Adolescents have the unhealthiest diets of all age groups [1–4], and most adolescents do not meet the national guidelines for physical activity (PA), spending too much time being sedentary [4]. These behaviours can lead to obesity and increase the risk of a range of non-communicable diseases (NCDs) such as diabetes, cancer, and heart disease in later life [5–7]. There is an additional challenge with adolescents as they are in a developmental stage where a sense of autonomy develops and many adolescents are resistant to interventions that they feel impede their independence [8]. In response to the poor health behaviours of adolescents, as well as the unique challenges associated with changing the behaviours of this group, a range of interventions have been developed and tested. Many of these focussed on giving diet or PA education and are often school-based [9–13]. In the context of the studies included in this review, education components include classroom-based lectures, face-to-face provision of information, or teaching through printed materials or digital media. Other interventions for improving adolescents’ health behaviours are community-based [14–16] and may include parental or family involvement [17, 18]. Recently, however, there has been an explosion in the use of digital interventions to improve health behaviours.
In the last few years, internet usage and smartphone ownership have seen a worldwide increase; approximately 90% of adults in the US and UK use the internet and 91% of millennials in these countries own smartphones [19]. US data from 2015 suggested that 92% of adolescents accessed the internet daily, with 24% saying that they were online almost constantly [20]. In addition, the advent of fitness trackers such as Fitbit® has introduced a new platform for motivating people to be physically active, although evidence for their effectiveness is limited [21]. Digital means of communication are considered to be acceptable to adolescents, and a review of text messaging interventions for preventing obesity in adolescents confirmed this [22]. Given the nearly universal accessibility of digital media in high income countries, as well as the affordability and scalability of interventions using these platforms, it is not surprising that there is now considerable interest in developing digital interventions for behaviour change.
To develop effective interventions that result in sustained change to the health behaviours of adolescents, it is necessary to understand which elements of such interventions are effective. A systematic review of digital interventions for increasing PA in adolescents, published in 2011, found that such interventions could produce small but significant increases in PA, and that they were most effective when combined with other delivery methods such as face-to-face contact [23]. Since then, there has been a rapid change in the way adolescents use digital media, coinciding with an increase in the number of digital interventions that have been developed. For example, social media platforms such as Snapchat[24] and Instagram [25] have been launched since 2010, and are widely used amongst young people. In addition, the popular running app ‘Zombies, Run!’ was launched in 2012 and gained record-breaking popularity [26]. The dynamic nature of the digital world and the ways in which it is used by adolescents mean that up-to-date reviews of evidence are required to understand the factors that influence the effectiveness of digital interventions for improving the diet and PA behaviours of adolescents.
More recently, Lappan et al. reviewed RCTs of interventions that included text messages, websites or smartphone apps that aimed to improve diet, physical activity or BMI in children or adolescents [27]. They found that digital platforms often supported improvements in diet and physical activity, and sometimes in body weight or BMI. The authors also concluded that it was important to use a behaviour change theory to design digital interventions for improving health behaviours. In our review, we contributed to the growing body of knowledge on digital interventions for improving the health behaviours of adolescents. Our search was not limited to RCTs, or to any specific form of digital intervention. We aimed to identify specific intervention components that characterise the more successful interventions.
As well as assessing the effectiveness of these interventions with regard to improving diet and PA, it is imperative to understand the cost-effectiveness of each approach [28]. Evaluation of cost-effectiveness assesses whether an intervention is a good use of resources and, in healthcare, can be calculated as cost per quality-adjusted life year (QALY). We aimed to take a very broad definition and, were they available, would include any data about the cost of a given intervention. Digital platforms are often regarded as representing a cost-effective resource for intervention [29, 30]. Healthcare interventions delivered digitally have been found to be cost-effective [31, 32], but data for cost-effectiveness of behaviour change interventions are lacking [32]. Therefore, this review aimed to collate cost-effectiveness data presented in included publications
Aims
The aim of this review was to synthesise evidence on the effectiveness of digital interventions to improve diet quality and increase PA in adolescents, to identify the most effective intervention components and to assess the cost-effectiveness of these interventions.
The following questions were addressed:
-
1)
How can digital interventions be used to improve quality of diet and increase physical activity in adolescents, and which intervention features characterise successful interventions?
-
2)
How cost-effective are such interventions?
Methods
Study selection
The methods for this systematic review followed best practice guidelines for the conduct of systematic reviews, developed by the Centre for Reviews and Dissemination (CRD) [33]. First, a search was carried out in November 2015 by an information specialist using electronic databases MEDLINE, PsycINFO, CINAHL, PubMed Central, Embase, ERIC, the NHS EED and CENTRAL with no restrictions on date of publication (from earliest available through November 2015). A combination of MeSH and free text terms were selected in order to find publications pertaining to adolescent health behaviours, nutrition, PA, and specifically intervention studies that aimed to improve them. The complete search strategy is in Appendix A.
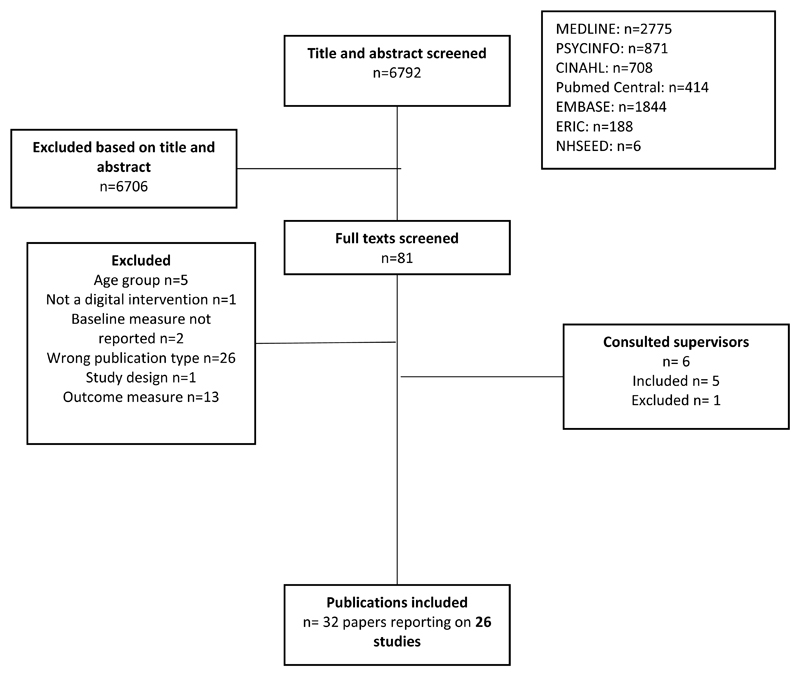
After removing duplicates, this search led to the identification of 6,791 publications, which were independently screened by two researchers (TR and CJ) who compared the titles and abstracts against the inclusion and exclusion criteria listed in Table 1. A total of 31 publications reporting on 26 studies met review inclusion criteria (Figure 1). Reference lists of included studies were screened for additional publications that might address review questions. In addition, experts in the field were consulted to identify further relevant publications, which resulted in one additional publication so the review included a total of 32 publications reporting on 26 studies.
Table 1. Inclusion and exclusion criteria.
| Criteria | Justification | |
|---|---|---|
|
| ||
| Inclusion |
|
|
|
| ||
| Exclusion |
|
|
|
| ||
Figure 1.
Flow diagram of study
Studies were selected if they met inclusion criteria based on study design, target population, intervention type and study outcomes. All included studies described an intervention study using an experimental or quasi-experimental design, with or without a control group. Given the relative paucity of studies, we took a decision to include studies without a control group despite the increased risk of bias, but took account of this bias in the narrative synthesis. Observational studies were not included. Included interventions were aimed at adolescents, using the WHO definition of 10-19 years, and were conducted in any setting. The interventions described were digital, which could include use of websites, mobile phones or smartphones, email, personal digital assistants, social media or any multicomponent intervention that included these. Only studies that reported change from baseline in a dietary and/or PA behaviour were included.
Data extraction and quality assessment
Data were extracted using a form designed to capture the key content of each study. Concurrent with data extraction, a quality assessment was applied to each study. For this, a quality rubric was designed according to the quality assessment criteria described by the CRD [33]. The checklist was tailored to this review and aimed to assess risk of bias resulting from study design, randomisation, blinding, selection, attrition, assessment, intervention fidelity, analysis and handling of confounding. Risk of bias scores ranged from -7 to +5 and level of risk of bias as presented in Table 4 was classified according to these scores. Studies with a score between -2 and +2 were categorised as having a medium risk of bias. Scores below -2 and above +2 were determined to have a low and high risk of bias respectively. The process of data extraction and quality assessment was performed by a single researcher (TR), and a second researcher (CJ) independently reviewed one in three studies (n=9) and there was good agreement between the two researchers. Quality scoring of all studies is presented in Appendix B.
Table 4. Findings from included studies.
| Author, publication year, country, journal | Participants | Main findings | Conclusion | Risk of bias | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample size and follow-up | Engagement with interventions | |||||||||||
| Website interventions | ||||||||||||
| Frenn et al, 2005, United States, Applied Nursing Research[42] | 103
participants 77% follow-up |
No data reported |
Diet Those participating in more than half the sessions decreased dietary fat from 30.7% to 29.9% (p=0.008) Control participants showed no change (31.5% vs 31.6%) The 6 students who received less than half of the dietary sessions were not significantly different from the control participants (0.08) |
This intervention delivered via Blackboard.com showed favourable results with regards to physical activity and dietary fat consumption amongst Midwestern middle school students. | High | |||||||
|
Physical
activity Intervention students who completed more than half of sessions increased MVPA by an average of 22 minutes, compared with a decrease of 46 min in the control group (p=0.05). Those who completed all three sessions increased activity by 33 minutes. | ||||||||||||
|
Williamson et al, 2005, United States, Eating and Weight Disorders
– Studies on Anorexia, Bulimia and Obesity[73] AND
Williamson et al, 2006, United States, Obesity[39] |
Intervention
n=28 Control n=29 70% follow-up |
For all weight loss behaviours,
baseline values were a significant
covariate. Intervention arm had significantly more hits on the website than control. Parent and adolescent use of the website were significantly correlated. Within the intervention group, change in body fat was negatively correlated with email submissions, percent correct answers on quizzes and use of weight graph component. |
Diet At 12 months: The intervention participants showed a significant decrease in energy intake while control participants did not. However, participants in the control group showed a significant decrease in overeating while intervention participants did not. At 24 months: Participants in both groups showed a significant decrease in overeating (p<0.05), although the control group showed a greater improvement. Participants in the behavioural group ate less fattening foods than the control group (p<0.05) at 12 months and 18 months, but not at 24 months. |
Compared to the passive intervention, the behavioural intervention showed a greater improvement in physical activity and diet amongst very overweight and obese African-American girls. However, the changes were not sustained at 24 months. | Medium | |||||||
|
Physical
activity In both groups, adolescents showed significant improvement in physical activity from baseline (p<0.05) with control participants showing a larger improvement at 18 months, but both groups being similar at other time points. | ||||||||||||
|
Jago et al, 2006, United States, Preventive Medicine[45]
Thompson et al, 2009, United States, Preventive Medicine[46] |
Physical activity
n=240 Diet n=233 88% follow-up |
44% of those whose parents had
college education provided data at both time points compared to 27% of
those whose parents did not. Participants for whom complete data were obtained had significantly lower BMI than those who did not (21.0 vs 22.4) 75% of intervention and 78% of control participants logged on at least once a week. |
Diet There was a significant group x time interaction for fruit juice consumption at 1 month post-intervention only. There was also a significant group x time x wave interaction for low-fat vegetable consumption from baseline to 6 months post-intervention. Results presented as M(SE) |
The internet intervention
resulted in a small but significant increase in light physical activity
among the spring participants, but not the autumn participants. The
authors suggest that this could be due to seasonality in
children’s physical activity behaviours, especially in a hot
climate. The group who received the physical activity intervention in the spring wave also showed a significant increase in low-fat vegetable consumption compared to those who received the dietary intervention. |
Medium | |||||||
| Variable | Diet group | Physical Activity group | ||||||||||
| Fruit/juice consumption | ||||||||||||
| Baseline | 2.5 (0.1) | 2.3 (0.1) | ||||||||||
| 1 month* | 3.5 (0.1) | 2.9 (0.1) | ||||||||||
| 6 months | 2.8 (0.1) | 3.0 (0.1) | ||||||||||
| Low-fat vegetable consumption | ||||||||||||
| Baseline | 2.0 (0.1) | 1.6 (0.0) | ||||||||||
| 1 month | 2.5 (0.1) | 1.9 (0.0) | ||||||||||
| 6 months** | 2.1 (0.1) | 2.2 (0.0) | ||||||||||
| *Significant difference in mean
change between groups **Significant difference in mean change between groups amongst the spring wave only | ||||||||||||
|
Physical
activity There was a significant increase in light intensity physical activity from baseline to 1 month post-intervention in the Spring group only. 79% of participants received the Fit for Life badge at the end of the intervention, but there were no group x time effects. Results are presented as mean (SE) physical activity per day | ||||||||||||
| Variable | Spring | Fall | ||||||||||
| PA group | Diet group | PA group | Diet group | |||||||||
| Sedentary minutes | ||||||||||||
| Baseline | 908.4 (6.2) | 906.8 (7.1) | 919.5 (5.4) | 926.8 (5.2) | ||||||||
| 1 month* | 896.3 (6.3) | 901.9 (6.9) | 925.9 (4.9) | 925.1 (4.5) | ||||||||
| 6 months | 912.2 (6.7) | 919.1 (7.8) | 916.7 (5.7) | 930.1 (4.8) | ||||||||
| Light minutes | ||||||||||||
| Baseline | 143.6 (4.9) | 145.0 (5.6) | 136.7 (4.2) | 132.1 (4.1) | ||||||||
| 1 month** | 155.9 (4.9) | 150.3 (5.4) | 129.9 (3.9) | 132.0 (3.5) | ||||||||
| 6 months | 136.2 (5.3) | 135.2 (6.1) | 136.1 (4.5) | 125.7 (3.8) | ||||||||
| MVPA minutes | ||||||||||||
| Baseline | 27.1 (2.2) | 28.1 (2.5) | 23.9 (1.9) | 2.1 (1.8) | ||||||||
| 1 month | 25.3 (2.2) | 27.7 (2.4) | 24.1 (1.7) | 22.8 (1.6) | ||||||||
| 6 months | 29.4 (2.4) | 28.9 (2.7) | 27.2 (1.9) | 24.2 (1.7) | ||||||||
| Counts per minute | ||||||||||||
| Baseline | 445.5 (17.8) | 453.7 (20.2) | 415.2 (15.3) | 390.7 (14.9) | ||||||||
| 1 month | 451.8 (18.0) | 450.9 (19.6) | 398.6 (14.2) | 397.0 (12.8) | ||||||||
| 6 months | 448.5 (19.1) | 425.6 (22.3) | 428.3 (16.2) | 397.7 (13.7) | ||||||||
| *approaching significant (p=0.051)
3-way group x time x wave interaction **significant (p=0.011) group x time x wave interaction for light physical activity | ||||||||||||
| Slootmaker et al, 2010, Netherlands, Preventive Medicine[49] | Intervention
n=31 Control n=46 90% follow-up |
26 of 41 participants filled in
evaluation questionnaire. 17 reported having worn the PAM regularly or
often. 6 participants set a personal goal rather than the standard goal. 10 read the tailored advice, and half of these found it not appealing. |
