Abstract
Background
Surgical managements were recommended for unstable distal clavicle fracture owing to the high incidence of nonunion. The present study compared the efficacy of anatomical locking plate with versus without additional suture anchor fixation for the treatment of unstable Neer type II distal clavicle fractures.
Material/Methods
Between January 2013 to January 2015, 28 consecutive patients with unstable Neer type II fractures were treated by using anatomical locking plate with or without additional suture anchor fixation. The patients were divided into anatomical locking plate group (group A) and anatomical locking plate combined with suture anchor group (group B) according to the surgical method. The operative-related parameters such as operation time, blood loss, length of hospitalization, union time, functional outcomes (Constant score, UCLA score and DASH score) and CC distance were compared.
Results
The mean follow-up period of the 28 patients was 19.60 months (21.80 versus 18.39 months, respectively). No statistical differences in general and peri-operative parameters were found between 2 groups. The group B had significant higher Constant score than group A (P=0.004, 91.67 versus 83.10). While no statistical differences were reached in the UCLA score and DASH score between 2 groups (P=0.112 and 0.163, respectively). The group A had longer CC distance than group B (11.67 versus 8.94 mm), while no statistic difference was found (P=0.067).
Conclusions
For the treatment of acute unstable Neer type II distal clavicle fractures, both surgical methods could offer satisfactory outcome. However, anatomical locking plate combined with additional suture anchor fixation had a better functional and radiographic outcome than that without additional suture anchor fixation.
MeSH Keywords: Bone Plates, Clavicle, Fracture Fixation
Background
Distal clavicle fractures are very uncommon and account for approximately 21–28% of all fractures of the clavicle [1]. The weight of the arm, pectoralis major, pectoralis minor, latissimus dorsi, trapezius, and scapular motions act on the fracture site to impair union in unstable Neer type II clavicle fractures. Nonunion or malunion frequently occur after conservative treatment [2]. Therefore, surgical treatment is recommended for unstable Neer type II clavicle fractures[3].
Various surgical treatment techniques have been described for unstable Neer type II clavicle fractures, including trans-acromial Kirschner wires and Knowles pins, tension band wiring, coracoclavicular screw fixation, hook plate fixation, and locking compressive plate fixation [4–10]. However, none of these surgical methods is regarded as the criterion standard treatment.
Anatomical locking plate fixation is a popular surgical method for unstable distal clavicle fractures [10]. The advantage of the anatomical locking plate is that the acromioclavicular joint and the subacromial space are not violated [11]. However, the vertical stability of the fracture with plate fixation alone might not be sufficient due to small lateral fragments. Biomechanical research has shown that coracoclavicular (CC) internal fixation combined with fracture fixation can increase fracture stability more than any other surgical technique alone [12]. Recently, more and more fractures are reduced and fixed with additional suture anchors. Therefore, anatomical locking plate fixation combined with suture anchor fixation might be an alternative option for the treatment of distal clavicle fractures [13]. However, few studies have compared the results of anatomical locking plate fixation with or without CC ligament stabilization for unstable Neer type II clavicle fractures. The present study aimed to retrospectively compare the clinical and radiographic outcomes of these 2 surgical techniques.
Material and Methods
Source of patients
We retrospectively reviewed the clinical database of our hospital from January 2013 to January 2015. The inclusion criteria were: (1) Neer type II fractures; (2) Acute and unilateral fractures; (3) The surgical method should be anatomical locking plate for fixation alone or anatomical locking plate combined with CC ligament augmentation; (4) Normal shoulder function before injury; and (5) At least 12 months follow-up. Eventually, 28 patients (10 fixations with anatomical locking plate alone and 18 fixations with anatomical locking plate combined with CC ligament augmentation by using anchors) were selected according to these criteria. The patients were divided according to surgical method into an anatomical locking plate group (group A) and an anatomical locking plate combined with anchors group (group B). General information about these 28 patients is summarized in Table 1. The research was permitted by Ethnics Committee of the institute.
