Abstract
Disinfectant use has been associated with adverse respiratory effects among healthcare workers. However, the specific harmful agents have not been elucidated. We examined the association between occupational exposure to disinfectants and asthma control in the Nurses’ Health Study II, a large cohort of female nurses.
Nurses with asthma were invited in 2014 to complete two questionnaires on their current occupation and asthma (response rate: 80%). Asthma control was defined by the Asthma Control Test (ACT). Exposure to major disinfectants was evaluated by a Job-Task-Exposure Matrix (JTEM).
Analyses included 4,102 nurses with asthma (mean age: 58 years). Asthma control was poor (ACT=16–19) in 12% of nurses and very poor (≤15) in 6%. Use of disinfectants to clean medical instruments (19% exposed) was associated with poorly (odds ratio 1.37; 95%CI: [1.05–1.79]) and very poorly (1.88 [1.38–2.56]) controlled asthma (P-trend 0.004, after adjustment for potential confounders). Using JTEM estimates, exposure to formaldehyde, glutaraldehyde, hypochlorite bleach, hydrogen peroxide and enzymatic cleaners was associated with poor asthma control (all P-trend<0.05); exposure to quaternary ammonium compounds and alcohol was not.
Use of several disinfectants was associated with poor asthma control. Our findings suggest targets for future efforts to prevent worsening of asthma control in healthcare workers.
INTRODUCTION
To achieve and maintain asthma control is the primary target of asthma management international guidelines [1]. However, population-based studies in Europe and in the U.S. have shown that asthma control is suboptimal in 40–50% of adult patients, with even higher rates among women [2, 3]. While asthma management recommendations mainly focus on treatment, identification and avoidance of exposures contributing to poor asthma control are recognized as important steps in disease management [1]. Nevertheless, few epidemiological studies have focused on determinants of asthma control among adults [1, 4].
Workplace exposures contribute to poor asthma control and severe exacerbations [5, 6], and their reduction has been suggested as one of the public health interventions likely to have the greatest effect in improvement of respiratory health [7]. A substantial part of work-related asthma cases have been identified in the healthcare industry, which is one of the largest employment sectors in the U.S. and in Europe [8, 9].
Increased risk of asthma symptoms/exacerbations among healthcare workers is believed to be related in large part to exposure to cleaning products and disinfectants [8, 10–12]. Although some of the chemicals contained in these products (e.g., bleach, quaternary ammonium compounds [quats], ammonia) have been associated with current asthma or asthma symptoms/exacerbations [10, 12–14], results from epidemiological studies are limited or inconsistent regarding most specific agents. This question is of particular importance in healthcare settings as work-related asthma prevention strategies, usually based on avoidance of the harmful agent(s), need to be implemented in accordance with infection control guidelines regarding disinfection procedures, to protect patients from infections [15].
The Nurses’ Health Study II (NHSII) is a large, ongoing, prospective study of U.S. female nurses. In 2014, we initiated a case-control study on asthma nested within the NHSII, to study occupational determinants of asthma. In a recent publication, we address the challenge of assessing exposure to a wide range of disinfectants in this population, for which we developed a Job-Task-Exposure Matrix (JTEM) [16]. In the present paper, we investigated the association between occupational exposure to cleaning/disinfection tasks and specific agents, and asthma control.
MATERIAL AND METHODS
Population
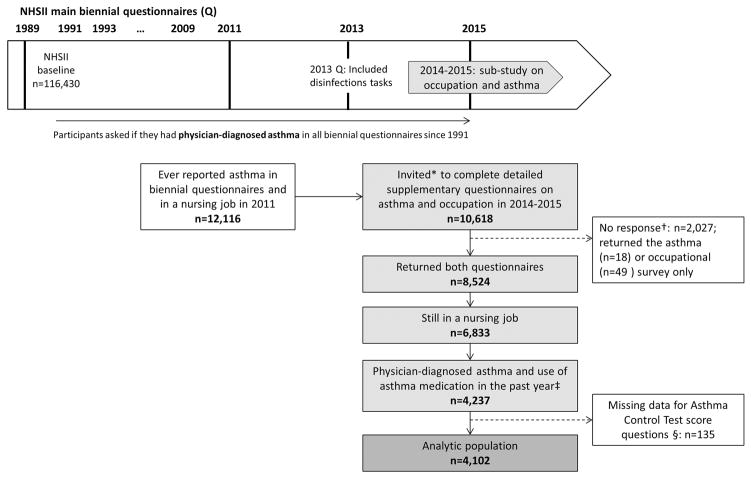
The NHSII began in 1989 when 116,430 female registered nurses from 15 U.S. states, aged 25–44 years, completed a questionnaire on their medical history and lifestyle characteristics [17–19]. Follow-up questionnaires have been sent every 2 years since. In 2014, 10,618 participants who ever reported physician-diagnosed asthma in biennial questionnaires and were in a nursing job in 2011 were invited to complete two questionnaires, one on occupational exposures and one on asthma (Figure 1, response rate: 80%). This investigation was approved by the Institutional Review Board at the Brigham and Women’s Hospital, (Boston, MA).
Figure 1. Flow-chart of the study population.
In NHSII, the active follow-up rate (number of person-years in the cohort when participants are censored after their last questionnaire response) from 1989 to 2013 was 86% of the potential person-years.
* Women with asthma invited to complete the surveys were selected among women who reported physician-diagnosed asthma in biennial questionnaires, but only recent respondents (i.e., who returned 2013 or 2015 questionnaires) were invited. The first invite to complete the survey was sent by email to participants with email address (85%) and by regular mail to participants without email address (15%). After this first attempt (including two email reminders for women with email address), all non-respondents received up to two more invites by regular mail.