Physical
activity In intervention boys, there was a significant decrease in sedentary behaviour at 8 months and in intervention girls, there was a significant increase in moderate physical activity at 3 months, but not at 8 months. Physical activity outcomes for boys, presented as median (IQR) |
There was a relative decrease in
sedentary behaviour amongst boys at 8 months in the intervention group
vs the control group. There was a significant increase in moderate physical activity amongst intervention girls at 3 months, but this disappeared at 8 months. Overall, this internet intervention was not very effective at increasing physical activity amongst adolescents |
Medium | |||||||
| Outcome measure (min/week) | Intervention | Control | Difference β (95% CI) | |||||||||
| Sedentary time | ||||||||||||
| Baseline | 4332 (2360; 4950) | 2640 (1450; 4151) | ||||||||||
| 3 months | 2600 (2237; 4363) | 2678 (1904; 3772) | -494 (-1859; 870) | |||||||||
| 8 months | 2915 (1879; 3881) | 3175 (1691; 5494) | -1801 (-3545; -57)* | |||||||||
| Light PA | ||||||||||||
| Baseline | 1375 (925; 2340) | 565 (401; 900) | ||||||||||
| 3 months | 585 (375; 965) | 555 (180; 1130) | -245 (-919; 428) | |||||||||
| 8 months | 968 (646; 1313) | 618 (310; 2069) | -379 (-1184; 424) | |||||||||
| Moderate PA | ||||||||||||
| Baseline | 780 (420; 1495) | 930 (523; 1558) | ||||||||||
| 3 months | 430 (153; 700) | 505 (319; 1301) | -201 (-562; 158) | |||||||||
| 8 months | 530 (133; 840) | 615 (404; 1029) | -149 (-443; 143) | |||||||||
| Vigorous PA | ||||||||||||
| Baseline | 180 (5; 600) | 55 (0; 528) | ||||||||||
| 3 months | 50 (0; 345) | 33 (0; 568) | -54 (-363; 253) | |||||||||
| 8 months | 233 (0; 453) | 63 (0;420) | -16 (-221; 188) | |||||||||
| MVPA | ||||||||||||
| Baseline | 1380 (720; 1650) | 1120 (553; 1993) | ||||||||||
| 3 months | 600 (272; 1060) | 920 (449; 1425) | -123 (-587; 339) | |||||||||
| 8 months | 825 (485; 1065) | 840 (546; 1334) | -156 (-509; 197) | |||||||||
| *p<0.05 Physical activity outcomes for girls, presented as median (IQR) | ||||||||||||
| Outcome measure (min/week) | Intervention | Control | Difference β (95% CI) | |||||||||
| Sedentary time | ||||||||||||
| Baseline | 2692 (1976; 4580) | 3285 (2278; 3960) | ||||||||||
| 3 months | 2640 (1888; 4200) | 3120 (2055; 3851) | 35 (-830; 901) | |||||||||
| 8 months | 2825 (1950; 4917) | 3200 (2460; 3935) | 86 (-674; 846) | |||||||||
| Light PA | ||||||||||||
| Baseline | 985 (598; 1566) | 1470 (718; 2352) | ||||||||||
| 3 months | 810 (300; 1405) | 788 (614; 1265) | 316 (-269; 9020) | |||||||||
| 8 months | 735 (554; 1360) | 960 (540; 1140) | 253 (-362; 869) | |||||||||
| Moderate PA | ||||||||||||
| Baseline | 453 (206; 1238) | 440 (115; 768) | ||||||||||
| 3 months | 510 (110; 1080) | 373 (106; 593) | 411 (1; 824)* | |||||||||
| 8 months | 478 (105; 740) | 435 (135; 680) | -13 (-277; 250) | |||||||||
| Vigorous PA | ||||||||||||
| Baseline | 0 (0; 158) | 0 (0; 188) | ||||||||||
| 3 months | 0 (0, 83) | 45 (0; 300) | -46 (-146; 52) | |||||||||
| 8 months | 0 (0; 191) | 0 (0; 270) | -27 (-143; 89) | |||||||||
| MVPA | ||||||||||||
| Baseline | 740 (281; 1414) | 450 (150; 1003) | ||||||||||
| 3 months | 510 (110; 1303) | 473 (303; 795) | 357 (-86; 801) | |||||||||
| 8 months | 525 (297; 960) | 600 (205; 930) | -46 (-319; 226) | |||||||||
| *p<0.05 | ||||||||||||
|
De Bourdeaudhuij et al, 2010, Cities participating in HELENA
(Vienna, Ghent, Herakion, Dortmund, Athens and Stockholm), Journal
of Adolescent Health[47]
AND Cook et al, 2014, Cities participating in HELENA (see above), Journal of School Health[48] |
Intervention
n=581 Control n=469 Retention varied widely by school. 47% overall |
Moderation analysis showed that responsiveness to the intervention was increased by male sex, older age, higher baseline intention to increase exercise, higher perceived social support or modelling level by siblings, and low perceived social support by friends. |
Physical
activity Baseline to 1 month In the total sample (n=1050), there was a significant condition effect for cycling for transportation, moderate activity in leisure time, vigorous activity in leisure time, and total MVPA |
Computer-tailored physical activity advice resulted in a significant increase in physical activity in the intervention group compared to the control group. These effects were still seen at 3 months post-intervention, and were stronger amongst those who were not doing an hour of physical activity per day at baseline. | Medium | |||||||
| Activity (min/week) |
Control (n=469)
Mean (SD) |
Intervention (n=581)
Mean (SD) |
βCondition (SE) | |||||||||
| Cycling for transportation | -19.13 (7.59)* | |||||||||||
| Baseline | 62(138) | 68 (153) | ||||||||||
| 1 month | 62 (125) | 89 (169) | ||||||||||
| Walking for transportation | -13.91 (10.67) | |||||||||||
| Baseline | 166 (219) | 171 (221) | ||||||||||
| 1 month | 164 (221) | 183 (231) | ||||||||||
| Walking in leisure time | -10.69 (9.43) | |||||||||||
| Baseline | 122 (194) | 138 (207) | ||||||||||
| 1 month | 125 (197) | 149 (221) | ||||||||||
| Moderate activity in leisure time | -32.79 (15.66)* | |||||||||||
| Baseline | 241 (292) | 260 (316) | ||||||||||
| 1 month | 211 (274) | 259 (318) | ||||||||||
| Vigorous activity in leisure time | -27.99 (11.59)* | |||||||||||
| Baseline | 189 (236) | 197 (254) | ||||||||||
| 1 month | 189 (230) | 225 (291) | ||||||||||
| Moderate activity at school | -3.76 (4.53) | |||||||||||
| Baseline | 61 (78) | 60 (79) | ||||||||||
| 1 month | 60 (80) | 63 (81) | ||||||||||
| Vigorous activity at school | -5.25 (4.37) | |||||||||||
| Baseline | 53 (79) | 49 (74) | ||||||||||
| 1 month | 52 (76) | 54 (80) | ||||||||||
| Total MVPA | -44.80 (34.11)* | |||||||||||
| Baseline | 538 (407) | 539 (417) | ||||||||||
| 1 month | 515 (405) | 559 (423) | ||||||||||
| *p<0.05 Baseline to 3 months In the total sample, there was a condition x gender effect for vigorous activity in leisure time β=-55.06 (24.45). There were significant condition effects for cycling for transportation, walking in leisure time, moderate activity in leisure time, vigorous activity in leisure time, and total MVPA. | ||||||||||||
| Activity (min/week) |
Control (n=469)
Mean (SD) |
Intervention (n=581)
Mean (SD) |
βCondition (SE) | |||||||||
| Cycling for transportation | -23.01 (7.97)** | |||||||||||
| Baseline | 62(138) | 68 (153) | ||||||||||
| 3 months | 61 (134) | 89 (176) | ||||||||||
| Walking for transportation | -19.10 (11.03) | |||||||||||
| Baseline | 166 (219) | 171 (221) | ||||||||||
| 3 months | 166 (224) | 186 (231) | ||||||||||
| Walking in leisure time | -19.76 (10.01)* | |||||||||||
| Baseline | 122 (194) | 138 (207) | ||||||||||
| 3 months | 126 (207) | 158 (229) | ||||||||||
| Moderate activity in leisure time | 46.84 (15.45)** | |||||||||||
| Baseline | 241 (292) | 260 (316) | ||||||||||
| 3 months | 222 (286) | 281 (345) | ||||||||||
| Vigorous activity in leisure time | -32.56 (14.18)* | |||||||||||
| Baseline | 189 (236) | 197 (254) | ||||||||||
| 3 months | 196 (244) | 234 (300) | ||||||||||
| Moderate activity at school | -6.01 (5.03) | |||||||||||
| Baseline | 61 (78) | 60 (79) | ||||||||||
| 3 months | 61 (79) | 66 (86) | ||||||||||
| Vigorous activity at school | -7.81 (4.80) | |||||||||||
| Baseline | 53 (79) | 49 (74) | ||||||||||
| 3 months | 52 (79) | 58 (81) | ||||||||||
| Total MVPA | -59.14 (20.20)** | |||||||||||
| Baseline | 538 (407) | 539 (417) | ||||||||||
| 3 months | 520 (406) | 527 (424) | ||||||||||
| *p<0.05 **p<0.01 Among participants who were inactive at baseline, there was a significant condition x gender effect for vigorous activity at school β=-18.76 (9.57). There were significant condition effects for walking for transportation, walking in leisure time, moderate activity in leisure time, vigorous activity in leisure time, moderate activity in school, vigorous activity at school, and total MVPA. Results for those who were inactive at baseline at 3 months | ||||||||||||
| Activity (min/week) |
Control (n=221)
Mean (SD) |
Intervention (n=277)
Mean (SD) |
βCondition (SE) | |||||||||
| Cycling for transportation | -20.19 (13.19) | |||||||||||
| Baseline | 17 (43) | 17 (46) | ||||||||||
| 3 months | 25 (73) | 43 (121) | ||||||||||
| Walking for transportation | -36.34 (15.55)* | |||||||||||
| Baseline | 123 (164) | 119 (168) | ||||||||||
| 3 months | 126 (174) | 156 (205) | ||||||||||
| Walking in leisure time | -29.94 (14.61)* | |||||||||||
| Baseline | 76 (127) | 75 (136) | ||||||||||
| 3 months | 82 (151) | 107 (182) | ||||||||||
| Moderate activity in leisure time | -49.24 (22.18) | |||||||||||
| Baseline | 67 (76) | 67 (81) | ||||||||||
| 3 months | 95 (129) | 123 (217) | ||||||||||
| Vigorous activity in leisure time | -64.09 (23.65)** | |||||||||||
| Baseline | 41 (60) | 44 (67) | ||||||||||
| 3 months | 61 (100) | 109 (207) | ||||||||||
| Moderate activity at school | -11.31 (5.59)* | |||||||||||
| Baseline | 28 (48) | 27 (44) | ||||||||||
| 3 months | 34 (55) | 44 (69) | ||||||||||
| Vigorous activity at school | -15.09 (5.26)** | |||||||||||
| Baseline | 20 (38) | 17 (35) | ||||||||||
| 3 months | 25 (46) | 36 (64) | ||||||||||
| Total MVPA | -83.81 (31.65)** | |||||||||||
| Baseline | 173 (131) | 172 (131) | ||||||||||
| 3 months | 236 (241) | 300 (311) | ||||||||||
| *p<0.05 **p<0.01 | ||||||||||||
| Maes et al, 2011, Cities participating in HELENA (see above), Public Health Nutrition[51] | Intervention
n=713 Control n=585 55% retention overall |
Boys found the advice to be less
believable, relevant, interesting, logical, and useful. Overweight
participants found the advice more interesting and helpful than the
normal weight participants. Overweight participants were more likely to have read the advice and said that they would use it. |
Diet At 1 month, there was a significant decrease in dietary fat in the intervention group of approximately 1% of total energy There were no significant results at 3 month follow-up (not shown) Results at 1 month, presented at Mean(SD) |
This computer-mediated intervention had a moderate effect on fat intake that was not sustained at 3 months. | High | |||||||
| Control | Intervention | F (condition) | ||||||||||
| Fibre (g/4184 kJ) | 0.00 | |||||||||||
| Baseline | 9.47 (3.24) | 9.21 (3.24) | ||||||||||
| 1 month | 9.55 (3.16) | 9.69 (3.59) | ||||||||||
| Vitamin C (mg/4184 kJ) | 1.09 | |||||||||||
| Baseline | 33.05 (17.10) | 33.60 (17.78) | ||||||||||
| 1 month | 33.13 (16.17) | 34.59 (18.12) | ||||||||||
| Ca (mg/4184 kJ) | 2.55 | |||||||||||
| Baseline | 397.91 (177.0) | 349.96 (142.92) | ||||||||||
| 1 month | 363.17 (156.09) | 372.56 (156.78) | ||||||||||
| Fe (mg/4184 kJ) | 2.22 | |||||||||||
| Baseline | 6.02 (1.10) | 6.38 (1.31) | ||||||||||
| 1 month | 5.95 (1.06) | 6.27 (1.32) | ||||||||||
| Fat (% of energy) | 4.82* | |||||||||||
| Baseline | 30.54 (0.07) | 29.50 (0.07) | ||||||||||
| 1 month | 31.01 (0.07) | 29.96 (0.07) | ||||||||||
| Chen et al, 2011, United States, Journal of Adolescent Health[43] | Intervention n=27
pairs Control n=27 pairs 93% follow-up |
63 families enrolled in the
study, but 9 never logged on to the website. The average weekly logon rate was 71.8% for the intervention group and 71.3% in the control group. |
Diet Increase in fruit and vegetable consumption had an effect size of .14 (p=0.001) t-tests also showed that fruit and vegetable intake differed significantly between each time point in the intervention group (p<0.5), but not in the control group. Control |
This website intervention, which included parental involvement, was effective at increasing fruit and vegetable consumption as well as physical activity in Chinese American adolescents, even at 8 month follow up. | Medium | |||||||
| T0 | T1 | T2 | T3 | |||||||||
| Fat % | 28.34 (2.91) | 27.95 (2.88) | 27.72 (3.29) | 27.78 (2.57) | ||||||||
| Fruit and vegetable consumption (servings/day) | 2.28 (.61) | 2.14 (.66) | 2.11 (.55) | 2.34 (.66) | ||||||||
|
Intervention | ||||||||||||
| T0 | T1 | T2 | T3 | |||||||||
| Fat % | 29.34 (2.42) | 28.37 (2.44) | 28.09 (2.27) | 27.99 (2.04) | ||||||||
| Fruit and vegetable consumption (servings/day) | 2.19 (.48) | 2.36 (.64) | 2.41 (.64) | 2.63 (.71) | ||||||||
|
Physical
activity Physical activity increased significantly in the intervention group, but not the control group. P=0.01 | ||||||||||||
| T0 | T1 | T2 | T3 | |||||||||
| Control | 624.89 | 617.1 | 610.75 | 615.67 | ||||||||
| Intervention | 534.84 | 674.72 | 671.54 | 674.37 | ||||||||
| Ezendam et al, 2012, Netherlands, Archives of Paediatrics and Adolescent Medicine[40] | Intervention
n=485 Control n=398 Retained 85% of intervention and 88% of control participants. |
48% of participants completed a
process evaluation questionnaire. 72% of these reported having put the advice into practice. Vocational training versus pre-university students were more likely to appreciate the feedback and to find it more interesting and useful. They were also more likely to have discussed it with their parents than pre-university students. Girls were more likely to have read the advice well and learned new things than boys. Students who were overweight found the information more useful than normal weight students. |
Diet There were some favourable effects for dietary behaviour at 4 months, but these were not sustained at 2 years. Analyses were adjusted for sex, education, ethnicity, and baseline values. Results for all participants at 4 months presented as mean (SD) |
There were some favourable
effects for dietary behaviour at 4-month follow-up, but not 2-year
follow-up. There were more significant improvements amongst the risk
group. Physical activity changes were mixed, as the step count increased, but participation in sport outside school decreased in the intervention group. |
Low | |||||||
| Outcome | Baseline | 4 months | β | OR | ||||||||
| SSB % >400 mL/day | 0.54 (0.34 to 0.88) | |||||||||||
| Intervention | 74.4 | 64.3 | ||||||||||
| Control | 78.1 | 75.8 | ||||||||||
| Snacks per day | -0.81 (-1.33 to -0.29) | |||||||||||
| Intervention | 5.5 (3.8) | 4.9 (3.8) | ||||||||||
| Control | 5.2 (3.3) | 5.5 (4.1) | ||||||||||
| Fruit pieces per day | 0.11 (-0.08 to 0.31) | |||||||||||
| Intervention | 1.67 (1.25) | 1.74 (1.32) | ||||||||||
| Control | 1.63 (1.24) | 1.58 (1.26) | ||||||||||
| Vegetables g/day | 19.34 (7.54 to 31.21) | |||||||||||
| Intervention | 107 (79) | 118 (81) | ||||||||||
| Control | 106 (76) | 99 (72) | ||||||||||
| Whole wheat bread (% sometimes, seldom, never) | 1.08 (0.67 to 1.75) |
|||||||||||
| Intervention | 43.4 | 40.0 | ||||||||||
| Control | 42.8 | 40.9 | ||||||||||
| β-coefficients are presented for
continuous variables and OR is presented for categorical variables. Both
are shown with 95% CI Amongst those not meeting physical activity recommendations at baseline, there were larger effect sizes in some categories at 4 months. These were not sustained at 2 year follow-up. Results for risk group | ||||||||||||
| Outcome | Baseline | 4 months | β | OR | ||||||||
| SSB % >400 mL/day | 0.62 (0.34 to 1.13) | |||||||||||
| Intervention | 100 | 75.5 | ||||||||||
| Control | 100 | 82.4 | ||||||||||
| Snacks per day | -0.97 (-1.70 to -0.24) | |||||||||||
| Intervention | 7.6 (3.4) | 5.7 (3.4) | ||||||||||
| Control | 6.9 (2.8) | 6.2 (3.9) | ||||||||||
| Fruit pieces per day | 0.39 (0.13 to 0.66) | |||||||||||
| Intervention | 0.60 (0.49) | 1.33 (1.27) | ||||||||||
| Control | 0.61 (0.49) | 0.96 (1.05) | ||||||||||
| Vegetables g/day | 16.72 (5.43 to 28.07) | |||||||||||
| Intervention | 86 (59) | 109 (79) | ||||||||||
| Control | 87 (58) | 94 (68) | ||||||||||
| Whole wheat bread (% sometimes, seldom, never) | 1.06 (0.63 to 1.78) |
|||||||||||
| Intervention | 100 | 68.7 | ||||||||||
| Control | 100 | 70.7 | ||||||||||
|
Physical
activity In the total sample, the intervention group showed a significant decrease in steps per week at 4 month follow-up, and there were no other significant physical activity changes. 2 Year results are not shown as there were no significant changes from baseline. Regression analyses are adjusted for sex, education, ethnicity, and baseline values. Results for all students presented as mean (SD) |
||||||||||||