Table 1.
General information of two groups.
| Group A (n=10) | Group B (n=18) | P value* (2-tailed) | |
|---|---|---|---|
| Age (years) | 40.20±12.58 | 36.89±10.99 | 0.475 |
| Gender, M/F | 7/3 | 14/4 | 0.649 |
| Side of injury, Rt/Lt | 3/7 | 6/12 | 0.856 |
| Mechanism of injury, V/F | 2/8 | 3/15 | 0.825 |
| Time from injury to surgery (days) | 6.20±2.39 | 4.67±1.68 | 0.058 |
| Follow-up time (months) | 21.80±7.67 | 18.39±3.55 | 0.118 |
M/F – Male/Female; Rt/Lt – right/left; V/F – vehicle accident/fall from a height.
Chi-square test or Independent sample t test as appropriate.
Surgical procedure
Group A
Under general or interscalene anesthesia, the patient was operated on in the beach chair position. A transverse incision was made. The deltoid insertion over the clavicle was partially detached with a periosteal elevator. The acromioclavicular (AC) joint was left intact. The fracture site was exposed and reduced. The status of the reduction was confirmed by fluoroscopy. According to the fracture length and the morphology of the clavicle, an appropriate anatomical locking plate (AO-synthesis, USA) was selected and slightly flattened to fit the configuration of the distal and proximal fragment. Fixation was then completed with locking screws. Intraoperative radiographs confirmed the final fixation and ensured that the plate did not cross the AC joint and that all screws remained extra-articular. The CC ligament was not explored and repaired in this group.
Group B
The surgery was performed in the beach chair position and the skin incision was similar to that in group A. The anterior deltoid muscle was split from the medial segment of the clavicle to access the base of the coracoid process. After clearing the fracture site, the unruptured CC ligament was explored and identified. The fracture was temporarily reduced with reduction forceps and 2 bone tunnels were drilled on the end of the proximal fragment. One or two 5-mm Titanium suture anchors (Zimmer, USA) were fixed to the coracoids process. The suturing threads were passed through the 2 holes that had been made earlier in the medial fragment of the clavicle and were tied off in the anatomical position. Then, an anatomical locking plate (AO-synthesis, USA) and multiple locking screws were applied for internal fixation. The CC ligament was examined and augmented in this group.
Postoperative rehabilitation
In both of these groups, the shoulder was immobilized with an arm sling for 4 weeks. Controlled passive mobilization of the shoulder was allowed during the first week. Active assisted exercises were allowed at 3–4 weeks, depending on patient situation.
Clinical and radiographic evaluation
All patients were assessed clinically and radiographically at each outpatient visit. All medical records and radiographic examinations were reviewed to compare the operation time, blood loss during the operation, the length of the incision, and union time (Table 2). Successful union was defined by obliteration of the fracture gap on plain radiographs and no tenderness or pain at the fracture site during shoulder exercises [14]. At the final follow-up, we used a picture archiving and communication system (PACS) (Centricity, GE Healthcare, Little Chalfont, UK) to measure the CC distance. The accuracy of the PACS was assessed by measuring a radiographic marker with a known distance and was found to be accurate to within 0.05 mm [15]. Figure 1 shows how we measured the CC distance.
Table 2.
Perioperative situation of two groups.
| Group A | Group B | P value* (2-tailed) | |
|---|---|---|---|
| Length of incision (cm) | 7.60±0.97 | 8.00±1.08 | 0.341 |
| Operation time (min) | 76.50±18.11 | 86.94±26.63 | 0.280 |
| Blood loss (ml) | 74.00±21.19 | 97.50±42.29 | 0.114 |
| Length of hospital stay (days) | 6.80±1.48 | 6.11±1.45 | 0.242 |
Independent sample t test is applied.
Figure 1.
