Abstract
Background:
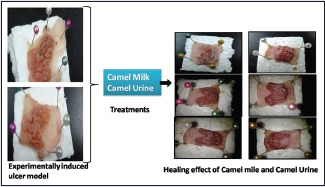
Camel milk has been reportedly used to treat dropsy, jaundice, tuberculosis, and diabetes while camel urine is used to treat diarrhea and cancer. However, there is no scientific evidence on the antiulcer activity of camel milk and urine. Thus, the present is designed to investigate the gastroprotective and ulcer healing effect of camel milk and urine on experimentally induced gastric ulcer models in rats.
Materials and Methods:
The gastroprotective effect was investigated in HCl/EtOH, water-restraint stress (WRS) and non-steroidal anti-inflammatory drugs (indomethacin)-induced ulcer models while ulcer healing activity was investigated in indomethacin-induced ulcer model. Cimetidine (100 mg/kg) was used as a standard antiulcer drug.
Results:
Acute toxicity study done up to a dosage of 10 ml/kg of camel milk and urine showed no signs of toxicity and mortality among the rats, indicating the present dosage of 5 ml/kg is safe to be administered to the rats. In the HCl/EtOH model, oral administration of cimetidine (100 mg/kg), camel urine (5 ml/kg), and camel milk (5 ml/kg) significantly (P < 0.05) inhibited gastric lesions by 83.7, 60.5 and 100%, respectively. In the WRS-induced model, cimetidine, and camel urine showed an ulcer inhibition of 100% while camel milk showed an inhibition of 50%. Similarly, in the indomethacin-induced ulcer model, cimetidine, camel milk, and urine showed an ulcer inhibition of 100, 33.3, and 66.7%, respectively. In addition, camel milk and urine also showed a significant (P < 0.05) ulcer healing effect of 100% in indomethacin-induced ulcer model, with no ulcers observed as compared to that of cimetidine, which offers a healing effect of 60.5%.
Conclusion:
The antiulcer activity of camel milk and urine may be attributed to its cytoprotective mechanism and antioxidant properties.
SUMMARY
Acute toxicity findings revealed the dosage of 10 ml/kg of camel milk and urine seems no toxic and indicating the dosage of 5 ml/kg is safe to be administered to the rats
Oral administration of cimetidine (100 mg/kg), camel urine (5 ml/kg), and camel milk (5 ml/kg) significantly inhibited gastric lesions by 83.7, 60.5 and 100% in the HCl/EtOH experimental model
The results of this investigation have proven that camel milk and urine showed strong ulcer healing effect in indomethacin-induced gastric damage.
Abbreviations used: NSAIDs: Non-steroidal anti-inflammatory drugs, UI: Ulcer index, ANOVA: One-way analysis of variance, WRS: Water-restraint stress, ROS: Reactive oxygen species
Keywords: Antioxidant, cimetidine, camel milk, HCl/EtOH model, indomethacin, urine
INTRODUCTION
Peptic ulcer disease is one of the most common and widespread diseases in the world and affects a considerable number of people globally every year. The epidemiology of peptic ulcer disease largely reflects the epidemiology of the 2 major etiologic factors, Helicobacter pylori infection and use of non-steroidal anti-inflammatory drugs (NSAIDs). Peptic ulcer is a breach in the gastric or duodenal mucosa down to the submucosa as a result of corrosion caused by digestive juices secreted by stomach cells. Small or shallow breaches are termed “erosions” while sometimes insignificant, these may herald ulcers.[1] In the Developed nations, H. pylori incidence has been slowly declining over the past 50 years, and NSAID use has increased. This has resulted in a decline in duodenal ulcers (almost always associated with H. pylori infection) and an increase in gastric ulcers (the main site of ulcers caused by NSAIDs). Peptic ulcers remain common worldwide, especially in the developing world where H. pylori infection is highly prevalent. Despite the progress in conventional chemistry and pharmacology in producing highly effective antiulcer drugs, most of them produce adverse reactions and side effects. For example, H2-receptor antagonists (e.g., cimetidine) may cause gynecomastia in men and galactorrhea in women[2] while proton-pump inhibitors (e.g., omeprazole and lansoprazole) can cause nausea, abdominal pain, constipation, and diarrhea.[3] Therefore, several efforts have been made to find a novel antiulcer drug with potentially less or no side effects.
Camel milk and urine have traditionally been used to treat many diseases over the years. Camel milk is known to have medicinal properties and healing effects such as to treat dropsy, jaundice, problems of the spleen, tuberculosis, asthma, anemia, piles, and diabetes.[4] In addition, camel milk possesses both antiviral and antibacterial properties, which makes it effective in killing microbial agents and protecting the body from various diseases, even to the extent of treating some types of cancer.[5] Camel urine has been found to have anticancer properties which are attributed to the presence of nanoparticles in urine that can attack cancer cells with success while maintaining healthy cells in a cancer patient.[6] Besides, camel urine also possesses antibacterial and antifungal activity.[7,8] Any potent antiulcer drug should possess both gastroprotective as well as ulcer healing property.[9]
Camel milk contains high levels of Vitamins C, A, B2, and E (acidic pH) and is rich in magnesium and zinc.[8] These vitamins are useful in reducing the oxidative stress caused by toxic agent, and magnesium is very essential for absorption and metabolism of Vitamins, B, C, and E.[9] In addition, magnesium is essential for the biosynthesis of glutathione; prevents damage to cellular components caused by free radicals, peroxides, and heavy metals. More recently, magnesium significantly enhances the antioxidant defense. A protective effect of zinc has been reported against the cellular toxicity due to the palliative effect on oxidative stress and apoptosis, activation of the antioxidant system to decreased lipid peroxides.[10] Moreover, camel milk can generate nitric oxide it stimulates mucus production, inhibits the adherence of neutrophils to the endothelial cells and, especially, increases the blood flow to the gastric mucous membrane.[11]
The current study was undertaken to evaluate the gastroprotective activity of camel milk and urine in HCl/EtOH, indomethacin (NSAIDs), and water-restraint stress (WRS)-induced ulcer in rats. In addition, the healing effect of camel milk and urine in the indomethacin-induced ulcer model was also investigated.