| Outcome | Baseline | 4 months | β | OR | ||||||||
| Days with 60 min of moderate activity | -0.21 (-0.54 to 0.13) | |||||||||||
| Intervention | 2.61 (1.92) | 2.95 (2.02) | ||||||||||
| Control | 2.96 (1.90) | 3.23 (2.10) | ||||||||||
| Transport to school | -10.7 (-28.2 to 6.8) | |||||||||||
| Intervention | 131 (137) | 135 (133) | ||||||||||
| Control | 156 (117) | 160 (114) | ||||||||||
| Sport outside school (%yes) | 0.54 (0.30 to 1.00) | |||||||||||
| Intervention | 81.8 | 80.4 | ||||||||||
| Control | 124 | 90.9 | ||||||||||
| Step count (steps/week) | -10856 (-21556 to -101) | |||||||||||
| Intervention | 81046 (28987) | 79350 (25623) | ||||||||||
| Control | 84679 (21697) | 89934 (29796) | ||||||||||
| Screen time | -5.4 (-25.2 to 14.5) | |||||||||||
| Intervention | 299.7 (163.6) | 287.1 (162.3) | ||||||||||
| Control | 312.9 (163.9) | 295.2 (154.6) | ||||||||||
| Values in bold are statistically
significant β-coefficients are presented for continuous variables and OR is presented for categorical variables. Both are shown with 95% CI In the risk group, there was an inverse effect on sport outside school. The intervention group showed a small decrease and the control group showed an increase. At 2 year follow-up, there was a significant increase in step count from baseline in the intervention group. Results for risk group presented as mean (SD) | ||||||||||||
| Outcome | Baseline | 4 months | β | OR | ||||||||
| Days with 60 min of moderate activity | -0.46 (-0.98 to 0.08) | |||||||||||
| Intervention | 2.00 (1.58) | 2.46 (1.88) | ||||||||||
| Control | 2.35 (1.59) | 2.96 (2.08) | ||||||||||
| Transport to school | -0.9 (-21.5 to 19.8) | |||||||||||
| Intervention | 81 (103) | 2.46 (1.88) | ||||||||||
| Control | 124 (97) | 2.96 (2.08) | ||||||||||
| Sport outside school (%yes) | 0.45 (0.24 to 0.85) | |||||||||||
| Intervention | 63.8 | 66.5 | ||||||||||
| Control | 72.9 | 82.3 | ||||||||||
| Step count (steps/week) | -13636 (-23938 to -3281) | |||||||||||
| Intervention | 73052 (24049) | 71007 (20943) | ||||||||||
| Control | 80465 (22335) | 82672 (27369) | ||||||||||
| Screen time | -4.1 (-25.5 to 17.5) | |||||||||||
| Intervention | 326.8 (154.5) | 296.7 (155.3) | ||||||||||
| Control | 330.0 (156.8) | 299.4 (146.6) | ||||||||||
| β -coefficients are presented for continuous variables and OR is presented for categorical variables. Both are shown with 95% CI | ||||||||||||
| Whittemore et al, 2012, United States, Journal of Adolescent Health[67] | Website + coping skills
n=207 Website n=177 95% follow-up |
Participants completed 83% of
lessons overall. 70% of Health[e]Teen and 53% of Health[e]Teen + CST
completed all sessions. Participants completed self-monitoring assessments an average of 5.26 times. |
Diet There were no significant differences between groups, but there were significant differences over time for both groups. Specifically, there were significant improvements in healthy eating behaviour, fruit/vegetable intake, sugar sweetened beverages, and junk food. |
These results suggest that the HEALTH[e]TEEN internet programme had a significant effect on eating behaviours and physical activity, but the additional CST component did not make a difference. However, there was no control condition so results are not conclusive. | Medium | |||||||
| Group | Baseline | 3 months | 6 months | P value | ||||||||
| Fruit and vegetables (servings per day) | ||||||||||||
| All | 4.5 (2.2) | 4.9(2.2) | 5.0 (2.0) | <0.01 | ||||||||
| Internet + CST | 4.4 (2.3) | 5.0 (2.3) | 4.9 (2.1) | <0.01 | ||||||||
| Internet only | 34.6 (2.0) | 4.9 (2.0) | 5.1 (1.9) | <0.01 | ||||||||
| Breakfast (days per week) | ||||||||||||
| All | 3.6 (2.6) | 4.1 (2.5) | 3.8 (2.6) | 0.18 | ||||||||
| Internet + CST | 3.4 (2.6) | 4.1 (2.6) | 3.7 (2.7) | 0.29 | ||||||||
| Internet only | 3.7 (2.5) | 4.2 (2.4) | 3.9 (2.5) | 0.40 | ||||||||
| Sugar sweetened beverages (servings per day) | ||||||||||||
| All | 6.3 (3.1) | 5.8 (2.8) | 5.6 (2.8) | <0.01 | ||||||||
| Internet + CST | 6.5 (3.3) | 5.9 (2.9) | 5.8 (2.9) | <0.01 | ||||||||
| Internet only | 6.2 (2.8) | 5.6 (2.8) | 5.4 (2.6) | 0.01 | ||||||||
| Fast food (times per week) | ||||||||||||
| All | 0.85 (1.05) | 0.78 (1.01) | 0.82 (1.02) | 0.78 | ||||||||
| Internet + CST | 0.90 (1.12) | 0.83 (1.09) | 0.80 (1.03) | 0.18 | ||||||||
| Internet only | 0.78 (0.96) | 0.72 (0.91) | 0.85 (1.00) | 0.28 | ||||||||
| Junk food (servings per day) | ||||||||||||
| All | 3.0 (2.4) | 2.5 (2.1) | 2.6 (2.2) | <0.01 | ||||||||
| Internet + CST | 3.1 (2.7) | 2.5 (2.2) | 2.7 (2.4) | 0.01 | ||||||||
| Internet only | 2.9 (2.2) | 2.4 (2.0) | 2.5(1.9) | 0.06 | ||||||||
| Eating behaviour score (0-97) | ||||||||||||
| All | 52.9(12.0) | 56.7 (11.5) | 56.8 (11.3) | <0.01 | ||||||||
| Internet + CST | 52.4 (12.3) | 56.8 (11.9) | 56.4 (11.9) | <0.01 | ||||||||
| Internet only | 53.5 (11.6) | 56.6 (11.1) | 57.2 (10.6) | <0.01 | ||||||||
|
Physical
activity Results for exercise at each time point are shown as Mean (SD) and the p value represents the time effect. Group x time effects are all insignificant, and so are not shown here. | ||||||||||||
| Baseline | 3 months | 6 months | P value | |||||||||
| Sedentary behaviours: weekday (hours/day) | ||||||||||||
| All | 5.9 (2.3) | 5.5 (2.2) | 5.2 (2.3) | <0.01 | ||||||||
| Internet + CST | 5.9 (2.2) | 5.4 (2.2) | 5.2 (2.3) | <0.01 | ||||||||
| Internet only | 5.9 (2.5) | 5.6 (2.2) | 5.3 (2.3) | <0.01 | ||||||||
| Sedentary behaviours: weekend (hours/day) | ||||||||||||
| All | 6.2 (2.7) | 5.7 (2.7) | 5.4 (2.7) | <0.01 | ||||||||
| Internet + CST | 6.1 (2.6) | 5.6 (2.7) | 5.3 (2.6) | <0.01 | ||||||||
| Internet only | 6.4 (2.8) | 5.8 (2.7) | 5.4 (2.9) | <0.01 | ||||||||
| Vigorous exercise (days/week of 20 minutes) | ||||||||||||
| All | 3.4 (2.4) | 3.9 (2.2) | 4.1 (2.1) | <0.01 | ||||||||
| Internet + CST | 3.4 (2.4) | 4.1 (2.2) | 4.1 (2.1) | <0.01 | ||||||||
| Internet only | 3.4 (2.3) | 3.7 (2.2) | 4.1 (2.1) | <0.01 | ||||||||
| Moderate exercise (days/week of 30 minutes) | ||||||||||||
| All | 3.8 (2.4) | 4.0 (2.2) | 4.3 (2.1) | <0.01 | ||||||||
| Internet + CST | 3.8 (2.4) | 4.2 (2.2) | 4.1 (2.1) | <0.01 | ||||||||
| Internet only | 3.9 (2.4) | 3.9 (2.1) | 4.3 (2.0) | 0.06 | ||||||||
| Stretching (days/week) | ||||||||||||
| All | 2.4 (2.5) | 2.8 (2.4) | 2.9 (2.5) | <0.01 | ||||||||
| Internet + CST | 2.5 (2.5) | 3.0 (2.5) | 3.0 (2.6) | 0.03 | ||||||||
| Internet only | 2.2 (2.5) | 2.5 (2.3) | 2.8 (2.5) | 0.03 | ||||||||
| Muscle strengthening (days/week) | ||||||||||||
| All | 2.4 (2.5) | 2.8 (2.4) | 2.6 (2.5) | 0.12 | ||||||||
| Internet + CST | 2.6 (2.6) | 2.8 (2.4) | 2.8 (2.5) | 0.18 | ||||||||
| Internet only | 2.2 (2.4) | 2.7 (2.5) | 2.4 (2.5) | 0.40 | ||||||||
| Cullen et al, 2013, United States, Health Education Research[44] | Randomised to conditions in a 4:1
ratio (102 in control and 288 in intervention) 75% follow-up |
Of 366 participants who began the
study, 75% logged on at least once during the study
period. Participants who did not complete the post-intervention questionnaire were more likely to be Black (versus White or Hispanic), obese, live in a single-parent family with three or more children and have lower parent education. 91% of participants set goals, and those in the intervention group were significantly more likely to have set five or more goals during the study period. 33% of the intervention group reported using the diary 3 or more times. 88% visited the ‘did you know’ page at least once and 42% used it six or more times. |
Diet There was a significant increase in the number of participants who ate vegetables 3 or more times per day. Results are presented as percentages of each group who reported engaging in behaviours in the past 7 days |
Compared to the control website,
the intervention website was effective at increasing the number of
adolescents who consumed at least three servings of vegetables per
day. Physical activity significantly improved in both groups, suggesting that the website is effective, even without the self-regulating components. |
Medium | |||||||
|
Control baseline |
Control follow-up |
Intervention baseline |
Intervention follow-up |
|||||||||
| Ate fruit or drank 100% fruit juice 2 or more times per day | 27.13 | 20.62 | 29.95 | 33.30 | ||||||||
| Ate vegetables 3 or more times per day* | 7.33 | 4.85 | 9.22 | 18.22 | ||||||||
| Ate fruits and veg 5 or more times per day | 13.57 | 7.64 | 10.88 | 22.89 | ||||||||
| Drank soda at least one time per day | 60.31 | 64.71 | 57.04 | 60.37 | ||||||||
| Drank 3 or more glasses of milk per day | 1.25 | 0.61 | 1.52 | 0.66 | ||||||||
| *group x time effect P<0.05 | ||||||||||||
|
Physical
activity There was a significant increase in physical activity as well as a significant decrease in television viewing for both groups. Results are presented as percentages of each group who reported engaging in behaviours in the past 7 days | ||||||||||||
|
Control baseline |
Control follow-up |
Intervention baseline |
Intervention follow-up |
|||||||||
| Physically active at least 60 min per day on all 7 days*** | 3.83 | 14.87 | 4.71 | 11.49 | ||||||||
| Physically active at least 60 min per day on 5 or more days | 16.08 | 17.10 | 26.97 | 22.56 | ||||||||
| Attended physical education classes at least one time per week | 87.49 | 70.93 | 89.65 | 89.88 | ||||||||
| Used computers more than 3 hours per day | 12.65 | 8.95 | 16.64 | 16.69 | ||||||||
| Watched television 3 or more hours per day ** | 23.67 | 8.43 | 25.09 | 12.06 | ||||||||
| Played on at least one sport team in the past 12 months | 76.68 | 87.92 | 75.14 | 90.47 | ||||||||
| **p<0.01 regardless of
group *** p<0.001 regardless of group | ||||||||||||
| Patrick et al, 2013, United States, Journal of Diabetes Science and Technology[41] | Website only
n=26 Website + SMS n=24 Website + groups n=26 Usual care n=25 63% follow-up overall |
Logon rates declined in all
groups. Website only group: 16/19 in week one and 4/19 in week
50 Website + SMS: 15/19 in week one and 3/19 in week 50 Website + group: 8/15 in week one and 1/15 in week 50 |
Diet While there were significant treatment effects for diet change strategies, there were no significant results for dietary behaviour. Results are presented as mean (SE) |
The website element of this intervention showed a significant decrease in sedentary behaviour, but none of the iterations of the intervention showed a significant change in moderate and vigorous physical activity or dietary behaviours. | Medium | |||||||
| W | P | WSMS | P | WG | P | UC | ||||||
|
%Calories from fat |
0.219 | 0.979 | 0.719 | |||||||||
| Baseline | 29.1 | 30.3 | 28.2 | 33.4 | ||||||||
| 6 Month | 29.5 | 29.4 | 27.7 | 32.5 | ||||||||
| 12 month | 30.0 | 28.5 | 27.3 | 32.0 | ||||||||
| Fruit/veg servings per 1000 calories | 0.685 | 0.369 | 0.398 | |||||||||
| Baseline | 1.9 (0.01) | 2.0 (0.01) | 2.3 (0.01) | 1.9 (0.01) | ||||||||
| 6 month | 2.1 (0.01) | 2.3 (0.01) | 2.6 (0.01) | 2.0 (0.01) | ||||||||
| 12 month | 2.9 (0.01) | 2.6 (0.01) | 2.9 (0.01) | 2.0 (0.01) | ||||||||
|
Physical
activity Significant treatment effects were found for sedentary behaviour in the website only group. There were no significant changes in moderate and vigorous physical activity. | ||||||||||||
| Website | p | WSMS | p | WG | p | UC | ||||||
| MVPA (min/week) | 0.509 | 0.544 | 0.339 | |||||||||
| Baseline | 320.3 (2.1) | 312.5 (2.5) | 326.1 (2.1) | 378.5 (2.3) | ||||||||
| 6 months | 322.7 (1.3) | 306.9 (1.4) | 332.9 (1.3) | 319.0 (4.0) | ||||||||
| 12 months | 306.0 (2.2) | 301.6 (2.2) | 348.6 (2.8) | 263.6 (0.01) | ||||||||
| Sedentary behavior (h/day) |
0.006 | 0.458 | 0.221 | |||||||||
| Baseline | 4.9 (1.12) | 3.9 (1.13) | 4.6 (1.12) | 5.4 (1.12) | ||||||||
| 6 months | 3.1 (1.11) | 3.8 (1.11) | 4.3 (1.11) | 5.3 (4.0) | ||||||||
| 12 months | 2.8 (1.14) | 3.6 (2.2) | 3.8 (1.16) | 5.3 (1.15) | ||||||||
| Jones et al, 2014, United States, Journal of Medical Internet Research[38] | Healthy Habits
n=225 Weight management n=111 85% follow-up |
Pilot study. No process outcomes are reported. |
Diet There were significant increases in fruit and vegetable consumption at follow up, but sweetened beverage consumption increased in the Healthy Habits group and decreased in the Weight Management group. Results for dietary behaviours are presented as n (%) of participants who met the recommendation over the previous 7 days. P values are for change from baseline. |
Both tracks showed an increase in
fruit consumption and the HH track showed in increase in vegetable
consumption. Physical activity results and soda consumption changes were split between tracks, so few conclusions can be drawn. |
High | |||||||
| Variable | HH track | P value | WM track | P value | ||||||||
| Two or more servings of fruit per day | 61 (31.6) | <0.001 | 26 (28.5) | <0.001 | ||||||||
| Two or more servings of veg per day | 41 (21.2) | <0.001 | 22 (24.1) | 0.752 | ||||||||
| Consumption of soda at least once per day | 34 (17.6) | 0.001 (increase) |
24 (26.4) | 0.002 (decrease) |
||||||||
|
Physical
activity Physical activity results differed between groups. Results for physical activity are presented as n (%) of participants who met the recommendation over the last 7 days. P values are for change from baseline. | ||||||||||||
| Variable | HH track | P value | WM track | P value | ||||||||
| 60 min PA at least 5 of last 7 days | 85 (44.0) | <0.001 (decrease) | 31 (34.1) | <0.001 (increase) | ||||||||
| Watched TV for more than 2 hours per day | 52 (26.9) | <0.001 (increase) | 34 (37.4) | <0.001 (decrease) | ||||||||
| Video games for more than 2 hours per day | 44 (22.8) | <0.001 (decrease) | 26 (28.6) | P<0.001 (increase) | ||||||||
| Lana et al, 2014, Spain and Mexico, Preventive Medicine[35] | Control
n=987 Intervention n=1014 37% follow-up |
Factors that increased the odds of
completing the trial included being Mexican, mothers having a university
degree, and high self-efficacy. Factors associated with dropping out were being 15 or older and having relatives or friends who smoked. |
Diet In all three groups (comparison, internet, and internet + text) the percentage of participants who did not eat the recommended amount of fruit per day decreased significantly (p<0.001). Control decreased by 66.8% Internet group decreased by 62.6% Internet + text group decreased by 71.5% Vegetable and fat intake did not change in any groups. |
Various analyses were preformed to assess change in cancer risk behaviours, and some significant results were found. However, the only dietary/physical activity result was found in consumption of fruit, which changed significantly in the control group as well as the intervention groups. Therefore, the intervention did not appear to have any significant effects on any dietary or physical activity behaviours. | High | |||||||
|
Physical
activity There were no significant effects in any group for sedentary behaviour. | ||||||||||||
| Guthrie et al, 2015, United States, PLOS ONE[50] | Passive control n=59 Active control n=61 Intervention n=62 96% follow-up |
Participants wore accelerometers on 63% of
study days regardless of group. 82% of intervention participants visited
the website at least once. Median incentive earned was $5 (IQR $1.60, $8.30) Boys were significantly more active overall, and showed a significantly higher increase in MVPA over the study period (76% increase vs 39%) |
Over the 6 week period, there was
a significant difference between groups in average MVPA duration
(p<0.0001). Over the course of the study: Passive control group did an average of 10.27 min/day Active control group averaged 9.12 min/day Intervention group averaged 15.26 min/day These results did not significantly differ over time. There was a significant difference between genders (p=0.0384) with girls increasing MVPA by 39% (p=0.0049) and boys showing an increase of 76% (p<0.0001) |
Over a 6-week period, using the pedometer and website that included feedback and a reward system, led to a physical activity level that was approximately 50% higher than those not using the intervention. | Low | |||||||
| Sousa et al, 2015, Portugal, European Journal of Pediatrics[36] | Intervention
n=48 Control n=46 50% follow-up |
In the intervention group, 22/48
participants were excluded because they never accessed the website.