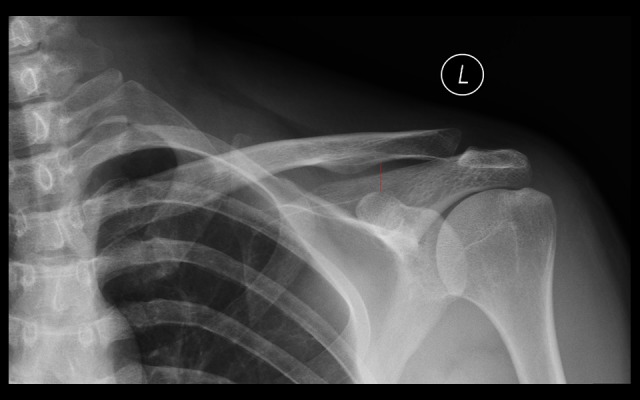
The measurement method of coracoclavicular(CC) distance on the anteroposterior radiograph.
For the evaluation of shoulder functional outcomes, Constant scores and University of California Los Angeles (UCLA) scores were recorded by the physician at the final follow-up. The test was performed by a surgeon who was not involved in treatment of patients. Furthermore, Disabilities of the Arm, Shoulder, and Hand (DASH) score was used to assess the upper extremity function, which was a questionnaire filled in by the patient at the final follow-up.
Data analysis
For quantitative data, the one-sample Kolmogorov-Smirnov test was used to test the normality of distribution. The independent-samples t test was used for approximately normally distributed parameters. Data are expressed as mean ±SD. For qualitative data, the chi-square test was used to compare differences between 2 groups. We considered P value <0.05 as statistically significant, and all tests were two-sided. SPSS17.0 was used for statistical analysis (SPSS, Chicago, IL, USA).
Results
General and peri-operative parameters
This study included a total of 28 cases. Group A comprised 10 patients (7 males, 3 females) treated with anatomical locking plate alone, and ages ranged from 24 to 56 years (mean 40.20 years). Three fractures occurred on the right side and 7 occurred on the left side. Two injuries were caused by vehicle accident and the 8 left fractures were caused by falls from a height. One of the patients also had an ipsilateral scapula fracture. Time from injury to surgery ranged from 3 to 10 days (mean 6.20 days). The follow-up time ranged from 12 to 35 months (mean 21.80 months). Group B comprised 18 patients (14 males, 4 females) treated with anatomical locking plate combined with anchors, and were ages 20–57 years (mean 36.89 years). Six fractures occurred on the right side and 12 occurred on the left side. Three injuries were caused by vehicle accident and the 15 left fractures were caused by falls from a height. Time from injury to surgery ranged from 2 to 9 days (mean 4.67 days). The follow-up time ranged from 15 to 25 months (mean 18.39 months). No significant differences existed in general parameters between the 2 groups (Table 1).
The peri-operative parameters between the 2 groups are presented in Table 2. No significant differences were found between the 2 groups in the incision length, operation time, blood loss, or length of hospital stay (p=0.341, 0.280, 0.114, and 0.242, respectively). Although these parameters were not significantly different, group A had shorter mean operation time (76.50 versus 86.94 min) and less intraoperative blood loss (74.00 versus 97.50 ml) than in group B.
Clinical and radiographic outcomes
The clinical and radiographic outcomes are presented in Table 3. For all patients, group B had significantly higher Constant scores than group A (P=0.004, 91.67 versus 83.10). Group A had lower UCLA score than group B, but the difference was not significantly different (P=0.112, 27.10 versus 29.44). Furthermore, the mean DASH score in group A was higher than in group B (P=0.163, 4.08 versus 2.82). However, a difference of only 1–3 points on the UCLA or DASH score might be clinically irrelevant. Group A had a longer CC distance (11.67 versus 8.94 mm) than in group B, but the difference was not statistically significant. Figures 2 and 3 show typical cases.
Table 3.