† Non-respondents were significantly younger and were more often current smokers, obese and nonwhite than respondents. Non-respondents reported higher use of disinfectants in 2011 (weekly use of disinfectants to clean surfaces: 47%) than respondents (43%).
‡ Participants who reiterated on the supplemental questionnaire that a physician had diagnosed her as having asthma, and reported use of any asthma medication in the past year.
§ Participants with missing data for Asthma Control Test score questions did not differ from included participants for age, smoking status, BMI, race, ethnicity, or self-reported use of disinfectants.
NHSII: Nurses’ Health Study II.
Asthma
Participants who reported asthma in biennial questionnaires were categorized on the basis of supplemental asthma questionnaires according to validated case definitions, as described previously [17–19]. We selected participants who reiterated on the supplemental questionnaire that a physician had diagnosed her as having asthma, and who reported use of any asthma medication in the past year [17]. Sensitivity analyses were conducted using a more stringent asthma definition, based on the latter criteria and additional report of use of a prescribed long-term preventive medication (ie, inhaled corticosteroids, cromolyn sodium, nedocromil, salmeterol, theophylline) in the past year. Among them, asthma control was defined using the Asthma Control Test score (range 5–25), based on five questions on activity limitations, frequency of symptoms, and frequency of use of quick-relief medication in the past four weeks [20].
Exposure to disinfectants
Information on general disinfection tasks (frequency of use of disinfectants to clean surfaces/medical instruments, use of spray) was collected in the occupational questionnaire [10, 21], as described previously [16]. These questions also were asked in the 2013 main questionnaire, i.e., before and independently of the 2014–2015 asthma sub-study (Figure 1).
Exposure to seven major disinfectants/cleaning products (formaldehyde, glutaraldehyde, hypochlorite bleach, hydrogen peroxide, alcohol, quats, and enzymatic cleaners) was evaluated by a nurse-specific JTEM. The JTEM was designed using information collected by questionnaire in a random sample of NHSII participants without asthma (n=9,073), as described in details elsewhere [16] and in online supplement. The JTEM assigned exposure level (low, medium, or high) based on combinations of types of nursing jobs and general disinfection tasks (“job-task” axis).
Exposure to eight other products with lower exposure prevalence (ortho-phtalaldehyde, peracetic acid, acetic acid, ammonia, phenolics, ethylene oxide, chloramine T and “green” products) was not evaluated by the JTEM but by self-report [16]. Results regarding these eight products are presented in online supplement.
Analyses
Associations between exposure to disinfectants and asthma control were evaluated by logistic regressions. Asthma control (outcome) was classified into four categories (25: controlled; 20–24: partly controlled; 16–19: poorly controlled; ≤15: very poorly controlled) and considered either as a categorical variable or as an ordinal variable. Disinfection tasks were studied using dichotomous variables (task performed 1–3 or 4–7 days/week vs. never or <1 day/week). Exposure to specific disinfectants according to JTEM was studied using 3-level variables (low, medium, or high exposure level). First, we studied exposure to each disinfectant separately. Then, as nurses were classified as exposed to several products, we studied exposure to combinations of several specific products evaluated by JTEM, for the products found associated with asthma control when studied separately. Analyses were adjusted for age, smoking status, body mass index (BMI), race (white vs. other) and ethnicity (Hispanic vs. other). A two-sided P<0.05 was considered statistically significant. Analyses were run using SAS V.9 (SAS Institute, Cary, NC, USA).
RESULTS
Of the 8,524 participants who returned both questionnaires on asthma and occupation, 6,833 were still in a nursing job in 2014–2015 (Figure 1). Among them, n=4,237 reported use of any asthma medication in the past year. Participants with missing data for ACT questions (n=135) were excluded. This yielded a population of 4,102 women eligible for analysis. Participants were on average 58 years of age and 70% were never smokers. Regarding cleaning/disinfection tasks, 46% of the nurses reported weekly use of disinfectants to clean surfaces, 19% to clean medical instruments, and 19% reported weekly use of sprays. Weekly use of disinfectants was associated with younger age (P=0.001), but no significant difference was observed regarding smoking status, BMI, race, or ethnicity. The ACT score ranged from 7 to 25 (median: 23, Q1–Q3: 21–25). Asthma was controlled in 32% of nurses, partly controlled in 50%, poorly controlled in 12% and very poorly controlled in 6%. Women with poor asthma control were more often current or ex-smoker and had a higher BMI (Table 1). Description of each of the ACT score components in the study population is presented in Table 2.
Table 1.
Characteristics of the participants according to asthma control, among 4,102 nurses with asthma
| Asthma Control Test score
|
P | ||||
|---|---|---|---|---|---|
| 25 | 20–24 | 16–19 | ≤15 | ||
| n (%) | 1,303 (32) | 2,035 (50) | 496 (12) | 268 (6) | |
| Age, m (sd) | 58.4 (4.4) | 58.8 (4.3) | 58.9 (4.2) | 59.0 (4.2) | 0.01 |
| Race (non white), % | 5 | 6 | 5 | 8 | 0.23 |
| Ethnicity (Hispanic), % | 2 | 2 | 1 | 1 | 0.49 |
| Smoking status*, % | |||||
| Never smoker | 70 | 67 | 64 | 61 | 0.01 |
| Ex-smoker | 28 | 29 | 32 | 33 | |
| Current smoker | 2 | 4 | 4 | 6 | |
| BMI*, % | |||||
| <25 kg/m2 | 33 | 29 | 23 | 18 | < 0.001 |
| 25–29.9 kg/m2 | 31 | 29 | 28 | 31 | |
| ≥ 30 kg/m2 | 36 | 42 | 49 | 51 | |
BMI – Body Mass Index.