Non-adherence was significantly associated with sedentary behaviour and
poor nutrition at baseline. Only one parent accessed the website. Those who completed the intervention accessed the platform on average 10.68 times and completed 13.66% of activities. |
In the Next.Step group, 48% were
excluded because one was referred for bariatric surgery and 22 never
accessed the website. Some of the results are unclear as data from different questionnaires are presented together and some are not well defined. Results of both ITT and PP analyses are presented. Change from baseline to T2 (24 months) was analysed |
Results show that the Next.Step platform did not result in a significant improvement in diet or physical activity behaviours compared with usual care in a population of obese adolescents in Portugal. | Medium | |||||||
| Lifestyle factor | Change: Mean (SD) | Time effect p | Group effect p | |||||||||
| Physical activity | ||||||||||||
| Next.Step - ITT | 0.14 (0.49) | 0.025 | 0.122 | |||||||||
| Control | 0.12 (0.61) | 0.266 | ||||||||||
| Next.Step - PP | 0.11 (0.54) | 0.144 | 0.307 | |||||||||
| ALP total score | ||||||||||||
| Next.Step – ITT | 0.11 (0.29) | 0.018 | 0.723 | |||||||||
| Control | 0.09 (0.24) | 0.019 | ||||||||||
| Next.Step - PP | 0.12 (0.32) | 0.106 | 0.147 | |||||||||
| Text message interventions | ||||||||||||
| Newton et al, 2009, New Zealand, Diabetes Care[54] | Intervention
n=38 Control n=40 95% follow-up |
37% of participants stopped wearing the pedometers before the end of the study period. |
Physical
activity There were no significant changes in physical activity at 12 week follow-up |
Pedometers and weekly text messaging showed no effects on physical activity of adolescents with type 1 diabetes. | Medium | |||||||
| Outcome | Control | Intervention | p | |||||||||
| Baseline | Mean change |
Baseline | Mean change |
|||||||||
| Daily step count | 10,900 (8324- 13240) |
-840 (-1947-266) |
11242 (8380-13537) |
-22 (-1407-1364) |
0.4 | |||||||
| MVPA (min/week) | 645 (298-895) |
712 (420-1000) |
38.5 (-95-172) |
48.4 (-89-185) |
0.9 | |||||||
| Sirriyeh et al, 2010, United Kingdom, British Journal of Health Psychology[55] | Affective intervention
n=31 Instrumental intervention n=30 Combined n=31 Control n=28 94% follow-up |
None reported |
Physical
activity In the entire sample, there was an average increase of 31.5 minutes of moderate activity per week per person. In the primary analysis, there was a significant condition effect. Specifically, the affective group showed higher levels of PA than the other groups, but the post hoc test was not sufficiently powered to identify significant differences between groups. In the secondary analysis, there was no significant effect for those who were active at baseline (p=0.860), but there was a significant effect for the inactive group (p<0.005). Also, the affective condition produced a significantly greater increase in PA than the other conditions. Results of post hoc analysis for inactive participants |
Daily text messages that targeted affective attitudes toward physical activity resulted in a significant increase in reported physical activity compared to those targeting instrumental beliefs, a combined intervention, and a control. This was only the case for those who were inactive at baseline. | Medium | |||||||
| Condition | Comparison condition | Mean difference (MET) | P value | |||||||||
| Affective | Instrumental | 17186.92 | 0.012 | |||||||||
| Combined | 21313.64 | 0.002 | ||||||||||
| Control | 17150.00 | 0.018 | ||||||||||
| Instrumental | Affective | -17186.93 | 0.012 | |||||||||
| Combined | 4126.71 | 1.00 | ||||||||||
| Control | -36.92 | 1.00 | ||||||||||
| Combined | Affective | -21313.64 | 0.002 | |||||||||
| Instrumental | -4126.71 | 1.00 | ||||||||||
| Control | -4163.64 | 1.00 | ||||||||||
| Control | Affective | -17150.00 | 0.018 | |||||||||
| Instrumental | 36.92 | 1.00 | ||||||||||
| Combined | 4163.64 | 1.00 | ||||||||||
| Bech-Larsen and Gronhoj, 2012, Denmark, International Journal of Consumer Studies[52] | Intervention
n=169 Control n=87 90% follow-up |
Average response rate over the
study period was 82%. This decreased from 91% in week 1 to 71% in week
4. Average goals also decreased significantly from 2.47 servings of
fruit in week one to 2.23 in week four. Vegetable goals decreased slightly from 2.11 servings in week one to 1.95 in week four. However, this decrease was only seen amongst those who were meeting recommendations at baseline. |
Diet Over the course of the four weeks, the added average daily units across the whole sample decreased from 5.48 to 5.28 daily units. This was not a significant result. In the SMS group, average daily intake did not significantly change. There was a significant difference between high and low users in both fruit and vegetable consumption, but not between intervention and control groups. Specifically, low baseline users increased their consumption of fruit and vegetables while high baseline users decreased their consumption. Intervention group |
This SMS intervention did not
have a significant effect, but the intervention as a whole with the
nutrition lessons did show a significant increase in fruit and vegetable
consumption. Furthermore, over time, the participants who were low users at baseline increased their consumption and high users decreased their consumption. The effect of this group allocation was the only significant result. |
High | |||||||
| n |
Baseline mean (SD) |
Follow up mean | Difference | |||||||||
| Total veg | 153 | 4.0 (1.08) | 4.2 (1.00) | +0.2 | ||||||||
| High users | 74 | 4.8 (0.50) | 4.6 (0.79) | -0.2 | ||||||||
| Low users | 79 | 3.1 (0.81) | 3.7 (0.99) | +0.6 | ||||||||
| Total fruit | 152 | 3.4 (1.20) | 3.9 (1.03) | +0.5 | ||||||||
| High users | 57 | 4.6 (0.58) | 4.5 (0.79) | -0.1 | ||||||||
| Low users | 95 | 2.7 (0.76) | 3.5 (0.96) | +0.8 | ||||||||
|
Control group | ||||||||||||
| n |
Baseline mean (SD) |
Follow up mean | Difference | |||||||||
| Total veg | 67 | 4.3 (0.90) | 4.3 (0.93) | 0 | ||||||||
| High users | 38 | 5.0 (0.54) | 4.6 (0.79) | -0.4 | ||||||||
| Low users | 29 | 3.5 (0.55) | 3.9 (0.95) | +0.4 | ||||||||
| Total fruit | 67 | 3.6 (1.19) | 4.0 (0.93) | +0.4 | ||||||||
| High users | 27 | 4.8 (0.53) | 4.5 (0.72) | -0.3 | ||||||||
| Low users | 40 | 2.8 (0.82) | 3.6 (0.91) | +0.8 | ||||||||
| Lau et al, 2012, Hong Kong, Cyberpsychology, Behavior, and Social Networking[53] | Control
n=40 Intervention n=38 100% follow-up |
All intervention participants
logged on to the website at least once and 66% logged on more than once.
Average duration of website visit was 3.75 minutes with 30
minutes’ exposure per person total. 79% read an average of 1.3 texts per week and 47% replied to 3.8 messages. Reading SMS was positively associated with change in SMR, while website exposure had no significant effects. |
Physical
activity There were no significant between group differences, but the intervention group showed a significant increase in physical activity score at the end of the intervention and the control group did not. |
Website logon rates were poor, with 66% logging on two or more times, and most participants logging on a total of three times over the study period. However, there were still significant improvements in physical activity in the intervention group, suggesting that the text messages were effective. | High | |||||||
| PACQ score mean (SD) | Control (n=40) | Intervention (n=38) | ||||||||||
| Baseline | 1.77 (0.36) | 185 (0.27) | ||||||||||
| Post-intervention | 1.85 (0.63) | 2.03 (0.52)* | ||||||||||
| *p<0.05 | ||||||||||||
| Games | ||||||||||||
| Adamo et al, 2010, Canada, Applied Physiology Nutrition and Metabolism [56] | 13 per group 85% follow-up |
The music group attended significantly more
sessions than the video game group. Music group: 93.2% (3.9%) Video game group: 86.1% (5.8%) |
Physical
activity The music group spent significantly more time exercising at peak HR (p=0.05) Music group: 24.9 (20.0) Video game group: 13.7 (12.8) The average distance pedalled was significantly higher in the music group (p=0.03) Music group: 12.5 (2.8) Video game group: 10.3 (2.2) No other measures were significantly different |
While both conditions led to improved physical health and fitness, music was significantly more effective than a cycling video game at promoting adherence as well as encouraging vigorous activity. | Medium | |||||||
| Baranowski et al, 2011, United States, American Journal of Preventive Medicine[57] | Intervention
n=103 Control n=50 Follow-up: 90% in the intervention group 80% in the control group |
Process data not reported |
Diet There was a significant group x time effect for fruit consumption. Significant group effect for fruit and vegetable consumption p=0.018 |
Playing video games resulted in a
significant increase in fruit consumption by 0.05 pieces per day when
compared to the control group, which decreased from 0.42 to 0.19 pieces
per day. However, physical activity behaviours remained unchanged. |
Medium | |||||||
| Diet (serves) | Treatment | Control | Group x time p | |||||||||
| Post 1 | Post 2 | Post 3 | Post 1 | Post 2 | Post 3 | |||||||
| FV | 1.88 | 1.85 | 2.15 | 1.56 | 1.72 | 1.48 | 0.083 | |||||
| Fruit | 0.58 | 0.49 | 0.63 | 0.42 | 0.34 | 0.19 | 0.029 | |||||
| Veg | 0.75 | 0.79 | 0.85 | 0.76 | 1.02 | 0.77 | 0.089 | |||||
| Water (oz.) | 12.81 | 12.82 | 12.32 | 11.69 | 10.07 | 9.99 | 0.704 | |||||
| Total energy (kcal) | 1604 | 1568 | 1362 | 1657 | 1693 | 1653 | 0.370 | |||||
|
Physical activity There were no significant effects for physical activity. | ||||||||||||
| Direito et al, 2015, New Zealand, Journal of Medical Internet Research[58] | Zombies, Run! n=16 Get Running n=16 Control n=18 94% follow-up |
10/32 intervention participants reported using
the app twice per week and 10/32 reported using it three times per
week. In ‘Zombies, Run!’ the most often used features were workout missions and run log. Social networking features were not used. In ‘Get Running,’ the week runs feature was most often used and only one person used the social networking feature. |
There were no significant effects
for outcomes of physical activity, either self-reported or collected via
accelerometer. All p-values are greater than 0.4 and most are above 0.9 |
Running apps were not effective at increasing physical activing amongst adolescents in New Zealand. | Medium | |||||||
| Multi-component interventions with a digital element | ||||||||||||
| Lubans et al, 2009, Australia, Journal of Adolescent Health[11] | Intervention
n=58 Control n=66 Follow-up: 90% in the intervention condition 75% in the control condition |
Participants in both groups
attended approximately 80% of school sport sessions. 11% of intervention
participants reported wearing the pedometer every
day. Most (~2/3) participants said their parents never read or signed the handbooks. On a scale of 1-5, the emails were given an average score of 3.06. |
Diet There were no significant between-groups differences in dietary behaviour. However, the number of boys in the intervention group who consumed 3 or more snacks per day significantly decreased from 47% to 21% and the number of girls in the intervention group who ate 2 or more servings of fruit per day significantly increased. Results for boys – percent of participants who met the recommended intake per day |
Most participants reported that
their parents did not look at the material provided, and almost none of
the participants responded to the support emails
provided. 11% of participants reported wearing the pedometer every day. As a whole, Program X had a significant effect on the step count of those who were classified as low active at baseline. The authors conclude that self-monitoring with pedometers was the component of the intervention that resulted in this improvement. |
High | |||||||
| Intake | Intervention | Control | ||||||||||
| Baseline | Follow-up | Baseline | Follow-up | |||||||||
| ≥4 servings of vegetables/day | 20.0 | 25.0 | 13.6 | 5.6 | ||||||||
| ≥2 servings of fruit/day | 53.3 | 67.9 | 77.3 | 77.8 | ||||||||
| <250 ml soft drink/day | 56.7 | 71.4 | 36.4 | 61.1 | ||||||||
| ≥400 ml of water/day | 70.0 | 73.3 | 56.5 | 63.6 | ||||||||
| ≤2 unhealthy snacks/day* | 53.3 | 78.6 | 50.0 | 66.7 | ||||||||
| *P<0.05 | ||||||||||||
|
Results for girls – percent of participants who met the
recommended intake per day
| ||||||||||||
| Intake | Intervention | Control | ||||||||||
| Baseline | Follow-up | Baseline | Follow-up | |||||||||
| ≥4 servings of vegetables/day | 14.3 | 28.0 | 11.9 | 28.6 | ||||||||
| ≥2 servings of fruit/day* | 46.4 | 76.0 | 69.0 | 77.1 | ||||||||
| <250 ml soft drink/day | 78.6 | 84.0 | 76.2 | 74.3 | ||||||||
| ≥400 ml of water/day | 57.1 | 75.0 | 57.1 | 69.8 | ||||||||
| ≤2 unhealthy snacks/day | 78.6 | 76.0 | 81.0 | 74.3 | ||||||||
| *p<0.05 | ||||||||||||
|
Physical
activity Boys and girls both showed a significant group x time effect for mean steps per day. For those classified as low active at baseline, there was a significant treatment effect. Results for boys | ||||||||||||
| Behaviour | Intervention | Control | F | |||||||||
|
Baseline
Mean (SD) |
Follow-up
Mean (SD) |
Baseline
Mean (SD) |
Follow-up
Mean (SD) |
|||||||||
| Mean steps/day | 13306 (4945) |
12158 (3375) |
10805 (4395) |
8728 (3603) |
7.4* | |||||||
| TV hours/day | 2.47 (1.55) | 2.14 (1.18) | 2.86 (1.42) | 2.39 (0.70) | 0.17 | |||||||
| Computer hours/day | 1.17 (1.02) | 1.54 (1.20) | 1.68 (1.13) | 1.67 (1.09) | 1.9 | |||||||
| Electronic games hours/day | 1.27 (1.20) | 1.14 (1.24) | 1.00 (0.93) | 0.72 (0.75) | -0.08 | |||||||
| *p<0.05 | ||||||||||||
|
Results for girls
| ||||||||||||
| Behaviour | Intervention | Control | F | |||||||||
|
Baseline
Mean (SD) |
Follow-up
Mean (SD) |
Baseline
Mean (SD) |
Follow-up
Mean (SD) |
|||||||||
| Mean steps/day | 10547 (2810) |
11880 (2314) |
10739 (2742) |
8309 (2400) |
29.6* | |||||||
| TV hours/day | 2.50 (1.20) | 2.08 (1.32) | 2.19 (1.07) | 2.26 (0.98) | 3.63 | |||||||
| Computer hours/day | 1.54 (0.96) | 1.60 (1.04) | 2.21 (1.74) | 2.26 (1.58) | 0.04 | |||||||
| Electronic games hours/day | 0.25 (0.59) | 0.24 (0.60) | 0.45 (0.92) | 0.51 (1.04) | -1.00 | |||||||
| *p<0.05 | ||||||||||||
| Lubans et al, 2010, Australia, BMC Public Health[62] AND Lubans et al, 2012, Australia, Archives of Pediatrics and Adolescent Medicine[72] AND Dewar et al, 2014, Australia, Journal of Science and Medicine in Sport[63] | Intervention n=148 Control n=179 80% follow-up |
Average
attendance School sport sessions: 60.6% Nutrition workshops: 65% Optional lunchtime sessions: 24.6% On average, participants completed 8.8% of home challenges. No process data on text messaging element. |
There were no significant changes in any dietary, physical activity or sedentary behaviours at 1 year. | NEAT girls, which was a school-based multi-component intervention that included a text messaging element, did not result in any significant changes in diet or physical activity. | Medium | |||||||
| Smith et al, 2014, Australia, Pediatrics [65] | Intervention
n=181 Control n=180 80% follow-up |
65% of boys attended more than
70% of sport sessions 44% attended at least 2/3 of lunchtime sessions 70% of boys owned a smartphone or tablet and 63% reported using the ATLAS app. Of those who owned a smartphone, 70% reported using the goal setting function, 62% used the technique monitoring function, 49% used step tracking and 49% used the fitness challenge feature. Half of the group agreed that the push prompt was a useful reminder and 44% agreed that the app was enjoyable to use. However, 95% agreed that the ATLAS programme as a whole was enjoyable. |
Diet Intervention boys significantly decreased their sweetened beverage consumption compared to control boys. |
70% of participants had
smartphones and 63% reported using the app. This multicomponent intervention that included the use of a smartphone app and website was effective at reducing screen time and sweetened beverage consumption, but not at increasing physical activity amongst boys from deprived backgrounds. |
Medium | |||||||
| Outcome | Baseline | 8 months | Change | P value | Adjusted difference in change | P value | ||||||
| Sweetened beverage intake (glasses/day) | ||||||||||||
| Intervention | 3.9±0.40 | 3.1±0.41 | -0.8±0.19 | <0.001 | ||||||||
| Control | 3.9±0.36 | 3.7±0.36 | -0.1±0.18 | <0.001 | 5.7±.067 | .01 | ||||||
|
Physical
activity There were no improvements in physical activity, although boys in the intervention group reported less screen time at follow-up. Physical activity outcomes presented at mean ± SE. Models were adjusted for school clustering and participant socioeconomic status | ||||||||||||
| Outcome | Baseline | 8 Months | Change | P value | Adjusted difference in change | P value | ||||||
| Weekday PA (counts/min)1 | ||||||||||||
| Intervention | 538±30.81 | 515±33.51 | -23±18.08 | 0.21 | -19±23.30 | 0.41 | ||||||
| Control | 477±27.18 | 473±28.58 | -3±14.69 | 0.81 | ||||||||
| Weekend PA (counts/min)2 | ||||||||||||
| Intervention | 435±47.19 | 410±54.85 | -25±40.25 | 0.53 | -8±53.94 | 0.557 | ||||||
| Control | 404±42.42 | 387±47.13 | -17±35.97 | 0.64 | ||||||||
| Weekday MVPA, %1 | ||||||||||||
| Intervention | 8.6±0.58 | 8.3±0.63 | -0.4±0.34 | 0.28 | -0.7±0.44 | 0.14 | ||||||
| Control | 7.5±0.51 | 7.8±0.54 | 0.3±0.28 | 0.30 | ||||||||
| Weekend MVPA, %2 | ||||||||||||
| Intervention | 6.2±0.78 | 6.0±0.90 | -0.2±0.67 | 0.73 | -0.1±0.90 | 0.80 | ||||||
| Control | 5.8±0.70 | 5.7±0.78 | -0.1±0.60 | 0.82 | ||||||||
| Screen time (min/day) | ||||||||||||
| Intervention | 109±14.18 | 112±14.52 | 3±7.25 | 0.67 | -30±10.08 | 0.03 | ||||||
| Control | 132±12.78 | 165±12.94 | 33±7.0 | <0.001 | ||||||||
| ||||||||||||
| Email-delivered intervention | ||||||||||||
| Abroms et al, 2004, United States, American Journal of Health promotion[59] | Intervention
n=37 Control n=33 75% follow-up |
45.9% of participants replied to the Ezine at least once and 36.6% responded to each volume by answering quiz questions or interacting with the advice column. |
Diet There were no significant changes in fruit and vegetable consumption Intervention group Baseline: 9.7 servings/day Follow-up: 8.4 servings/day Control group Baseline: 10.6 servings/day Follow-up: 7.3 servings/day |
There were no significant changes in health behaviours as a result of the Ezine intervention. | High | |||||||
|
Physical
activity There were no significant changes in hours of exercise per week. Intervention group Baseline: 17.38 hours Follow-up: 12.31 hours Control group Baseline: 16.74 hours Follow-up: 12.6 hours | ||||||||||||
| Social media intervention | ||||||||||||
| Wojcicki et al, 2014, United States, JMIR Research Protocols [60] | Behavioural n=10 Informational n=11 95% follow-up |
80% of daily posts were viewed by all participants, but engagement with posts (likes, comments, shares) was low at 26.7% of posts. |
Physical
activity There were significant (p=0.009) improvements in self-reported physical activity over time, but there was no group x time interaction. There were no significant results for objectively measured physical activity or for self-reported sedentary behaviours in either group. |
While there was a significant increase in self-reported leisure activity, there was no change in objectively measured total physical activity as a result of this Facebook intervention. | Low | |||||||
Data synthesis
Review findings are reported in accordance with PRISMA guidelines [34] and a meta-analysis was not possible due to considerable heterogeneity in study design, study quality, intervention design, and study population [33].. Summary tables were produced describing the characteristics of included studies, their results and quality assessment (Tables 3, 4). In both tables, studies were grouped by the primary type of digital medium used to deliver the intervention. These groups were determined after reviewing all studies, and included website interventions, text message interventions, games and apps, email interventions, social media interventions and multi-component interventions that included a digital element,. If an intervention used multiple digital elements, it was grouped according to the element whose aim was to effect behaviour change rather than, for example, to collect data or act as a reminder. Within each group, studies were listed in chronological order by date of publication.
