Abstract
Objective
Psychopathology is posited to be transdiagnostically linked to chronic stress. Yet efforts to understand the specificity and directionality of these links have been sparse, and the ubiquitous comorbidity of psychopathology has made the seemingly non-specific links between psychological disorders and chronic stress difficult to interpret. The current study used a latent dimensional bifactor model of psychopathology to account for comorbidity and a multi-wave prospective design to disentangle temporal associations between psychopathology and chronic stress longitudinally during the critical adolescent period for psychopathology risk and stress reactivity.
Method
A community sample of 567 youth (55.5% female, age M=11.8 at baseline, M=15.1 at end of study) were followed prospectively for three years, with chronic stress assessed with the Youth Life Stress Interview and psychopathology symptoms assessed via both self and parent report.
Results
Exposure to chronic stress predicted what is common across forms of psychopathology (the p factor), which in turn predicted generation of chronic stress over time. After accounting for comorbidity via the p factor, externalizing behaviors also had specific transactional links to chronic stress, whereas links between internalizing psychopathology and chronic stress were completely accounted for by common psychopathology.
Conclusions
The results provide the first direct evidence that chronic stress is transdiagnostically and reciprocally linked to psychopathology, during a critical youth period for psychopathology onset and stress reactivity.
Keywords: chronic stress, p factor, internalizing, externalizing, latent variable
Chronic stress, defined as challenging or threatening conditions, is associated with depression (e.g., Hankin et al., 2015; Rudolph et al., 2000; Vrshek-Schallhorn et al., 2015), anxiety (Allen, Rapee, & Sandberg, 2008; Grover, Ginsburg, & Ialongo, 2005), and broad internalizing (Zandstra et al., 2015) and externalizing problems (Conway, Hammen, & Brennan, 2015; Rudolph et al., 2000; Zandstra et al., 2015). Moreover, youth with depression and anxiety engage in behaviors and select environments that lead to chronic stress (Hammen, Hazel, Brennan, & Najman, 2012; Uliaszek et al., 2012). These associations suggest that chronic stress may confer risk for, and be generated by, broad, common psychopathology rather than individual disorders. Unfortunately, evidence testing this hypothesis is limited because the majority of studies investigate stress with particular disorders (e.g., depression) but do not attend to known comorbidity among disorders. Thus, it is unknown whether chronic stress is a risk factor for, and/or is generated by common psychopathology or what is specific to internalizing and/or externalizing problems. Research is lacking that examines chronic stress in relation to latent dimensional models of psychopathology that properly account for co-occurrence of emotional and behavioral problems in youth.
A powerful approach to address these issues is through bifactor models that account for this co-occurrence by including a common psychopathology factor (i.e., the p factor; Caspi et al., 2014) as well as specific internalizing and externalizing factors. This structure has replicated in multiple youth samples (e.g., Castellanos-Ryan et al., 2016; Martel et al., 2017; Neumann et al., 2016; Snyder, Young, & Hankin, 2017; Tackett et al., 2013; Waldman, Poore, van Hulle, Rathouz, & Lahey, 2016). Converging evidence demonstrates the p factor is moderately heritable (Neumann et al., 2016; Waldman et al., 2016), has strong distress-related psychopathology loadings (Waldman et al., 2016) and is associated with negative emotionality (Castellanos-Ryan et al., 2016; Tackett et al., 2013) and poor executive function (Castellanos-Ryan et al., 2016; Huang-Pollock, Shapiro, Galloway-Long, & Weigard, 2016; Martel et al., 2017). Thus, one way to conceptualize the p factor is as shared (partially genetic) liability for psychopathology, characterized by transdiagnostic distress, potentially through the endophenotype of poorly-regulated emotion and cognition (e.g., Beauchaine & Zisner, 2017).
Yet, evidence on the extent to which stress relates to latent psychopathology factors is limited. Only one study has examined links between stress and the p factor, finding that childhood maltreatment predicted higher adult common psychopathology, fully accounting for associations with internalizing and externalizing (Caspi et al., 2014). A few studies tested links between stress and internalizing and/or externalizing factors without modeling a common factor. Only one included chronic stress, finding concurrent correlations with both internalizing and externalizing in adolescents (Conway, Hammen, & Brennan, 2012). Results with other stress types are mixed, finding that childhood maltreatment and major episodic stressors predict both internalizing and externalizing factors (Keyes et al., 2012) or externalizing only (Doyle, Murphy, & Shevlin, 2016; Jackson, Gabrielli, Fleming, Tunno, & Makanui, 2014). In the only study testing stress generation with latent factors, adolescent internalizing and externalizing predicted episodic stress, but in different domains (interpersonal for internalizing and non-interpersonal for externalizing; Conway et al., 2012). Importantly, it cannot be assumed that chronic stress and the other types of stress studied to date have the same relations with psychopathology, as they are conceptually distinct and differ in severity, type, timing and duration (e.g., Hammen, 2015; Hankin et al., 2016).
These extant studies leave unanswered questions about stress exposure and generation processes for latent dimensional models of psychopathology. First, links with stress could be driven either by the specific internalizing or externalizing factors or un-modeled common psychopathology. Second, previous research focused on individual disorders with failure to account for comorbidity, lack of longitudinal follow-up, and lack of research on chronic stress. Thus, it is unknown whether chronic stress is a risk factor for, and/or is generated by: (1) common psychopathology (p factor), (2) what is specific to internalizing and/or externalizing, or (3) both. The current study addressed these issues by testing prospective associations (over three years) between chronic stress and common psychopathology and internalizing- and externalizing-specific factors. We did so in a community sample of youth, from late childhood thorough adolescence–a critical developmental period of modal psychopathology onset (Merikangas et al., 2010) and heightened stress experience (Grant et al., 2014). We also tested the specificity of links to age, gender, and stress domains.
We hypothesized that chronic stress would be bidirectionally associated with the p factor, (i.e., stress exposure and generation). Given previous mixed findings, exploratory analyses examined whether chronic stress may have additional associations with internalizing- and externalizing-specific factors. We examined whether chronic stress, assessed earlier in time, predicted individual differences in latent psychopathology levels. For the stress generation direction, we tested whether psychopathology factors predicted chronic stress over time, controlling for earlier stress.
