Abstract
Introduction
Treatment of unresectable liver metastases (LM) from uveal melanoma (UM) remains a major clinical challenge. Systemic chemotherapy and chemoimmunotherapy regimens extrapolated from cutaneous melanoma are considered to be ineffective in therapy of metastases from uveal melanoma. Studies suggest that the progression of hepatic metastases rather than the primary tumor or metastases in other organs determines survival.
Case report
We report a case of transarterial chemoembolization of 57-year-old man diagnosed with unresectable liver metastases from uveal melanoma with irinotecan eluting beads. Therapy resulted in long progression free survival and overall survival, 41 months and 45 months after diagnosis of metastatic disease respectively. Patient did not experience any major side effects of the therapy. Follow-up CTs indicate stable disease in mRECIST criteria and partial response in CHOI criteria.
Conclusions
Transarterial chemoembolization with drug eluting beads loaded with irinotecan may be an effective treatment of unresectable liver metastases from uveal melanoma.
Keywords: endovascular procedures, melanoma, therapeutic chemoembolization, liver neoplasms, eye neoplasms/pathology
Introduction
Treatment of unresectable liver metastases (LM) from uveal melanoma (UM) remains a major clinical challenge. UM is the most common primary ocular tumor in adults and the second most common melanoma after cutaneous sources, representing approximately 5% of all melanoma diagnoses. The incidence of uveal melanoma in Europe differs according to the country of origin of the patient, with an average incidence of 8 per million in the northern countries and 2 per million in the southern countries [1]. Approximately 4% of patients have metastatic disease at the time of diagnosis of the primary lesion [2]. Despite undergoing treatment of the primary tumor with either enucleation or radiation therapy, approximately 50% of patients develop metastatic uveal melanoma (MUM). The liver is the most common site of metastasis in ocular melanoma and its occurrence is estimated at 89–93% of the cases according to different studies [2, 3]. Systemic chemotherapy and chemoimmunotherapy regimens extrapolated from cutaneous melanoma are considered to be ineffective in therapy of metastases from uveal melanoma [3]. Those with metastatic disease have poor prognosis, with median overall survival 2 to 15 months [3]. There are various possibilities of treatment of metastatic uveal melanoma, including systemic treatment with immunotherapy, chemotherapy, surgery and regional approaches such as percutaneous hepatic perfusion, hepatic isolated perfusion, radiofrequency