Table 3. Descriptions of included studies.
| Author, publication year, country, journal | Study design | Intervention features | Setting and participants | Assessment | Analysis and confounding | |||
|---|---|---|---|---|---|---|---|---|
| Website interventions | ||||||||
| Frenn et al, 2005, United States, Applied Nursing Research [42] | Quasi-experimental
design 3 classes were allocated to intervention and 3 were allocated to control Control participants had usual assignments |
|
Set in an urban public middle school in the Midwest of America. Participants were 103 7th grade students (age 12-14) in 6 classes. Most participants (70-75%) qualified for free lunch, and 70% were girls. About half of participants were Hispanic, 20% were Black, and the rest were White or another ethnicity. |
Diet Assessments were completed 1 week pre- and 1 week post-intervention. For dietary fat, 7 staging questions were asked. A Food habits questionnaire was used to measure percentage dietary fat. This includes a 21-item survey about various high-and low-fat food with a 5-option response |
Only those who completed more than half of the sessions (3 sessions for diet and 2 sessions for PA) were included in the intervention group for analysis. Because data were treated this way, general linear model analysis was not possible, so t-tests were used. | |||
|
Physical
activity Assessments were completed 1 week pre- and 1 week post-intervention. Child and Adolescent Activity log was used to collect physical activity data. | ||||||||
|
Williamson et al, 2005, United States, Eating and Weight Disorders
- Studies on Anorexia, Bulimia and Obesity [68] AND
Williamson et al, 2006, United States, Obesity [39] |
Randomised controlled
trial The control group received information, but no behavioural elements. |
|
Participants were 57
overweight or obese African American girls and one obese parent. In
every case but one, the parent was the girl's
mother. Adolescents were aged 11-15 and the average parent age was 43. Average adolescent BMI was 36.4 and body fat % was 45.9 on average. Parents’ values were 38.4 BMI and 48.4% fat on average. Participants were required to contribute $300 toward the purchase of a new computer. |
Diet Assessment completed at baseline, and months 6, 12, 18 and 24. Dietary assessment was conducted in the clinic, using a face-to-face questionnaire. |
ITT was used, according to last
value carried forward methodology. ANCOVA was used to analyse change over time and baseline values were included as a covariate. |
|||
|
Physical
activity Assessment completed at baseline, and months 6, 12, 18 and 24. The Weight Loss Behaviour Scale (WLBS) was completed online and used to assess behaviours. | ||||||||
|
Jago et al, 2006, United States, Preventive Medicine [45]
Thompson et al, 2009, United States, Preventive Medicine[46] |
Randomised controlled
trial. Run in two waves: a Spring wave and an Autumn wave. One intervention arm received a physical activity intervention while the other received a mirror image fruit/vegetable intervention. |
|
Trial run with boy scouts in
Houston, TX. Participants were 473 10- to 14-year-old boy scouts from 42 troops. The majority of participants were White. Parental education was significantly associated with intervention group and wave. |
Physical
activity Assessments completed at baseline, immediately post-intervention and 6 months post-intervention. Physical activity was measured for 3 consecutive days at each time point using an accelerometer. Diet Fruit and vegetable consumption was measured using a modified FFQ and asked about consumption over the past 7 days. |
PA data were categorized into sedentary,
light, and moderate to vigorous. Results were analysed using chi-square tests and independent t tests. Repeated measures ANOVA using the Proc Mixed procedure was used to detect differences in physical activity over time between groups. Fixed effects included main effects for treatment group, visit time, wave and interactions within groups, visit time, and wave main effects. Analyses were run separately where either sedentary behaviour, light PA, MVPA, or counts per minute was the dependent variable. Diet was analysed using nested repeated measures to detect changes over time. Models were controlled for BMI, ethnicity and parental education. |
|||
| Slootmaker et al, 2010, Netherlands, Preventive Medicine [49] | Randomised controlled
trial. Control group received a single informational brochure with general physical activity advice. The trial was run for 3 months. |
|
Online intervention where
participants were recruited in secondary schools in
Amsterdam. Volunteers were aged 13-17 and the least active 50% were invited to participate. |
Physical
activity Assessed at baseline, end of 3-month intervention, and 5 months post-intervention. The Activity Questionnaire for Adolescents and Adults was used to record physical activity in the last week of light, moderate and vigorous activity in metabolic equivalent (MET), as well as sedentary time. |
ITT was used. Linear regression analysis was used to test the differences between the intervention and control group at follow-up. Baseline values were included as covariates. Models were checked for effect modification by gender, and adjusted for programme adherence based on login frequency. |
|||
|
De Bourdeaudhuij et al, 2010, Cities participating in HELENA
(Vienna, Ghent, Heraklion, Dortmund, Athens and Stockholm), Journal
of Adolescent Health [47]
AND Cook et al, 2014, Cities participating in HELENA (see above), Journal of School Health [48] |
Quasi-experimental study where schools were
randomised to intervention or control. The intervention lasted 20 minutes and participants received the advice at baseline and 1 month. |
|
The intervention was completed in
classrooms during school hours, but some teachers refused to allow class
time, so these students were asked to complete the intervention at
home. Participants were aged 12-17 51% were boys 47.6% were not complying with the recommended 60 minutes of moderate to vigorous physical activity per day at baseline. The trial was run in 6 different cities across Europe, so there was a wide range of demographic characteristics. |
Physical
activity Baseline, 1 month, and 3 months. Screening questionnaires the students filled in were used to collect data. PA levels were determined using an adolescent adaptation of the International Physical Activity Questionnaire, which asked for minutes of activity of different types. |
Intention to treat: baseline observation
carried forward. Linear mixed models with condition as between-subjects factor was used to analyse changes from baseline to 1 month. Gender was included as a factor in this model, and analyses were adjusted for baseline PA and age. This was repeated to assess longer term changes at 3 months. All analyses were repeated using only those who did not meet the recommended 60 minutes per day MVPA at baseline. |
|||
| Maes et al, 2011, Cities participating in HELENA (see above), Public Health Nutrition [51] | Controlled trial (pilot evaluation). Not randomised. |
|
The intervention was completed as
part of HELENA, in classrooms during school hours. Participants were
aged 12-17. The trial was run in 2007. |
Diet A short-term FFQ was completed at 1 month and medium term FFQ was completed at 3 months. FFQ was based on a validated computerized FFQ for fat intake, and further adapted to measure intake of target nutrients. Each country could include country-specific items. Results were analysed using a food composition database with 137 items. |
Only those with complete data sets (data at
each time point) were included in the analysis. Linear mixed models were used to analyse intervention effects on dietary measures. Condition was the between-subjects factor. Other factors included gender, and weight status. Adjusted for baseline intake and age. This was done for data from 1 month and 3 months. |
|||
| Chen et al, 2011, United States, Journal of Adolescent Health [43] | Randomised controlled trial where
Chinese American parent/adolescent pairs were randomised to intervention
or control. Run for 8 weeks |
|
Internet intervention
that could be accessed from any computer. Mean participant age was 12.5 (SD: 3.15) and all identified as Chinese or Chinese-American. Parents generally had a low acculturation score. 1/3 of participating adolescents were overweight. |
Diet Adolescents completed questionnaires at baseline, 2 months, 6 months, and 8 months after baseline assessment. A 3-day food diary was used to assess diet. |
Linear mixed effects modelling was
used to analyse change over time. T-tests were used to analyse differences between results at each follow up time point. |
|||
|
Physical
activity Adolescents completed questionnaires at baseline, 2 months, 6 months, and 8 months after baseline assessment. A dual-mode actigraph was worn on the hip for 7 days, and the output was average counts in moderate and vigorous physical activity. | ||||||||
| Ezendam et al, 2012, Netherlands, Archives of Paediatrics and Adolescent Medicine [40] | Cluster randomised controlled
trial Run for 10 weeks |
‘FAT ain’t
PHAT’
|
Set in schools in the
Rotterdam area. Participants were 833 pupils aged 12-13. There were significant differences between groups with regards to gender and ethnicity. The intervention group had significantly more boys and the control group had significantly more participants of western ethnicity. Most participants were normal weight. 9% were underweight and 15% were overweight or obese. |
Diet Assessments completed at baseline, 4 month follow-up, and 2 year follow-up. Food frequency questionnaire for sugar-sweetened beverages 24-hour recall for snacks and fruit and vegetable consumption. |
Intention to treat: baseline
observation carried forward and last observation carried
forward. Multilevel linear and logistic regression models were used, regressing outcome measures on treatment group and baseline values. Models were adjusted for sex, education, and ethnicity. Analyses were conducted separately for each time point, and were done for the entire group as well as for only those not meeting MVPA recommendations at baseline (risk group). |
|||
|
Physical
activity Completed at baseline, 4 month follow-up, and 2 year follow-up. Flemish validated questionnaire to assess sports during leisure time, active transportation to school, television viewing, and computer use in the past 7 days. Questionnaire asked about number of days doing at least 1 hour MVPA. Pedometers were worn by a random subsample of 5 students per class for 7 consecutive days. | ||||||||
| Whittemore et al, 2012, United States, Journal of Adolescent Health [67] | Cluster RCT (clustered by class) to compare two school-based internet obesity prevention programmes. | HEALTH[e]TEEN
|
Set in three high
schools in two cities in the north east of America. 384 pupils were recruited from biology classes at participating schools. Participants were aged 14-17, with about 70% aged 14-15. 60% of participants were female, and 40% were overweight or obese. |
Diet Assessments were completed at baseline, 3 months and 6 months. Nutrition behaviour was measured with a 22-item survey. Key items were evaluated, and total scores were also calculated ranging from 0 (unhealthy) to 97 (healthy). |
Mixed model analyses with autoregressive covariance for repeated data were used, including an ITT analysis. The analyses tested for time effect as well as group x time effect. Analyses were adjusted for age, gender, and race/ethnicity. Random effect of school or class was added to the model when it was significant. | |||
|
Physical
activity Assessments were completed at baseline, 3 months and 6 months. Sedentary behaviour was measured using a validated questionnaire. Physical activity was measured using the PA items from YRBS. | ||||||||
| Cullen et al, 2013, United States, Health Education Research [44] | Randomised controlled trial Run for 8 weeks |
Teen Choice: Food & Fitness
|
The trial was run in Houston,
Texas. Participants were 390 adolescents aged 12-17 with internet access. 70% were normal weight and 30% were overweight (>85th percentile BMI for age and gender) |
Assessments were completed immediately before
the trial period and at the end of the trial period. (Week 1 and week
8) Validated youth risk behaviour survey (YRBS) was used to collect data on diet and physical activity. |
One way analyses of covariance and logistic regression were conducted for each dependent variable, including all potential confounding (gender, age, race, SES, parent education level, numbers of children and adults at home, TV availability in child's bedroom and social desirability) as covariates. | |||
| Patrick et al, 2013, United States, Journal of Diabetes Science and Technology [41] | Randomised controlled trial with
multiple interventions including a website. The trial was run for 1 year |
Website
|
The trial was run through a diabetes clinic in San Diego, California. Participants were aged 12-16 and at high risk for diabetes, but did not have diabetes. Average BMI was 97.6th percentile for age and gender |
Diet Assessments were completed at baseline, 6 months, and at the end of the intervention (12 months). Diet was assessed using the youth/adolescent FFQ (validated questionnaire for adolescents). |
Mixed model analysis was used to
test group effects at 12 months. The model used maximum likelihood
repeated measures and ITT analysis was conducted. Analyses looked at the
effect of treatment group as well as the interaction between treatment
group and time. Relative change scores were calculated as (12 month measure – baseline measure)/baseline measure. These were used in partial correlation analyses to test the correlations between change in anthropometrics and behavioural outcomes, and between behavioural outcomes and use of change strategies |
|||
|
Physical
activity Assessments completed at baseline, 6 months, and at the end of the intervention (12 months).Physical activity was assessed using a 7-day physical activity recall interview. Sedentary behaviour was measured using an eight-item survey. | ||||||||
| Jones et al, 2014, United States, Journal of Medical Internet Research [38] | Uncontrolled feasibility study using a parallel, nonrandomized design. | Students who were overweight were
assigned to the Weight Management (WM) track, and those who were normal
weight were assigned to Healthy Habits (HH) track. Two tracks differ mostly in language used to discuss topics, rather than topics themselves. Weight management track also includes an optional weight logging chart.