MATERIALS AND METHODS
Biological materials
Camel milk and urine were obtained from Hargeisa, Somaliland. The samples for urine and camel were obtained by following aseptic techniques and transferred into sterile tubes. The samples were transported from Hargeisa, Somaliland to Kuala Lumpur, Malaysia, in an ice-cold special container, and as soon as they arrived UCSI University, it was stored at −80°C.
Stability test
The pH of camel milk and urine was determined with a pH meter before administering to the animals. The pH meter was calibrated with three different buffer solutions at pH 7 (neutral), pH 4 (acidic), and pH 10 (alkaline). The pH probe was rinsed with water before the start of calibration. The pH probe was placed into the pH 7 solution, and pH reading was allowed to settle. The pH 7 screw on the top side of the meter was adjusted until the meter read 7. The probe was then rinsed with water, and the same steps were repeated for pH 4 and then 10. The pH 4/10 screw on the bottom side of the meter was adjusted until the meter read 4 or 10. Care should be taken to immerse the whole probe into the solution or else reading will not be accurate. Once the meter is calibrated, the pH of camel milk and urine was determined.
Animals
Approximately 95 Sprague-Dawley rats of either sex aged 7–8 weeks and weighing 180–220 g were purchased from the animal house of Universiti Kebangsaan Malaysia, Bangi, Selangor, and kept in UCSI animal holding area. The research was approved by UCSI Ethical Committee ethical code Proj-FAS-EC-13-030. The rats were placed in a 1 L plastic beaker and weighed with an electronic balance on the first day and before the start of the experiment. The rats were maintained in clean polypropylene cages containing wood shavings and fed with standard rat pellet and water ad-libitum. The rats were kept under standard laboratory conditions which include temperature between 25°C ± 2°C and humidity of 60–70%, under 12 h light/12 h dark cycle. Care was taken to prevent coprophagia among rats. The rats were allowed for 2 weeks to acclimatize before commencing the experiment. All rats fasted before each experiment as most drugs were administered orally.
Acute toxicity test
A safe oral dose of camel milk and urine was determined by the acute oral toxic test in rats as described by Boonchum et al.[12] with slight modifications. The test was based on observational changes among the animals. A total of 15 animals were used for this test. The control and treated group consisted of five animals each. The control group was treated with saline while the treated groups were given camel milk and urine, respectively. The animals fasted overnight before receiving dosage. Camel milk and urine were administered orally to each animal at a dosage of 10 ml/kg. The food was withheld for a further 3–4 h after administration of milk and urine. The animals were observed for any abnormal behavior such as diarrhea, salivation, respiratory distress, hyperexcitability, and incidence of mortality for the first 30 min, followed by 2, 4, 24, and 48 h and thereafter daily for a period of 2 weeks after the administration of drugs[13] compared with the control group.
Study design
Three models were adopted in the analysis of the gastroprotective effects, which are HCl/EtOH-, NSAIDs (indomethacin)-, and WRS-induced ulcer in rat models. In the healing (treatment) method, one model was adopted which was NSAIDs (indomethacin)-induced ulcer model. The rats were randomly divided into four groups which consisted of five rats in a group in an assay. The rats treated with the respective test solutions according to their respective groups.
A normal control group where rats were given only saline but not induced with any drugs was used as a reference point for other negative control groups. There was only one normal control group for the whole experiment. In Group 1 and 2, the rats were given saline (5 ml/kg) and cimetidine (100 mg/kg), respectively and induced with an ulcer agent while in Group 3 and 4, rats were given milk and urine (5 ml/kg), respectively and induced with an ulcer agent.
All drugs were prepared freshly just before administration and were administered orally except for indomethacin which was administered intraperitoneally in the gastroprotective method. All animals were fed by oral gavages with the help of a feeding tube (16G) in oral administration while an injection needle (25G) was used in the intraperitoneal injection administration.