In 2013 (main Nurse’s Health Study II questionnaire). Missing values for smoking status: n=5; BMI: 37.
Table 2.
Description of Asthma Control Test score components, among 4,102 nurses with asthma
| Asthma Control Test score
|
||||
|---|---|---|---|---|
| 25 | 20–24 | 16–19 | ≤15 | |
| n (%) | 1,303 (32) | 2,035 (50) | 496 (12) | 268 (6) |
| Asthma Control Test score components, score† ≤3, % | ||||
| Activity limitations | 0 | 3 | 21 | 56 |
| Shortness of breath | 0 | 6 | 48 | 92 |
| Woken up by asthma symptoms at night | 0 | 5 | 35 | 78 |
| Use of β-agonist inhaler | 0 | 15 | 66 | 92 |
| Poor self-rated asthma control | 0 | 7 | 54 | 92 |
The asthma control test (ACT) score was based on responses to five questions (components) on activity limitations, frequency of symptoms, and frequency of use of quick-relief medication in the last four weeks. Each question was scored using a 5-point scale (1: poor control to 5: good control). Scores for each question are then summed to give the ACT score (range 5–25).
Results presented as percentage of participants with a score ≤3 for a given component: activity limitations (asthma keep from getting as much done at work, school or at home), “some of the time” to “all of the time”; shortness of breath, “3–6 times/week” to “more than once daily”; woken up by asthma symptoms at night - “once/week” to “every night”; use β-agonist inhaler “2 times/week” to “3+ times daily”; self-rated asthma control, “Somewhat controlled” to “Not controlled at all”.
Cleaning/disinfection tasks and asthma control
In multivariable models (Table 3), weekly use of disinfectants to clean medical instruments was associated with poorly and very poorly controlled asthma (odds ratio [OR], 95% Confidence Interval [CI]: 1.37, 1.05–1.79 and 1.88, 1.38–2.56, respectively; P-trend<0.001), but no association was observed for the use of disinfectants to clean surfaces. Associations were similar in participants with childhood-onset and adult-onset asthma (age at onset <18 vs. ≥18 years, P interaction=0.92) and with or without atopy (defined by report of ever having had hay fever, seasonal allergy or allergic rhinitis, P interaction=0.76). Weekly use of spray was also associated with poorer asthma control (Table 3, P-trend=0.002), in particular sprays used for surface cleaning/disinfection, patient care, and air-refreshing sprays (Supplementary Table E1). When examining frequency of cleaning/disinfection tasks (Supplementary Table E2), associations with poor asthma control were generally stronger among nurses with the highest frequency of use (4–7 days/week). However, for spray use, significant associations were observed even among nurses with infrequent use (<1 day/week).
Table 3.
Associations between self-reported cleaning/disinfection tasks and asthma control
| Asthma Control Test score
|
P trend | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 25 (ref.) | 20–24 | 16–19 | ≤15 | |||||||
|
| ||||||||||
| n | % | OR* | % | OR* (95% CI) | % | OR* (95% CI) | % | OR* (95% CI) | ||
| Weekly use of disinfectant | ||||||||||
| To clean surfaces | ||||||||||
| No (ref.) | 2,179 | 32 | 1 | 49 | 1 | 13 | 1 | 6 | 1 | |
| Yes | 1,893 | 31 | 1 | 50 | 1.07 (0.93–1.23) | 12 | 0.96 (0.77–1.18) | 7 | 1.26 (0.96–1.65) | 0.36 |
| To clean instruments | ||||||||||
| No (ref.) | 3,299 | 32 | 1 | 50 | 1 | 12 | 1 | 6 | 1 | |
| Yes | 769 | 28 | 1 | 49 | 1.16 (0.96–1.40) | 14 | 1.37 (1.05–1.79) | 9 | 1.88 (1.38–2.56) | <0.001 |
| Surface and/or instruments | ||||||||||
| None (ref.) | 2,068 | 33 | 1 | 49 | 1 | 12 | 1 | 6 | 1 | |
| Surface only | 1,235 | 32 | 1 | 51 | 1.04 (0.89–1.23) | 11 | 0.85 (0.66–1.09) | 6 | 1.00 (0.73–1.38) | 0.61 |
| Instruments | 769 | 28 | 1 | 49 | 1.19 (0.97–1.44) | 14 | 1.29 (0.97–1.70) | 9 | 1.87 (1.34–2.62) | <0.001 |
| Weekly use of sprays† | ||||||||||
| No (ref.) | 3,301 | 33 | 1 | 50 | 1 | 11 | 1 | 6 | 1 | |
| Yes | 766 | 28 | 1 | 49 | 1.13 (0.94–1.36) | 15 | 1.50 (1.16–1.94) | 8 | 1.38 (1.00–1.92) | 0.002 |
OR from multinomial logistic regressions, adjusted for age, smoking status, body mass index, race and ethnicity.
Use of spray for patient care, instrument cleaning or disinfection, surface cleaning or disinfection, air-refreshing or other.
Results in bold are statistically significant.
All exposure variables had <1% missing values.
OR – odds ratio; CI – confidence interval; JTEM – Job-Task-Exposure Matrix
We found similar results in sensitivity analyses (a) studying associations between disinfection tasks reported in the 2013 main questionnaire and asthma control evaluated in 2014–2015, (Supplementary Table E3), and (b) using a more stringent asthma definition (Supplementary Table E4).