ablation and transarterial chemoembolization (TACE) [4]. Studies suggest that the progression of hepatic metastases rather than the primary tumor or metastases in other organs determines survival [5, 6]. The present study describes a patient treated with TACE who underwent 16 TACE procedures with irinotecan eluting beads (DEBIRI), had long progression free and overall survival and did not experience any major side effects of the therapy.
Case study
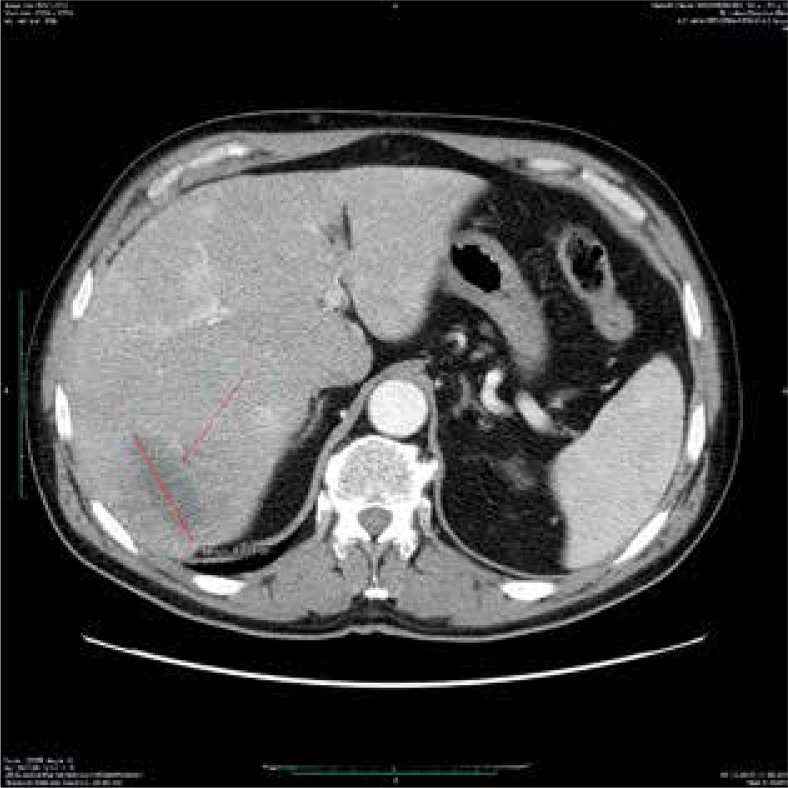
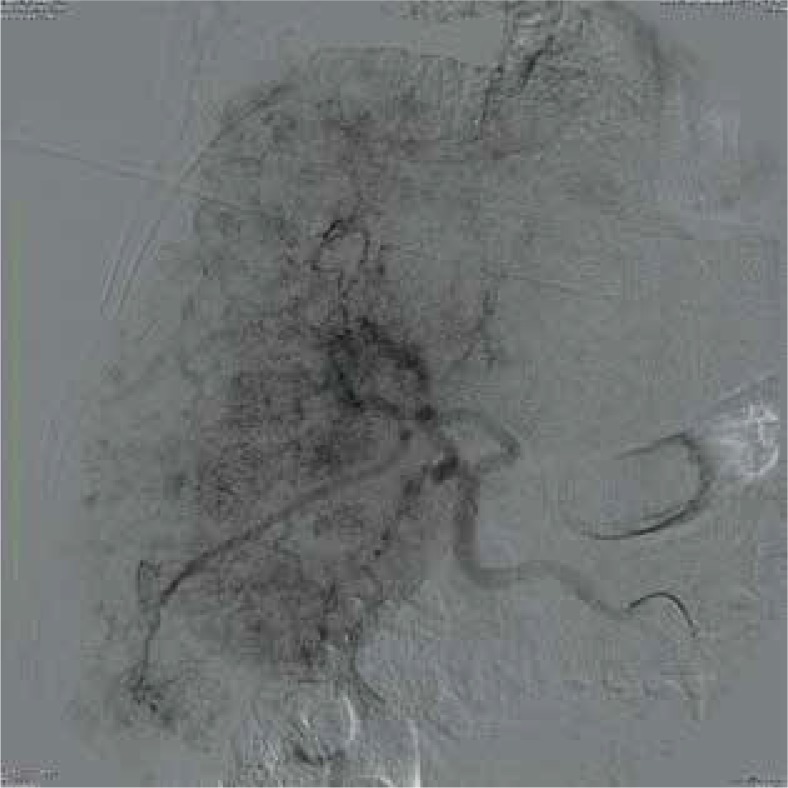
The patient, a 57-year-old caucasian male, was diagnosed with left sided uveal melanoma in December 2010. The primary tumor was treated with brachytherapy Ru106. In November 2012 liver metastases were diagnosed. The patient underwent systemic chemotherapy. Subsequently, based on CT scans, as well as a clinical evaluation the patient was qualified for transarterial chemoembolization (Fig. 1, 2). The liver was a dominant place of metastases, involved in less than 60% of volume and the lesions were unresectable. The angiographic image of metastases was diffuse infliltrative staining pattern without distinct nodularity (Fig. 3). He underwent four cycles of TACE between 31st Aug 2014 and 5th Nov 2015, 4 procedure per cycle. The procedure consisted of two stages: digital subtraction angiography (DSA) and subsequent administration of drug-loaded beads. Seldinger technique was used to access the common femoral artery, using 5F introductor (Balton, Warsaw, Poland). Superior mesenteric and celiac trunk angiographies was performed with catheter Cobra 5F (Glidecath, Terumo, USA) to evaluate for flow direction and variant arterial anatomical features. Angiography revealed multiple, diffuse metastatic lesions in both lobes of the liver. Celiac trunk angiography was followed by subselection of left of right hepatic artery with a catheter Cobra 4F (Glidecath, Terumo, USA) and administration of 1 mg of atropine. Subsequently, DC Beads (Biocompatibles International plc, Surrey, UK) with diameter of 100–300 μm loaded with 100 mg of irinotecan admixed with 8 ml of contrast medium (Ultravist 300) were infused at the rate of 1ml/min under fluoroscopic guidance. TACE was performed under analogosedation. After each procedure patient was hospitalized on the surgical ward, usually for two days for monitoring and pain control. Treatment related morbidity was low grade and included transient loss of appetite and abdominal pain lasting for approximately 12 hours after the procedure. No major adverse reactions were noted and the patient’s liver function tests and bilirubin levels were within normal limits. The procedures were performed in two week intervals.
