SUMMARY
Background
To evaluate the efficacy and safety of ramucirumab (IMC-1121B; LY3009806), a fully human monoclonal antibody targeting the vascular endothelial growth factor receptor-2, alone and in combination with dacarbazine in chemotherapy-naïve patients with metastatic melanoma (MM).
Methods
Eligible patients received ramucirumab (10 mg/kg) + dacarbazine (1000 mg/m2) (Arm A) or ramucirumab only (10 mg/kg) (Arm B) every 3 weeks. The primary endpoint was progression-free survival (PFS); secondary endpoints included overall survival (OS), overall response, and safety.
Findings
Of 106 randomized patients, 102 received study treatment (Arm A, N = 52; Arm B, N = 50). Baseline characteristics were similar in both arms. Median PFS was 2·6 months (Arm A) and 1·7 months (Arm B); median 6-month PFS rates were 30·7% and 17·9% and 12-month PFS rates were 23·7% and 15·6%, respectively. In Arm A, 9 (17·3%) patients had partial response (PR) and 19 (36·5%), stable disease (SD); PR and SD in Arm B were 2 (4·0%) and 21 (42·0%), respectively. Median OS was 8·7 months in Arm A and 11·1 months in Arm B. Patients in both arms tolerated the treatment with limited grade 3/4 toxicities.
Interpretation
Ramucirumab alone or in combination with dacarbazine was associated with an acceptable safety profile in patients with MM. Although the study was not powered for comparison between treatment arms, PFS appeared greater with combination therapy. Sustained disease control was observed on both study arm
Funding
Funded by ImClone Systems LLC, a wholly-owned subsidiary of Eli Lilly and Company, Bridgewater, NJ
INTRODUCTION
Metastatic melanoma is an aggressive and frequently fatal cancer. For patients with metastatic disease, overall 5-year survival rates are less than 15%.1 Despite the recent introduction of effective therapies for advanced disease (such as ipilimumab and vemurafenib), the median overall survival (OS) remains between eight and 18 months.2
Angiogenesis and specifically the vascular endothelial growth factors (VEGFs) and their receptors have been shown to promote melanoma growth and metastasis in xenograft models.3 Higher circulating levels of angiogenic factors including VEGF-A (hereafter referred to as VEGF) have been associated with higher tumor burden and diminished prognosis in melanoma.4–8 VEGF may also attenuate antitumor responses by inhibiting the maturation of antigen-presenting cells.9,10 These findings suggest that targeting angiogenesis may be valuable for the treatment of melanoma. In a randomized phase 2 study (BEAM), the anti-VEGF antibody bevacizumab was combined with carboplatin/paclitaxel in previously untreated advanced melanoma and was associated with modest prolongation of progression-free survival (PFS).11
Ramucirumab (IMC-1121B; LY3009806) is a fully human monoclonal antibody of the immunoglobulin G1 subtype targeted against the human vascular endothelial growth factor receptor-2 (VEGFR-2). Ramucirumab binds VEGFR-2 with high specificity and affinity, and inhibits tumor angiogenesis and growth in preclinical models.4,12 In two phase 1 trials, ramucirumab was evaluated at doses and schedules ranging from 2 mg/kg every week to 20 mg/kg every 3 weeks.13,14 Disease control of more than 5 months was observed in 40% of patients with diverse, predominantly treatment-resistant malignancies; dose-limiting toxicities were observed infrequently and included hypertension and deep vein thrombosis.
Dacarbazine is approved in metastatic melanoma but confers limited efficacy and is associated with modest toxicity including myelosuppression.15 Dacarbazine has been associated in vitro with VEGF upregulation in melanoma,16 and it has been postulated that VEGF inhibition might reduce melanoma resistance to this agent.17
This phase 2 study was designed to determine the efficacy, safety, and tolerability of ramucirumab as monotherapy, or in combination with dacarbazine in patients with metastatic melanoma who had not received prior chemotherapy for metastatic disease. This study did not include a dacarbazine monotherapy control arm because of the substantial literature available and the limited risk/benefit profile associated with this agent in advanced melanoma.
PATIENTS AND METHODS
Patients
Eligible patients included those ≥18 years of age with histologically or cytologically confirmed cutaneous metastatic melanoma.18 Other eligibility criteria included adequate hematologic, hepatic, and renal function; an Eastern Cooperative Oncology Group performance status of 0 or 1; and measurable disease as defined by Response Evaluation Criteria in Solid Tumors (RECIST 1·0).19 Patients were excluded for any of the following: prior cytotoxic therapy for metastatic melanoma; mucosal or intra-ocular melanoma; known brain or leptomeningeal metastases; more than one prior line of biologic, immunologic, or vaccine-based therapy for malignant melanoma; and other factors including pregnancy and uncontrolled or poorly controlled hypertension.
The study was conducted according to the ethical principles of the Declaration of Helsinki and Good Clinical Practice. The protocol was approved by the institutional review boards of the participating institutions. All patients provided written informed consent before any trial procedures.
Study Design
This was a phase 2, open-label, randomized (1:1), multicenter study, in which eligible patients with metastatic melanoma received ramucirumab with or without dacarbazine. The primary objective of the study was to determine the PFS of patients with advanced or metastatic melanoma who had not received prior chemotherapy (for metastatic disease) when treated with ramucirumab alone or in combination with dacarbazine.