Use of a face mask or other respiratory protection devices when working with disinfectant was reported by 5% of the participants overall, but was more frequent (P=0.03) among women with poorer asthma control. Use of latex gloves (24%) was not associated with asthma control. No significant difference in the association between use of disinfectants to clean instruments and poorer asthma control (Pinteraction ≥0.40) was observed according to use of respiratory protection devices or to use of latex gloves (Supplementary Figure E1).
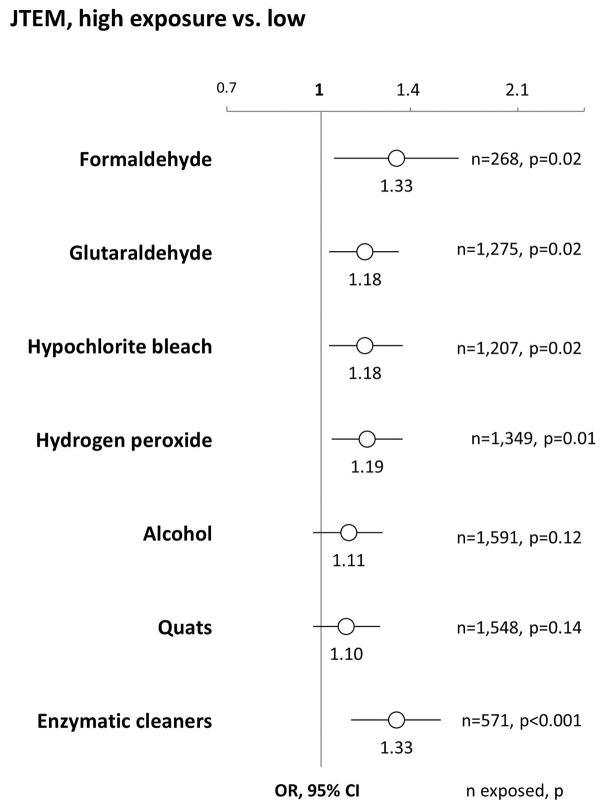
Specific disinfectants/cleaning products evaluated by the JTEM and asthma control
In multivariable models, using JTEM estimates, high level of exposure to formaldehyde (P-trend=0.02), glutaraldehyde (P-trend=0.02), hypochlorite bleach (P-trend=0.02), hydrogen peroxide (P-trend=0.01) and enzymatic cleaners (P-trend<0.001) were significantly associated with poorer asthma control (Figure 2); quats (P-trend=0.14) and alcohol (P-trend=0.12) were not. More detailed results for each category of asthma control are presented in Supplementary Table E5.
Figure 2.
Associations between exposure to specific disinfectants/cleaning products evaluated by the JTEM and asthma control. Results are presented as odds ratio (OR) and 95% confidence intervals (CI) for a decrease in Asthma Control Test score category (25: controlled; 20–24: partly controlled; 16–19: poorly controlled; ≤15: very poorly controlled), analyzed as an ordinal variable (ordinal logistic regression), and adjusted for age, smoking status, body mass index, race and ethnicity. Associations presented compare high exposure level vs. low exposure level, for each product; no association was observed when comparing medium to low exposure level. JTEM – Job-Task-Exposure Matrix.
Nurses generally were classified as exposed to several products (i.e., we did not identify subgroups of nurses with exposure to a single product). Based on this observation, we studied a combination of specific products evaluated by JTEM (Table 4). In this analysis, no associations with asthma control were observed among nurses exposed (i) to hypochlorite bleach or hydrogen peroxide but not to the other products; or (ii) to aldehydes (formaldehyde or glutaraldehyde) but not to the other products. In contrast, a significant increased risk of poorer asthma control was observed (P-trend=0.05) among nurses exposed to hypochlorite bleach/hydrogen peroxide and aldehydes; and among those further exposed to enzymatic cleaners (P-trend=0.001). The latter exposure combination was observed in participants employed in various nursing jobs (emergency room, operating room, outpatient or community, other hospital nursing or nursing outside hospital), and among them, most (83%) reported weekly use of disinfectants to clean medical instruments.
Table 4.
Associations between combinations of specific disinfectants/cleaning products evaluated by JTEM and asthma control
| Asthma Control Test score
|
P trend | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 25 (ref.) | 20–24 | 16–19 | ≤15 | |||||||
|
| ||||||||||
| Exposure combinations (JTEM estimates) † | n | % | OR* | % | OR* (95% CI) | % | OR* (95% CI) | % | OR* (95% CI) | |
| Low exposure level for all products (ref.)‡ | 1,832 | 33 | 1 | 49 | 1 | 12 | 1 | 6 | 1 | |
| (i): high exposure level to hypochlorite bleach or hydrogen peroxide | 537 | 34 | 1 | 47 | 0.95 (0.76–1.18) | 12 | 0.95 (0.68–1.31) | 7 | 1.11 (0.73–1.68) | 0.95 |
| (ii): high exposure level to formaldehyde or glutaraldehyde | 408 | 34 | 1 | 49 | 1.01 (0.79–1.29) | 11 | 0.88 (0.60–1.29) | 6 | 0.96 (0.59–1.57) | 0.71 |
| (iii): (i) + (ii) | 332 | 28 | 1 | 51 | 1.21 (0.92–1.60) | 12 | 1.16 (0.78–1.74) | 9 | 1.71 (1.07–2.73) | 0.05 |
| (iv): (i) + (ii) + high exposure level to enzymatic cleaners§ | 571 | 28 | 1 | 49 | 1.20 (0.96–1.50) | 14 | 1.35 (0.99–1.85) | 9 | 1.91 (1.31–2.79) | 0.001 |
OR from multinomial logistic regression, adjusted for age, smoking status, body mass index, race and ethnicity.