Fig. 1.
Pretreatment CT shows one target lesion measuring 87 mm in diameter and attenuation of 81 HU (arrow)
Fig. 2.
CT scan after the last cycle of TACE showing decrease in diameter of the target lesion (60 mm) and a decrease in attenuation – 39 HU (arrow)
Fig. 3.
Pretreatment angiogram shows diffuse pattern of contrast enhancement throughout liver without distinct nodules
Each TACE cycle was followed by a CT scan in order to assess the efficacy of the treatment and to qualify patient for the next cycle. Response to the treatment was quantified using modified response evaluation criteria in solid tumors (mRECIST) and modified Choi criteria. The sum of diameters of the viable target lesions was reduced by 25% after the last cycle of TACE which qualifies as stable disease in mRECIST criteria. Mean tumors attenuation of the target lesions decreased by 52% (from 95 HU to 42 HU) which combined with the decrease in the size of the tumors is a partial response according to Choi criteria.
The patient’s quality of life was monitored by means of WHOQOL – BREF questionnaire before the first cycle and throughout the treatment. The results indicate maintenance of the overall quality of life.
In the first half of 2016, patient developed anemia which required multiple transfusions. In April 2016 PET scan indicated progressive disease with multiple metastases in peritoneum, bones and subcutaneous tissue of abdomen, head and neck. Patient died in August 2016. Therefore, the progression free survival after the diagnosis of the metastases was 41 months and 20 months after the beginning of TACE. His overall survival was 45 months.
Discussion
Although UM is the most common primary ocular malignancy in adults and uveal tract is the second most common site of melanomas, it is a rare disease with an average incidence of 8 per million in the northern European countries and 2 per million in the southern European countries [1]. Local therapy of uveal melanoma has improved significantly with increased use of conservative treatment and preservation of the eye. Nevertheless, improvements in the management of primary lesion have not been reflected in a significant increase in survival rates, and metastatic disease remains a leading cause of death among patients with uveal melanoma [7]. Up to 50% of patients develop metastatic disease and liver is most common site of metastases (89–93%), with other common sites being the lungs (24%) and bones (16%) [2, 3]. The prognosis of patients with metastatic uveal melanoma is poor, with median overall survival of 2 to 15 months [3, 8]. Studies suggest that the progression of hepatic metastases determines patients’ survival more than the primary tumor or metastases in other organs [1, 5, 6].
There are multiple possible approaches to the management of metastatic uveal melanoma, which include systemic treatment with chemotherapy, immunotherapy, surgery and locoregional approaches such as percutaneous hepatic perfusion, hepatic isolated perfusion, radiofrequency ablation and transarterial chemoembolization (TACE) [2, 3, 7, 9].
The review by Agarwala et al. analyzed the results of six comparative studies evaluating the efficacy of surgical excision as treatment of LM from UM. The matastesectomy offered a survival benefit with median overall survival ranging from 14 to 24 months after resection while survival in nonsurgical care group was 3 to 12 months. However, most of the patients with LM from UM are usually not surgical candidates and only 2% to 7% are offered surgery [2, 10]. For the rest of the patients the possible treatment options are systemic and regional therapies. Multiple chemotherapeutic and immunotherapeutic agents have been tested in patients with MUM, however the reported response rates were generally less than 5% and the median overall survival ranged from 6.0 to 14.0 months [2, 7, 9]. Moreover, the biology of uveal melanoma differs significantly from that of cutaneous melanoma. BRAF, RAS and KIT mutations are generally rare in ocular melanoma and therefore the targeted therapies developed for cutaneous melanoma are unlikely to be efficacious in treatment of UM [9, 11, 12]. Studies of several UM specific target agents (e.g. selumatinib, sorafenib, cixutumumab, vorinostat, everolimus, pasireotide, AEB071, genetespib, cabozantinib) are being investigated [9].