Gastroprotective activity
HCl/Ethanol-induced ulcer
The gastric ulcers were induced in rats by administering HCl/EtOH solution. The rats were deprived of food, but not water, 24 h before the experiment. Saline (5 ml/kg), cimetidine (100 mg/kg), camel milk, and urine (5 ml/kg) were orally administered to the rats at the start of the experiment according to their respective groups in the study design. One hour later, each rat was orally treated with 0.2 ml of HCl-EtOH mixture (0.3M HCl and 60% EtOH) to induce gastric ulcer.[14] The rats were then killed 1 h after the administration of HCl/EtOH with an overdose of chloroform, and the stomachs were surgically removed and opened along the lesser curvature.[15] The stomachs were gently rinsed with saline. The mean ulcer score was expressed as ulcer index (UI), and this was determined by calculating the average of the total lesion length (mm) in each rat stomach according to Equation 1.[16,17] The degree of ulcer inhibition was calculated using Equation 2.[18,19]
Water restraint stress-induced ulcer
Ulcers were induced by subjecting the rats to WRS. The rats fasted 24 h prior to the experiment. They were deprived of food but not water. At the start of the experiment, animals received an oral treatment of saline (5 ml/kg), cimetidine (100 mg/kg), camel milk and urine (5 ml/kg) according to their groups. After 30 min, rats were immobilized in a restrainer which is supported with a retort stand and clamp, and immersed vertically in water to xiphoid level at the temperature of 25°C ± 2°C, in the presence of intense light according to the method of Malairajan et al. [Figure 1].[20] After 3 h, the rats were removed and killed by an overdose of chloroform, and the stomachs were surgically removed and opened along the lesser curvature. The stomachs were gently rinsed with saline. The gastric injury was scored on a 0–4 point scale based on the severity of formation of hemorrhages, according to the method used by Akuodor et al.[21] with slight modifications.
Figure 1.
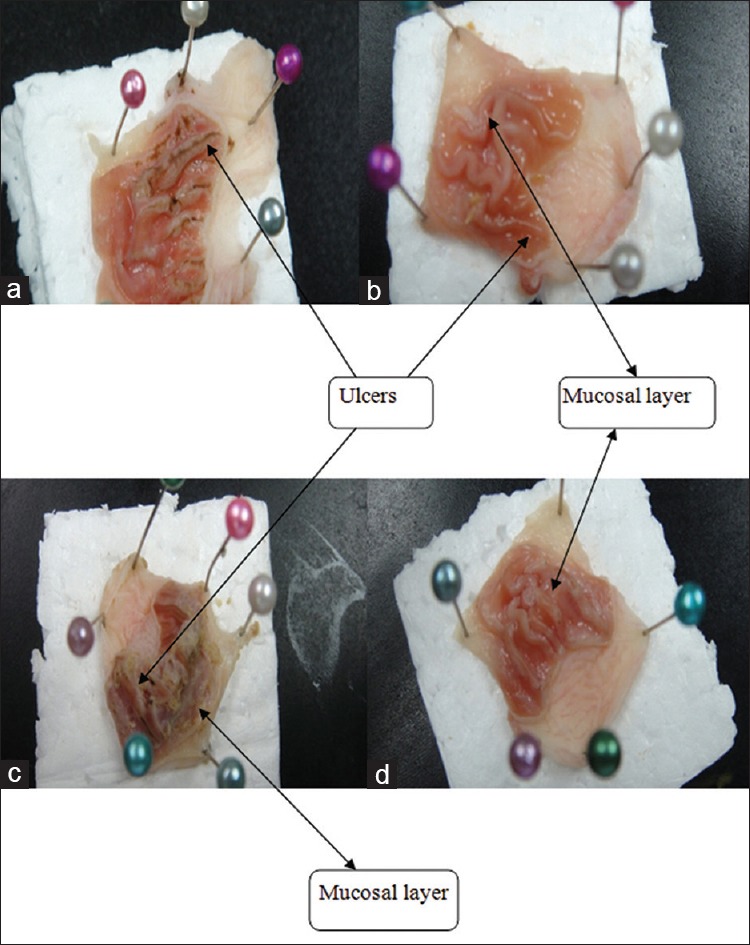
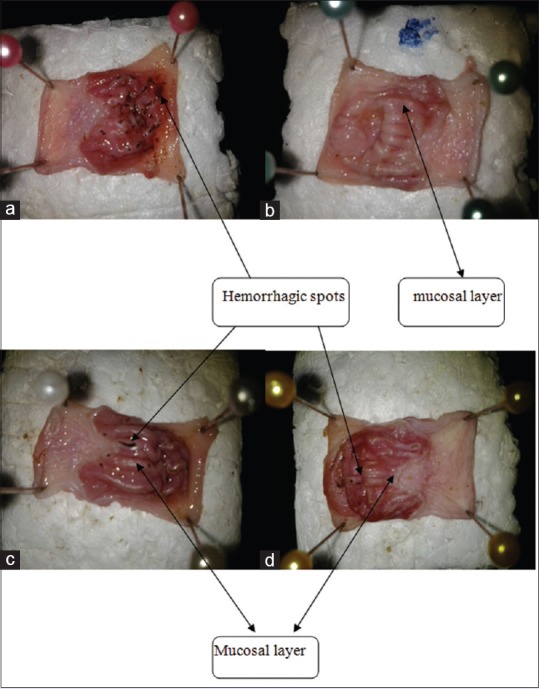
Gastroprotective effect of the respective test drugs on the gastric tissue of HCl/EtOH-induced ulcer: (a) Saline (negative control), (b) cimetidine (positive control), (c) camel milk, (d) camel urine. Arrows indicate the appearance of ulcers. Double arrows indicate the presence of mucosal layer
0 – Almost normal (no spots)
1 – Mild (1–5 spots)
2 – Moderate (6–10 spots)
3 – Severe (more than 10 spots)
4 – Very severe (spots all over the mucosa surface).
UI was expressed as the average of the total ulcer score in each rat according to Equation 3. Megala and Geetha[19] while the percentage of ulcer inhibition was determined according to Equation 2.