|
Set in 1 high school in San
Francisco and 1 high school in St Louis. Participants were assigned to Healthy Habits (HH) or Weight Management (WM) based on BMI. There were some significant differences between groups at baseline, so data are presented in the table below. Data are presented as n(%) |
Youth Risk Behaviour Survey was used at baseline and 1 week post-intervention to assess both diet and physical activity | Regression analysis was used to
examine intervention effects, controlling for baseline
measures. Analytical methods are not well described |
|||
| Variable | HH track (n=225) | WM track (n=111) | P value | |||||
| Age, mean (SD) | 14.3 (0.63) | 14.3 (0.74) | 0.999 | |||||
| White | 91 (40.4) | 13 (11.7) | <0.001 | |||||
| Black | 30 (13.3) | 26 (23.4) | 0.029 | |||||
| Multiracial | 94 (41.8) | 63 (56.8) | 0.011 | |||||
| Hispanic/Latino | 90 (40.0) | 56 (50.5) | 0.079 | |||||
| Ate fruit 2 or more times per day | 48 (24.8) | 23 (25.3) | 0.894 | |||||
| Ate vegetables 2 or more times per day | 35 (18.1) | 16 (17.6) | 0.370 | |||||
| Drank soda once or more per day | 29 (15.0) | 29 (31.2) | 0.003 | |||||
| PA 5 or more days per week | 112 (58.0) | 29 (31.8) | <0.001 | |||||
| 2 hours or more of TV per day | 47 (24.3) | 44 (48.4) | <0.001 | |||||
| Played video games 2 hours or more per day | 47 (24.3) | 24 (26.4) | 0.692 | |||||
| Lana et al, 2014, Spain and Mexico, Preventive Medicine [35] | Randomised controlled trial | Cancer prevention intervention
called PREVENCANADOL
|
Set in secondary schools in Spain
and Mexico. Participant characteristics at baseline Percentages reported here |
Diet Assessments were completed at baseline and at the end of the academic year. The study focused on various cancer risk behaviours. Food was assessed using a validated FFQ. Physical activity Assessments were completed at baseline and post-intervention. Sedentary behaviour was assessed, but details of this tool are not provided. |
Students completed a cancer risk
questionnaire which assessed smoking, diet, alcohol, sedentary
behaviours and sun exposure. These factors were scored separately, and
used to come up with a final risk score. Changes in risky behaviours were analysed using McNemar’s and Wilcoxon’s tests. Then GLM was used to test for association between changes in behaviour and group allocation. Logistic regression was performed to assess OR for giving up risky behaviours at post-test according to study group. Binary logistic regression was used to assess whether there was a difference in outcome between those who received text messages and those who did not. |
|||
| Characteristic | Control (n=987) | Intervention (n=1014) | P value | |||||
| From Mexico | 80.6 | 75.6 | <0.01 | |||||
| Female | 54.2 | 55.4 | 0.310 | |||||
|
Age 12 years 13 years 14 years 15-16 years |
20.5 42.7 26.4 9.4 |
26.6 38.5 25.7 9.2 |
<0.01 | |||||
|
Father’s
education Primary Secondary University |
6.9 43.5 49.6 |
7.7 42.0 50.3 |
0.211 | |||||
|
Mother’s
education Primary Secondary University |
7.6 37.6 54.8 |
5.2 41.8 53.0 |
0.061 | |||||
|
Cancer risk
behaviours Not enough fruits Not enough vegetables Dietary fat Overweight/obesity Sedentarism |
38.6 33.3 55.1 16.2 28.1 |
35.4 36.5 50.1 15.1 27.5 |
0.175 0.169 <0.05 0.800 0.317 |
|||||
| Guthrie et al, 2015, United States, PLOS ONE [50] | Randomised controlled pilot
study Run for 6 weeks |
There were three study conditions, all of
which used the Zamzee activity meter (accelerometer), which tracks MVPA,
and uploads data to a website.
Received Zamzee meters, but had no access to the website, and received no other intervention or feedback. Condition 2: Active control (n=61) Received Zamzee meters and the Dance Dance Revolution game. Did not receive any feedback or further information. Condition 3: Intervention group (n=62) Received Zamzee device as well as access to the website |
Participants were 182 middle school students in West Virginia and California. The age range was 11-14, about half of participants were girls and half were Caucasian. | Physical activity was monitored constantly via Zamzee device (accelerometer) | Physical activity was analysed as total MVPA
per day as well as well as MVPA rate (MVPA divided by duration of
wearing the device per day). Mixed effects linear modelling was used. Where significant group or group x time effects were found, follow-up contrast analyses assessed the statistical significance of pairwise differences among groups. ITT analysis was used Analysis of MVPA duration was controlled for duration of meter wearing. Analysis of MVPA rates were weighted by daily meter wear duration. All analyses were controlled for study site, sex, BMI. |
|||
| Sousa et al, 2015, Portugal, European Journal of Pediatrics[36] | Quasi-experimental pre- post- design | In addition to care received in the obesity
clinic, which included medical, psychological, nutritional and physical
activity counselling, intervention participants received access to the
e-therapeutic platform (Next.Step).
|
The trial was run through a
paediatric obesity clinic in Portugal – internet
intervention. Participants were 94 adolescents who attended the clinic. Average age was 14 and the average hours of physical activity per week was approximately 4.5 and screen time was 22 hours per week. |
Assessments were completed at 12 weeks and 24 weeks. Self-report instruments were used. ALP (adolescent lifestyle profile) provided data on healthy behaviours. Analyses health responsibility, physical activity, nutrition, positive life perspective, interpersonal relationship, stress management and spiritual and provides an index score. | Generalized linear models with likelihood
ratio test. Group was the fixed factor and baseline measures were
covariates. Both ITT and PP analyses were conducted. |
|||
| Text Message Interventions | ||||||||
| Newton et al, 2009, New Zealand, Diabetes Care [54] | Randomised controlled trial | Brief text message intervention
|
Outpatient setting from four
regional adolescent diabetes services in New
Zealand. Participants were adolescents aged 11-18 with type 1 diabetes. |
Assessment was completed at baseline and post-intervention (12 weeks). 4 day step count was measured by closed pedometer and 7 day physical activity self-reported on a validated questionnaire. | Linear regression was performed to assess
final differences between groups. ITT methodology: baseline measures carried forward. Individuals with missing baseline data were not included. |
|||
| Sirriyeh et al, 2010, United Kingdom, British Journal of Health Psychology [55] | Exploratory pilot randomised controlled trial | Daily text messages that targeted instrumental
beliefs, affective beliefs, or both, regarding physical
activity. The control group received weekly messages. Affective intervention: Messages regarding the anticipatory affective gains associated with regular exercise, such as ‘physical activity can make you feel cheerful. What activity will you do today?’ Instrumental intervention: Messages regarding the instrumental gains associated with regular exercise, such as ‘physical activity can help maintain a healthy weight. What activity will you do today?’ Combined: An equal number of messages from the affective and instrumental intervention were sent. Control: Messages were neutral, and ended with, ‘what activity will you do today?’ |
Participants were recruited from 6th form states schools in West Yorkshire. They were Students at participating schools, age 16-19, 70% female. | Assessment was completed at baseline and at
the end of the 14-day intervention. Validated questionnaire: International Physical Activity Questionnaire. Only questions regarding moderate and vigorous activity were included, as these tend to be more accurately reported. Data were analysed as metabolic equivalent (MET) minutes, where moderate and vigorous MET minutes were calculated using the compendium of physical activities. |
ANCOVA was used to assess treatment effects,
while controlling for baseline physical activity. Where main effects were identified, a post hoc Bonferroni test was used to identify which intervention produced the effect. Another ANCOVA was run to compare the effects for those who were meeting activity guidelines at baseline and those who were not. |
|||
| Bech-Larsen and Gronhoj, 2012, Denmark, International Journal of Consumer Studies [52] | Cluster randomised controlled trial (classes
were randomly assigned). Run for 8 weeks |
Text message feedback diary
|
12 classes of 12 year olds from
different schools in Denmark. Students were contacted via SMS
system. No further demographic data are presented. |
Each student was given a pre-intervention
(week 1) and post-intervention (6 weeks after completion of the study)
questionnaire about fruit and vegetable consumption. The intervention group reported fruit and vegetable intake daily via the SMS system. Both the control and intervention groups completed self-administered surveys 1 week prior to the start of the intervention and 6 weeks after completion. |
Based on pre-intervention results, students
were split into high consumption and low consumption groups, and
analysed separately. Median consumption of the entire sample was used to
split the groups. 4 weeks of SMS diary from the intervention group data was analysed by comparing means and performing t-tests and ANOVA. GLM repeated measure analyses were used to test for significant changes between pre-intervention and post-intervention consumption of fruits and vegetables. |
|||
| Lau et al, 2012, Hong Kong, Cyberpsychology, Behavior, and Social Networking[53] | Quasi-experimental pilot study with a control group. | Website and SMS
intervention Teen-step.com
|
Participants were recruited from
secondary schools in Hong Kong, and the intervention was internet-based,
to be accessed at home. 78 adolescents in Hong Kong. Characteristics of groups at baseline presented as mean (SD) or % |
Assessment was completed at
baseline and at the end of the 8-week intervention. Nine item Physical Activity Questionnaire for Older Children (PAQC) was used to measure PA in the last 7 days. Previously validated. A validated staging algorithm was used to measure stage of motivational readiness. |
ITT (last observation carried
forward). Repeated measures ANOVA was conducted to analyse treatment x time effect on physical activity level. |
|||
|
Control
(n=40) |
Intervention (n=38) | |||||||
| Age* | 13.26 (1.14) | 12.29 (0.87) | ||||||
| BMI | 18.99 (3.22) | 18.31 (3.48) | ||||||
| % female | 62.5% | 68.4% | ||||||
|
Internet usage (days/week)*
None 1-2 days 3-4 days 5-6 days 7 days |
35% 32.5% 12.5% 5% 15% |
7.9% 21.1% 15.8% 21.1% 34.2% |
||||||
| *differences between groups p<0.05 | ||||||||
| Games and Apps | ||||||||
| Adamo et al, 2010, Canada, Applied Physiology Nutrition and Metabolism[56] | Randomised trial with a comparison
group Run for 10 weeks |
The intervention was a cycling video game
called Game Bike, which used a stationary bicycle. Participants were
asked to come to the clinic twice per week to exercise for 60 minutes on
the Game Bike, but could stop and rest as often as they wanted. There
were multiple cycling video games that participants could choose
from. The comparison group used the same stationary bike, but listened to music of their choice rather than playing the game. |
Participants were recruited in the
Endocrinology clinic at a children’s hospital in Ontario. They
were aged 13-15 and were obese or they were overweight with a further
risk factor for cardiovascular disease or diabetes. There were 7 boys and 6 girls per group. |
Assessments were completed at the beginning
and at the end of the 10-week intervention period. Energy expenditure
was measured using polar heart rate monitors. Distance and speed of exercise was calculated by the computer system attached to the stationary bike. Exercise intensity was measured by comparing predicted maximum heartrate to average heartrate throughout the session. |
Only t tests were used, so adjustment for confounding was not possible. | |||
| Baranowski et al, 2011, United States, American Journal of Preventive Medicine [57] | Randomised controlled trial to evaluate the effectiveness of two computer games played consecutively | Participants played ‘Escape
from Diab’ and then ‘Nanoswarm: Invasion from Inner
Space,’
|
Set in
participants’ homes. Participants were aged 10-12 and within the 50th-95th percentile BMI for age and gender. 56% male in both groups Predominantly White, with 24.2% African-American, 28.1% Hispanic, and 7.8% other 68.6% had a household member with a college degree or more. At baseline there were significant differences between groups with regards to fruit/vegetable consumption, total energy intake, physical activity and BMI z-score. |
Diet Assessments were completed at baseline, between games, after the second game, and at 2 months post-intervention. Three 24-hour dietary recalls. The first was in person, the next two were over the phone and all were conducted by registered dietitians who were blinded to treatment group. |
Mixed model assessed effects of
video games on fruit and vegetable intake, water consumption, and PA.
Group x time effects were calculated. Separate models were used for each dependent variable with baseline measures used as a covariate. Post-hoc analyses were used for significant interactions to assess linear or quadratic trend over time. Analyses also controlled for potential confounding variables including age group, gender, race, household education, social desirability of response, and duration of game play. |
|||
|
Physical
activity Assessments completed at baseline, between games, after the second game, and at 2 months post-intervention. Accelerometer. Only those who provided 4 days of accelerometer data were included in the analysis. | ||||||||
| Direito et al, 2015, New Zealand, Journal of Medical Internet Research [58] | 3 arm parallel randomised controlled trial run for 8 weeks | Comparing ‘Zombies, Run! 5k
training app’ (immersive) and ‘Get Running – Couch
to 5k’ (non-immersive) Participants were encouraged to use the app 3 times per week, but no additional measures were taken to enforce this. |
The trial was set in Auckland, New
Zealand. Participants were aged 14-17, the majority were described as NZ European and slightly more than half in each group were female. |
Assessment was completed at baseline and 8
weeks. Physical activity was self-reported using the Physical Activity Questionnaire for Adolescents (validated). Participants wore an accelerometer for 7 days and completed a log of accelerometer use. |
Intention to treat
analysis. ANCOVA was used to measure differences between groups, adjusting for baseline measure and gender. Per-protocol analyses were also performed using the same methodology. |
|||
| Multi-component interventions with a digital element | ||||||||
| Lubans et al, 2009, Australia, Journal of Adolescent Health [11] | Randomised controlled trial | Program X consisted of 5
components
|
School based
intervention with additional email support. 6 secondary schools
participated. They were in urban areas with low-to-moderate
socioeconomic status. Participants were secondary school students aged 13-15. |
Diet Assessments completed at baseline and at the end of the 6-month study period. Diet was assessed using a questionnaire from the NSW Schools Physical Activity and Nutrition Study (SPANS). |
Assessments completed at baseline
and post-intervention. Sealed pedometers were worn for 5 days (including
4 school days and 1 weekend day) Sedentary behaviour was measured using an adapted version of the Adolescent Sedentary Activity Questionnaire. |
|||
|
Physical
activity Assessments completed at baseline and post-intervention. Sealed pedometers were worn for 5 days (including 4 school days and 1 weekend day) Sedentary behaviour was measured using an adapted version of the Adolescent Sedentary Activity Questionnaire. | ||||||||
| Lubans et al, 2010, Australia, BMC Public Health [62] AND Lubans et al, 2012, Australia, Archives of Pediatrics and Adolescent Medicine [72] AND Dewar et al, 2014, Australia, Journal of Science and Medicine in Sport [63] | Group randomised controlled
trial Run for 1 year |
NEAT girls: school-based
intervention
|
Set in secondary
schools in the bottom 50% of SEIFA index in
Australia. Eligible girls were in grade 8, attending one of the schools, considered by PE teacher to be disengaged in PE and/or not currently participating in sport. |
Diet Assessments were completed at baseline and 12 months. Diet was assessed using validated Australian Eating Survey FFQ. |
Accelerometer data were included
if participants were them for at least 600 minutes per day for at least
3 days, including a weekend day. Analysis was done using ITT principles Mixed models were analysed using PROC MIXED statement in SAS. |
|||
|
Physical
activity Assessments were completed at baseline and 12 months. Accelerometers were worn for 7 consecutive days during each monitoring period. Sedentary activity was assessed using accelerometer data as well as validated Adolescent Sedentary Activity Questionnaire for specific sedentary activities. | ||||||||
| Smith et al, 2014, Australia, Pediatrics [65] | Cluster randomised controlled
trial Run for 17 weeks |
|
Set in secondary
schools within low-income areas of New South Wales,
Australia. The intervention targeted adolescent boys from low-income communities. The average age was 12.5 and most participants were born in Australia. |
Diet Assessment completed at baseline and immediately post-intervention (8 months). A 2 item questionnaire about sweetened beverage intake was used. |
ITT
methodology Linear mixed modelling was used, adjusting for school clustering and SES. |
|||
|
Physical
activity Assessment completed at baseline and immediately post-intervention (8 months). Accelerometers were used to assess MVPA. Data were included for participants who wore their monitor at least 600 min/day for 3 weekdays and at least 1 weekend day. Screen time was self-reported using a validated questionnaire. | ||||||||
| Email-delivered intervention | ||||||||
| Abroms et al, 2004, United States, American Journal of Health promotion[59] | Non-randomised controlled study where those who provided email addresses were allocated to the intervention condition | Interactive email magazine:
STRENGTH Ezine
|
Set in a shopping mall
in Massachusetts, USA. Participants were 93 girls aged 15-17. |
Diet Fruit and vegetable consumption was measured at baseline and 1 year follow-up using a 6-item scaled modified from the Youth Risk Behaviour Survey. Items: fruit, fruit juice, green salad, potatoes, carrots, other vegetables. |
Only t tests were used to analyse results. Therefore, there was no adjustment for confounding. | |||
|
Physical
activity Total hours of physical activity were measured at baseline and 1 year follow-up using a 23-item scale adapted from two validated questionnaires. | ||||||||
| Social media intervention | ||||||||
| Wojcicki et al, 2014, United States, JMIR Research Protocols[60] | Pilot randomised controlled trial | SMART Facebook group
|
Participants were adolescents in
Illinois who had an active Facebook account. Only those who were not meeting physical activity guidelines at baseline were included. 57% were overweight or obese, about half were female, and the age range was 13-15. 70% of participants lived in households with an income greater than $100,000 per year. |
Data were collected at baseline and at week 8.