As there has been no effective systemic treatment for metastatic disease and most of patients with MUM are not suitable for surgical excision, regional therapies have been investigated. They share an advantage of delivering treatment directly to radiologically evident tumors while simultaneously minimizing systemic toxicity [2, 7, 13]. The regional treatments include hepatic intra-arterial infusions (HIA), chemoembolization (TACE), and isolated and percutaneous hepatic perfusions (IHP and PHP). Some of the procedures require open surgical techniques while others are minimal access procedures. The latest studies regarding HIA with fotemustine in MUM had overall response rate ranging from 16 to 36%, and median overall survival from 9 to 21 months [14–17]. In IHP the vaculature supply to the liver is surgically isolated. Melphalan has been the most commonly employed chemotherapeutic agent in that approach. A couple of studies reported high overall response rate in the range of 33 to 60%, however median overall survival was between 10 and 12 months [18, 19]. PHP is a nonoperative alternative to IHP. A randomized controlled phase 3 trial of PHP with melphalan compared to best alternative care reported. a prolonged hepatic progression free survial with PHP (8.1 vs. 1.6 months) with no advantage in terms of overall survival (11.4 vs. 9.9 months) [20]. A recent multi-centre study of percutaneous isolated hepatic perfusion with Melphalan conducted by Vogl et al. [21] reported median OS of 9.6 months (range 1.6–41.0 months) and median PFS of 12.4 months (range 0.9–41.0 months). The partial response rate in this study was 44% (8/18).
Our case study, as well as reports by others demonstrate the efficacy of TACE in patients suffering from this condition. Our patient’s survival of 45 months after diagnosis of metastatic disease and 24 months survival since the first chemoembolization compares favorably to other studies. Moreover, absence of any significant adverse effect despite undergoing 16 TACE procedures and stable quality of life score affirm TACE’s role as a palliation. Schuster et al. [22] conducted a study of 25 patients who failed systemic therapy and were treated with TACE with fotemustine or cisplatin mixed with starch microspheres (Spherex). He reported median overall survival time of 6 months and median progression free survival was 3 months. Carling et al. [23] treated 14 patients with DEBIRI TACE and the median overall survival in this study was 9,4 months. They suggested that there was no significantly different impact on survival to other chemoembolization techniques. Venturini et al. [24] reported DEBIRI as a first-line approach in five chemotherapy-naïve patient suffering from uveal melanoma metastasis to the liver. The mean follow-up period in this study was 16.3 months. In 2005 Patel et al. [25] conducted a phase II clinical trial for patients with LMs from UM and showed that survival in patients with LMs from UM depends on the radiologic response to the treatment. Patients with complete or partial response had median survival of 21.9 months, for patients with stable disease 8.7 months and for patients with progressive disease 3.3 months. In our case study patient had a long survival despite stable disease according to mRECIST criteria. Similar results were published by Huppert et al. in 2008 [26]. However, there are several papers based on results of treatment of hepatocellular carcinoma, that have reported necrosis of liver tumors despite absence of a substantial regression in radiologic studies [27, 28]. These can account for our patient’s long survival despite having stable disease according to mRECIST. Moreover, in modified Choi criteria the patient’s response was assessed as partial response. In 2008 Sharma et al. [29] reported a significantly better survival in patients with nodular angiographic pattern of liver metastases compared to patients with diffuse tumors (mean 621 days vs. 115 days). On the contrary, our patient had a diffuse angiographic pattern of liver tumors and experienced a long survival.
Conclusions
Therapy of unresectable liver metastases from uveal melanoma remains a major clinical problem. In the absence of effective systemic agents, regional therapies are an important option for patients with unresectable liver metastases from uveal melanoma. We present a case of a 56 man who was treated for LMs from UM with TACE with irinotecan eluting beads who achieved PFS of 41 months and OS of 45 months. According to mRECIST the response was stable disease while regarding modified Choi criteria it was a partial response. Moreover, absence of any significant adverse effect despite undergoing 16 TACE procedures and stable quality of life score affirm TACE’s role as a palliation.
Footnotes
The authors declare no conflict of interest.