Non-steroidal anti-inflammatory drugs (indomethacin)-induced ulcer
The gastric ulcers were induced in rats by indomethacin suspension in 0.5% carboxymethyl cellulose, which was intraperitoneally injected at a dose of 50 mg/kg.[12] The rats were fasted 24 h before to the experiment while water was provided to them. At the start of the experiment, saline (5 ml/kg), cimetidine (100 mg/kg), camel milk, and urine (5 ml/kg) were orally administered to the rats in the respective groups. After 30 min, each rat was injected with 1 ml of indomethacin (50 mg/kg). Four hours later, the rats were killed with an overdose of chloroform. The stomachs were surgically removed and opened along the lesser curvature and gently rinsed with saline. The severity of the gastric injury was graded based on the number of hemorrhagic spots formed according to a 0–4 point scale based on the modified method of Akuodor et al.[21] as follows:
0 – Almost normal (no spots)
1 – Mild (1–5 spots)
2 – Moderate (6–10 spots)
3 – Severe (more than 10 spots)
4 – Very severe (spots all over the mucosa surface).
UI was expressed as the average of the total ulcer score in each rat according to Equation 3 while the percentage of ulcer inhibition was determined according to Equation 2.
Healing activity
Non-steroidal anti-inflammatory drugs (indomethacin)-induced ulcer
Gastric ulcers were induced in rats by orally administering 1 ml of indomethacin (5 mg/kg) once for 5 days after which treatment was started the next day after induction for another 5 days.[22] The rats were treated with saline (5 ml/kg), cimetidine (100 mg/kg), camel milk, and urine (5 ml/kg) once daily according to their respective groups. The animals were sacrificed on the fifth day after the last day of test solutions administration by an overdose of chloroform. The stomachs were removed and opened along the lesser curvature. The stomachs were gently rinsed with saline. The total length of ulcers was measured, and the mean ulcer score was expressed as UI, and this was determined by calculating the average of the total lesion length (mm) in each rat stomach (Equation 1) while the ulcer inhibition percentage was determined according to Equation 2.[23]
Statistical analysis
Data were expressed as mean ± standard deviation of the mean. Data were analyzed by one-way analysis of variance (ANOVA) followed by Dunnett's test using Graph Pad Prism 6 software version. The significance of difference was accepted at P < 0.05.
RESULTS
Acute toxicity study
The administration of camel milk and urine at a high dosage of 10 ml/kg demonstrated that it did not show any sign of toxicity and mortality in the animals during 2 weeks of observation. There was no abnormal behavior observed among the animals in terms of diarrhea, salivation, respiratory distress, hyperexcitability, and mortality for the first 30 min, and subsequent hours after that for 2 weeks compared to the control group. Therefore, it is concluded that the camel milk and urine at a lower dosage of 5 ml/kg is safe to be administered to the animals.
pH and physical observations of camel milk and urine
Camel milk and urine were successfully obtained from Somalia and used for this experiment. The pH of camel milk and urine was determined daily with a pH meter to ensure that it remained in the ideal range before administering to the animals. Determination of the pH of camel milk throughout the experiment showed that it was in the range of 6.0–6.4, which was slightly acidic. This observation is in line with Khaskheli et al.,[24] which reported that the ideal range of pH of camel milk is between 6.0 and 6.7. Similarly, the pH of camel urine was determined to be between 8.5 and 8.9, which was slightly alkaline. The previous studies have reported that the pH values of urine can vary to be either acidic or alkaline.[25]
Camel milk appeared to be opaque and white with no abnormal smell at the start of the experiment. The milk normally has a sweet and sharp taste, but sometimes can have a salty taste due to the type of plants eaten by the camels.[4] The changes in taste are mainly caused by the type of fodder and availability of drinking water.[26] Camel milk is frothy when shaken slightly. Camel urine appeared to have a dark and smoky yellow color, with a strong odor. This smell is probably similar to that of sweet hay.[27,28] Both camel milk and urine were stored at a temperature of −80°C until further use. In the present study, storage at this temperature was able to maintain the durability of camel milk and urine in terms of the maintenance of its pH values.
HCl/ethanol-induced ulcer
In this present study, oral administration of HCl/ethanol mixture at a volume of 0.2 ml/animal and concentration of 60% EtOH, and 0.3M HCl was sufficient to induce ulcers in the animals, as can be observed from the characteristic lesions and inflammation (reddening) in the glandular portion of the rat stomach in the negative control group [Figure 1]. However, the administration of cimetidine (100 mg/kg), camel urine (5 ml/kg), and camel milk (5 ml/kg) showed a significant (P < 0.05) ulcer inhibition of 83.7, 60.5, and 100%, respectively. The mean UI was reduced significantly (P < 0.05) from 17.2 ± 0.84 mm in the negative control group to 2.8 ± 0.84, 6.8 ± 0.84, and 0 ± 0.00 mm in the cimetidine, camel milk, and urine models, respectively [Table 1].
Table 1.
Gastroprotective effect of the respective test drugs against HCl/EtOH-induced gastric lesion in rats
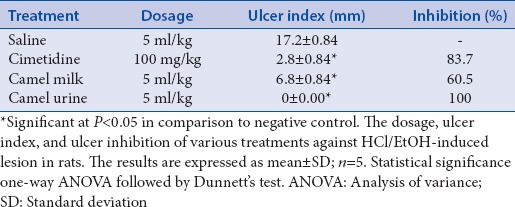
The clear presence of ulcer was observed on the gastric mucosa of rats in the milk model, besides the negative control. However, the portion of ulcers observed was fewer than that of the negative control model. In the cimetidine model, a slight portion of ulcer was observed. However, there were no ulcers observed in the urine model. The results suggest that camel milk and urine showed a significant anti-ulcer effect in this model. However, camel urine at a dosage of 5 ml/kg showed a better effect than camel milk. In addition, the presence of gastric mucosal layer observed in the cimetidine, milk, and urine model shows the protective effect offered by these compounds [Figure 1].