Method
Participants
Community youth and a parent were recruited from the third, sixth and ninth grades of public schools in the Denver and central New Jersey metro areas (for additional details see Hankin et al., 2015). Parents reported that both the parent and child were fluent in English, children did not have autism spectrum or psychotic disorders, and had IQ>70. The sample was similar to US ethnic/racial demographics (Table 1). The current analyses used data from the three laboratory visits: baseline (T1), 18-month (T2), and 36-month (T3). A total of 567 youth-parent pairs completed psychopathology measures at T2. Of these, 544 youth completed chronic stress interviews at T1 and thus were included in stress exposure analyses; 489 youth completed chronic stress interviews at T3 and were included in stress generation analyses. On average, participants were 11.79 years old at T1 (SD=2.39, range=7–16), 13.58 at T2 (SD=2.37, range=9–17) and 15.07 at T3 (SD= 2.36, range=10–19). All procedures were approved by the University of Denver and Rutgers University Institutional Review Boards. Parents provided informed consent and youth provided informed assent.
Table 1.
Demographics and Descriptive Statistics
| Demographics | ||||||||
|---|---|---|---|---|---|---|---|---|
| Gender (% female) | 56% | |||||||
| Ethnicity (% Hispanic/Latino) | 12% | |||||||
| Race (%) | 70% white, 12% African American, 9% Asian/Pacific Islander, 9% Other/more than one | |||||||
| Median family income | $86,500 | |||||||
| Free/reduced lunch | 18.3% | |||||||
| Lifetime psychiatric diagnoses/symptoms in clinical range | 24% MDD, 16% anxiety (social, GAD, OCD, panic, PTSD), 5% ADHD, 6% CD | |||||||
|
| ||||||||
| Mean | SD | n | α | |||||
|
| ||||||||
| Questionnaires (T2) | Child | Parent | Child | Parent | Child | Parent | Child | Parent |
|
| ||||||||
| CDI depression | 5.27 | 3.99 | 5.86 | 5.16 | 550 | 566 | .88 | .88 |
| MASC physical symptoms | 6.44 | 4.78 | 5.73 | 4.63 | 560 | 561 | .85 | .84 |
| MASC social anxiety | 7.53 | 9.56 | 5.79 | 5.44 | 560 | 562 | .87 | .88 |
| MASC separation anxiety | 5.23 | 5.97 | 4.40 | 4.81 | 560 | 562 | .76 | .79 |
| CBCL/YSR oppositional-defiant | 2.12 | 1.80 | 1.89 | 2.04 | 559 | 565 | .66 | .78 |
| CBCL/YSR conduct disorder | 2.71 | 1.85 | 2.59 | 2.53 | 559 | 565 | .70 | .78 |
| EATQ aggression1 | 11.24 | 15.14 | 4.08 | 4.89 | 571 | 564 | .78 | .74 |
| SNAP inattention | - | 8.12 | - | 6.65 | - | 558 | - | .94 |
| SNAP hyperactivity | - | 4.28 | - | 4.83 | - | 558 | - | .90 |
|
| ||||||||
| Chronic Stress Interview (T1 & T3) | T1 | T3 | T1 | T3 | T1 | T3 | ||
|
| ||||||||
| Academic | 1.75 | 1.79 | 0.70 | 0.76 | 544 | 486 | ||
| Behavioral | 1.44 | 1.19 | 0.67 | 0.52 | 544 | 486 | ||
| Peer | 1.91 | 1.69 | 0.74 | 0.69 | 544 | 486 | ||
| Romantic | 1.35 | 1.39 | 0.60 | 0.60 | 542 | 477 | ||
| Family | 1.95 | 1.84 | 0.59 | 0.61 | 544 | 486 | ||
| Neighborhood | 1.53 | 1.54 | 0.70 | 0.66 | 544 | 487 | ||
| Violence | 1.45 | 1.22 | 0.77 | 0.53 | 543 | 487 | ||
| Average Stress | 1.63 | 1.53 | 0.41 | 0.39 | 544 | 489 | ||
Note. For interpretability, variables are in their original, raw metric, prior to rescaling for analysis.
CDI = Children’s Depression Inventory; MASC = Manifest Anxiety Scale for Children; CBCL/YSR = Child Behavior Checklist/Youth Self Report; EATQ = Early Adolescent Temperament Questionnaire; SNAP = Swanson, Nolan, and Pelham scale.
Parent questionnaire has one additional item compared to child questionnaire.
Measures
Youth Life Stress Interview Chronic Stress (YLSI, Rudolph & Flynn, 2007)
The YLSI is a reliable, valid, semi-structured contextual stress interview (considered the gold-standard approach, Hammen, 2015) to assess youths’ chronic stress level in multiple domains (academic, behavioral, peer, family, romantic, neighborhood and violence). Youth were interviewed by trained interviewers, who used prompts and follow-up questions to elicit information on chronic stress in each domain over the previous 18 months. Interviewers ascertained from youth the duration and quality of the stressful contextual experiences described. These interview narratives were then presented to a team of ≧3 coders (with other information, especially psychopathology, about the participants masked), who came to a consensus on an overall severity score for each domain, from 1 (little/no stress) to 5 (severe stress), based on manualized objective ratings for each stressor type.
Children’s Depression Inventory (CDI, Kovacs, 1985)
The CDI assesses depressive symptoms in youth, with good reliability and validity (Klein, Dougherty, & Olino, 2005).
Manifest Anxiety Scale for Children (MASC, March, Parker, Sullivan, Stallings, & Conners, 1997)
The MASC assesses anxious symptoms in youth with subscales for: (1) physical symptoms, (2) harm avoidance, (3) social anxiety, and (4) separation anxiety. The current study did not use the harm avoidance subscale, given evidence that it assesses risk-aversion not anxiety (Snyder et al., 2015). The MASC has good reliability and validity (March et al., 1997).