Objective physical activity data were collected using an accelerometer
to be worn for 7 consecutive days during the assessment
periods. Self-reported behaviour data were collected online via the Godin Leisure Time Exercise Questionnaire (validated). Self-reported sedentary time was assessed using the Adolescent Sedentary Activity Questionnaire. |
ITT approach Group x time repeated measures design was used. Interactions and main effects were examined, as well as effect sizes. This was done with mixed model ANOVAS. |
|||
Once compiled, tables were used to examine the effectiveness of the various types of intervention in improving dietary and PA behaviours of adolescents. As the studies were grouped by type of digital platform, this factor was closely examined as a first step. Individual intervention features were also analysed to determine which of these were most often associated with efficacy, and in what conditions. Here, all of the features of each intervention were listed in Table 3. Many of these, such as goal-setting, appeared in multiple studies allowing for comparison of studies that included the same component. Other features were unique to a particular study and these were also listed in the table. Data about participant engagement were also examined. Data related to cost-effectiveness, if available, were also assessed.
Results
The results of this systematic review are presented as a narrative synthesis. Of the 26 included studies, more than half (n=15) were website interventions, four were delivered via text message, three were games or apps, one was delivered via email, one used social media and three were multi-component interventions. Two studies reported dietary outcomes only, ten reported PA outcomes, and 15 reported results for both diet and PA. The earliest study was published in 2004, with 21 of the 27 studies being published since 2010. The majority of studies were targeted at a general population of adolescents (age 10-19) and five were targeted at a specific at-risk population. There was considerable variation in the risk of bias between studies, but selection bias and handling of confounding most consistently fell into the high risk category. None of the 26 included studies used random sampling and one study adequately adjusted for confounding. A summary table of bias scoring is in Appendix B. The results for intervention effectiveness are grouped by digital platform and described below.
Website interventions (n = 15)
Ten of the 15 website intervention studies were randomised controlled trials and only one study did not use a control group. Despite this, most of the studies had a medium or high risk of bias, with only two of the 15 website intervention studies being rated as having a low risk. Details about trial design are presented in Table 3 and risk of bias scores are shown in Table 4. A summary of the outcomes of all website intervention trials is presented in Table 2. Eleven of the 15 interventions that were delivered via websites assessed both dietary and PA outcomes. Two of these studies found no significant improvements in diet or PA [35, 36]. Four of these 11 had inconclusive results; in two, the main reason was the lack of a control group [37, 38] and in one, the study had a medium risk of bias and only reported results in line graphs, requiring some interpretation [39]. Here, a website and counselling intervention was trialled with obese African American girls and one obese parent. Both groups showed a significant decrease in overeating, and the intervention group showed a decrease in fattening foods that was sustained to 18 months, but not 24 months. The final study with inconclusive results had a low risk of bias. This Dutch study tested the effectiveness of a computer-tailored intervention that consisted of health information, an assessment of behaviour, tailored feedback and an option to set a health goal. There were improvements in some dietary behaviours at four months post-intervention, but none were sustained at two years [40]. For PA, there was a significant decrease in step count from baseline amongst the intervention group, but a subgroup analysis showed a significant increase in participation in sport outside of school. Due to these mixed results, it cannot be concluded that this intervention was either effective or ineffective.
Table 2. Summary of website intervention trial results*.
| Result of intervention | Number of studies (reference numbers in brackets) | ||
|---|---|---|---|
| PA | Sedentary behaviour | Diet | |
| Significant improvement | 5 [42–44, 47, 48, 50] | 2 [41, 44] | 3 [42–44] |
| No change | 3 [35, 36, 41] | 0 | 3 [35, 36, 41] |
| Inconclusive | 6 [38–40, 45, 49, 67] | 0 | 4 [38–40, 51] |
The number of trials in each cell of the table do not add up to the number of trials in this category as many appear more than once.
Five of the 11 website interventions that targeted both diet and PA resulted in significant improvements, and for one of these, the only significant result was for sedentary behaviour. This study had a medium risk of bias and tested a website intervention that was targeted at patients of a diabetes clinic in America [41]. The website provided nutrition education and included weekly challenges, goal-setting, skill-building, a reward system and feedback. Participants were also encouraged to use a pedometer for self-monitoring. This study showed a significant decrease in sedentary behaviour of 2 hours per day at 6 months and 12 months. There was no change in % calories from fat or servings of fruit and veg per 1000 calories.
Four website interventions resulted in significant improvements for both diet and PA, and one had a high risk of bias. This consisted of eight 40-minute educational sessions delivered via Blackboard.com [42]. The other three had a medium risk of bias. The first of the medium-risk studies was targeted at Chinese-American adolescents and their parents [43]. Website content was tailored to participants’ stage of change and aimed to increase self-efficacy. Parents were given three short coaching sessions to support their children. At the end of the intervention, there was an increase in fruit and vegetable intake as well as in PA and both changes were sustained at eight months. The second medium risk study was an intervention targeted at American adolescents and used a website that provided information about nutrition and PA, videos, recipes and a blog [44]. Participants were also asked to set one goal per week. At the end of the eight-week study, the intervention group showed a significant increase in vegetable consumption. Both the intervention and the control groups showed a highly significant increase in PA. Thirdly, an American study trialled a Boy Scout badge programme with a physical activity intervention arm and a dietary intervention arm, which were compared. The study did not include a control group. Groups received ‘mirror-image’ website interventions that employed goal-setting and rewarded those who met their goals with a badge [45, 46]. This trial showed only short-term (1 month) seasonal increases in exercise amongst the group that received the PA intervention. This group also showed a significant increase in low-fat vegetable consumption at 6 months compared to those who received the dietary intervention.
Three of the website interventions aimed to increase PA only. One was a part of the HELENA study, set in Austria, Belgium, Greece, Germany and Sweden, and had a medium risk of bias [47, 48]. This website collected data about physical activity behaviours and psychological determinants, and provided tailored advice based on this. This study showed significant increases in some measures of PA (cycling for transportation, moderate activity in leisure time, vigorous activity in leisure time and total moderate and vigorous physical activity). The other two PA interventions employed self-monitoring via accelerometers and websites that allowed for self-monitoring and provided support. The first had a medium risk of bias and included low active adolescents in the Netherlands [49]. This study showed a relative decrease in sedentary behaviour. The second was targeted at American adolescents and had a low risk of bias [50]. Over the study period, those using the activity meter and website showed a level of PA that was higher than those using the activity meter alone.
One trial targeted improvement of dietary behaviours only. This trial was another part of the HELENA study mentioned above, but focused on diet rather than PA. Similar to the PA programme, the website collected information via baseline survey about dietary behaviours and provided tailored advice. This intervention had a high risk of bias and showed a small, but not sustained, decrease in dietary fat [51].
Text message interventions
Of the four text message interventions, three aimed to increase PA and one focussed on dietary behaviours. The dietary intervention used a text message fruit and vegetable diary along with a nutrition education component, and had a high risk of bias. The text message intervention did not have a significant effect, but the intervention as a whole with nutrition lessons did show a significant increase in fruit and vegetable consumption [52]. Another with a high risk of bias was a PA intervention based in Hong Kong that had a website element and also sent text messages from a ‘virtual friend’ [53]. There was a significant increase in PA from baseline in the intervention group, and engagement with the text message component was much better than with the website.
The other two text message interventions had a medium risk of bias and aimed to increase PA. The first was targeted at adolescents with type 1 diabetes in New Zealand, and consisted of pedometers and weekly text messages [54]. This intervention did not show any significant effects for PA. The second was set in England, and the majority (70%) of participants were girls aged 16-19 [55]. It compared the effectiveness of ‘affective’ text messages (highlighting the way exercise can make a person feel) against ‘instrumental’ text messages (highlighting the instrumental gains of regular exercise, such as maintaining a healthy weight). Here, there was a statistically significant increase in reported PA amongst those who were inactive at baseline for the affective text message group.
Games and Apps
Three studies reported on gamified interventions, and all of them had a medium risk of bias. One was based in Canada and targeted patients of an endocrinology clinic [56]. This intervention consisted of a cycling video game attached to a stationary bike and used listening to music whilst riding the stationary bike as a control condition. Here, the control arm showed significantly better attendance and time spent doing vigorous activity than the intervention condition. It is not clear from the publication why listening to music may have led to better adherence than a video game. The second gamified intervention was based in America and consisted of two video games that aimed to increase knowledge about energy balance [57]. The only significant result was an increase in consumption of fruit by 0.05 pieces per day compared to a decrease in consumption amongst control participants. The third was set in New Zealand and compared two popular PA apps against a control group, where participants were simply given the app and asked to use it three times per week [58]. Here, neither the ‘Zombies, Run! 5k training app’ nor ‘Get Running’ showed any significant effects for outcomes of PA in adolescents, although the sample size for this study was very small (n=51).
Email-delivered intervention
There was one intervention that used email to promote fruit and vegetable consumption and PA amongst American girls age 15-17 [59]. This study had a high risk of bias, and is the earliest study in this review, being published in 2004. This intervention did not show any significant changes to dietary or PA behaviours at one-year follow-up.
Social media intervention
One study used Facebook as the primary mode of delivery [60]. This was a low risk of bias study conducted in America, and aimed to increase PA amongst adolescents who were not meeting guidelines. The Facebook page was open to participants and a parent, and provided informational content and weekly private messages to encourage exercise. While the intervention showed a significant increase in self-reported leisure-time PA, there were no significant results for total PA as measured by accelerometer.
Multi-component interventions with a digital element
Three multi-component interventions including a digital element were conducted in Australian secondary schools. All aimed to improve diet and PA in adolescents who were from areas of lower socioeconomic status. The schools ran programmes that included a number of different non-digital components as well as a digital element. While these interventions were not primarily digital, we took the decision to include them in this review as the digital element of each study was a particular focus to the researchers and they reported on use of these components specifically. Non-digital intervention components included nutrition lessons, parental involvement, sport sessions and self-monitoring. The first study included emails for additional support, the second text messaging, and the third used a smartphone app and website to support behaviour change.
The intervention that included emails showed a significant increase in step count among those who were classified as ‘low active’ at baseline[61]. This was a high risk of bias study, while the other two had a medium risk. The intervention that included text messaging, and was targeted at girls, did not show any significant improvements in diet or PA [9, 62–64]. The intervention that used a smartphone app and was targeted at boys showed a significant reduction in sweetened beverage consumption only [65], with 63% reporting using the app.
Features of effective interventions
Most (n=22) interventions included diet or PA education, and eight of these resulted in a significant improvement in at least one behaviour [39, 41, 42, 44, 65–68]. Educational elements generally consisted of providing information about the importance of healthy behaviours as well as instruction on how to eat a healthy diet or do enough physical activity. One study showed that a nutrition education element alone resulted in a significant improvement in diet while additional intervention components did not provide further benefit [52]. Some studies with educational elements did not show significant results, or were inconclusive [9, 11, 36, 40, 60], but findings of this review suggest that health education is a potentially valuable component for interventions aimed at improving health behaviours of adolescents. This may be delivered through a range of media including websites, tailored advice pages, classroom education, or social media.
Goal-setting and self-monitoring were very common components of digital interventions, and these two elements appeared to be most effective when paired. A total of 11 studies used goal-setting, and 14 used self-monitoring; of these, six interventions used both. Crucially, almost all the interventions that included goal setting showed a significant improvement in at least one measure of diet [40, 52, 57, 69], physical activity [41, 49] or both [44, 65, 68]. Self-monitoring was less effective without goal setting [9, 36, 54, 70].
Parental or family involvement was also an important factor in some of the interventions. Most interventions that included this showed some significant improvement in behaviour [10, 38, 39, 41, 43, 60, 65]. However, in interventions where parents were supposed to participate, but did not, there was little intervention effect [9, 11, 57, 67]. In addition to parental engagement, data on participants’ engagement with the intervention can provide useful insight into the ways in which behaviour change can be supported. Of the 26 studies included in this review, only four did not report any data on implementation or engagement [38, 42, 55, 57]. For all other studies, available process data are reported in Table 4. Due to the variation in data reported and in intervention components, generalisations about engagement and implementation could not be drawn.
Cost effectiveness
None of the studies included a cost-effectiveness analysis or any discussion about the cost of the interventions.
Discussion
Despite the recent popularity in using digital media to improve dietary and PA behaviours, little is known about their effectiveness amongst adolescents. This review has found some evidence that website interventions can effect diet and physical activity behaviour change amongst adolescents. However, these changes are often not sustained in the medium or long term. This may be partially due to the variability in engagement with interventions, as shown in Table 4. While implementation and engagement were not consistently reported, a number of studies published some data about acceptability or use of the digital intervention and this variation was sometimes related to intervention effectiveness [39, 45, 46]. There is a marked lack of evidence for other digital approaches to behaviour change, including text messages, email, smartphones and social media. Despite these gaps, this review showed that particular intervention features, namely health education, goal setting, self-monitoring and targeting to specific populations, can lead to improved diet and physical activity behaviours in adolescents.
Effectiveness of digital interventions for improving diet and physical activity behaviours of adolescents
This review showed that digital interventions can be effective in improving the diet and physical activity behaviours of adolescents, although these changes are often not sustained in the longer term. The largest evidence base exists for website-delivered interventions. Regarding other digital media, there is much interest in developing smartphone apps for changing health behaviours. As this is a new area, there is a paucity of evidence for their effectiveness and this review did not find any significant results for app interventions. However, one of the school-based multicomponent interventions in Australia that included a smartphone app did find a significant reduction in sweetened beverage consumption [65]. We cannot draw conclusions about text messages or emailing because there were few intervention studies that employed these means of communication and most were ineffective at changing behaviours.
Features of effective interventions
Whatever the digital platform, the evidence from this review suggests that there are components that most often characterise effective digital interventions for health behaviour change in adolescents. Firstly, while educating adolescents using a range of methods on the importance of good diet and PA habits is not enough to change behaviour, it is an important element of effective interventions. It is also clearly beneficial to encourage adolescents to set specific diet or PA goals and to provide a means by which progress can be monitored. Examples of approaches to achieving this are pedometers, food diaries, exercise logs, and weight loss trackers.
A component that was sometimes associated with significant improvements in diet and/or PA was parental involvement. This agrees with the findings of a systematic review conducted in 2014 on interventions to prevent childhood obesity. In that review, Kelishadi et al concluded that familial involvement was amongst the key intervention components that encouraged significant improvement in children’s health behaviours [71]. As discussed above, most interventions that included a parental element showed significant improvement, but in cases where parents did not participate, their adolescent children failed to improve their health behaviours. Therefore, intervention design might consider whether it is likely that the target population could benefit from an additional component aimed at adolescents’ parents.
Cost-effectiveness
In developing public health interventions, it is important to consider their cost-effectiveness, so this review aimed to extract and analyse cost data from included studies. Unfortunately, cost-effectiveness is often not assessed in any formal way, and none of the 32 publications included in this review reported cost-effectiveness data on their interventions. Furthermore, the heterogeneity of interventions precludes the synthesis of general conclusions about cost because most interventions included other components in addition to the digital platform and because some studies required participants to have their own technology while others provided the necessary devices. This is a clear gap in the literature, and should be addressed in future public health intervention trials. As digital platforms are assumed to provide an opportunity for low-cost, scalable interventions, this is especially relevant.
Strengths and limitations
This review followed established guidance on the conduct of systematic reviews [33]. The literature search was comprehensive, and designed to capture a wide range of digital interventions for improving the health behaviours of adolescents. The screening process was undertaken by two independent researchers, and final lists were compared to reduce the chance of omitting any relevant studies. Data extraction was rigorous and used a data extraction form that was piloted at the start of the review. Similarly, quality criteria were clearly defined from the outset, so the quality assessment process was consistent and transparent. Only one reviewer carried out all data extraction, but in order to reduce bias a second reviewer assessed one in three studies and there was agreement about results and conclusions in every case.
There was considerable heterogeneity between studies included in this review. While they could be grouped reasonably well by digital media platform, there was still variation within these groups with regards to intervention content, duration, intensity, setting, target population and outcome measures. The heterogeneity of studies meant that a meta-analysis was not feasible. However, a narrative synthesis was carried out, grouping interventions by digital platform, and then examining the frequencies of key features of each intervention to look for trends.
While most included studies were randomised controlled trials, the majority (19 of 27) had a medium to high risk of bias overall. Common sources of bias were small sample size, participant selection bias and poor handling of confounding factors in data analysis. A source of bias in many systematic reviews is publication bias, which results from the fact that studies with positive findings are more likely to be published than studies that do not show an effect. For this review, only published studies were included, but consultation with experts did not reveal any unpublished works that should be included.
Conclusions
Digital media are widely accessed by adolescents, and may represent a scalable and inexpensive opportunity for engaging this group in behaviour change. The findings of this review suggest that digital interventions that include health education, goal-setting, self-monitoring, and parent involvement can produce significant improvements in the dietary and PA behaviours of adolescents. This is particularly the case with interventions using websites as this platform represented 15 of the 27 included studies. There is less evidence for the effectiveness of other digital platforms such as apps, text messages and social media, despite the constantly growing number of interventions using these resources, due to the paucity of well-designed trials of these interventions. Smartphone-based interventions are widely accessible and low-cost, and make use of resources already used by most adolescents. Therefore, it is important that more high-quality trials be conducted and published in the academic literature, and apps that have already been developed should be formally trialled in order to inform the development of future behaviour change interventions.