References
- 1.Jovanovic P, Mihajlovic M, Djordjevic-Jocic1 J, Vlajkovic S, Cekic S, Stefanovic V. Ocular melanoma: an overview of the current status. Int J Clin Exp Pathol. 2013;6:1230–44. [PMC free article] [PubMed] [Google Scholar]
- 2.Agarwala SS, Eggermont AMM, O’Day S, Zager JS. Metastatic Melanoma to the liver: a contemporary and comprehensive review of surgical, systemic, and regional therapeutic options. Cancer. 2014;120:781–9. doi: 10.1002/cncr.28480. [DOI] [PubMed] [Google Scholar]
- 3.Goh AYL, Layton CJ. Evolving systemic targeted therapy strategies in uveal melanoma and implications for ophthalmic management: a review. Clin Experiment Ophthalmol. 2016;44:509–19. doi: 10.1111/ceo.12688. [DOI] [PubMed] [Google Scholar]
- 4.Valpione S, Aliberti C, Parrozzani R, Bazzi M, Pigozzo J, Midena E, Pilati P, Campana LG, Chiarion-Sileni V. A retrospective analysis of 141 patients with liver metastases from uveal melanoma: a two-cohort study comparing transarterial chemoembolizan. Melanoma Res. 2015:164–8. doi: 10.1097/CMR.0000000000000129. [DOI] [PubMed] [Google Scholar]
- 5.Diener-West M, Hawkins BS, Markowitz JA, Schachat AP. A review of mortality from choroidal melanoma. Part II. A meta-analysis of 5-year mortality rates following enucleation, 1966 through 1988. Arch Ophtalmol. 1992;110:245–50. doi: 10.1001/archopht.1992.01080140101036. [DOI] [PubMed] [Google Scholar]
- 6.Rajpal S, Moore S, Karakousis CP. Survival in metastatic ocular melanoma. Cancer. 1983:334–36. doi: 10.1002/1097-0142(19830715)52:2<334::aid-cncr2820520225>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 7.Singh AD, Turell ME, Topham AK. Uveal melanoma: trends in incidence, treatment, and survival. Ophtalmology. 2011;118:1881–5. doi: 10.1016/j.ophtha.2011.01.040. [DOI] [PubMed] [Google Scholar]
- 8.Sato T, Babazono A, Shields JA, Shields CL, De Potter P, Mastrangelo MJ. Time to systemic metastases in patients with posterior uveal melanoma. Cancer Invest. 1997;15:98–105. doi: 10.3109/07357909709115761. [DOI] [PubMed] [Google Scholar]
- 9.Buder K, Gesierich A, Gelbrich G, Goebeler M. Systemic treatment of metastatic uveal melanoma: review of literature and future perspectives. Cancer Medicine. 2013;2:674–86. doi: 10.1002/cam4.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mariani P, Piperno-Neumann S, Servois V, et al. Surgical management of liver metastases from uveal melanoma: 16 years’ experience at the Institut Curie. Eur J Surg Oncol. 2009;35:1192–7. doi: 10.1016/j.ejso.2009.02.016. [DOI] [PubMed] [Google Scholar]
- 11.Hofmann UB, Kauczok-Vetter CS, Houben R, Becker JC. Overexpression of the KIT/SCF in uveal melanoma does not translate into clinical efficacy of imatinib mesylate. Clin Cancer Res. 2009;15:324–9. doi: 10.1158/1078-0432.CCR-08-2243. [DOI] [PubMed] [Google Scholar]
- 12.Rimoldi D, Salvi S, Lienard D, et al. Lack of BRAF mutations in uveal melanoma. Cancer Res. 2003;63:5712–5. [PubMed] [Google Scholar]
- 13.Lewandowski R, Geschwind JF, Liapi E, Salem R. Transcathether Intraarterial Therapies: Rationale and Overview. Radiology. 2011;259:641–57. doi: 10.1148/radiol.11081489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agarwala SS, Kirkwood JM. Phase I/II randomized trial of intrahepatic arterial infusion chemotherapy with cisplatin and chemoembolization with cisplatin and polyvinyl sponge inpatients with ocular melanoma metastatic to the liver. Melanoma. 2004;14:217–22. doi: 10.1097/01.cmr.0000129377.22141.ea. [DOI] [PubMed] [Google Scholar]
- 15.Farolfi A, Ridolfi L, Guidoboni M, et al. Liver metastases from melanoma hepatic intra-arterial chemotherapy. A retrospective study. J Chemother. 2011;23:300–5. doi: 10.1179/joc.2011.23.5.300. [DOI] [PubMed] [Google Scholar]