Child Behavior Checklist/Youth Self Report (CBCL/YSR, Achenbach & Rescorla, 2001)
We used the Oppositional Defiant (ODD) and Conduct (CD) DSM-oriented scales, which have good reliability and validity (Achenbach & Rescorla, 2001).
Aggression scale of the Early Adolescent Temperament Questionnaire Revised (EATQ-R, Ellis & Rothbart, 2001)
This scale assesses hostile reactivity and aggressive physical and verbal actions in youth, with good reliability (Ellis & Rothbart, 2001) and validity (Snyder et al., 2015).
MTA Swanson, Nolan, and Pelham scale (MTA SNAP-IV)
Parents completed the NIMH Collaborative Multisite Multimodal Treatment Study of Children with Attention-Deficit/Hyperactivity Disorder (MTA) version (Swanson et al., 2001). It has inattention and hyperactivity subscales with good reliability and validity (Bussing et al., 2008).
Statistical Analysis
Analyses were conducted in Mplus (Muthén & Muthén, 2012) using full information maximum likelihood estimation to handle missing data. False Discovery Rate (FDR) correction was applied across analyses testing each hypothesis.
p factor model
This model is identical (same participants, time-point, measures, and specifications) to the T1 model in a previous article (Snyder et al., 2017). In brief, all measures were loaded onto the p factor (except MASC separation anxiety, which significantly loaded only on internalizing) and their specific factor representing unique variance not accounted for by the p factor associated with internalizing (CDI depression and MASC physical, social and separation anxiety) or externalizing (CBCL/YSR ODD and CD, and EATQ-R aggression; SNAP hyperactivity and inattention loaded significantly only on the p factor; see Snyder et al. (2017) for discussion). The model had good fit (CFI =.97, TLI=.95, RMSEA=.054, SRMR=.044; Hu & Bentler, 1999), and better fit than one or two factor models (Snyder et al., 2017).
Structural equation models
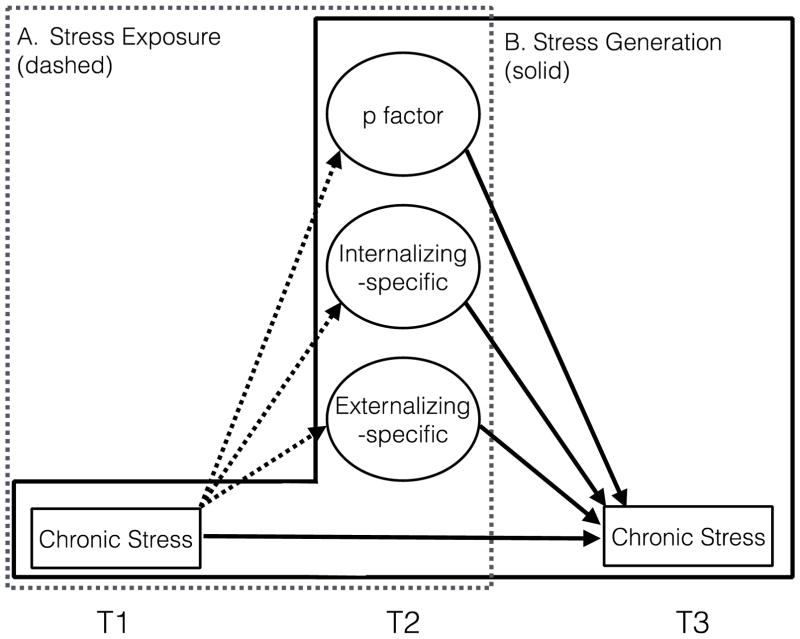
For analyses examining stress exposure, T1 stress predicted T2 psychopathology factors, controlling for age and gender (Figure 1a). We conducted analyses that investigated associations between total stress and each separate stress domain, and then an analysis including all domains to determine specificity of effects. Additional analyses tested for interactions between stress and age and gender in predicting psychopathology factors. For analyses examining stress generation, T2 psychopathology factors predicted T3 stress, controlling for age, gender, and T1 stress (Figure 1b). To determine specificity, these analyses were repeated with residualized stress variables, removing shared variance with other stress domains. Additional analyses tested for latent interactions between psychopathology factors and age and gender. Given non-normality of stress ratings, these models used robust standard error estimation (MLR). For both models, separate analyses were run for each stress domain, and for age and gender interactions.
Figure 1.
Schematic of structural equation models testing (A) associations between chronic stress exposure at T1 and latent psychopathology factors at T2, and (B) associations between latent psychopathology factors at T2 and chronic stress generation at T3, controlling for T1 chronic stress.
Results
See Table 1 for descriptive statistics and Table 2 for manifest correlations. All analyses control for age and gender.
Table 2.