Patients in both Arm A (combination therapy) and Arm B (monotherapy) received 10 mg/kg ramucirumab administered as an intravenous (I.V.) infusion over 1 hour on day 1 of each 21-day cycle. Patients in Arm A also received dacarbazine 1000 mg/m2 as a 1-hour I.V. infusion following completion of the ramucirumab infusion on day 1 of each cycle. Treatment continued until progressive disease (PD) or unacceptable toxicity occurred, or other withdrawal criteria were met. The dose of ramucirumab or dacarbazine could be modified in the event of specific treatment-related Grade 3 or 4 adverse events (AEs).
Randomization was stratified by serum lactate dehydrogenase (normal versus elevated [≥1·1 × upper limit of normal]) and the extent of disease (skin, subcutaneous tissue, distant lymph nodes, or lung vs. all other visceral sites, including liver, spleen, gastrointestinal tract, adrenal glands, bone, and other).
Statistical Analyses
One hundred and four patients were planned for this study (52 patients per treatment group). This sample size provided 80% power to rule out the possibility of no difference in the PFS time with respect to dacarbazine that was used as a reference regimen. The sample size calculation was based on the following assumptions: a) median PFS of 3 months (target for either investigational arm; based on a PFS of 1·6 months associated with standard-of-care dacarbazine therapy); b) accrual time of 9 months; c) follow-up time of 4 months; d) loss to follow-up of 10%; and e) α level of 5% (There was no evidence to reject the null hypothesis based on the two two-sided-confidence-intervals [CIs]).
The null hypothesis was that the median PFS in either study arm was the same as with dacarbazine (1·6 months), the standard of care at the time of study conduct, versus the alternative hypothesis that the median PFS of either arm was not equal to the reference regimen. The protocol was not sufficiently powered to enable a formal comparison of PFS between study arms. The median PFS results from each arm were calculated together with their 95% CIs. Since both CIs contain the null hypothesis value of 1·6 months, the null hypothesis could not be rejected at the 0·05 level of significance. No adjustment to the level of significance was performed due to this double comparison. Demographics and baseline characteristics, disposition, and efficacy analyses were performed on the modified intent-to-treat (mITT) population. Efficacy and safety analyses were performed using SAS® version 9·1·3 or above (SAS Institute, Cary, NC).
Efficacy Analyses
The primary efficacy endpoint was PFS, defined as the time from the first day of therapy to the first evidence of progression or death from any cause, whichever occurred first. Patients who did not have documented progression, had missed at least two visits, or had no post-baseline assessment were censored on the day of their last tumor assessment. The Kaplan-Meier method was used to analyze PFS and to estimate the median survival time with the corresponding 95% CI. Patients were evaluated for tumor response according to RECIST 1·0 guidelines.19 Secondary efficacy endpoints were overall response rate, median duration of response, disease control rate at 12 weeks, the 12-week response rate, and OS. Time-to-event data were analyzed using the Kaplan-Meier method with 95% CIs. Post-hoc exploratory analyses of an AE of hypertension were evaluated for both PFS and OS. Analyses investigating an association between treatment-emergent hypertension on ramucirumab and greater efficacy are limited both by the lack of an appropriate control (any association may be confounded by independent patient characteristics associated with better prognosis), as well as the small sample size of the study.20
Safety Analyses
AEs were summarized by Medical Dictionary for Regulatory Activities (MedDRA®) System Organ Class and preferred term and classified from verbatim terms, using the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI-CTCAE) v 3·0. The incidence and percentage of patients with at least one occurrence of a preferred term were included, according to the most severe NCI-CTCAE grade (Grades 0–5). AEs were considered associated with the study treatment if their causal relationship with the treatment was described as “possible,” “probable,” or “certain/definite.”
RESULTS
Patient disposition
This study was conducted at 14 study centers in the United States of America from 13 November 2007 to 28 March 2011. One hundred and six patients were enrolled and randomized (Arm A, N = 54; Arm B, N = 52); 102 of these patients received at least one dose of study treatment (Arm A, n = 52; Arm B, n = 50) (table 1). Two patients in each arm did not receive the study treatment. Forty patients in each treatment arm (Arm A, 74·1%; Arm B, 76·9%) had therapy discontinued due to PD. Three patients in Arm A (5·6%) and five patients in Arm B (9·6%) discontinued due to an AE (table 1).
Table 1.
Patient Disposition
| Variable | RAM + DTIC N = 54 n (%) |
RAM N = 52 n (%) |
|
|---|---|---|---|
| Treated patients, mITT population | 52 (96·3) | 50 (96·2) | |
| Safety population | 52 (96·3) | 50 (96·2) | |
| Reasons for discontinuation from study | |||
| Adverse event | 3 (5·6) | 5 (9·6) | |
| Death | 1 (1·9) | 1 (1·9) | |
| PD | 40 (74·1) | 40 (76·9) | |
| Clinical deterioration | 2 (3·7) | 3 (5·8) | |
| Withdrawal of consent | 3 (5·6) | 1 (1·9) | |
| Others | 5 (9·3) | 2 (3·8) | |
Abbreviations: RAM, ramucirumab; DTIC, dacarbazine; mITT, modified intent-to-treat; PD, progressive disease.
Note: two patients in RAM + DTIC and two patients in RAM were randomized but not treated; these patients were not included in mITT and safety populations.