Mutually exclusive categories.
Classified as low exposure level for all 7 products evaluated by the JTEM.
All nurses with high level of exposure to enzymatic cleaners also had high level of exposure to glutaraldehyde and/or formaldehyde, and to hydrogen peroxide and/or hypochlorite bleach.
Results in bold are statistically significant.
All exposure variables had <1% missing values.
OR – odds ratio; CI – confidence interval; JTEM – Job-Task-Exposure Matrix
In addition, we further examined the associations between exposure to alcohol and quats and asthma control (a) among nurses not exposed to high level of any of the other five products, and (b) among all nurses, in multivariable models further adjusted for the other five products (combined). In both analyses, the absence of association between exposure to alcohol or quats and asthma control was confirmed, with ORs close to the null and P-trends >0.30.
DISCUSSION
In this study of 4,102 U.S. nurses with asthma, disinfections tasks, in particular disinfection of medical instruments, were associated with poor asthma control. We found increased risks of poor asthma control associated with exposure to glutaraldehyde, formaldehyde, enzymatic cleaners, hypochlorite bleach and hydrogen peroxide, in particular for nurses exposed to several of these products. Exposure to quats and alcohol were not associated with poor asthma control.
To our knowledge, this is the first time that asthma control has been studied in relation to occupational exposure to disinfectants among a large cohort of healthcare workers. Asthma was well-characterized in this population of nurses; a previous validation study in NHSII indeed confirmed 95% of the nurses’ reports of doctor-diagnosed asthma.[17] Moreover, we evaluated asthma control using a standardized and validated definition (ACT) [1, 22], integrating the main domains of asthma control (symptoms, use of rescue therapy, sleep interference, activity limitations). Many studies on work-related asthma have focused on distinguishing risk factors for occupational asthma (i.e., new-onset asthma caused by occupational exposure) and work-exacerbated asthma (worsening of a pre-existing asthma) [23, 24]. In the current study, the association between use of disinfectants and poor asthma control was similar among nurses with childhood-onset (i.e., pre-existing) and adult-onset (i.e., potentially caused by occupational exposures) asthma. Although the distinction between occupational and work-exacerbated asthma is important for legal considerations (workers’ compensation), it may be less relevant from a public health perspective as both occupational and work-exacerbated asthma have long-term socio-economic and health consequences [25]. To minimize risk of exacerbations and accelerated lung function decline in workers, experts have called for research on occupational exposures contributing to poor asthma control [6]. Our results are consistent with a few recent studies showing that exposure to occupational asthmagens [5, 26, 27], and in particular cleaning agents [5, 28], are associated with uncontrolled asthma. Mechanisms by which disinfectants and cleaning products impact respiratory health remain unclear and require further research [11]. Some products (e.g. enzyme-based products) have sensitizing potential, but most agents are assumed to act as respiratory irritants [11], and may cause injury of the airway epithelium, oxidative stress and long-lasting neurogenic inflammation [23, 24, 29]. Regardless of the exact mechanisms, our results support the need to consider occupation and potential exposure to disinfectants in clinical practice to improve management of patients with asthma [6, 30].
Identifying the specific tasks and agents associated with poor asthma control is of particular importance to improve asthma management among healthcare workers. We found that medical instrument disinfection was associated with poor asthma control, pointing toward a role of high-level disinfectants used on critical or semi-critical items [15]. We did not find evidence of an association between use of disinfectants to clean surface and asthma control, although this type of task has been associated with increased risk of physician-diagnosed asthma in a study of healthcare workers in Texas [14]. Few epidemiological studies have investigated the relationship between specific cleaning agents and disinfectants and asthma outcomes in healthcare workers [10, 12, 13], and they were limited in terms of number/variety of specific products studied and attempt to control for correlated exposures. In the current study, although we could not fully study the independent effect of each chemical - because we did not find subgroups of nurses with exposure to a single product – we attempted to identify combinations of exposures associated with greater risk of poor asthma control. We found particularly increased risk among nurses with exposure to aldehydes (formaldehyde or glutaraldehyde), hypochlorite bleach or hydrogen peroxide, and enzymatic cleaners, based on JTEM estimates. Formaldehyde has been known as an asthmagen for long [31]. Glutaraldehyde and hydrogen peroxide also have been suggested as agents implicated in occupational asthma among healthcare workers in a smaller study in Canada [32] or case reports in France and in the U.S. [33, 34]. Associations between the use of hypochlorite bleach and asthma outcomes have been reported in European studies [11]. Enzymatic products are used to clean items before high level disinfection or sterilization. A role of enzymatic cleaners in asthma among healthcare workers was suspected based on case reports in healthcare settings [35], and earlier reports in the detergent industry [36] in the U.K. We believe this is the first time these agents have been implicated in an epidemiological study. Finally, a strong association between exposure to quats and physician-diagnosed asthma has been reported in a study of 543 French healthcare workers [12], in contrast with our results. Exposure to quats is particularly difficult to evaluate [21]. In our study, although we integrated information collected on products’ brand names and review of the corresponding safety date sheets, as recommended [12], when creating the JTEM, exposure to quats may still be under-estimated. However, any trend for an association between exposure to quats and poor asthma control disappeared after controlling for exposure to other products.