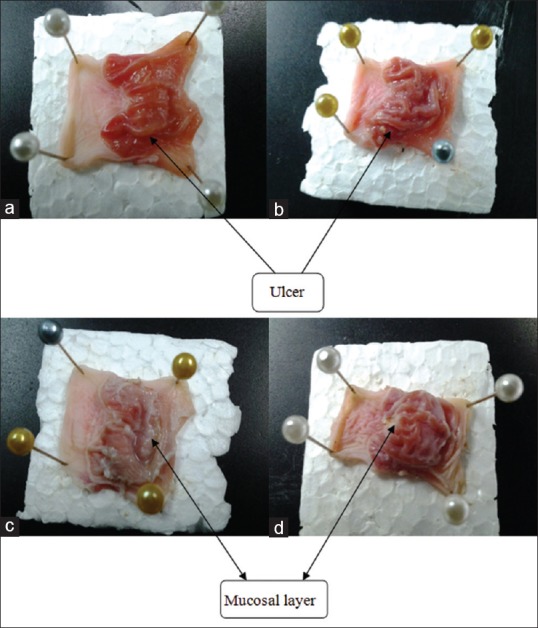
Water-restraint stress-induced ulcer
Ulcers were successfully induced by subjecting the animals to WRS for 3 h. It is previously reported that 3 h was sufficient to induce ulcer in rats in this model.[20] WRS-induced serious gastric erosions, as indicated by the formation of hemorrhagic streaks across the whole gastric mucosa in the negative control model [Figure 2]. However, the administration of cimetidine (100 mg/kg) and camel urine (5 ml/kg) showed an ulcer inhibition of 100%. Similarly, camel milk (5 ml/kg) inhibited ulcer formation by 50% [Table 2]. There were hemorrhagic spots in the camel milk model although not as much as the negative control while hemorrhagic streaks could be observed in the negative control, hemorrhagic spots were observed in the milk model indicating the lesser extent of severity. The severity of the gastric ulcer in the milk model was classified as moderate (2.0 ± 0.0) as compared to that of the negative control which was very severe (4.0 ± 0.0). In the cimetidine and urine model, no hemorrhagic spots or lesions were observed. Both the gastric tissue looks almost like a normal mucosa. However, the extent of inflammation (reddening) was greater in the cimetidine model compared to the camel urine model. The mucosal layer observed in the urine model indicates the strong protective effect offered by camel urine, and this probably contributed to the lesser extent of inflammation.
Figure 2.
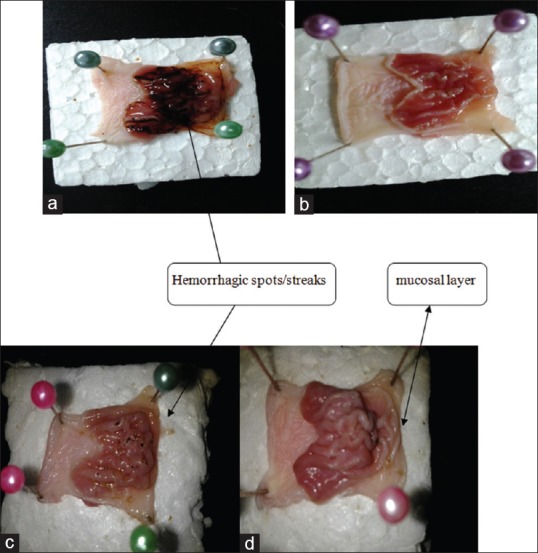
Gastroprotective effect of the respective test drugs on the gastric tissue of water-restraint stress-induced ulcer: (a) Saline (negative control), (b) cimetidine (positive control), (c) camel milk, (d) camel urine. Arrows indicate the presence of hemorrhagic spots or streaks. Double arrows indicate the mucosal layer
Table 2.
Gastroprotective effect of the respective test drugs against water-restraint stress-induced gastric lesion in rats
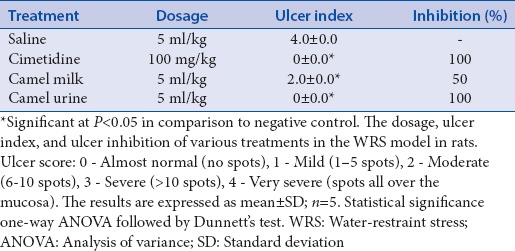
Non-steroidal anti-inflammatory drugs (indomethacin)-induced ulcer
Ulcers were successfully induced in the experimental rats using indomethacin at a dosage of 50 mg/kg. This can be shown by the extensive gastric mucosal damage lesion which appeared as blackish red hemorrhagic spots in the negative control model. It is reported that indomethacin produced a significant number of gastric lesions 4 h after dosing in experimental rats.[28] Similarly, Oluwabunmi et al.[29] reported the production of hemorrhages in indomethacin-induced ulcer in rats after 4 h. In the present study, administration of cimetidine (100 mg/kg), camel milk (5 ml/kg), and urine (5 ml/kg) reduced the severity of the gastric mucosa in terms of the formation of hemorrhagic spots by 100, 33.3, and 66.7%, respectively [Table 3]. The positive control model (cimetidine) showed an almost normal gastric mucosa with no hemorrhagic spots observed. The milk model showed few hemorrhagic spots (moderate), with an UI of 2.0 ± 0.0, while the urine model showed fewer hemorrhagic spots (mild), with an UI of 1.0 ± 0.0. The clear appearance of whitish mucosal layer was observed in the cimetidine, camel milk and urine models [Figure 3]. The protective effect of the mucosal layer probably contributed to the lesser extent of hemorrhagic severity.