Bivariate Manifest Variable Correlations
| Average Stress | Academic | Behavioral | Peer | Romantic | Family | Neighborhood | Violence | ||
|---|---|---|---|---|---|---|---|---|---|
| CDI depression | Child | .316/.278 | .314/.223 | .201/.086 | .161/.150 | .254/.240 | .149/.214 | .155/.216 | .130/.037 |
| Parent | .333/.373 | .312/.346 | .215/.311 | .254/.236 | .147/.168 | .254/.303 | .077/.140 | .193/.119 | |
| MASC physical symptoms | Child | .171/.174 | .121/.139 | .049/−.002 | .092/.112 | .146/.125 | .129/.164 | .086/.108 | .117/.083 |
| Parent | .192/.182 | .179/.169 | .121/.129 | .124/.060 | .079/.113 | .145/.193 | .057/.116 | .155/.012 | |
| MASC social anxiety | Child | .072/.227 | . −.079/.151 | −.072/.018 | .078/.146 | .125/.153 | .100/.198 | .044/.148 | .027/.107 |
| Parent | .196/.209 | .077/.201 | .054/.152 | .229/.144 | .033/.055 | .171/.196 | .065/.114 | .099/.047 | |
| MASC separation anxiety | Child | −.059/−.009 | −.072/.003 | −.062/−.067 | .060/.064 | −.090/−.117 | .028/.012 | −.166/.024 | −.002/.032 |
| Parent | .108/.033 | .007/.050 | −.007/.076 | .067/.037 | −.125/−.128 | .044/.091 | .005/−.005 | .110/.048 | |
| CBCL/ YSR oppositional-defiant | Child | .342/.327 | .278/.255 | .265/.153 | .125/.144 | .275/.274 | .186/.279 | .133/.137 | .221/.139 |
| Parent | .285/.341 | .221/.293 | .233/.337 | .146/.169 | .106/.135 | .230/.330 | .106/.127 | .177/.116 | |
| CBCL/ YSR conduct disorder | Child | .356/.316 | .319/.266 | .333/.189 | .065/.115 | .350/.314 | .121/.242 | .156/.131 | .184/.145 |
| Parent | .320/.376 | .252/.319 | .247/.372 | .174/.196 | .160/.135 | .281/.354 | .117/.145 | .153/.137 | |
| SNAP inattention | Parent | .265/.300 | .328/.359 | .237/.242 | .210/.170 | .065/.052 | .154/.235 | .045/.122 | .080/.082 |
| SNAP hyperactivity | Parent | .237/.251 | .154/.232 | .239/.267 | .253/.163 | .024/.069 | .181/.223 | .021/.077 | .129/.118 |
| EATQ aggression | Child | .275/.266 | .236/.210 | .237/.134 | .133/.131 | .255/.251 | .083/.222 | .091/.079 | .142/.120 |
| Parent | .234/.292 | .204/.244 | .193/.333 | .169/.131 | .039/.138 | .208/.269 | .049/.052 | .135/.150 | |
| Average Stress | .542 | ||||||||
| Academic | .373 | ||||||||
| Behavioral | .346/.382 | .253 | |||||||
| Peer | .270/.298 | .300/.237 | .371 | ||||||
| Romantic | .263/.252 | .291/.163 | .209/.195 | .399 | |||||
| Family | .223/.423 | .266/.208 | .347/.349 | .154/.311 | .495 | ||||
| Neighborhood | .198/.306 | .206/.101 | .226/.254 | .238/.238 | .248/.331 | .309 | |||
| Violence | .334/.314 | .335/.332 | .287/.282 | .258/.193 | .270/.326 | .234/.202 | .222 | ||
| Age | .270/.198 | .233/.148 | .173/.070 | .000/.023 | .432/.400 | .050/.089 | .132/.103 | .163/.021 |
Note. Correlations before slashes are T1 (r > .084, p < .05; r > .141, p < .001), after slashes are T3 (r > .089, p < .05; r >.149; p < .001). On-diagonal stress correlations are auto-correlations between that measure at T1 and T3.
CDI = Children’s Depression Inventory; MASC = Manifest Anxiety Scale for Children; CBCL/YSR = Child Behavior Checklist/Youth Self Report; EATQ = Early Adolescent Temperament Questionnaire; SNAP = Swanson, Nolan, and Pelham scale.
Stress Exposure (Table 3)
Table 3.
Chronic stress severity at T1 predicting latent psychopathology factors at T2 controlling for age and gender
| Individual Regressions | Multiple Regression (controlling for all other stress domains) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Stress Domain | Psychopathology Factor | β | SE | z | p | Est. Corr. | β | SE | z | p |
| Academic | p factor | .481 | .056 | 8.65 | <.001** | .538 | .366 | .059 | 6.19 | <.001** |
| Internalizing-specific | .095 | .063 | 1.80 | .072 | −.049 | .085 | .057 | 1.50 | .134 | |
| Externalizing-specific | .293 | .086 | 3.42 | .001** | .378 | .197 | .088 | 2.22 | .026* | |
|
| ||||||||||
| Behavioral | p factor | .357 | .066 | 5.38 | <.001** | .401 | .136 | .064 | 2.15 | .032* |
| Internalizing-specific | .055 | .054 | 1.01 | .314 | −.052 | .007 | .058 | 0.12 | .903 | |
| Externalizing-specific | .381 | .070 | 5.43 | <.001** | .446 | .287 | .068 | 3.13 | <.001** | |
|
| ||||||||||
| Family | p factor | .310 | .054 | 5.76 | <.001** | .339 | .148 | .057 | 2.58 | .010* |
| Internalizing-specific | .031 | .050 | 0.72 | .536 | .018 | .041 | .055 | 0.25 | .805 | |
| Externalizing-specific | .252 | .070 | 3.60 | <.001** | .274 | .167 | .069 | 2.40 | .016* | |
|
| ||||||||||
| Romantic | p factor | .213 | .061 | 3.47 | .001** | .398 | .066 | .060 | 1.09 | .275 |
| Internalizing-specific | .040 | .055 | 0.72 | .471 | −.150 | .038 | .058 | 0.66 | .509 | |
| Externalizing-specific | .244 | .069 | 3.52 | <.001** | .385 | .161 | .067 | 2.40 | .016* | |
|
| ||||||||||
| Peer | p factor | .320 | .060 | 5.36 | <.001** | .321 | .166 | .059 | 2.82 | .005** |
| Internalizing-specific | .042 | .050 | 0.84 | .399 | .047 | .026 | .056 | 0.46 | .642 | |
| Externalizing-specific | .079 | .092 | 0.87 | .387 | .080 | −.155 | .072 | −2.16 | .031* | |
|
| ||||||||||
| Neighborhood | p factor | .165 | .056 | 2.96 | .003** | .245 | −.041 | .057 | −0.73 | .465 |
| Internalizing-specific | −.072 | .049 | −1.46 | .144 | −.116 | −.113 | .053 | −2.13 | .033* | |
| Externalizing-specific | .128 | .064 | 1.99 | .046* | .181 | .016 | .061 | 0.26 | .799 | |
|
| ||||||||||
| Violence | p factor | .203 | .057 | 3.57 | <.001** | .284 | −.022 | .057 | −0.73 | .465 |
| Internalizing-specific | .082 | .050 | 1.63 | .103 | .011 | .071 | .056 | 1.27 | .203 | |
| Externalizing-specific | .205 | .065 | 3.16 | .002** | .266 | .039 | .066 | 0.60 | .552 | |
|
| ||||||||||
| Total Stress | p factor | .495 | .053 | 9.42 | <.001** | .569 | ||||
| Internalizing-specific | .076 | .052 | 1.46 | .144 | −.055 | |||||
| Externalizing-specific | .403 | .081 | 4.97 | <.001** | .502 | |||||
Note.
p < .05 uncorrected
p < .05 FDR corrected
There were both domain-general and domain-specific associations between stress exposure at T1 and higher levels of common and externalizing-specific psychopathology at T2, suggesting multiple routs by which chronic stress may maintain or be a risk factor for psychopathology.