Clinical and radiographic outcomes.
| Group A | Group B | P value* (2-tailed) | |
|---|---|---|---|
| Constant score | 83.10±6.92 | 91.67±6.99 | 0.004 |
| UCLA score | 27.10±3.18 | 29.44±3.82 | 0.112 |
| DASH score | 4.08±2.43 | 2.82±2.10 | 0.163 |
| Union time (weeks) | 10.30±1.49 | 9.61±1.33 | 0.221 |
| CC distance (mm) | 11.67±5.37 | 8.94±2.19 | 0.067 |
UCLA – University of California – Los Angeles; DASH – disabilities of the arm, shoulder and hand; CC – coracoclavicular.
Independent sample t test is applied.
Figure 2.
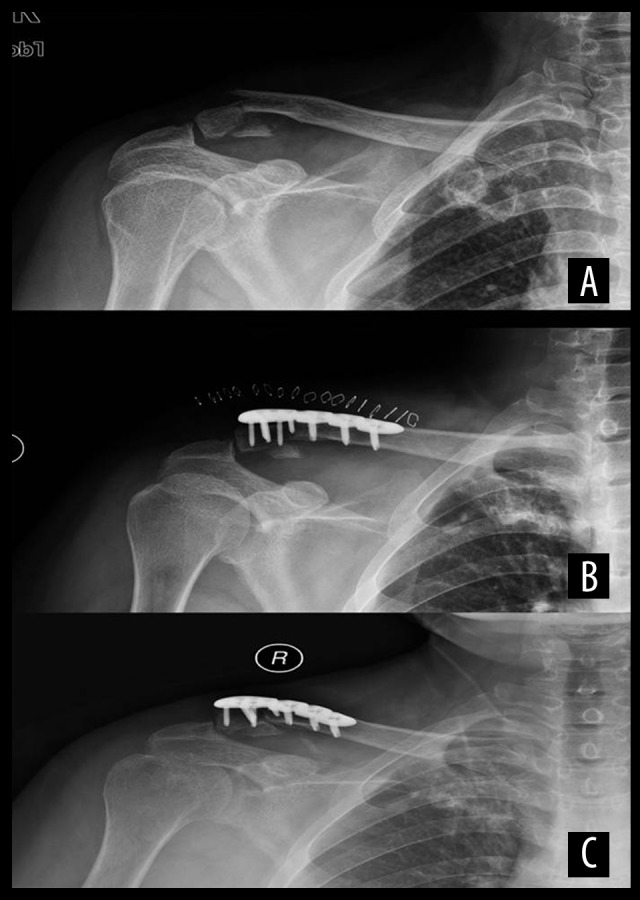
A 34-year-old male patient had a left distal clavicle fracture treated with an anatomical locking plate without coracoclavicular (CC) augmentation. (A) Preoperative X-ray showed a Neer type IIb distal clavicle fracture. (B) Radiograph in the immediate postoperative period showed good fracture reduction. (C) X-rays at 23 months after surgery showed good fracture healing.
Figure 3.