Patient baseline demographic and clinical characteristics
Baseline demographics and clinical characteristics were well balanced between the two treatment arms (table 2). Most patients were Caucasian (Arm A, 96·2%; Arm B, 100%, data not shown) and male (Arm A, 71·2%; Arm B, 76·0%). The majority of the enrolled patients had advanced disease, with more than 80% of patients in each arm with M1c disease stage (Arm A, 86·5%; Arm B, 82·0%).
Table 2.
Patient Baseline Demographics and Clinical Characteristics of mITT Population
| Variable | RAM+DTI C N = 52 n (%) |
RAM N = 50 n (%) |
|
|---|---|---|---|
| Gender | |||
| Male | 37 (71·2) | 38 (76·0) | |
| Female | 15 (28·8) | 12 (24·0) | |
| Age (years) | |||
| 18 to ≤65 | 30 (57·7) | 30 (60·0) | |
| >65 | 22 (42·3) | 20 (40·0) | |
| Median age, (range) | 63·0 (21–87) | 61·5 (36–85) | |
| ECOG PS | |||
| 0 | 37 (71·2) | 33 (66·0) | |
| 1 | 15 (28·8) | 17 (34·0) | |
| LDH status | |||
| Normal | 38 (73·1) | 31 (62·0) | |
| Elevated | 14 (26·9) | 18 (36·0) | |
| Missing | 0 (0·0) | 1 (2·0) | |
| Extent of metastases | |||
| Lung | 6 (11·5) | 8 (16·0) | |
| Skin, subcutaneous tissue, distant lymph nodes | 2 (3·8) | 2 (4·0) | |
| All other visceral sites | 44 (84·6) | 40 (80·0) | |
| Baseline M stage | |||
| M1a | 2 (3·8) | 2 (4·0) | |
| M1b | 5 (9·6) | 7 (14·0) | |
| M1c | 45 (86·5) | 41 (82·0) | |
| Previous treatment | |||
| Carmustine | 1 (1.9) | 1 (2.0) | |
| Interleukin-2 | 4 (7.7) | 1 (2.0) | |
| Ipilimumab | 9 (17.3) | 4 (8.0) | |
| Temozolomide than one previous therapy* | 13 (25.0 | 20 (40.0) | |
| Interleukin-2 + Ipilimumab | 2 (3.8) | 0 (0.0) | |
| Interleukin-2 + Temozolomide | 1 (1.9) | 0 (0.0) | |
| Ipilimumab + Temozolomide | 1 (1.9) | 2 (4.0) | |
| Carmustine + Temozolomide | 0 (0.0) | 1 (2.0) | |
For patients who received more than one previous treatment, the therapies were administered sequentially
Abbreviations: mITT, modified intent-to-treat; RAM, ramucirumab; DTIC, dacarbazine; ECOG, Eastern Cooperative Oncology Group; PS, performance status; LDH, lactate dehydrogenase; M, distant metastasis.
Primary efficacy endpoint
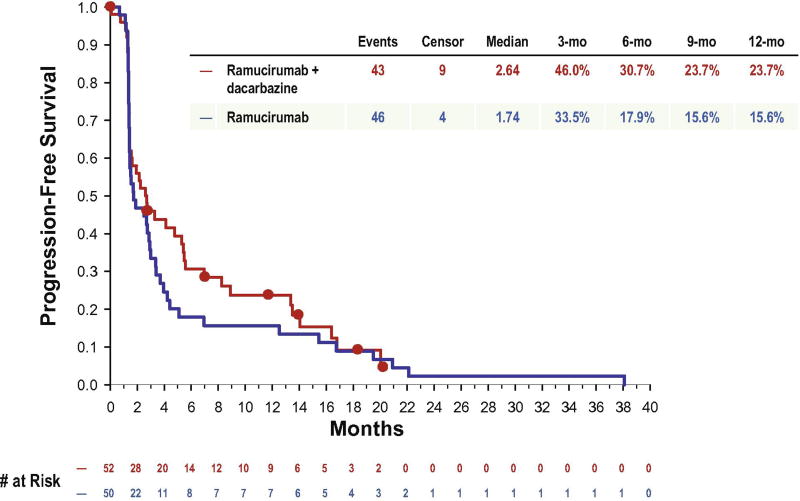
The median PFS was 2·6 months (95% CI: 1·4–5·4) in patients treated with ramucirumab + dacarbazine (Arm A) and 1·7 months (95% CI: 1·4–2·9) in patients treated with ramucirumab alone (Arm B). The 6-month PFS rates were 30.7% (95% CI: 18·4%–43·9%) for Arm A and 17·9% (95% CI: 8·4%–30·2%) for Arm B (figure 1a). The 12-month PFS rates were 23·7% (95% CI: 12·7%–36·6%) for Arm A and 15·6% (95% CI: 6·9%–27·6%) for Arm B.