Besides the active ingredients, specific types of tasks and products’ application procedures may influence respiratory health effects and are interesting targets for interventions [15]. Spraying has been associated with increased risk of asthma or respiratory symptoms, likely because of the higher potential for inhalation exposure when using sprays [13]. Consistently, we found in the current study that use of spray was associated with poor asthma control.
Major strengths of our study included the large sample size and the use, for the first time, of a nurse-specific JTEM. Most existing studies on the relationship between the use of specific cleaning/disinfecting products and asthma relied on self-reported exposures, raising the issue of both non-differential and differential misclassification bias, potentially leading to bias either toward or away from the null [21]. Use of job-exposure matrices (JEM) is generally favored in occupational epidemiology for exposure assessment in large populations [37]. Because nursing jobs are heterogeneous (i.e., nurses with the same job title may perform different tasks), we showed that taking into account disinfection tasks (within job variability) in exposure assessment by creating a JTEM provides better exposure estimates than a JEM, i.e. reduces exposure misclassification [16]. In the present study, we observed associations between exposure to several products, as evaluated by the JTEM, and asthma control. However, as we used questionnaires to evaluate disinfection tasks, some of our results may be subject to differential misclassification bias (i.e. differential recall of exposure according to asthma outcomes, possibly leading to spurious associations). To address this question, we performed a sensitivity analysis studying prospectively the associations between disinfection tasks in 2013 and asthma control in 2014–2015, and found similar results, suggesting that differential misclassification bias is not likely a major explanation for our findings regarding disinfection tasks. Potential for recall bias in the association between self-reported cleaning/disinfection tasks and asthma has been formally evaluated in the Texas healthcare workers study; although the author warn against the possibility of such bias, only a slight effect was reported [38]. Finally, other studies where evaluation of disinfectant exposure was based on expert assessment (i.e., independent of participants’ recall), have reported associations with current or physician-diagnosed asthma [12, 13].
The cross-sectional design of our study also prevents addressing the question of a healthy worker effect, i.e. a tendency of workers with asthma history or more severe asthma to avoid or leave jobs involving harmful exposures such as disinfectants. Such an effect has been suggested in a previous analysis of this cohort of women who have been in nursing jobs for several decades [19], and may cause underestimation of some associations in the current study. However, it is notable that we observed strong positive associations between exposure to several disinfectants and poor asthma control despite a potential healthy worker effect – which typically bias associations toward the null [19]. In future studies, assessing the association between disinfectant exposures and asthma control among healthcare workers at an earlier career stage, and the impact of exposure duration, would be of particular interest.
Finally, in our study, exposure to eight specific disinfectants could not be evaluated using the JTEM as exposure prevalence was too low (<10% with weekly exposures in all nursing job types) to create such estimates [16], which was a limitation. However, we evaluated risks associated with exposure to major disinfectants and cleaning agents used in healthcare settings [39]. Our results also confirmed that latex exposure was no longer the major concerns for respiratory health among healthcare workers, as suggested in the last years [8], most likely because of the reduction of use of powdered latex gloves.
In our study, the use of respiratory protection devices when handling disinfectants was limited – in accordance with a previous report [39] - although it was more frequent among nurses with poor asthma control. Even with more than 4,000 nurses, because of low numbers, we could not determine whether use of respiratory protection devices had an impact on the association between disinfectants use and asthma control. However, use of personal protective equipment is generally not considered as the most effective measure of work-related asthma prevention. Elimination of hazardous substances and replacement with safer alternatives is preferred [15]. In accordance with earlier reports, we found that many chemicals in healthcare settings may have an impact on respiratory health, including products (e.g., hydrogen peroxide) used as alternative to known asthmagens (e.g. aldehydes) [39]. Our result thus support the investigation of emerging non-chemical technologies for disinfection (e.g., steam, ultraviolet light) as a potential alternative to chemical disinfection [15], and further research on green cleaning, integrating health risk reduction among the products’ standards [40].
The U.S. has more than 3 million registered nurses, and over 12 million workers are employed in the healthcare industry [41]; in Europe, healthcare worker represent ~10% of the workforce [8]. We found that the use of several specific disinfectants in nurses was associated with poor to very poor asthma control. Our findings highlight the urgency of integrating occupational health considerations to guidelines for cleaning and disinfection in healthcare [15]; they suggest targets for future efforts to improve asthma management in a large group of workers.
Supplementary Material
Take home message.
Frequent use of disinfectants is associated with poor asthma control in nurses.
Acknowledgments
The Nurses’ Health Study II is coordinated at the Channing Division of Network Medicine, Brigham and Women’s Hospital, Boston, MA, USA. We would like to thank the participants and staff of the Nurses’ Health Study II for their valuable contributions. In particular, we would like to thank Lisa Abramovitz, Krislyn Boggs, Charlotte Marsh, Chidiogo Onwuakor and Christina Staffiere for their help with data cleaning and management. We also thank Francine Kauffmann for her participation in the study conception.
Funding:
Centers for Disease Control and Prevention R01 OH-10359; National Institutes of Health UM1 CA176726; Hubert Curien Partnerships for French–Dutch cooperation, French Ministry of Higher Education and Research and OCW Dutch Ministry (Ministerie van Onderwijs, Cultuur en Wetenschap) PHC Van Gogh 33653RF. The research leading to these results has received funding from the People Programme (Marie Curie Actions) of the European Union’s Seventh Framework Programme (FP7/2007–2013) under REA grant agreement n. PCOFUND-GA-2013-609102, through the PRESTIGE programme coordinated by Campus France.