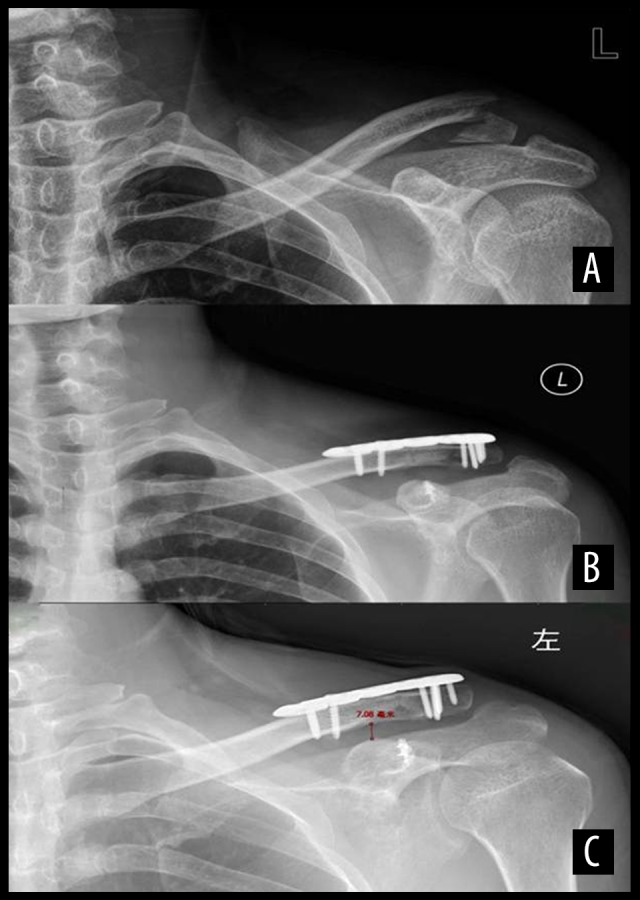
A 47-year-old female patient had left distal clavicle fracture treated with an anatomical locking plate with coracoclavicular (CC) augmentation. (A) Preoperative X-ray showed a Neer type IIb distal clavicle fracture. (B) Radiograph at the immediate postoperative period showed good fracture reduction. (C) X-rays at 32 months after surgery showed good fracture healing.
Complications
All patients in 2 groups achieved bony union in the final follow-up. The union time was 10.30 weeks in group A and 9.61 weeks in group B. There was not significant difference in union time between the 2 groups. One patient in group A had superficial wound infection and the plate has been placed inappropriately. After the administration of antibiotics, the wound healed well and the implant was removed 3 months postoperatively. The patient showed satisfactory function at the final follow-up (Figure 4). Two patients in B group reported implant-related discomfort during shoulder motion. The symptom disappeared after removal of the plate. All patients were eventually able to resume their previous occupation with no difficulty.
Figure 4.
A 24-year-old male patient had a left distal clavicle fracture treated with an anatomical locking plate. (A) Preoperative X-ray showed a Neer type IIb distal clavicle fracture. (B) Radiograph at the immediate postoperative period showed good fracture reduction, but the plate was placed inappropriately. (C) Radiograph immediately after removal of the plate 3 months after surgery. (D) X-rays 12 months after surgery showed good fracture healing.
Discussion
Unstable distal clavicle fractures usually have a high rate of nonunion or delayed union due to the specific biomechanical feature [2]. The significance of nonunion has been greatly debated in the past. Nowak et al. [16] studied 222 patients and verified that 93 patients still had sequelae at 6 months with conservative treatment. Moreover, long-term immobilization might result in muscle atrophy and resultant shoulder joint dyskinesia. Restoration of these kinetics requires extensive physiotherapy and biokinetic training, which is expensive and time-consuming [13,17]. Therefore, surgical treatment might be more suitable for these injuries. Various surgical methods are described in the literature [4,6–10,18–20]. Although a few studies reported the outcomes of surgical methods on anatomical locking plate fixation or anatomical locking plate fixation combined with CC stabilization, none of these studies had control groups [10,20,21]. To the best of our knowledge, the present study is the first to compare the result of the anatomical locking plate fixation alone versus anatomical locking plate fixation combined with CC augmentation by using anchors.
One surgical method commonly used for distal clavicle fractures is hook plate fixation. Although hook plate fixation can provide stable fixation to prevent AC joint displacement, various complications had been reported, such as subacromial shoulder impingement, rotator cuff lesion, subacromial bony erosion, and acromial osteolysis [22–24]. Furthermore, a second operation is often needed to remove the implant. However, anatomical locking plate for distal clavicle is reported to achieve firm and stable fixation with multiple screw placement in the distal fragment [21]. The multiple, divergent, fixed-angled screws in the distal fragment seem to increase pullout strength because the stability provided by the locking plate and screws does not solely depend on the friction between the bone and plate. Moreover, the angular stability of the locking plate and screws can provide better resistance against bending and torsion forces than use of the traditional compressive plate. Since the anatomical locking plate does not violate the subacromial space and AC joint, complications such as AC joint osteoarthritis, subacromial shoulder impingement, fixation failure, and subacromial bursitis can be reduced.