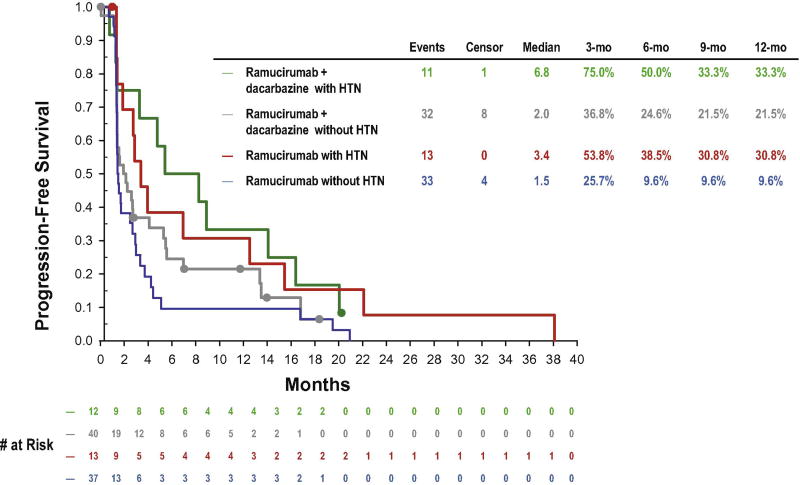
Figure 1.
a. Kaplan-Meier plot for progression-free survival by treatment arm of mITT population.
b. Exploratory analyses of the effect of an adverse event (AE) of hypertension of progression-free survival (PFS), (mITT population). Kaplan-Meier plot for PFS of patients with or without an AE of hypertension (n=12 in Arm A; n=13 in Arm B). In both treatment arms, the median PFS appeared longer in patients with an AE of hypertension (6·8 months [95% CI: 1·3–16·4] for RAM + DTIC; 3·4 months [95% CI: 1·4–12·5] for RAM) than that in patients without an AE of hypertension (2·0 months [95% CI: 1·4–4·1] for RAM + DTIC; 1·5 months [95% CI: 1·4–2·7] for RAM).
Secondary efficacy endpoints
Nine (17·3%) patients in Arm A and 2 (4·0%) patients in Arm B achieved a PR as their best overall response (table 3). The overall response rate was 17·3% (95% CI: 8·2%–30·3%) in Arm A and 4·0% (95% CI: 0·5%–13·7%) in Arm B. The disease control rates, 12-week response rates, and durations of response are summarized in table 3.
Table 3.
Secondary Endpoints in mITT Population
| Variable | RAM+DTI C N = 52 |
RAM N = 50 |
|||
|---|---|---|---|---|---|
|
| |||||
| n | % | n | % | ||
| Best overall response | |||||
| Complete response (CR) | 0 | 0·0 | 0 | 0·0 | |
| Partial response (PR) | 9 | 17·3 | 2 | 4·0 | |
| Stable disease (SD) | 19 | 36·5 | 21 | 42·0 | |
| Progressive disease (PD) | 22 | 42·3 | 24 | 48·0 | |
| Not evaluable (NE) | 2 | 3·8 | 3 | 6·0 | |
| Overall response rate, mopnths, % (95% CI) | |||||
| Response rate, % (CR+PR) | 17·3 (8·2–30·3) | 4·0 (0·5–13·7) | |||
| Disease control rate, % (CR+PR+SD) | 53·8 (39·5–67·8) | 46.0 (31·8–60·9) | |||
| 12-week response rate, months, % (95% CI) | |||||
| Response rate, % (CR+PR) | 13·5 (5·6–25·8) | 4·0 (0·5–13·7) | |||
| Duration of response, months, median, (min-max) | 11·0 (3·5–17·1) | 8·6 (3·2–14·0) | |||
| Overall survival, months, median (95% CI) | 8·7 (7·1–12·9) | 11·1 (7·7–14·6) | |||
Abbreviations: RAM, ramucirumab; DTIC, dacarbazine; mITT, modified intent-to-treat; CI, confidence interval; min-max, minimum-maximum
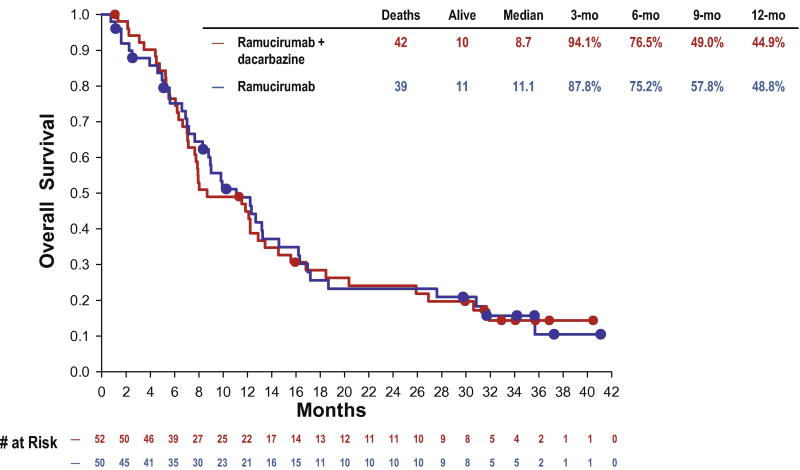
The median OS for patients in Arm A was 8·7 months (95% CI: 7·1–12·9 months) and 11·1 months (95% CI: 7·7–14·6 months) in Arm B (Table 3; figure 2a).