Table 3.
Gastroprotective effect of the respective test drugs against nonsteroidal antiinflammatory drugs (indomethacin)-induced gastric lesion in rats
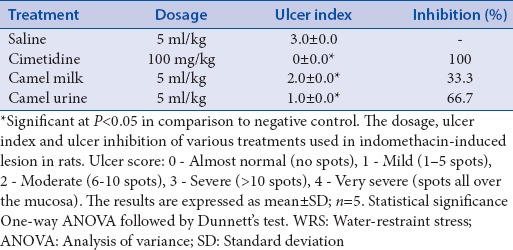
Figure 3.
Gastroprotective effect of the respective test drugs on the gastric tissue of non-steroidal anti-inflammatory drugs (indomethacin)-induced ulcer: (a) saline (negative control), (b) cimetidine (positive control), (c) camel milk, (d) camel urine. Arrows indicate the formation of hemorrhagic spots. Double arrows indicate the formation of mucosal layer
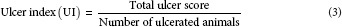
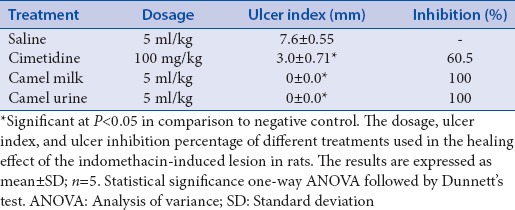
Non-steroidal anti-inflammatory drugs (indomethacin)-induced ulcer healing
Indomethacin (5 mg/kg) was successful in inducing ulcer in the animals as can be observed from the negative control model (saline) which showed extensive lesion area (7.6 ± 0.55 mm), with signs of inflammation (reddening). As can be observed from the results, no ulcers could be seen in the camel milk and urine model, both exerting a 100% healing effect. To further illustrate, thick, whitish gastric mucosal layer can be seen lining the stomach tissue in both camel milk and urine models as compared to the negative control model [Figure 4]. The positive control (cimetidine) model showed a bit of lesion area (3.0 ± 0.71 mm) with a significant healing effect of 60.5% [Table 4].
Figure 4.
Healing effect of the respective test drugs on the gastric tissue of non-steroidal anti-inflammatory drugs (indomethacin)-induced ulcer: (a) Saline (negative control), (b) cimetidine (positive control), (c) camel milk, (d) camel urine. Arrows indicate the ulcers on gastric mucosa. Double arrows indicate the mucosal layer
Table 4.
Healing effect of the respective test drugs against nonsteroidal anti-inflammatory drugs (indomethacin)-induced gastric lesion in rats
DISCUSSION
Peptic ulcer has become a global disease affecting people in all geographical regions. It is generally accepted that peptic ulcer results from an imbalance between aggressive factors and the maintenance of mucosal integrity through the endogenous defense mechanisms.[30] To regain the balance, different therapeutic agents including plant extracts may be used. Indomethacin is known to induce gastric ulcer by inhibition of prostaglandins which are cytoprotective to the gastric mucosa, particularly due to the inhibition of COX pathway of arachidonic acid metabolism resulting in excessive production of leukotrienes and other products of 5-lipoxygenase pathway.[31]
In the stomach, prostaglandins play a vital protective role, stimulating the secretion of bicarbonate and mucus, maintaining mucosal blood flow, and regulating mucosal cell turnover and repair.[32] Thus, the suppression of prostaglandins synthesis by NSAIDs results in increased susceptibility to mucosal injury and gastroduodenal ulceration. Several studies have indicated that gastroduodenal protection by prostaglandins is due to increase in the mucosal resistance as well as the decrease in aggressive factors such as acid and pepsin secretion.[33] It is a known fact that indomethacin and other members of the NSAIDs can slow down the healing process of peptic ulcer, this is further established by the results obtained in this experiment. These actions of indomethacin are due to its anti-inflammatory activity.[34]
The results of this study indicate that the camel milk and urine displays an antiulcerogenic effect related to its gastroprotective activity, it significantly reduced indomethacin-induced gastric ulcers, camel milk, and urine showed an antiulcer effect in all three models in the gastroprotective method. In the HCl/EtOH model, cimetidine, camel milk, and urine offered a significant (P < 0.05) protection of 83.7, 60.5, and 100%, respectively. In the WRS-induced model, cimetidine and camel urine showed an ulcer inhibition of 100% while camel milk showed an inhibition of 50%. Similarly, in the indomethacin-induced model, cimetidine, camel milk, and urine showed an ulcer inhibition of 100, 33.3 and 66.7%, respectively.