However, fixation failure in the distal fragment with the use of anatomical locking plate and screws for clavicle fracture has been reported [25]. Coracoclavicular ligament augmentation has been described as a treatment for unstable distal clavicle fractures [14,26]. This technique might be a supplementary method to the locking plate to reduce the fixation failure. A few studies have investigated the outcome of CC ligament augmentation with different surgical techniques [27–30]. Herrmann et al. [27] studied 8 people who underwent surgery by using locking T-plates and suture anchor stabilization for the treatment of unstable distal fracture. The results showed that the mean Constant score was 93.3 and the CC distance was successfully restored with a mean 1-mm side-to-side difference, and all patients reached an early clinical and radiographic outcome, with a mean follow-up time of only 8.3 months. Johnston et al. [28] reported 6 patients with clinically unstable type II distal clavicle fractures undergoing treatment by using fracture-specific plate and coracoclavicular augmentation with a suture button, showing that patients had reliable union rates and excellent functional scores.
Biomechanical analysis comparing the results of distal clavicle fracture fixed with anatomical locking plate with or without CC fixation has been reported. Madsen et al. [19] used 12 fresh-frozen matched cadaveric specimens (2 groups, with or without CC fixation) to determine the effect of CC fixation on biomechanical stability in type IIb distal clavicle fractures fixed with a superior locking plate. The results revealed that CC fixation added stability to type IIb distal clavicle fractures fixed with a plate and screws when loaded to failure. Therefore, CC fixation might be a useful method to augment stability of distal clavicle fractures. However, no clinical trial has compared the results of distal clavicle fractures fixed with an anatomical locking plate with versus without CC fixation.
The present study compared functional scores and postoperative CC distance between these 2 groups by using anatomical locking plate fixation with or without CC augmentation. The results showed that all patients had relatively good clinical results. Although a few complications were found, all patients achieved bony union and satisfactory function at the final follow-up. However, patients fixed with an additional CC fixation had a better clinical and radiographic outcome than patients without CC fixation at the final follow-up. Moreover, patients in group A had a relatively longer CC distance than patients in group B, although the difference was not significant. CC fixation can augment the stability of distal clavicle fractures, enabling the patient to return to work earlier than treatment without CC fixation, which requires prolonged immobilization. This means that use of an anatomical locking plate is useful for treatment of distal clavicle fractures, and CC fixation might be an effective supplement to augment the stability of distal clavicle fractures.
There were a few limitations to our study. First, this was a retrospective study and was not randomized. Second, the sample was relatively small and the follow-up period was relatively short. Third, this study did not measure the CC distance on the uninjured side after surgery. Fourth, the operation was not performed by a single surgeon, which might have influenced the outcomes. A larger, multi-center, prospective, randomized study is needed to confirm the surgical methods presented in this study.
Conclusions
Both of these surgical techniques for unstable distal fractures by using anatomical locking plate with or without CC augmentation can achieve bony union and have good functional results. However, use of an anatomical locking plate with CC augmentation has better functional and radiographic outcomes than treatment without CC augmentation. Therefore, a combination of anatomical locking plate and CC ligament augmentation is a reliable treatment option for unstable distal clavicle fractures.