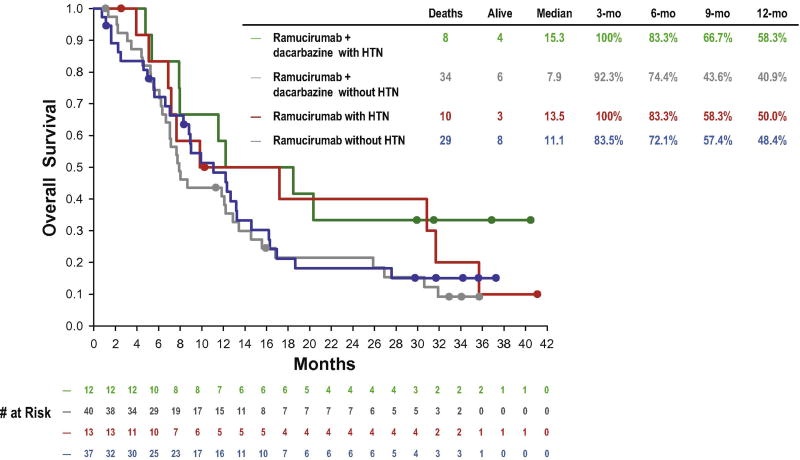
Figure 2.
a. Kaplan-Meier plot for overall survival by treatment arm of mITT population.
b. Exploratory analyses of the effect of an AE of hypertension of overall survival (OS), (mITT population). Kaplan-Meier plot for OS of patients with or without an AE of hypertension (n=12 in Arm A; n=13 in Arm B). In both treatment arms, the median OS appeared longer in patients with an AE of hypertension (15·3 months, [95% CI: 5·4–‘not applicable’] for RAM + DTIC; 13·5 months [95% CI: 5·1–31·7] for RAM) than that in patients without (7·9 months [95% CI 6·3–12·9] for RAM + DTIC; 11·1 months [95% CI 7·0–13·2] for RAM).
Safety
Extent of exposure
The median duration of treatment was 8·9 weeks (range, 3–90 weeks) for Arm A. Patients received a median of three infusions (range, 1–27 infusions). For Arm B, the median duration of ramucirumab treatment was 6 weeks (range, 3–167 weeks). Patients received a median of two infusions (range, 1–54 infusions).
Adverse events and dose modifications
Of the 102 patients comprising the safety population, 101 patients had at least one AE regardless of causality. One patient in Arm B had no AEs. Overall AE rates were similar in both treatment arms (100·0% in Arm A, 98·0% in Arm B). A slightly higher proportion of patients in Arm A experienced AEs ≥Grade 3 (30 patients, 57·7%) compared with Arm B (24 patients, 48·0%). Fatigue was the most common AE in both treatment groups (63·5% in Arm A and 56·0% in Arm B) (table 4). In Arm A, the other most common AEs were thrombocytopenia (38·5%), neutropenia (34·6%), and hypertension (23·1%). In Arm B, the other most common AEs were headache (32·0%), hypertension (26·0%), and back pain (20·0%).
Table 4.
Treatment-emergent Adverse Events Occurring in ≥10% of the Patients in Either Treatment arm in Safety Population*
| Preferred Term | RAM+DTIC N = 52 n (%) |
RAM N = 50** n (%) |
||||
|---|---|---|---|---|---|---|
| Grade | Any | 3 | 4 | Any | 3 | 4 |
|
| ||||||
| Anemia | 7 (13·5) | 2 (3·8) | 0 (0·0) | 2 (4·0) | 1 (2·0) | 0 (0·0) |
| Neutropenia | 18 (34·6) | 11 (21·2) | 4 (7·7) | 0 (0·0) | 0 (0·0) | 0 (0·0) |
| Thrombocytopenia | 20 (38·5) | 6 (11·5) | 2 (3·8) | 4 (8·0) | 0 (0·0) | 1 (2·0) |
| Fatigue | 33 (63·5) | 4 (7·7) | 0 (0·0) | 28 (56·0) | 2 (4·0) | 0 (0·0) |
| IRR† | 4 (7·7) | 0 (0·0) | 0 (0·0) | 7 (14·0) | 2 (4·0) | 1 (2·0) |
| Back pain | 9 (17·3) | 2 (3·8) | 0 (0·0) | 10 (20·0) | 2 (4·0) | 0 (0·0) |
| Headache | 9 (17·3) | 1 (1·.9) | 0 (0·0) | 16 (32·0) | 1 (2·0) | 0 (0·0) |
| Proteinuria | 4 (7·7) | 2 (3·8) | 0 (0·0) | 6 (12·0) | 0 (0·0) | 1 (2·0) |
| Epistaxis | 7 (13·5) | 1 (1·9) | 0 (0·0) | 4 (8·0) | 0 (0·0) | 0 (0·0) |
| Hypertension | 12 (23·1) | 6 (11·5) | 0 (0·0) | 12 (24·0) | 7 (14·0) | 0 (0·0) |
Abbreviations: RAM, ramucirumab; DTIC, dacarbazine; IRR, infusion-related reaction.
The adverse events listed in the table did not occur at a Grade-5 level in either treatment arm.
One patient did not have any AEs.
Incidence of IRRs was reduced following a recommendation for premedication (histamine [H1] antagonists) after 37 patients received initial treatment on study. Prior to the recommendation, IRRs were observed in 6 of 37 patients (16·2%, Arms A + B); subsequent to the recommendation, IRRs were observed in 5 of 65 patients (7·7%, Arms A + B).
