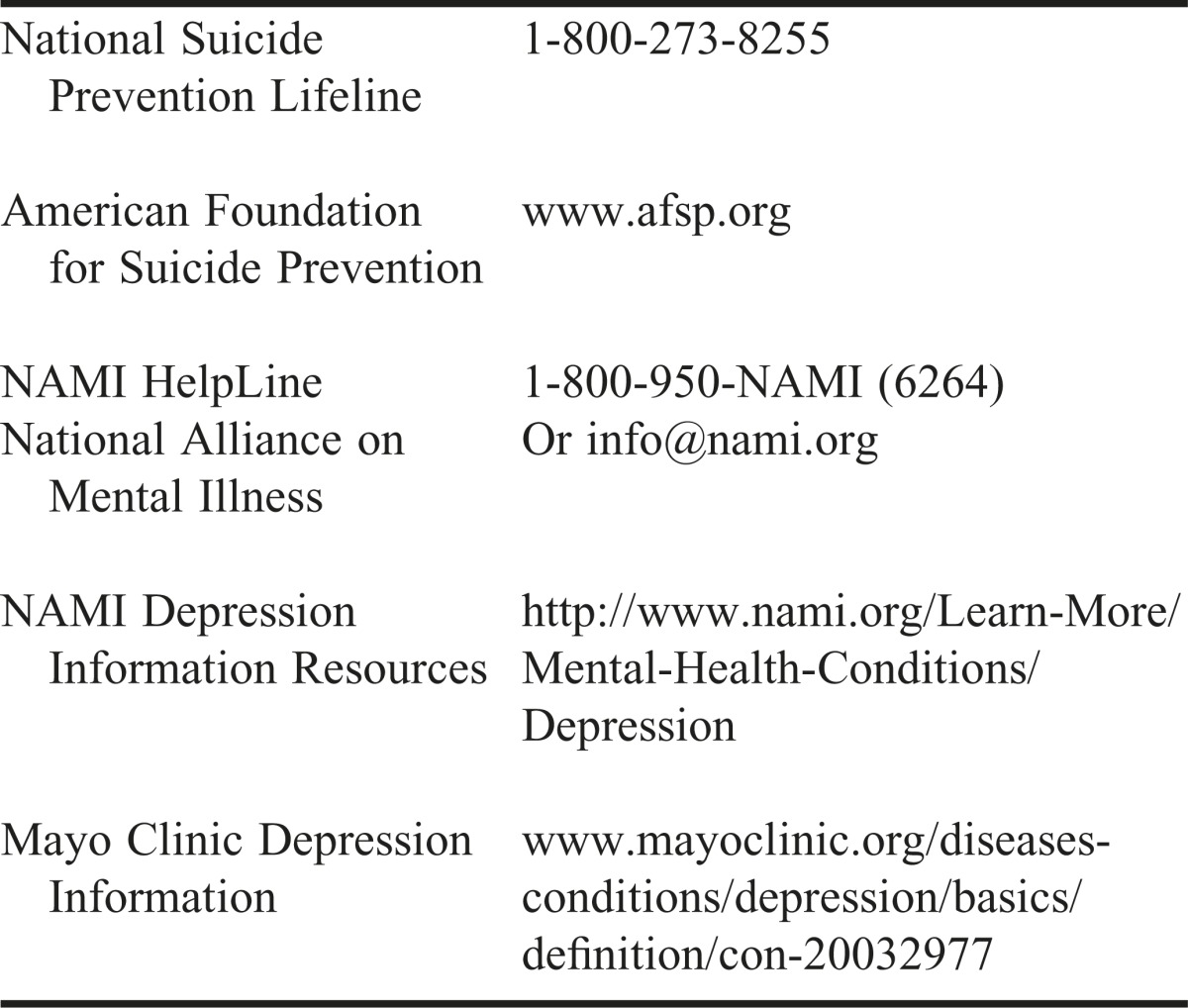
Table 4.
Mental Health Benefit Resources
CONCLUSION
In a society that now encourages employers to promote wellness incentives for their employees, mental wellness should be an intentional inclusion. Moutier and colleagues found that providing mental health benefit resources and services helped alleviate feelings of being overwhelmed or depressed.18 However, there are no data that illustrates how many programs offer these resources or if they are being utilized. Exploring the concept of providing mental health benefit resources may lead to the improvement of pharmacy resident mental wellness, as demonstrated in medical residencies, and warrants future research.18 The mental well-being of pharmacy residents needs to be a priority among residency directors. Pharmacy residents need to be educated now on how to take care of their mental health. The authors hope the results of this study will help start that discussion.