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
References
- 1.Papaioannou AI, Kostikas K, Zervas E, Kolilekas L, Papiris S, Gaga M. Control of asthma in real life: still a valuable goal? Eur Respir Rev. 2015;24:361–369. doi: 10.1183/16000617.00001615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Braido F, Brusselle G, Guastalla D, Ingrassia E, Nicolini G, Price D, Roche N, Soriano JB, Worth H. Determinants and impact of suboptimal asthma control in Europe: The International Cross-Sectionnal And Longitudinal Assessment On Asthma Control (LIAISON) study. Respir Res. 2016;17:51. doi: 10.1186/s12931-016-0374-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fuhlbrigge A, Reed ML, Stempel DA, Ortega HO, Fanning K, Stanford RH. The status of asthma control in the U.S. adult population. Allergy Asthma Proc. 2014;30:529–533. doi: 10.2500/aap.2009.30.3276. [DOI] [PubMed] [Google Scholar]
- 4.Schatz M. Predictors of asthma control: what can we modify? Curr Opin Allergy Clin Immunol. 2012;12:263–268. doi: 10.1097/ACI.0b013e32835335ac. [DOI] [PubMed] [Google Scholar]
- 5.Le Moual N, Carsin A-E, Siroux V, Radon K, Norback D, Torén K, Olivieri M, Urrutia I, Cazzoletti L, Jacquemin B, Benke G, Kromhout H, Mirabelli MC, Mehta AJ, Schlünssen V, Sigsgaard T, Blanc PD, Kogevinas M, Antó JM, Zock J-P. Occupational exposures and uncontrolled adult-onset asthma in the European Community Respiratory Health Survey II. Eur Respir J. 2014;43:374–386. doi: 10.1183/09031936.00034913. [DOI] [PubMed] [Google Scholar]
- 6.Boulet L-P. Asthma control in the workplace. Eur Respir J. 2014;43:319–321. doi: 10.1183/09031936.00137713. [DOI] [PubMed] [Google Scholar]
- 7.Beasley R, Semprini A, Mitchell EA. Risk factors for asthma: is prevention possible? Lancet. 2015;386:1075–1085. doi: 10.1016/S0140-6736(15)00156-7. [DOI] [PubMed] [Google Scholar]
- 8.Wiszniewska M, Walusiak-Skorupa J. Occupational allergy: respiratory hazards in healthcare workers. Curr Opin Allergy Clin Immunol. 2014;14:113–118. doi: 10.1097/ACI.0000000000000039. [DOI] [PubMed] [Google Scholar]
- 9.White GE, Mazurek JM, Moorman JE. Asthma in Health Care Workers: 2008 and 2010 Behavioral Risk Factor Surveillance System Asthma Call-back Survey. J Occup Env Med. 2013;55:1463–1468. doi: 10.1097/JOM.0000000000000006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arif AA, Delclos GL. Association between cleaning-related chemicals and work-related asthma and asthma symptoms among healthcare professionals. Occup Env Med. 2012;69:35–40. doi: 10.1136/oem.2011.064865. [DOI] [PubMed] [Google Scholar]
- 11.Siracusa A, De Blay F, Folletti I, Moscato G, Olivieri M, Quirce S, Raulf-Heimsoth M, Sastre J, Tarlo SM, Walusiak-Skorupa J, Zock J-P. Asthma and exposure to cleaning products - a European Academy of Allergy and Clinical Immunology task force consensus statement. Allergy. 2013;68:1532–1545. doi: 10.1111/all.12279. [DOI] [PubMed] [Google Scholar]
- 12.Gonzalez M, Jégu J, Kopferschmitt M-C, Donnay C, Hedelin G, Matzinger F, Velten M, Guilloux L, Cantineau A, de Blay F. Asthma among workers in healthcare settings: role of disinfection with quaternary ammonium compounds. Clin Exp Allergy. 2014;44:393–406. doi: 10.1111/cea.12215. [DOI] [PubMed] [Google Scholar]
- 13.Dumas O, Donnay C, Heederik D, Héry M, Choudat D, Kauffmann F, Le Moual N. Occupational exposure to cleaning products and asthma in hospital workers. Occup Env Med. 2012;69:883–889. doi: 10.1136/oemed-2012-100826. [DOI] [PubMed] [Google Scholar]
- 14.Arif AA, Delclos GL, Serra C. Occupational exposures and asthma among nursing professionals. Occup Env Med. 2009;66:274–278. doi: 10.1136/oem.2008.042382. [DOI] [PubMed] [Google Scholar]
- 15.Quinn MM, Henneberger PK, Braun B, Delclos GL, Fagan K, Huang V, Knaack JLS, Kusek L, Lee SJ, Le Moual N, Maher KAE, McCrone SH, Mitchell AH, Pechter E, Rosenman K, Sehulster L, Stephens AC, Wilburn S, Zock JP. Cleaning and disinfecting environmental surfaces in health care: Toward an integrated framework for infection and occupational illness prevention. Am J Infect Control. 2015;43:424–434. doi: 10.1016/j.ajic.2015.01.029. [DOI] [PubMed] [Google Scholar]
- 16.Quinot C, Dumas O, Henneberger PK, Varraso R, Wiley AS, Speizer FE, Golberg M, Zock J-P, Camargo CA, Jr, Le Moual N. Development of a job-task-exposure matrix to assess occupational exposure to disinfectants among US nurses. Occup Env Med. 2017;74:130–137. doi: 10.1136/oemed-2016-103606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Camargo CA, Jr, Weiss ST, Zhang S, Willett WC, Speizer FE. Prospective study of body mass index, weight change, and risk of adult-onset asthma in women. Arch Intern Med. 1999;159:2582–2588. doi: 10.1001/archinte.159.21.2582. [DOI] [PubMed] [Google Scholar]