Individual stress domain analyses
Higher T1 total stress was associated with higher levels of both the p factor and externalizing-specific factor at T2. Stress in every domain was associated with the p factor. The externalizing-specific factor was predicted by behavioral, academic, family, romantic, and violence stress. No stress domain significantly predicted the internalizing-specific factor.
Multiple stress domains analysis
Academic and peer stress uniquely predicted the p factor, and behavioral stress uniquely predicted the externalizing-specific factor, controlling for all other stress domains. No stress domain predicted the internalizing-specific factor with FDR correction.
Age and gender interactions
Academic (β=.237) and violence (β=.254) stress were more strongly associated with the p factor in older than younger youth. No other age, nor any gender interactions were significant with FDR correction.
Stress Generation (Table 4)
Table 4.
Latent psychopathology factors at T2 predicting chronic stress at T3 controlling for age, gender, and T1 chronic stress
| Raw Stress1 | Residualized Stress | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Stress Domain | Psychopathology Factor | β | SE | z | p | Est. Corr. | β | SE | z | p | Est. Corr. |
| Academic | p factor | .470 | .087 | 5.39 | <.001** | .495 | .243 | .067 | 3.60 | <.001** | .297 |
| Internalizing-specific | .150 | .109 | 1.38 | .168 | .155 | .061 | .091 | 0.68 | .499 | .074 | |
| Externalizing-specific | .280 | .126 | 2.22 | .026* | .294 | .020 | .108 | 0.18 | .856 | .037 | |
|
| |||||||||||
| Behavioral | p factor | .343 | .112 | 3.08 | .002** | .324 | .138 | .111 | 1.24 | .214 | .124 |
| Internalizing-specific | .079 | .106 | 0.75 | .456 | .080 | .024 | .101 | 0.24 | .812 | .021 | |
| Externalizing-specific | .462 | .148 | 3.13 | .002** | .445 | .302 | .110 | 2.75 | .006* | .306 | |
|
| |||||||||||
| Family | p factor | .285 | .064 | 4.47 | <.001** | .360 | .121 | .070 | 1.71 | .087 | .138 |
| Internalizing-specific | .134 | .082 | 1.64 | .101 | .189 | .045 | .077 | 0.59 | .555 | .081 | |
| Externalizing-specific | .387 | .117 | 3.31 | .001** | .464 | .294 | .117 | 2.55 | .012* | .337 | |
|
| |||||||||||
| Romantic | p factor | .171 | .070 | 2.44 | .015** | .230 | .016 | .066 | 0.24 | .811 | .027 |
| Internalizing-specific | .015 | .077 | 0.20 | .842 | .031 | −.053 | .059 | −0.89 | .372 | −.045 | |
| Externalizing-specific | .160 | .129 | 1.25 | .213 | .244 | .022 | .133 | 0.17 | .868 | .088 | |
|
| |||||||||||
| Peer | p factor | .198 | .063 | 3.12 | .002** | .293 | .060 | .057 | 1.05 | .295 | .096 |
| Internalizing-specific | .083 | .083 | 1.00 | .318 | .134 | .026 | .070 | 0.38 | .706 | .055 | |
| Externalizing-specific | .135 | .089 | 1.52 | .129 | .140 | −.029 | .086 | −0.33 | .740 | −.088 | |
|
| |||||||||||
| Neighborhood | p factor | .177 | .070 | 2.51 | .012** | .211 | .021 | .070 | 0.30 | .762 | .008 |
| Internalizing-specific | .176 | .087 | 2.02 | .043* | .181 | .136 | .078 | 1.74 | .082 | .124 | |
| Externalizing-specific | .021 | .096 | 0.22 | .827 | .068 | −.108 | .096 | −1.13 | .258 | −.104 | |
|
| |||||||||||
| Violence | p factor | .121 | .074 | 1.64 | .102 | .213 | −.100 | .072 | −1.38 | .168 | −.105 |
| Internalizing-specific | .015 | .080 | 0.08 | .854 | .038 | −.065 | .079 | −0.83 | .416 | −.054 | |
| Externalizing-specific | .218 | .099 | 2.20 | .028* | .290 | .028 | .103 | 0.27 | .787 | .041 | |
|
| |||||||||||
| Total Stress | p factor | .389 | .093 | 4.20 | <.001** | .493 | |||||
| Internalizing-specific | .166 | .132 | 1.26 | .209 | .202 | ||||||
| Externalizing-specific | .347 | .140 | 2.48 | .013** | .426 | ||||||
Note.
Results remained similar controlling for stress at T2 (contemporaneous with psychopathology assessment), with only the p factor associations with neighborhood and romantic stress becoming non-significant. Controlling for stress at T2, higher levels of the p factor predicted higher levels of T3 total (β=.284**) academic (β=.463**), behavioral (β=.380**), family (β=.197**), and peer (β=.168**) stress. Higher levels of the externalizing-specific factor predicted higher levels of total (β=.260*), behavioral (β=.449**) and family (β=.313**) stress. ** p < .05 FDR corrected, * p < .05 uncorrected
p < .05 uncorrected
p < .05 FDR corrected
Both common and externalizing-specific psychopathology at T1 predicted generation of higher levels of chronic stress at T3 across multiple stress domains, with little evidence of domain-specificity.