- 16.Heusner TA, Antoch G, Wittkowski-Sterczewski A, et al. Transarterial hepatic chemoperfusion of uveal melanoma metastases: survival and response to treatment. Rofo. 2011;183:1151–60. doi: 10.1055/s-0031-1281743. [DOI] [PubMed] [Google Scholar]
- 17.Peters S, Voelter V, Zografos L, et al. Intra-arterial hepatic fotemustine for the treatment of liver metastases from uveal melanoma: experience in 101 patients. Ann Oncol. 2006;17:578–83. doi: 10.1093/annonc/mdl009. [DOI] [PubMed] [Google Scholar]
- 18.Alexander HR, Libutti SK, Pingpank JF, et al. Hyperthermic isolated hepatic perfusion using melphalan for patients with ocular melanoma. Clin Cancer Res. 2003;9:6343–9. [PubMed] [Google Scholar]
- 19.van Iersel LB, Hoekman EJ, Gelderblom H, et al. Isolated hepatic perfusion with 200 mg melphalan for advanced noncolorectal liver metastases. Ann Surg Oncol. 2008;15:1891–988. doi: 10.1245/s10434-008-9881-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pingpank JF, Hughes M, Alexander HR, et al. Percutaneous hepatic perfusion (PHP) vs. best alternative care for patients with melanoma liver metastases: efficacy update of the phase 3 trial. Eur J Cancer. 2011;47 abstract 9304. [Google Scholar]
- 21.Vogl TJ, Koch SA, Lotz G, et al. Percutaneous Isolated Hepatic Perfusion as a Treatment for Isolated Hepatic Metastases of Uveal Melanoma: Patient Outcome and Safety in a Multi-centre Study. Cardiovasc Intervent Radiol. 2017;40:864. doi: 10.1007/s00270-017-1588-2. [DOI] [PubMed] [Google Scholar]
- 22.Schuster R, Lindner M, Wacker F, Krössin M, Bechrakis N, Foerster MH, Thiel E, Keilholz U, Schmittel A. Transarterial chemoembolization of liver metastases from uveal melanoma after failure of systemic therapy: toxicity and outcome. Melanoma Research. 2010;20:191–6. doi: 10.1097/CMR.0b013e328334c36e. [DOI] [PubMed] [Google Scholar]
- 23.Carling U, Dorenberg E, Haugyik S, Eide N, Bertzen, Bjorn E, Dueland S. Transarterial Chemoembolization of Liver Metastases from Uveal Melanoma Using Irinotecan-Loaded Beads: Treatment Response and Complications. Cardiovasc Intervent Radiol. 2015;38:1532–1541. doi: 10.1007/s00270-015-1093-4. [DOI] [PubMed] [Google Scholar]
- 24.Venturini M, Pilla L, Agostini G, Cappio S, Losio C, Orsi M, Ratti F, Aldrighetti L, De Cobelli F, Del Maschio A. Transarterial Chemoembolization with Drug-eluting Beads Preloaded with Irinotecan as a First-Line Approach in Uveal Melanoma Liver Metastases: Tumor Response and Predictive Value of Diffusion- weighted MR Imaging in Five Patients. J Vasc Interv Radiol. 2012;23:937–41. doi: 10.1016/j.jvir.2012.04.027. [DOI] [PubMed] [Google Scholar]
- 25.Patel K, Sullivan K, Berd D, Mastrangelo MJ, Shields CL, Shields JA, Sato T. Chemoembolization of the hepatic artery with BCNU for metastatic uveal melanoma: results of a phase II study. Melanoma Research. 2005;15:297–304. doi: 10.1097/00008390-200508000-00011. [DOI] [PubMed] [Google Scholar]
- 26.Huppert P E, Fierlbeckc G, Pereirab P, et al. Transarterial chemoembolization of liver metastases in patients with uveal melanoma. Eur J Radiol. 2010;74:38–44. doi: 10.1016/j.ejrad.2009.03.064. [DOI] [PubMed] [Google Scholar]
- 27.Ebied OM, Federle MP, Carr BI, Pealer KM, Li W, Amesur N, et al. Evaluation of responses to chemoembolization in patients with unresectable hepatocellular carcinoma. Cancer. 2003;97:1042–50. doi: 10.1002/cncr.11111. [DOI] [PubMed] [Google Scholar]
- 28.Takayasu K, Arii S, Matsuo N, Yoshikawa M, Ryu M, Takasaki K, et al. Comparison of CT findings with resected specimens after chemoembolization with iodized oil for hepatocellular carcinoma. Am J Roentgenol. 2000;175:699–704. doi: 10.2214/ajr.175.3.1750699. [DOI] [PubMed] [Google Scholar]
- 29.Sharma KV, Gould JE, Harbour JW, Linette GP, Pilgram TK, Dayani PN, Brown DB. Hepatic arterial chemoembolization for management of metastatic melanoma. AJR Am J Roentgenol. 2008;190:99–104. doi: 10.2214/AJR.07.2675. [DOI] [PubMed] [Google Scholar]