Footnotes
Chi-squared test was used to compare residents who self-reported symptoms of depression (n=8) and residents with a clinical diagnosis of depression (n=19). There were six residents who self-reported depression and reported having a clinical diagnosis of depression (p=.03).
REFERENCES
- 1.Center for Behavioral Health Statistics and Quality. Behavioral health trends in the United States: results from the 2014 National Survey on Drug Use and Health. https://www.samhsa.gov/data/sites/default/files/NSDUH-FRR1-2014/NSDUH-FRR1-2014.pdf. Accessed October 23, 2017.
- 2.Agency for Healthcare Research and Quality. Wier LM. HCUP facts and figures: statistics on hospital-based care in the United States, 2009. https://www.hcup-us.ahrq.gov/reports/factsandfigures/2009/pdfs/FF_report_2009.pdf. Accessed March 31, 2016. [DOI] [PubMed]
- 3.National Center for Injury Prevention and Control. Center for Disease and Control (CDC). Web-based Injury Statistics Query and Reporting System (WISQARS). http://www.cdc.gov/injury/wisqars/index.html. Accessed November 1, 2016.
- 4.Dyrbye LN, West CP, Satele D, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89:443–451. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 5.Jennings ML, Slavin SJ. Resident wellness matters: optimizing resident education and wellness through the learning environment. Acad Med. 2015;90(9):1246–1250. doi: 10.1097/ACM.0000000000000842. [DOI] [PubMed] [Google Scholar]
- 6.Perry L, Lamont S, Brunero S, Gallagher R, Duffield C. The mental health of nurses in acute teaching hospital settings: a cross-sectional survey. BMC Nursing. 2015;14:15. doi: 10.1186/s12912-015-0068-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rubin R. Recent suicides highlight need to address depression in medical students and residents. JAMA. 2014;312(17):1725–1727. doi: 10.1001/jama.2014.13505. [DOI] [PubMed] [Google Scholar]
- 8.Bowers P. Bridge jumper identified. Charleston City Paper. December 19, 2011. http://www.charlestoncitypaper.com/charleston/bridge-jumper-identified-as-tosin-oyelowo/Content?oid=3662179. Accessed October 31, 2016.
- 9.Roberts SE, Jaremin B, Lloyd K. High risk occupations for suicide. Psychol Med. 2013;43(6):1231–1240. doi: 10.1017/S0033291712002024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bech P, Rasmussen NA, Olsen LR, Noerholm V, Abildgaard W. The sensitivity and specificity of the Major Depression Inventory, using the Present State Examination as the index of diagnostic validity. J Affect Disord. 2001;66(2-3):159–164. doi: 10.1016/s0165-0327(00)00309-8. [DOI] [PubMed] [Google Scholar]
- 11.Olsen LR, Jensen DV, Noerholm V, et al. The internal and external validity of the Major Depression Inventory in measuring severity of depressive states. Psychol Med. 2003;33(2):351–356. doi: 10.1017/s0033291702006724. [DOI] [PubMed] [Google Scholar]
- 12.Drug Topics’ 2015 salary survey. pharmacist income hold steady. http://drugtopics.modernmedicine.com/drug-topics/news/drug-topics-2015-salary-survey-pharmacist-incomes-hold-steady?page=0,0. Accessed November 1, 2016.
- 13.Tennessee Department of Mental Health & Substance Abuse Services. Behavioral Health Indicators for Tennessee and the United States. https://www.tn.gov/behavioral-health/article/behavioral-health-indicators-for-tennessee-and-the-united-states. Accessed October 23, 2017.
- 14.Wall TD, Bolden RI, Borrill CS, et al. Minor psychiatric disorder in NHS trust staff: occupational and gender differences. Br J Psychiatry. 1997;171(6):519–523. doi: 10.1192/bjp.171.6.519. [DOI] [PubMed] [Google Scholar]
- 15.Ladouceur R. Distress among residents. Can Fam Physician. 2015;61(2):105–106. [PMC free article] [PubMed] [Google Scholar]
- 16.West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174(4):527–533. doi: 10.1001/jamainternmed.2013.14387. [DOI] [PubMed] [Google Scholar]
- 17.Slavin SJ, Chibnall JT. Finding the why, changing the how: improving the mental health of medical students, residents, and physicians. Acad Med. 2016;91(9):1194–1196. doi: 10.1097/ACM.0000000000001226. [DOI] [PubMed] [Google Scholar]
- 18.Moutier C, Norcross W, Jong P, et al. The suicide prevention and depression awareness program at the University of California, San Diego School of Medicine. Acad Med. 2012;87(3):320–326. doi: 10.1097/ACM.0b013e31824451ad. [DOI] [PubMed] [Google Scholar]