Raw stress
Higher levels of the p factor at T2 predicted higher levels of T3 total stress, controlling for T1 stress. The p factor predicted higher levels of academic, behavioral, family, peer, neighborhood, and romantic, but not violence, stress. The externalizing-specific factor predicted higher total, behavioral and family stress, controlling for T1 stress. The internalizing-specific factor did not predict change in any stress domain after FDR correction.
Residualized stress
The p factor predicted higher levels of the unique component of academic stress, controlling for T1 residualized academic stress. No other effect was significant after FDR correction.
Age and gender interactions
No interactions between psychopathology factors and age or gender significantly predicted T3 stress with FDR correction.
Discussion
The current study used an empirically supported, latent dimensional bifactor model of psychopathology to account for comorbidity and enable more precise disentangling of longitudinal associations between chronic stress and psychopathology, during the critical adolescent period for psychopathology risk and stress reactivity. The present findings with a longitudinal design suggest that stress predicts, and is predicted by, what is commonly shared across multiple forms of psychopathology as well as unique externalizing behavior manifestations. These results, based on recent bifactor models of psychopathology, suggest new theoretical and clinical implications for stress and psychopathology associations in youth.
Specifically, this study provides the first direct evidence that chronic stress is transdiagnostically and reciprocally (stress exposure and generation) linked to common psychopathology. Previous research showed that childhood maltreatment is associated with the p factor (Caspi et al., 2014). Our findings extend this work to more typically-experienced chronic stress in multiple domains and directly demonstrate the role of common psychopathology in stress generation for the first time. Externalizing also had unique, bidirectional links with chronic stress independent from common psychopathology, demonstrating that previously reported associations were not simply driven by internalizing comorbidity (Doyle et al., 2016; Jackson et al., 2014; Keyes et al., 2012). Interestingly, there was no association between chronic stress in any domain and the internalizing specific dimension, despite scores of studies showing links between stress, depression, and anxiety (Grant et al., 2014). Importantly, this does not mean that internalizing symptoms are unrelated to chronic stress (see Table 2 showing manifest CDI and MASC correlations with stress), but rather that these associations are likely accounted for by common psychopathology (p factor) rather than relating to specific internalizing variance. Depression and many anxiety disorders (e.g., generalized anxiety) are distress disorders, and distress appears to be mostly captured by the p factor (Waldman et al., 2016).
A secondary aim was to investigate domain specificity versus generality of chronic stress links with latent psychopathology dimensions. Previous research, mainly on episodic but not chronic stress, has found that multiple stressors can lead to the same psychopathology outcomes (equifinality), and individual stressor types to multiple psychopathology outcomes (multifinality; Grant et al., 2014). Here, both the p factor and externalizing-specific factor were broadly bidirectionally related to chronic stress across domains, consistent with equifinality and multifinality. However, there was also some domain specificity: controlling for all other stressors, the p factor was linked to the unique aspects of peer and academic stress. During adolescence, academic pressures increase and peer relationships become paramount, potentially causing stress in these domains to be particularly salient and strongly linked to psychopathology (Hankin et al., 2016). In addition, the externalizing-specific factor was linked to unique aspects of behavioral stress. Externalizing, oppositional, behaviors likely directly contribute to behavioral stress (e.g., conflict with teachers). Future research on specific and general mediating mechanisms may help explain the equifinality/multifinality and domain-specific associations in the current study.
Lastly, we investigated whether stress-psychopathology links differed by age and gender. Psychopathology-chronic stress links were not an epiphenomenon of age or gender effects.1 However, total, academic, and violence stress were more strongly associated with later common psychopathology in older youth. Levels and frequency of chronic stress within particular contextual domains, and the salience and significance of such stress, may change with age, shifting relations with psychopathology. For example, poor grades in high school may have more serious implications (e.g., for college) than elementary school, potentially making academic stress more psychopathogenic for older adolescents. There may also be particular developmental windows of enhanced sensitivity to certain stressors, potentially due to changes in mediating mechanisms (e.g., increased rumination in older youth; Hampel & Petermann, 2005).
It is important to note several limitations which should be addressed by future research. First, the current study provided initial support for bidirectional links between chronic stress and latent psychopathology dimensions, consistent with the transactional stress exposure and generation models supported for episodic stress (Hammen, 2015). In contrast to episodic stressors, which occur at specific times, and disorder diagnoses, which are assigned specific onset and offset dates, disentangling cause and effect is considerably more challenging when investigating chronic stress (which by definition persists) and latent psychopathology dimensions (which exhibit strong homotypic continuity over time; Snyder et al., 2017). We demonstrated that psychopathology factors prospectively predicted higher levels of chronic stress, controlling for prior chronic stress–a strong test of stress generation. With respect to stress exposure, the prospective design enabled temporal ordering of chronic stress predicting later psychopathology. Results showed that chronic stress, assessed earlier, predicted future individual difference levels of latent psychopathology dimensions, although we could not test change due to the strong stability of the latent psychopathology factors in this sample and time frame (Snyder et al., 2017). Still, results show that enduring exposure to chronic stress may contribute to maintenance of psychopathology levels.
Second, future work is needed to better understand the mediating mechanisms that may account for chronic stress-psychopathology links, across levels of analysis (behavioral, neural, neuroendocrine), time scales (minutes, days, months, and years), and the lifespan. The associations in the current study between chronic stress and common psychopathology and externalizing-specific factors suggest that explanations for stress-psychopathology links are needed that apply to these broad transdiagnostic dimensions rather than to specific disorders. Importantly, stress links to latent psychopathology factors do not preclude additional links to individual disorders/symptom dimensions (e.g., Hankin et al., 2016). Finally, the current study involved a community youth sample broadly similar to the US population. Results may differ in other populations, such as high risk or clinically referred samples, other ages (younger children, adults), or those experiencing more extreme chronic stress (e.g., living in high-violence areas).