Every serious adverse event (SAE) occurred in one patient each. A total of 14 patients (9 [17·3%] in Arm A, 5 [10·0%] in Arm B) experienced SAEs considered possibly, probably, or definitely related to ramucirumab. Ramucirumab-related SAEs occurred in one patient in each arm, with the exception of infusion-related reactions (IRRs) that occurred in three patients, all in Arm B. The ramucirumab-related SAEs were febrile neutropenia, cardiac arrest, supraventricular tachycardia, proctalgia, IRRs, hepatic failure, tumor hemorrhage, cerebral hemorrhage, syncope, acute renal failure, proteinuria, hypertension, pelvic venous thrombosis, flushing, and hypotension. A total of four patients (7·7%) in Arm A experienced SAEs considered potentially related to dacarbazine which included febrile neutropenia, proctalgia, tumor hemorrhage, and acute renal failure.
Two patients in Arm A (3·8%) and one patient in Arm B (2·0%) had dose reductions of ramucirumab. Overall, 17 patients in Arm A and 10 patients in Arm B experienced ramucirumab dose delays. Eight patients in Arm A and six patients in Arm B had ramucirumab dose delays due to toxicity. In Arm A, 34 (65·4%) patients had no dacarbazine dose reductions. Only one patient had more than two dose reductions. Twenty-three patients had dacarbazine dosing delays, 19 of which were due to toxicity.
One death in Arm A and three deaths in Arm B occurred while on treatment or within 30 days of treatment discontinuation. Two deaths, one in each treatment group, were considered related to ramucirumab. The deaths were due to cardiac arrest (Arm A) and liver failure (Arm B). The other two patients in Arm B died due to PD and hepatic failure considered unrelated to ramucirumab treatment.
Infusion-related reactions (IRRs)
Of the 102 patients who received at least one dose of ramucirumab, 11 patients (10·8%) (four in Arm A and seven in Arm B) experienced symptoms consistent with IRRs, including three patients (2·9%) who had severe (Grade 3–4) reactions. Symptoms of suspected IRRs included back pain, chills/rigors, flushing, pruritus, dyspnoea (Grade 3–4 events), and additional cardiorespiratory symptoms including hypoxia, bronchospasm, tachycardia, and hypotension. In the patients who had Grade 1–2 IRRs, pulmonary signs or symptoms were present in one patient. Symptoms in both Grade 1–2 and Grade 3–4 events resolved following medical interventions. The incidence of IRRs was reduced following a recommendation for premedication (histamine [H1] antagonists) after 37 patients received initial treatment on study (prior to the recommendation, IRRs were observed in six of 37 patients [16·2%]; subsequent to the recommendation, IRRs were observed in five of 65 patients [7·7%]) (table 4).
Exploratory analyses of the association of an AE of hypertension on PFS and OS
An AE of hypertension was reported for 12 (23·1%) patients in Arm A and 13 (26·0%) patients in Arm B. The median PFS for patients with hypertension appeared longer than in patients without hypertension (Arm A: 6·8 months [95% CI: 1·3–16·4] versus 2 months [95% CI: 1·4–4·1]; Arm B: 3·4 months [95% CI: 1·4–12·5] vs. 1·5 months [95% CI: 1·4–2·7]) (figure 1b).
In both treatment groups, the median OS appeared slightly longer in patients with an AE of hypertension than in patients without hypertension (Arm A: 15.3 months [95% CI: 5·4–‘not applicable’] versus 7·9 months [95% CI: 6·3–12·9]; Arm B: 13·5 months [95% CI: 5·1–31·7] versus 11·1 months [95% CI: 7·0–13·2]) (figure 2b).
DISCUSSION
In this phase 2 study of patients with metastatic melanoma, ramucirumab in combination with dacarbazine (Arm A) was associated with a median PFS of 2·6 months, and ramucirumab monotherapy (Arm B) with a median PFS of 1·7 months. Although the primary objective of a median PFS of 3 months was not met, the median PFS (2·6 months) observed in the combination arm exceeded that often associated with dacarbazine in metastatic melanoma (1·5–1·6 months).15,21–22 The 6-month PFS rates in Arm A (30·7%) and B (17·9%) and 12-month PFS rates in Arms A (23·7%) and B (15·6%) exceeded those reported in studies evaluating many cytotoxic and other therapies in metastatic melanoma.23,24 The median OS in this study was 8·7 months for Arm A and 11·1 months for Arm B, exceeding the reported median OS in most published dacarbazine studies (6·4–7·9 months), although the availability of efficacious subsequent therapies may have contributed to this result.15,22
Both PFS and OS appeared longer in the subset of patients who developed an AE of hypertension while receiving ramucirumab. The 6- and 12-month PFS rates and the improved outcomes observed in patients who developed hypertension suggest that ramucirumab may confer anticancer activity in metastatic melanoma. However, these data are to be interpreted with caution, as the analyses investigating an association between treatment-emergent hypertension on ramucirumab and greater efficacy were exploratory, and their interpretation is limited both by the lack of an appropriate control. This could mean that any association within these exploratory analyses is confounded by independent patient characteristics associated with better prognosis, as well as the small sample size of the study.20
Although the transcriptional activation of VEGF occurring with chemotherapy may result in chemotherapy resistance in melanoma17, the efficacy of combination chemotherapy with anti-antigenic agents in this disease has been limited. Similar to our findings, the PFS enhancement associated with bevacizumab (when added to carboplatin/paclitaxel) was modest.11 It is likely that the addition of antiangiogenic therapy to cytotoxic regimens in metastatic melanoma is associated with limited benefit due to the lack of identification of potential predictive biomarkers. In this sample of patients with metastatic melanoma, ramucirumab 10 mg/kg once every 3 weeks as monotherapy or in combination with dacarbazine was generally safe and well tolerated. The AEs reported for Arm A were generally consistent with the known safety profile of dacarbazine,15 and those reported for Arm B were consistent with the known safety profile of ramucirumab.13 IRRs were reported, and recommendations regarding premedication for ramucirumab were implemented during this study. The incidences of IRRs (including those that were severe) appeared lower after the implementation of this recommendation, which included histamine (H1) antagonists, and other agents per investigator discretion.