Footnotes
Source of support: This work was supported by The Capital Medical Emergency Engineering Construction of Science and Technology Research (5 minutes)
References
- 1.Sambandam B, Gupta R, Kumar S, Maini L. Fracture of distal end clavicle: A review. J Clin Orthop Trauma. 2014;5(2):65–73. doi: 10.1016/j.jcot.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Edwards DJ, Kavanagh TG, Flannery MC. Fractures of the distal clavicle: A case for fixation. Injury. 1992;23(1):44–46. doi: 10.1016/0020-1383(92)90125-c. [DOI] [PubMed] [Google Scholar]
- 3.Bisbinas I, Mikalef P, Gigis I, et al. Management of distal clavicle fractures. Acta Orthop Belg. 2010;76(2):145–49. [PubMed] [Google Scholar]
- 4.Wang SJ, Wong CS. Extra-articular knowles pin fixation for unstable distal clavicle fractures. J Trauma. 2008;64(6):1522–27. doi: 10.1097/TA.0b013e3180593646. [DOI] [PubMed] [Google Scholar]
- 5.Neer CS., 2nd Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968;58:43–50. [PubMed] [Google Scholar]
- 6.Kao FC, Chao EK, Chen CH, et al. Treatment of distal clavicle fracture using Kirschner wires and tension-band wires. J Trauma. 2001;51(3):522–25. doi: 10.1097/00005373-200109000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Macheras G, Kateros KT, Savvidou OD, et al. Coracoclavicular screw fixation for unstable distal clavicle fractures. Orthopedics. 2005;28(7):693–96. doi: 10.3928/0147-7447-20050701-18. [DOI] [PubMed] [Google Scholar]
- 8.Daglar B, Delialioglu OM, Minareci E, et al. [An alternative fixation method for the treatment of unstable distal clavicle fractures: Locked distal radius plate]. Acta Orthop Traumatol Turc. 2009;43(4):324–30. doi: 10.3944/AOTT.2009.324. [in Turkich] [DOI] [PubMed] [Google Scholar]
- 9.Lee YS, Lau MJ, Tseng YC, et al. Comparison of the efficacy of hook plate versus tension band wire in the treatment of unstable fractures of the distal clavicle. Int Orthop. 2009;33(5):1401–5. doi: 10.1007/s00264-008-0696-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shin SJ, Ko YW, Lee J, Park MG. Use of plate fixation without coracoclavicular ligament augmentation for unstable distal clavicle fractures. J Shoulder Elbow Surg. 2016;25(6):942–48. doi: 10.1016/j.jse.2015.10.016. [DOI] [PubMed] [Google Scholar]
- 11.Klein SM, Badman BL, Keating CJ, et al. Results of surgical treatment for unstable distal clavicular fractures. J Shoulder Elbow Surg. 2010;19(7):1049–55. doi: 10.1016/j.jse.2009.11.056. [DOI] [PubMed] [Google Scholar]
- 12.Rieser GR, Edwards K, Gould GC, et al. Distal-third clavicle fracture fixation: A biomechanical evaluation of fixation. J Shoulder Elbow Surg. 2013;22(6):848–55. doi: 10.1016/j.jse.2012.08.022. [DOI] [PubMed] [Google Scholar]
- 13.Fleming MA, Dachs R, Maqungo S, et al. Angular stable fixation of displaced distal-third clavicle fractures with superior precontoured locking plates. J Shoulder Elbow Surg. 2015;24(5):700–4. doi: 10.1016/j.jse.2014.09.024. [DOI] [PubMed] [Google Scholar]
- 14.Chen CY, Yang SW, Lin KY, et al. Comparison of single coracoclavicular suture fixation and hook plate for the treatment of acute unstable distal clavicle fractures. J Orthop Surg Res. 2014;9:42. doi: 10.1186/1749-799X-9-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cook JB, Shaha JS, Rowles DJ, et al. Clavicular bone tunnel malposition leads to early failures in coracoclavicular ligament reconstructions. Am J Sports Med. 2013;41(1):142–48. doi: 10.1177/0363546512465591. [DOI] [PubMed] [Google Scholar]