Supplementary Material
References
- 1.Cutler GJ, et al. Major patterns of dietary intake in adolescents and their stability over time. J Nutr. 2009;139(2):323–8. doi: 10.3945/jn.108.090928. [DOI] [PubMed] [Google Scholar]
- 2.Larson NI, et al. Trends in Adolescent Fruit and Vegetable Consumption, 1999–2004: Project EAT. American Journal of Preventive Medicine. 2007;32(2):147–150. doi: 10.1016/j.amepre.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 3.Larson NI, et al. Fast Food Intake: Longitudinal Trends during the Transition to Young Adulthood and Correlates of Intake. Journal of Adolescent Health. 2008;43(1):79–86. doi: 10.1016/j.jadohealth.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 4.Sanchez A, et al. Patterns and correlates of physical activity and nutrition behaviors in adolescents. Am J Prev Med. 2007;32(2):124–30. doi: 10.1016/j.amepre.2006.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Doak C, et al. The prevention of overweight and obesity in children and adolescents: a review of interventions and programmes. Obesity reviews. 2006;7:111–136. doi: 10.1111/j.1467-789X.2006.00234.x. [DOI] [PubMed] [Google Scholar]
- 6.Lien N, Jacobs DR, Jr, Klepp KI. Exploring predictors of eating behaviour among adolescents by gender and socio-economic status. Public Health Nutr. 2002;5(5):671–81. doi: 10.1079/PHN2002334. [DOI] [PubMed] [Google Scholar]
- 7.Neumark-Sztainer D, et al. Factors Influencing Food Choices of Adolescents. Journal of the American Dietetic Association. 1999;99(8):929–937. doi: 10.1016/S0002-8223(99)00222-9. [DOI] [PubMed] [Google Scholar]
- 8.Lamb J, Puskar KR, Tusaie-Mumford K. Adolescent research recruitment issues and strategies: Application in a rural school setting. Journal of Pediatric Nursing. 2001;16(1):43–52. doi: 10.1053/jpdn.2001.20552. [DOI] [PubMed] [Google Scholar]
- 9.Lubans D, et al. Two-year outcomes from the NEAT Girls obesity prevention cluster randomized controlled trial. Journal of Science and Medicine in Sport. 2013;16:e34. [Google Scholar]
- 10.Lubans D, et al. Outcomes from the ATLAS school-based intervention incorporating smartphone technology for adolescent boys: A cluster RCT. Journal of Science and Medicine in Sport. 2014;18:e63. [Google Scholar]
- 11.Lubans DR, et al. Effects of integrating pedometers, parental materials, and E-mail support within an extracurricular school sport intervention. Journal of Adolescent Health. 2009;44(2):176–83. doi: 10.1016/j.jadohealth.2008.06.020. [DOI] [PubMed] [Google Scholar]
- 12.Covelli MM. Efficacy of a school-based cardiac health promotion intervention program for African-American adolescents. Applied Nursing Research. 2008;21(4):173–180. doi: 10.1016/j.apnr.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 13.Contento IR, et al. Adolescents demonstrate improvement in obesity risk behaviors after completion of choice, control & change, a curriculum addressing personal agency and autonomous motivation. Journal of the American Dietetic Association. 2010;110(12):1830–1839. doi: 10.1016/j.jada.2010.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Straker LM, et al. The impact of Curtin University's activity, food and attitudes program on physical activity, sedentary time and fruit, vegetable and junk food consumption among overweight and obese adolescents: a waitlist controlled trial. PLoS ONE. 2014; 9(11):e111954. doi: 10.1371/journal.pone.0111954. [Electronic Resource] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bogart LM, et al. Preliminary healthy eating outcomes of SNaX, a pilot community-based intervention for adolescents. Journal of Adolescent Health. 2011;48(2):196–202. doi: 10.1016/j.jadohealth.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shrewsbury VA, et al. Short-term outcomes of community-based adolescent weight management: The Loozit® Study. BMC pediatrics. 2011;11(1):1. doi: 10.1186/1471-2431-11-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pearson N, et al. A family-based intervention to increase fruit and vegetable consumption in adolescents: a pilot study. Public health nutrition. 2010;13(06):876–885. doi: 10.1017/S1368980010000121. [DOI] [PubMed] [Google Scholar]
- 18.Neumark-Sztainer DR, et al. New moves—preventing weight-related problems in adolescent girls: a group-randomized study. American journal of preventive medicine. 2010;39(5):421–432. doi: 10.1016/j.amepre.2010.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pew Research Center. Smartphone Ownership and Internet Usage Continues to Climb in Emerging Economies; but advanced economies still have higher rates of technology use [Google Scholar]
- 20.Amanda Lenhart. Teens, Social Media & Technology Overview 2015. Pew Research Center; Washington, DC: 2015. [Google Scholar]
- 21.Piwek L, et al. The rise of consumer health wearables: promises and barriers. PLoS Medicine. 2015 doi: 10.1371/journal.pmed.1001953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keating SR, McCurry MK. Systematic review of text messaging as an intervention for adolescent obesity. J Am Assoc Nurse Pract. 2015;27(12):714–20. doi: 10.1002/2327-6924.12264. [DOI] [PubMed] [Google Scholar]
- 23.Lau PW, et al. A systematic review of information and communication technology-based interventions for promoting physical activity behavior change in children and adolescents. Journal of Medical Internet Research. 2011;13(3):e48. doi: 10.2196/jmir.1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Snapchat. Snapchat-blog.com. Team stapchat; Let's chat. [Google Scholar]
- 25.Instagram. Our Story. [07 Apr 2016]; Available from: https://www.instagram.com/press/?hl=en.
- 26.Six to Start. Zombies, Run! History. [07 Apr 2016]; Available from: https://zombiesrungame.com/presskit/
- 27.Lappan L, Yeh M, Leung M. Technology as a platform for improving healthy behaviors and weight status in children and adolescents: a review. Obes Open Access. 2015;1(3) [Google Scholar]
- 28.National Institute for Health and Care Excellence. The guidelines manual: PMG6. [03 Apr 2017];2012 Available from: https://www.nice.org.uk/process/pmg6/chapter/assessing-cost-effectiveness#economic-evidence-and-guideline-recommendations. [PubMed]
- 29.Kraft P, Yardley L. Current issues and new directions in Psychology and Health: What is the future of digital interventions for health behaviour change? 2009 doi: 10.1080/08870440903068581. [DOI] [PubMed] [Google Scholar]
- 30.Yardley The Person-Based Approach to Intervention Development: Application to Digital Health-Related Behaviour Change Interventions. Journal of Medical Internet Research. 2015;17(1) doi: 10.2196/jmir.4055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Elbert NJ, et al. Effectiveness and cost-effectiveness of ehealth interventions in somatic diseases: a systematic review of systematic reviews and meta-analyses. Journal of medical Internet research. 2014;16(4):e110. doi: 10.2196/jmir.2790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Free C, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS med. 2013;10(1):e1001362. doi: 10.1371/journal.pmed.1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Centre for Reviews and Dissemination. Systematic Reviews: CRD's guidance for undertaking reviews in health care. York: University of York; 2009. [Google Scholar]
- 34.Moher D, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 35.Lana A, Faya-Ornia G, Lopez ML. Impact of a web-based intervention supplemented with text messages to improve cancer prevention behaviors among adolescents: results from a randomized controlled trial. Preventive Medicine. 2014;59:54–9. doi: 10.1016/j.ypmed.2013.11.015. [DOI] [PubMed] [Google Scholar]
- 36.Sousa P, et al. Controlled trial of an Internet-based intervention for overweight teens (Next.Step): effectiveness analysis. European Journal of Pediatrics. 2015;174(9):1143–57. doi: 10.1007/s00431-015-2502-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Whittemore R, et al. Implementation of a school-based internet obesity prevention program for adolescents. Journal of Nutrition Education & Behavior. 2013;45(6):586–94. doi: 10.1016/j.jneb.2013.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jones M, et al. Healthy weight regulation and eating disorder prevention in high school students: A universal and targeted web-based intervention. Journal of Medical Internet Research. 2014;16(2):28–39. doi: 10.2196/jmir.2995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Williamson DA, et al. Two-year internet-based randomized controlled trial for weight loss in African-American girls. Obesity. 2006;14(7):1231–43. doi: 10.1038/oby.2006.140. [DOI] [PubMed] [Google Scholar]
- 40.Ezendam NP, Brug J, Oenema A. Evaluation of the Web-based computer-tailored FATaintPHAT intervention to promote energy balance among adolescents: results from a school cluster randomized trial. Archives of Pediatrics & Adolescent Medicine. 2012;166(3):248–55. doi: 10.1001/archpediatrics.2011.204. [DOI] [PubMed] [Google Scholar]
- 41.Patrick K, et al. Outcomes of a 12-month technology-based intervention to promote weight loss in adolescents at risk for type 2 diabetes. Journal of Diabetes Science & Technology. 2013;7(3):759–70. doi: 10.1177/193229681300700322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Frenn M, et al. Changing the tide: an Internet/video exercise and low-fat diet intervention with middle-school students. Applied Nursing Research. 2005;18(1):13–21. doi: 10.1016/j.apnr.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 43.Chen JL, et al. The efficacy of the web-based childhood obesity prevention program in Chinese American adolescents (Web ABC study) Journal of Adolescent Health. 2011;49(2):148–54. doi: 10.1016/j.jadohealth.2010.11.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cullen KW, et al. Evaluation of a web-based program promoting healthy eating and physical activity for adolescents: teen choice: food and fitness. Health Education Research. 2013;28(4):704–14. doi: 10.1093/her/cyt059. [DOI] [PubMed] [Google Scholar]
- 45.Jago R, et al. Fit for Life Boy Scout badge: outcome evaluation of a troop and Internet intervention. Preventive Medicine. 2006;42(3):181–7. doi: 10.1016/j.ypmed.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 46.Thompson D, et al. Boy Scout 5-a-Day Badge: outcome results of a troop and Internet intervention. Preventive Medicine. 2009;49(6):518–26. doi: 10.1016/j.ypmed.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 47.De Bourdeaudhuij I, et al. Evaluation of a computer-tailored physical activity intervention in adolescents in six European countries: the Activ-O-Meter in the HELENA intervention study. Journal of Adolescent Health. 2010;46(5):458–66. doi: 10.1016/j.jadohealth.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 48.Cook TL, et al. Moderators of the effectiveness of a web-based tailored intervention promoting physical activity in adolescents: the HELENA Activ-O-Meter. Journal of School Health. 2014;84(4):256–66. doi: 10.1111/josh.12140. [DOI] [PubMed] [Google Scholar]
- 49.Slootmaker SM, et al. Accelerometers and Internet for physical activity promotion in youth? Feasibility and effectiveness of a minimal intervention [ISRCTN93896459] Preventive Medicine. 2010;51(1):31–6. doi: 10.1016/j.ypmed.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 50.Guthrie N, et al. Development of an accelerometer-linked online intervention system to promote physical activity in adolescents. PLoS ONE [Electronic Resource] 2015;10(5):e0128639. doi: 10.1371/journal.pone.0128639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Maes L, et al. Pilot evaluation of the HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) Food-O-Meter, a computer-tailored nutrition advice for adolescents: a study in six European cities. Public Health Nutrition. 2011;14(7):1292–302. doi: 10.1017/S1368980010003563. [DOI] [PubMed] [Google Scholar]
- 52.Bech-Larsen T, Gronhoj A. Promoting healthy eating to children: A text message (SMS) feedback approach. International Journal of Consumer Studies. 2013;37(3):250–256. [Google Scholar]
- 53.Lau EY, et al. Evaluation of an Internet-short message service-based intervention for promoting physical activity in Hong Kong Chinese adolescent school children: a pilot study. Cyberpsychology, behavior and social networking. 2012;15(8):425–34. doi: 10.1089/cyber.2012.0161. [DOI] [PubMed] [Google Scholar]
- 54.Newton KH, Wiltshire EJ, Elley CR. Pedometers and text messaging to increase physical activity: randomized controlled trial of adolescents with type 1 diabetes. Diabetes Care. 2009;32(5):813–5. doi: 10.2337/dc08-1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sirriyeh R, Lawton R, Ward J. Physical activity and adolescents: an exploratory randomized controlled trial investigating the influence of affective and instrumental text messages.[Erratum appears in Br J Health Psychol. 2015 May;20(2):447-8] British Journal of Health Psychology. 2010;15(Pt 4):825–40. doi: 10.1348/135910710X486889. [DOI] [PubMed] [Google Scholar]
- 56.Adamo KB, Rutherford JA, Goldfield GS. Effects of interactive video game cycling on overweight and obese adolescent health. Applied Physiology, Nutrition, & Metabolism = Physiologie Appliquee, Nutrition et Metabolisme. 2010;35(6):805–15. doi: 10.1139/H10-078. [DOI] [PubMed] [Google Scholar]
- 57.Baranowski T, et al. Video game play, child diet, and physical activity behavior change: A randomized clinical trial. American Journal of Preventive Medicine. 2011;40(1):33–38. doi: 10.1016/j.amepre.2010.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Direito A, et al. Apps for IMproving FITness and Increasing Physical Activity Among Young People: The AIMFIT Pragmatic Randomized Controlled Trial. Journal of Medical Internet Research. 2015;17(8):e210. doi: 10.2196/jmir.4568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Abroms LC, et al. The STRENGTH Ezine: an application of e-mail for health promotion in adolescent girls. American Journal of Health Promotion. 2004;19(1):28–32. doi: 10.4278/0890-1171-19.1.28. [DOI] [PubMed] [Google Scholar]
- 60.Wojcicki TR, et al. Promoting Physical Activity in Low-Active Adolescents via Facebook: A Pilot Randomized Controlled Trial to Test Feasibility. JMIR Research Protocols. 2014;3(4):e56. doi: 10.2196/resprot.3013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lubans DR, et al. Exploring the mechanisms of weight loss in the SHED-IT intervention for overweight men: a mediation analysis. International Journal of Behavioral Nutrition & Physical Activity. 2009;6:8p. doi: 10.1186/1479-5868-6-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lubans DR, et al. The Nutrition and Enjoyable Activity for Teen Girls (NEAT girls) randomized controlled trial for adolescent girls from disadvantaged secondary schools: rationale, study protocol, and baseline results. BMC Public Health. 2010;10:652. doi: 10.1186/1471-2458-10-652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dewar DL, et al. Exploring changes in physical activity, sedentary behaviors and hypothesized mediators in the NEAT girls group randomized controlled trial. Journal of Science & Medicine in Sport. 2014;17(1):39–46. doi: 10.1016/j.jsams.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 64.Lubans D, et al. Preventing obesity among adolescent girls: Outcomes of the nutrition and enjoyable activity for teen girls cluster randomized controlled trial. Journal of Science and Medicine in Sport. 2012;15:S332. doi: 10.1001/archpediatrics.2012.41. [DOI] [PubMed] [Google Scholar]
- 65.Smith JJ, et al. Smart-phone obesity prevention trial for adolescent boys in low-income communities: the ATLAS RCT. Pediatrics. 2014;134(3):e723–31. doi: 10.1542/peds.2014-1012. [DOI] [PubMed] [Google Scholar]
- 66.Chen J-L, Wilkosz ME. Efficacy of technology-based interventions for obesity prevention in adolescents: a systematic review. Adolescent health, medicine and therapeutics. 2014;5:159. doi: 10.2147/AHMT.S39969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Whittemore R, Jeon S, Grey M. An internet obesity prevention program for adolescents. Journal of Adolescent Health. 2013;52(4):439–47. doi: 10.1016/j.jadohealth.2012.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Williamson D, et al. Efficacy of an internet-based behavioral weight loss program for overweight adolescent African-American girls. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity. 2005;10(3):193–203. doi: 10.1007/BF03327547. [DOI] [PubMed] [Google Scholar]
- 69.Whittemore R, et al. An Internet Coping Skills Training Program for Youth With Type I Diabetes. Six-Month Outcomes. Nursing Research. 2012;61(6):395–404. doi: 10.1097/NNR.0b013e3182690a29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jones DJ, et al. Technology-enhanced program for child disruptive behavior disorders: development and pilot randomized control trial. Journal of clinical child and adolescent psychology : the official journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53. 2014;43(1):88–101. doi: 10.1080/15374416.2013.822308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kelishadi R, Soleiman FA. Controlling childhood obesity: A systematic review on strategies and challenges. Journal of Research in Medical Sciences. 2014;19(10)) [PMC free article] [PubMed] [Google Scholar]
- 72.Lubans DR, et al. Preventing Obesity Among Adolescent Girls: One-Year Outcomes of the Nutrition and Enjoyable Activity for Teen Girls (NEAT Girls) Cluster Randomized Controlled Trial. Archives of Pediatrics & Adolescent Medicine. 2012;166(9):821–7. doi: 10.1001/archpediatrics.2012.41. [DOI] [PubMed] [Google Scholar]
- 73.Williamson DA, et al. Efficacy of an internet-based behavioral weight loss program for overweight adolescent African-American girls. Eating & Weight Disorders: EWD. 2005;10(3):193–203. doi: 10.1007/BF03327547. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.