Clinical Implications
The current findings, and the bifactor psychopathology modeling approach more broadly, have potential implications for diagnosis, classification, assessment, and interventions (Hankin et al., 2016). Disentangling transdiagnostic and specific etiological factors is important for screening and can enable targeted interventions. For example, the finding that chronic stress predicts common psychopathology suggests that individuals experiencing high chronic stress should be screened for multiple forms of psychopathology and not only a singular disorder. Indeed, psychological treatments for a single disorder often lead to symptom improvement in comorbid disorders (e.g., Brown, Antony, & Barlow, 1995). Transdiagnostic interventions that target common processes (e.g., chronic stress) across disorders can provide an evidence-based alternative to disorder-specific interventions. Initial research shows promise for interventions transdiagnostically targeting more general psychopathology and broad-based problems (Farchione et al., 2012). Identifying transdiagnostic processes can help to identify promising foci for treatment, and knowledge emanating from bifactor models can inform such targets. For example, individuals with a broad array of psychopathology symptoms may benefit from interventions aimed at reducing stress exposure and preventing stress generation. The present findings suggest promise in continued future research that seeks to understand transdiagnostic mechanisms that can inform interventions that interrupt vicious transactional feedback loops between chronic stress and psychopathology, especially those common symptoms and features that cut across different disorders.
Acknowledgments
This research was supported by grants from the National Institute of Mental Health (R01MH077195, 1R01MH105501 and 1R21MH102210 to B.L.H.; R01MH077178 to J.F.Y.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Footnotes
Gender did not moderate stress-psychopathology links. Previous evidence, primarily with episodic stressful life events and childhood maltreatment, has found evidence for stronger stress reactivity for girls in predicting internalizing, with more limited evidence for stronger links between stress and externalizing in boys (for review, Grant et al., 2014). However, it may be that this effect is specific to acute stressful events, or to specific disorders (e.g., depression) as it did not extend to chronic stress associations with latent psychopathology factors in the current study.
Contributor Information
Hannah R. Snyder, Brandeis University
Jami F. Young, Rutgers University
Benjamin L. Hankin, University of Illinois Urbana-Champaign
Hannah R. Snyder, Department of Psychology, Brandeis University
Jami F. Young, Graduate School of Applied and Professional Psychology, Rutgers University
Benjamin L. Hankin, Department of Psychology, University of Illinois Urbana-Champaign
References
- Achenbach TM, Rescorla L. Manual for the ASEBA School-Age Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- Allen JL, Rapee RM, Sandberg S. Severe life events and chronic adversities as antecedents to anxiety in children: A matched control study. Journal of Abnormal Child Psychology. 2008;36:1047–1056. doi: 10.1007/s10802-008-9240-x. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Zisner A. Motivation, emotion regulation, and the latent structure of psychopathology: An integrative and convergent historical perspective. International Journal of Psychophysiology. 2017 doi: 10.1016/j.ijpsycho.2016.12.014. Advance online publication. [DOI] [PubMed]
- Brown TA, Antony MM, Barlow DH. Diagnostic comorbidity in panic disorder: Effect on treatment outcome and course of comorbid diagnoses following treatment. Journal of Consulting and Clinical Psychology. 1995;63:408–418. doi: 10.1037/0022-006X.63.3.408. [DOI] [PubMed] [Google Scholar]
- Bussing R, Fernandez M, Harwood M, Hou Garvan CW, Eyberg SM, Swanson JM. Parent and teacher SNAP-IV ratings of attention deficit hyperactivity disorder symptoms: psychometric properties and normative ratings from a school district sample. Assessment. 2008;15:317–328. doi: 10.1177/1073191107313888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, … Moffitt MT. The p Factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science. 2014;2:119–137. doi: 10.1177/2167702613497473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellanos-Ryan N, Brière FN, O’Leary-Barrett M, Banaschewski T, Bokde A, Bromberg U, … Conrad P. The structure of psychopathology in adolescence and its common personality and cognitive correlates. Journal of Abnormal Psychology. 2016;125:1039–1052. doi: 10.1037/abn0000193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway CC, Hammen C, Brennan PA. Expanding stress generation theory: Test of a transdiagnostic model. Journal of Abnormal Psychology. 2012;121:754–766. doi: 10.1037/a0027457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway CC, Hammen C, Brennan PA. Adolescent precursors of adult borderline personality pathology in a high-risk community sample. Journal of Personality Disorders. 2015;29:316–333. doi: 10.1521/pedi_2014_28_158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doyle MM, Murphy J, Shevlin M. Competing factor models of child and adolescent psychopathology. Journal of Abnormal Child Psychology. 2016;44:1559–1571. doi: 10.1007/s10802-016-0129-9. [DOI] [PubMed] [Google Scholar]
- Ellis LK, Rothbart MK. Revision of the early adolescent temperament questionnaire. Poster Presented at the 2001 Biennial Meeting of the Society for Research in Child Development; Minneapolis, MN. 2001. [Google Scholar]
- Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Thompson-Hollands J, Carl JR, … Barlow DH. Unified protocol for transdiagnostic treatment of emotional disorders: A randomized controlled trial. Behavior Therapy. 2012;43:666–678. doi: 10.1016/j.beth.2012.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant KE, McMahon SD, Carter JS, Carleton RA, Adam EK, Chen E. The influence of stressors on the development of psychopathology. In: Lewis M, Rudolph KD, editors. Handbook of Developmental Psychopathology. Boston, MA: Springer US; 2014. pp. 205–223. [DOI] [Google Scholar]
- Grover RL, Ginsburg GS, Ialongo N. Childhood predictors of anxiety symptoms: A longitudinal study. Child Psychiatry and Human Development. 2005;36:133–153. doi: 10.1007/s10578-005-3491-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C. Depression and stressful environments: Identifying gaps in conceptualization and measurement. Anxiety, Stress, and Coping. 2015;29:335–351. doi: 10.1080/10615806.2015.1134788. [DOI] [PubMed] [Google Scholar]