In short, camel urine showed a better preventive effect than camel milk in all three models in terms of formation of lesions or hemorrhages. In the healing model, results showed that both milk and urine possess a potent healing effect at a healing rate of 100%, with no ulcers observed. The standard drug cimetidine offered a healing effect of 60.5%. It can be considered that camel milk and urine are even more effective than the standard drug and can well be considered for the treatment of peptic ulcer in the future. The gastroprotective and healing effect of camel milk and urine could well be attributed to the presence of antioxidants. In vitro studies, such as determination of flavonoids, phenols, alkaloids, and vitamins can be done in the future to further ascertain the presence of antioxidants. Besides, in vivo studies can also be carried out for lipid peroxidation, superoxide dismutase, catalase, and glutathione peroxidase assay in stomach tissues. As these enzymatic antioxidants are produced endogenously and are used as markers of ulceration, it would be good to perform these assays to explore the effects of antioxidant defenses on the ulceration process.[34] Other models such as pyloric ligation-induced ulcer in rats can be done to investigate the antisecretory effect of camel milk and urine. As models such as HCl/EtOH, NSAIDs, and water stress-induced ulcer only investigate the cytoprotective mechanism of milk and urine, it would be ideal to also determine the antisecretory mechanism. Determination of the volume and pH of gastric juice can be carried out to determine the acid reducing capacity of camel milk and urine.
CONCLUSION
Administration of camel milk and urine appears to strengthen the mucosal barrier, which is the first line of defense against endogenous and exogenous ulcerogenic agents in HCl/EtOH, NSAIDs, and WRS-induced gastric damage. Camel milk and urine also showed strong ulcer healing effect in indomethacin-induced gastric damage. Camel milk and urine probably acted through its cytoprotective and reactive oxygen species scavenger capacity.
Thus, camel milk and urine merit further investigation as a gastric ulcer therapeutic and preventive agent in humans. In spite of the presented results, further studies are required to investigate the exact mechanism of the gastroprotective and healing effect of camel milk and urine and also the active compounds that are responsible for its antiulcer effect. One can explore the protection offered by camel milk and urine against gastric bacterial infection (H. pylori) as this is the main cause of peptic ulcer.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Majumdar D, Bebb J, Atherton J. Helicobacter pylori infection and peptic ulcers. Medicine. 2007;35:204–9. [Google Scholar]
- 2.Feldman M, Burton ME. Histamine2-receptor antagonists. Standard therapy for acid-peptic diseases 1. N Engl J Med. 1990;323:1672–80. doi: 10.1056/NEJM199012133232405. [DOI] [PubMed] [Google Scholar]
- 3.Franko TG, Richter JE. Proton-pump inhibitors for gastric acid-related disease. Cleve Clin J Med. 1998;65:27–34. doi: 10.3949/ccjm.65.1.27. [DOI] [PubMed] [Google Scholar]
- 4.Rao MB, Gupta RC, Dastur NN. Camels’ milk and milk products. Indian J Dairy Sci. 1970;23:71. [Google Scholar]
- 5.Gabry GH, Wadi FM. Nanoparticles in Camel's’ Urine. Vet Med J Giza. 2003;51:5. [Google Scholar]
- 6.Wadi FM. Nano-particles in Camels’ Urine May Help Treat Cancer. [Last accessed on 2012 May 29]. Available from: http://www.saudigazette.com.sa/index.cfm?method=home.regcon&contentID=2009071143333 .
- 7.Al-Jedabi A. Studies on the Antifungal Acitivity of Camel's Urine Against Some of the Pathogenic Fungi, for Revealing of the Scientific Miracles in the Prophetic Sunnah. Thesis. Saudi Arabia: The Education College of the Scientific Departments; 1999. [Google Scholar]
- 8.Al-Bashan MM. In vitro assessment of the antimicrobial activity and biochemical properties of camel's urine against some human pathogenic microbes. Middle-East J Sci Res. 2011;7:947–958. [Google Scholar]
- 9.Traber MG, Stevens JF. Vitamins C and E: Beneficial effects from a mechanistic perspective. Free Radic Biol Med. 2011;51:1000–13. doi: 10.1016/j.freeradbiomed.2011.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jihen El H, Sonia S, Fatima H, Mohamed Tahar S, Abdelhamid K. Interrelationships between cadmium, zinc and antioxidants in the liver of the rat exposed orally to relatively high doses of cadmium and zinc. Ecotoxicol Environ Saf. 2011;74:2099–104. doi: 10.1016/j.ecoenv.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 11.Al-Wabel NA, Hassan A, Abbas H, Muosa H. Antiulcerogenic effect of camel milk against ethanol induced gastric ulcers in rats. Webmedcentral Vet Med. 2012;3:WMC002804. [Google Scholar]
- 12.Boonchum W, Vacharapiyasophon P, Kanjanapothi D, Pekkoh J, Amornlerdpison D, Pumas C, et al. Anti-gastric ulcer and acute oral toxicity of aqueous extract of Turbinaria conoides from the Gulf of Thailand. Chiang Mai J Sci. 2012;39:292–9. [Google Scholar]