In conclusion, ramucirumab both in combination with dacarbazine and as monotherapy appeared safe and well tolerated in patients with metastatic melanoma. Modest clinical activity was observed in both treatment groups. Although the study was not powered to enable definitive comparisons between treatment groups, the combination therapy appeared to be associated with longer PFS. The sustained disease control observed in both study arms and the preliminary association between hypertension and efficacy suggest that identification of predictive biomarkers may be feasible and will be important for additional investigations of ramucirumab in metastatic melanoma. VEGFR-2 inhibition has been shown in preclinical melanoma models to increase T-lymphocyte activation and enhance immunotherapy-mediated tumor control; the addition of ramucirumab to efficacious, currently available immunotherapy (including ipilimumab), likely also merits investigation.25
Supplementary Material
Acknowledgments
The authors wish to thank all the patients and the investigators for their participation in this study. This study was sponsored by ImClone Systems LLC, a wholly-owned subsidiary of Eli Lilly and Company, Bridgewater, NJ.
Drs. Carvajal, Wong, Thompson, Gordon, Lewis, Pavlick, Wolchok, and Bedikian served as investigators of this study sponsored by the ImClone Systems, a wholly-owned subsidiary of Eli Lilly and Company, Bridgewater, NJ. Dr. Wolchok also served on the advisory committees of ImClone Systems and Eli Lilly and Company. Drs. Carvajal, Thompson, Gordon, Lewis, and Wolchok received research funding from ImClone Systems. Drs. Rojas and Schwartz are employees of ImClone Systems, a wholly-owned subsidiary of Eli Lilly and Company, Bridgewater, NJ and Dr. Schwartz owns company stocks.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented in part at the American Society of Clinical Oncology, Chicago, IL, USA, June 2010; and the 37th European Society for Medical Oncology, Vienna, Austria, September 2012.
Clinical Trial ID: NCT00533702, ClinicalTrials.gov
Contributions:
Medical writing assistance was provided by Durisala Desaiah, PhD, of Eli Lilly and Company and supported by Eli Lilly and Company, Indianapolis. IN, USA. Editorial assistance was provided by Anastasia Perkowski of ImClone Systems and supported by ImClone Systems, a wholly-owned subsidiary of Eli Lilly and Company.
Conflict of Interest:
Dr. Wong has no conflict to disclose.
References
- 1.American Cancer Society. Cancer Facts & Figures 2012. Atlanta, GA: American Cancer Society; 2012. [accessed August 28, 2013]. http://www.cancer.org/research/cancerfactsfigures/cancerfactsfigures/cancer-factsfigures-2012. [Google Scholar]
- 2.Finn L, Markovic SN, Joseph RW. Therapy for metastatic melanoma: the past, present, and future. BMC Medicine. 2012;10:23–32. doi: 10.1186/1741-7015-10-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rofstad E, Halsor E. Vascular endothelial growth factor, interleukin 8, platelet-derived endothelial cell growth factor, and basic fibroblastic growth factor promote angiogenesis and metastasis in human melanoma xenografts. Cancer Res. 2000;60:4932–8. [PubMed] [Google Scholar]
- 4.Lu D, Shen J, Vil MD, et al. Tailoring in vitro selection for a picomolar affinity human antibody directed against vascular endothelial growth factor receptor 2 for enhanced neutralizing activity. J Biol Chem. 2003;278:43496–507. doi: 10.1074/jbc.M307742200. [DOI] [PubMed] [Google Scholar]
- 5.Redondo P, Sánchez-Carpintero I, Bauzá A, Idoate M, Solano T, Mihm MC., Jr Immunologic escape and angiogenesis in human malignant melanoma. J Am Acad Dermatol. 2003;49:255–63. doi: 10.1067/s0190-9622(03)00921-6. [DOI] [PubMed] [Google Scholar]
- 6.Ascierto PA, Leonardi E, Ottaiano A, Napolitano M, Scala S, Castello G. Prognostic value of serum VEGF in melanoma patients: a pilot study. Anticancer Res. 2004;24:4255–8. [PubMed] [Google Scholar]
- 7.Demirkesen C, Büyükpinarbasili N, Ramazanoğlu R, Oğuz O, Mandel NM, Kaner G. The correlation of angiogenesis with metastasis in primary cutaneous melanoma: a comparative analysis of microvessel density, expression of vascular endothelial growth factor and basic fibroblastic growth factor. Pathology. 2006;38:132–7. doi: 10.1080/00313020600557565. [DOI] [PubMed] [Google Scholar]
- 8.Tas F, Duranyildiz D, Oğuz H, Camlica H, Yasasever V, Topuz E. Circulating serum levels of angiogenic factors and vascular endothelia growth factor receptors 1 and 2 in melanoma patients. Melanoma Res. 2006;16:405–11. doi: 10.1097/01.cmr.0000222598.27438.82. [DOI] [PubMed] [Google Scholar]