- Hammen C, Hazel NA, Brennan PA, Najman J. Intergenerational transmission and continuity of stress and depression: Depressed women and their offspring in 20 years of follow-up. Psychological Medicine. 2012;42:931–942. doi: 10.1017/S0033291711001978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampel P, Petermann F. Age and gender effects on coping in children and adolescents. Journal of Youth and Adolescence. 2005;34:73–83. doi: 10.1007/s10964-005-3207-9. [DOI] [Google Scholar]
- Hankin BL, Snyder HR, Gulley LD, Schweizer TH, Bijttebier P, Nelis S, … Vasey MW. Understanding comorbidity among internalizing problems: Integrating latent structural models of psychopathology and risk mechanisms. Development and Psychopathology. 2016;28:987–1012. doi: 10.1017/s0954579416000663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Young JF, Abela JRZ, Smolen A, Jenness JL, Gulley LD, … Oppenheimer CW. Depression from childhood into late adolescence: Influence of gender, development, genetic susceptibility, and peer stress. Journal of Abnormal Psychology. 2015;124:803–816. doi: 10.1037/abn0000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Huang-Pollock C, Shapiro Z, Galloway-Long H, Weigard A. Is poor working memory a transdiagnostic risk factor for psychopathology? Journal of Abnormal Child Psychology. 2016 doi: 10.1007/s10802-016-0219-8. Advance online publication. [DOI] [PMC free article] [PubMed]
- Jackson Y, Gabrielli J, Fleming K, Tunno AM, Makanui PK. Untangling the relative contribution of maltreatment severity and frequency to type of behavioral outcome in foster youth. Child Abuse & Neglect. 2014;38:1147–1159. doi: 10.1016/j.chiabu.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Eaton NR, Krueger RF, McLaughlin KA, Wall MM, Grant BF, Hasin DS. Childhood maltreatment and the structure of common psychiatric disorders. British Journal of Psychiatry. 2012;200:107–115. doi: 10.1192/bjp.bp.111.093062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DN, Dougherty LR, Olino TM. Toward guidelines for evidence-based assessment of depression in children and adolescents. Journal of Clinical Child & Adolescent Psychology. 2005;34:412–432. doi: 10.1207/s15374424jccp3403_3. [DOI] [PubMed] [Google Scholar]
- Kovacs M. The Children’s Depression, Inventory (CDI) Psychopharmacology Bulletin. 1985;21:995–998. [PubMed] [Google Scholar]
- March JS, Parker JD, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, and validity. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- Martel MM, Pan PM, Hoffmann MS, Gadelha A, do Rosário MC, Mari JJ, … Salum GA. A general psychopathology factor (p factor) in children: Structural model analysis and external validation through familial risk and child global executive function. Journal of Abnormal Psychology. 2017;126:137–148. doi: 10.1037/abn0000205. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, … Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén & Muthén; 2012. [Google Scholar]
- Neumann A, Pappa I, Lahey BB, Verhulst FC, Medina-Gomez C, Jaddoe VW, … Tiemeier H. Single nucleotide polymorphism heritability of a general psychopathology factor in children. Journal of the American Academy of Child and Adolescent Psychiatry. 2016;55:1038–1045. doi: 10.1016/j.jaac.2016.09.498. [DOI] [PubMed] [Google Scholar]
- Rudolph KD, Flynn M. Childhood adversity and youth depression: Influence of gender and pubertal status. Development and Psychopathology. 2007;19:497–521. doi: 10.1017/S0954579407070241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph KD, Rudolph KD, Hammen C, Hammen C, Burge D, Burge D, … Daley SE. Toward an interpersonal life-stress model of depression: The developmental context of stress generation. Development and Psychopathology. 2000;12:215–234. doi: 10.1017/s0954579400002066. [DOI] [PubMed] [Google Scholar]
- Snyder HR, Gulley LD, Bijttebier P, Hartman CA, Oldehinkel AJ, Mezulis A, … Hankin BL. Adolescent emotionality and effortful control: Core latent constructs and links to psychopathology and functioning. Journal of Personality and Social Psychology. 2015;109:1132–1149. doi: 10.1037/pspp0000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Young JF, Hankin BL. Strong homotypic continuity in common psychopathology-, internalizing-, and externalizing-specific factors over time in adolescents. Clinical Psychological Science. 2017;5:98–110. doi: 10.1177/2167702616651076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson JM, Kraemer HC, Hinshaw SP, Arnold LE, Conners CK, Abikoff HB, … Wu M. Clinical relevance of the primary findings of the MTA: Success rates based on severity of ADHD and ODD symptoms at the end of treatment. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:168–179. doi: 10.1097/00004583-200102000-00011. [DOI] [PubMed] [Google Scholar]
- Tackett JL, Lahey BB, van Hulle C, Waldman I, Krueger RF, Rathouz PJ. Common genetic influences on negative emotionality and a general psychopathology factor in childhood and adolescence. Journal of Abnormal Psychology. 2013;122:1142–1153. doi: 10.1037/a0034151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uliaszek AA, Zinbarg RE, Mineka S, Craske MG, Griffith JW, Sutton JM, … Hammen C. A longitudinal examination of stress generation in depressive and anxiety disorders. Journal of Abnormal Psychology. 2012;121:4–15. doi: 10.1037/a0025835. [DOI] [PubMed] [Google Scholar]
- Vrshek-Schallhorn S, Stroud CB, Mineka S, Hammen C, Zinbarg RE, Wolitzky-Taylor K, Craske MG. Chronic and episodic interpersonal stress as statistically unique predictors of depression in two samples of emerging adults. Journal of Abnormal Psychology. 2015;124:918–932. doi: 10.1037/abn0000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldman ID, Poore HE, van Hulle C, Rathouz PJ, Lahey BB. External validity of a hierarchical dimensional model of child and adolescent psychopathology: Tests using confirmatory factor analyses and multivariate behavior genetic analyses. Journal of Abnormal Psychology. 2016;125:1053–1066. doi: 10.1037/abn0000183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandstra ARE, Hartman CA, Nederhof E, van den Heuvel ER, Dietrich A, Hoekstra PJ, Ormel J. Chronic stress and adolescents’ mental health: Modifying effects of basal cortisol and parental psychiatric history. The TRAILS Study. Journal of Abnormal Child Psychology. 2015;43:1119–1130. doi: 10.1007/s10802-014-9970-x. [DOI] [PMC free article] [PubMed] [Google Scholar]