- 13.Zahra AA, Kadir FA, Mahmood AA, Al-Hadis AA, Suzy SM, Sabri SZ, et al. Acute toxicity study and wound healing potential of Gynura procumbens leaf extract in rats. J Med Plants Res. 2011;5:2551–8. [Google Scholar]
- 14.Krishnaveni M, Anbu J, Nithya S, Anjana A, Prema S. Gastric antisecretory, antiulcer and cytoprotective properties of Tamira parpam (Bio-Copper) from earthworm. Int J Pharm Bio Sci. 2012;3:250–9. [Google Scholar]
- 15.Guo S, Gao Q, Jiao Q, Hao W, Gao X, Cao JM. Gastric mucosal damage in water immersion stress: Mechanism and prevention with GHRP-6. World J Gastroenterol. 2012;18:3145–55. doi: 10.3748/wjg.v18.i24.3145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.West GB. Testing for drugs inhibiting the formation of gastric ulcers. J Pharmacol Methods. 1982;8:33–7. doi: 10.1016/0160-5402(82)90005-5. [DOI] [PubMed] [Google Scholar]
- 17.Okabe S, Takeuchi K, Murata T, Urushidani T. Effects of cimetidine on healing of chronic gastric and duodenal ulcers in dogs. Am J Dig Dis. 1978;23:166–8. doi: 10.1007/BF01073194. [DOI] [PubMed] [Google Scholar]
- 18.Gupta J, Kumar D, Gupta A. Evaluation of gastric anti-ulcer activity of methanolic extract of Cayratia trifolia in experimental animals. Asian Pacific J Trop Dis. 2012;2:99–102. [Google Scholar]
- 19.Megala J, Geetha A. Gastro protective and antioxidant effects of hydro alcoholic fruit extract of Pithecellobium dulce on ethanol induced gastric ulcer in rats. Pharmacology Online. 2010;2:353–72. [Google Scholar]
- 20.Malairajan P, Gopalakrishnan G, Narasimhan S, Veni KJ. Evalution of anti-ulcer activity of Polyalthia longifolia (Sonn.) Thwaites in experimental animals. Indian J Pharmacol. 2008;40:126–8. doi: 10.4103/0253-7613.42306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Akuodor GC, Akpan JL, Ezeunala Mercy N, Ajoku Gloria A, Essien AD, Megwas AU, et al. Evaluation of anti-ulcer and antimicrobial effects of Verbena hastata leaf extract. Afr J Pharm Pharmacol. 2012;6:778–82. [Google Scholar]
- 22.Khare S, Asad M, Dhamanigi SS, Prasad VS. Antiulcer activity of cod liver oil in rats. Indian J Pharmacol. 2008;40:209–14. doi: 10.4103/0253-7613.44152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gülçin I, Küfrevioglu OI, Oktay M, Büyükokuroglu ME. Antioxidant, antimicrobial, antiulcer and analgesic activities of nettle (Urtica dioica L.) J Ethnopharmacol. 2004;90:205–15. doi: 10.1016/j.jep.2003.09.028. [DOI] [PubMed] [Google Scholar]
- 24.Khaskheli M, Arain MA, Chaudhry S, Soomro AH, Qureshi TA. Physico-chemical quality of camel milk. J Agric Soc Sci. 2005;2:164–6. [Google Scholar]
- 25.Al-Abdullah MA, Al-Bayaty FH, Younis LT, Abu Hassan MI. Anti-ulcer activity of Centella asiatica leaf extract against ethanol-induced gastric mucosal injury in rats. J Med Plant Res. 2010;4:1253–9. [Google Scholar]
- 26.Farah Z. Camel Milk Properties and Products. St. Gallen, Switzerland: SKAT, Swiss Centre for Developments Cooperation in Technology and Management; 1996. [Google Scholar]
- 27.Read BE. Chemical constituents of camel urine. J Biol Chem. 1925;64:615–7. [Google Scholar]
- 28.Gandhi MN, Challa SR, Prasanth P, Gandhi TR. Role of leukotrienes in NSAID induced gastric ulceration and inflammation in wistar rats. Asian Pac J Trop Disease. 2012;2:215–19. [Google Scholar]
- 29.Oluwabunmi IJ, Abiola T. Gastroprotective effect of methanolic extract of Gomphrena celosioides on indomethacin induced gastric ulcer in Wistar albino rats. Int J Appl Basic Med Res. 2015;5:41–5. doi: 10.4103/2229-516X.149238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goel P, Ross-Degnan D, Berman P, Soumerai S. Retail pharmacies in developing countries: A behavior and intervention framework. Soc Sci Med. 1996;42:1155–61. doi: 10.1016/0277-9536(95)00388-6. [DOI] [PubMed] [Google Scholar]
- 31.Morsy MA, El-Moselhy MA. Mechanisms of the protective effects of curcumin against indomethacin-induced gastric ulcer in rats. Pharmacology. 2013;91:267–74. doi: 10.1159/000350190. [DOI] [PubMed] [Google Scholar]
- 32.El-Ashmawy NE, Khedr EG, El-Bahrawy HA, Selim HM. Gastroprotective effect of garlic in indomethacin induced gastric ulcer in rats. Nutrition. 2016;32:849–54. doi: 10.1016/j.nut.2016.01.010. [DOI] [PubMed] [Google Scholar]
- 33.Lehmann JM, Lenhard JM, Oliver BB, Ringold GM, Kliewer SA. Peroxisome proliferator-activated receptors alpha and gamma are activated by indomethacin and other non-steroidal anti-inflammatory drugs. J Biol Chem. 1997;272:3406–10. doi: 10.1074/jbc.272.6.3406. [DOI] [PubMed] [Google Scholar]
- 34.Atalay F, Odabasoglu F, Halici M, Cakir A, Cadirci E, Aslan A, et al. Gastroprotective and antioxidant effects of Lobaria pulmonaria and Its metabolite rhizonyl alcohol on indomethacin-induced gastric ulcer. Chem Biodivers. 2015;12:1756–67. doi: 10.1002/cbdv.201400432. [DOI] [PubMed] [Google Scholar]