- 9.Gabrilovich DI, Chen HL, Girgis KR, et al. Production of vascular endothelial growth factor by human tumors inhibits the function maturation of dendritic cells. Nat Med. 1996;2:1096–103. doi: 10.1038/nm1096-1096. [DOI] [PubMed] [Google Scholar]
- 10.Oyama T, Ran S, Ishida T, et al. Vascular endothelial growth factor affects dendritic cell maturation through the inhibition of nuclear factor kappa B activation in hemopoietic progenitor cells. J Immunol. 1998;160:1224–32. [PubMed] [Google Scholar]
- 11.Kim KB, Sosman JA, Fruehauf JP, et al. BEAM: a randomized phase II study evaluating the activity of bevacizumab in combination with carboplatin plus paclitaxel in patients with previously untreated advanced melanoma. J Clin Oncol. 2012;30:34–41. doi: 10.1200/JCO.2011.34.6270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prewett M, Huber J, Li Y, et al. Antivascular endothelial growth factor receptor (fetal liver kinase 1) monoclonal antibody inhibits tumor angiogenesis and growth of several mouse and human tumors. Cancer Res. 1999;59:5209–18. [PubMed] [Google Scholar]
- 13.Spratlin JL, Cohen RB, Eadens M, et al. Phase I pharmacologic and biologic study of ramucirumab (IMC-1121B), a fully human immunoglobulin G1 monoclonal antibody targeting the vascular endothelial growth factor receptor-2. J Clin Oncol. 2010;28:780–7. doi: 10.1200/JCO.2009.23.7537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chiorean E, Sweeney C, Hurwitz H, et al. Phase I dose-escalation study of the anti-VEGF-2 recombinant human IgG1 monoclonal antibody IMC-1121B, administered every other week or every 3 weeks in patients with advanced cancers. Molecular targets and cancer therapeutics; 19th annual AACR-NCI-EORTC conference; October 22–26, 2007; San Francisco, California, USA. (abstract # B15) [Google Scholar]
- 15.Middleton MR, Grob JJ, Aaronson N, et al. Randomized phase III study of temozolomide versus dacarbazine in the treatment of patients with advanced metastatic malignant melanoma. J Clin Oncol. 2000;18:158–66. doi: 10.1200/JCO.2000.18.1.158. [DOI] [PubMed] [Google Scholar]
- 16.Lev DC, Onn A, Melinkova VO, et al. Exposure of melanoma cells to dacarbazine results in enhanced tumor growth and metastasis in vivo. J Clin Oncol. 2004;22:2092–2100. doi: 10.1200/JCO.2004.11.070. [DOI] [PubMed] [Google Scholar]
- 17.Lev DC, Ruiz M, Mills L, McGary EC, Price JE, Bar-Eli M. Dacarbazine causes transcriptional up-regulation of interleukin 8 and vascular endothelial growth factor in melanoma cells: A possible escape mechanism from chemotherapy. Mol Cancer Ther. 2003;2:753–63. [PubMed] [Google Scholar]
- 18.American Joint Committee on Cancer 2002. [accessed August 28, 2013];AJCC Cancer Staging Manual (6th edition): Melanoma of the Skin. :209–17. http://www.cancerstaging.org/products/csmanual6ed-3.pdf.
- 19.Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Canc Inst. 2000;3:205–16. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 20.Anderson JR, Cain KC, Gelber RD. Analysis of survival by tumor response and other comparisons of time-to-event by outcome variables. J Clin Oncol. 2008;26:3913–15. doi: 10.1200/JCO.2008.16.1000. [DOI] [PubMed] [Google Scholar]
- 21.Eggermont AMM, Kirkwood JM. Re-evaluating the role of dacarbazine in metastatic melanoma: what have we learned in 30 years? Eur J Cancer. 2004;40:1825–36. doi: 10.1016/j.ejca.2004.04.030. [DOI] [PubMed] [Google Scholar]
- 22.Bedikian AY, Millward M, Pehamberger H, et al. Bcl-2 antisense (oblimersen sodium) plus dacarbazine in patients with advanced melanoma: the Oblimersen Melanoma Study Group. J Clin Oncol. 2006;24:4738–45. doi: 10.1200/JCO.2006.06.0483. [DOI] [PubMed] [Google Scholar]
- 23.Avril MF, Aamdal S, Grob JJ, et al. Fotemustine compared with dacarbazine in patients with disseminated malignant melanoma: a phase III study. J Clin Oncol. 2004;22:1118–25. doi: 10.1200/JCO.2004.04.165. [DOI] [PubMed] [Google Scholar]
- 24.Korn EL, Liu PY, Lee SJ, et al. Meta-analysis of phase II cooperative group trials in metastatic stage IV melanoma to determine progression-free and overall survival benchmarks for future phase II trials. J Clin Oncol. 2008;28:527–34. doi: 10.1200/JCO.2007.12.7837. [DOI] [PubMed] [Google Scholar]
- 25.Huang Y, Yuan J, Righi E, et al. Vascular normalizing doses of antiangiogenic treatment reprogram the immunosuppressive tumor microenvironment and enhance immunotherapy. Proc Natl Acad Sci U S A. 2012;109:17561–6. doi: 10.1073/pnas.1215397109. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.