- 16.Nowak J, Holgersson M, Larsson S. Sequelae from clavicular fractures are common: A prospective study of 222 patients. Acta Orthop. 2005;76(4):496–502. doi: 10.1080/17453670510041475. [DOI] [PubMed] [Google Scholar]
- 17.Jupiter JB, Leffert RD. Non-union of the clavicle. Associated complications and surgical management. J Bone Joint Surg Am. 1987;69(5):753–60. [PubMed] [Google Scholar]
- 18.Duralde XA, Pennington SD, Murray DH. Interfragmentary suture fixation for displaced acute type II distal clavicle fractures. J Orthop Trauma. 2014;28(11):653–58. doi: 10.1097/BOT.0000000000000122. [DOI] [PubMed] [Google Scholar]
- 19.Madsen W, Yaseen Z, LaFrance R, et al. Addition of a suture anchor for coracoclavicular fixation to a superior locking plate improves stability of type IIB distal clavicle fractures. Arthroscopy. 2013;29(6):998–1004. doi: 10.1016/j.arthro.2013.02.024. [DOI] [PubMed] [Google Scholar]
- 20.Schliemann B, Rosslenbroich SB, Schneider KN, et al. Surgical treatment of vertically unstable lateral clavicle fractures (Neer 2b) with locked plate fixation and coracoclavicular ligament reconstruction. Arch Orthop Trauma Surg. 2013;133(7):935–39. doi: 10.1007/s00402-013-1737-2. [DOI] [PubMed] [Google Scholar]
- 21.Lee SK, Lee JW, Song DG, Choy WS. Precontoured locking plate fixation for displaced lateral clavicle fractures. Orthopedics. 2013;36(6):801–17. doi: 10.3928/01477447-20130523-28. [DOI] [PubMed] [Google Scholar]
- 22.Lin HY, Wong PK, Ho WP, et al. Clavicular hook plate may induce subacromial shoulder impingement and rotator cuff lesion – dynamic sonographic evaluation. J Orthop Surg Res. 2014;9:6. doi: 10.1186/1749-799X-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Good DW, Lui DF, Leonard M, et al. Clavicle hook plate fixation for displaced lateral-third clavicle fractures (Neer type II): A functional outcome study. J Shoulder Elbow Surg. 2012;21(8):1045–48. doi: 10.1016/j.jse.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 24.Meda PV, Machani B, Sinopidis C, et al. Clavicular hook plate for lateral end fractures: A prospective study. Injury. 2006;37(3):277–83. doi: 10.1016/j.injury.2005.10.017. [DOI] [PubMed] [Google Scholar]
- 25.Brouwer KM, Wright TC, Ring DC. Failure of superior locking clavicle plate by axial pull-out of the lateral screws: a report of four cases. J Shoulder Elbow Surg. 2009;18(1):e22–25. doi: 10.1016/j.jse.2008.05.042. [DOI] [PubMed] [Google Scholar]
- 26.Shin SJ, Roh KJ, Kim JO, Sohn HS. Treatment of unstable distal clavicle fractures using two suture anchors and suture tension bands. Injury. 2009;40(12):1308–12. doi: 10.1016/j.injury.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 27.Herrmann S, Schmidmaier G, Greiner S. Stabilisation of vertical unstable distal clavicular fractures (Neer 2b) using locking T-plates and suture anchors. Injury. 2009;40(3):236–39. doi: 10.1016/j.injury.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 28.Johnston PS, Sears BW, Lazarus MR, Frieman BG. Fixation of unstable type II clavicle fractures with distal clavicle plate and suture button. J Orthop Trauma. 2014;28(11):e269–72. doi: 10.1097/BOT.0000000000000081. [DOI] [PubMed] [Google Scholar]
- 29.Choi S, Kim SR, Kang H, et al. Modified tension band fixation and coracoclavicular stabilisation for unstable distal clavicle fracture. Injury. 2015;46(2):259–64. doi: 10.1016/j.injury.2014.09.025. [DOI] [PubMed] [Google Scholar]
- 30.Souza Vilela JC, de Andrade RP, Jacques Goncalves LB, et al. Fractures of the distal clavicle: Comparison between two surgical treatment methods. Rev Bras Ortop. 2015;50(2):136–41. doi: 10.1016/j.rboe.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]