- 18.Le Moual N, Varraso R, Zock JP, Henneberger PK, Speizer F, Kauffmann F, Camargo CA., Jr Are operating room nurses at higher risk of severe persistent asthma? The Nurses’ Health Study. J Occup Env Med. 2013;55:973–977. doi: 10.1097/JOM.0b013e318297325b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dumas O, Varraso R, Zock JP, Henneberger PK, Speizer FE, Wiley AS, Le Moual N, Camargo CA., Jr Asthma history, job type and job changes among US nurses. Occup Env Med. 2015;72:482–488. doi: 10.1136/oemed-2014-102547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA, Kosinski M, Pendergraft TB, Jhingran P. Asthma Control Test: Reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol. 2006;117:549–556. doi: 10.1016/j.jaci.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 21.Donnay C, Denis MA, Magis R, Fevotte J, Massin N, Dumas O, Pin I, Choudat D, Kauffmann F, Le Moual N. Under-estimation of self-reported occupational exposure by questionnaire in hospital workers. Occup Env Med. 2011;68:611–617. doi: 10.1136/oem.2010.061671. [DOI] [PubMed] [Google Scholar]
- 22.Cloutier MM, Schatz M, Castro M, Clark N, Kelly HW, Mangione-Smith R, Sheller J, Sorkness C, Stoloff S, Gergen P. Asthma outcomes: Composite scores of asthma control. J Allergy Clin Immunol Elsevier Ltd. 2012;129:S24–S33. doi: 10.1016/j.jaci.2011.12.980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tarlo SM, Lemiere C. Occupational asthma. N Engl J Med. 2014;370:640–649. doi: 10.1056/NEJMra1301758. [DOI] [PubMed] [Google Scholar]
- 24.Dumas O, Le Moual N. Do chronic workplace irritant exposures cause asthma? Curr Opin Allergy Clin Immunol. 2016;16:75–85. doi: 10.1097/ACI.0000000000000247. [DOI] [PubMed] [Google Scholar]
- 25.Lemière C, Boulet LP, Chaboillez S, Forget A, Chiry S, Villeneuve H, Prince P, Maghni K, Kennedy WA, Blais L. Work-exacerbated asthma and occupational asthma: Do they really differ? J Allergy Clin Immunol. 2013;131:704–710. doi: 10.1016/j.jaci.2012.08.024. [DOI] [PubMed] [Google Scholar]
- 26.Marincu I, Frent S, Tomescu MC, Mihaicuta S. Rates and predictors of uncontrolled bronchial asthma in elderly patients from western Romania. Clin Interv Aging. 2015;10:963–967. doi: 10.2147/CIA.S83141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lindström I, Suojalehto H, Pallasaho P, Luukkonen R, Karjalainen J, Lauerma A, Karjalainen A. Middle-Aged Men With Asthma Since Youth. J Occup Environ Med. 2013;55:917–923. doi: 10.1097/JOM.0b013e31828dc9c9. [DOI] [PubMed] [Google Scholar]
- 28.Dumas O, Siroux V, Luu F, Nadif R, Zock JP, Kauffmann F, Le Moual N. Cleaning and asthma characteristics in women. Am J Ind Med. 2014;57:303–311. doi: 10.1002/ajim.22244. [DOI] [PubMed] [Google Scholar]
- 29.Dumas O, Matran R, Zerimech F, Decoster B, Huyvaert H, Ahmed I, Le Moual N, Nadif R. Occupational exposures and fluorescent oxidation products in 723 adults of the EGEA study. Eur Respir J. 2015;46:258–261. doi: 10.1183/09031936.00177614. [DOI] [PubMed] [Google Scholar]
- 30.Lemière C, To T, De Olim C, Ribeiro M, Liss G, Lougheed MD, Hoy R, Forget A, Blais L, Zhu J, Tarlo SM. Outcome of work-related asthma exacerbations in Quebec and Ontario. Eur Respir J. 2015;45:266–268. doi: 10.1183/09031936.00096114. [DOI] [PubMed] [Google Scholar]
- 31.Chan-Yeung M, Malo JL. Aetiological agents in occupational asthma. Eur Respir J. 1994;7:346–371. doi: 10.1183/09031936.94.07020346. [DOI] [PubMed] [Google Scholar]
- 32.Dimich-Ward H, Lee Wymer M, Chan-Yeung M. Respiratory health survey of respiratory therapists. Chest. 2004;126:1048–1053. doi: 10.1378/chest.126.4.1048. [DOI] [PubMed] [Google Scholar]
- 33.Cristofari-Marquand E, Kacel M, Milhe F, Magnan A, Lehucher-Michel MP. Asthma caused by peracetic acid-hydrogen peroxide mixture. J Occup Health. 2007;49:155–158. doi: 10.1539/joh.49.155. [DOI] [PubMed] [Google Scholar]
- 34.Hawley B, Casey ML, Cox-Ganser JM, Edwards N, Fedan KA, JCK Respiratory Symptoms and Skin Irritation Among Hospital Workers Using a New Disinfection Product — Pennsylvania, 2015. US Department of Health and Human Services/Centers for Disease Control and Prevention. Morbidity & Mortality Weekly Report. 2016;65:400–401. doi: 10.15585/mmwr.mm6515a3. [DOI] [PubMed] [Google Scholar]
- 35.Adisesh A, Murphy E, Barber CM, Ayres JG. Occupational asthma and rhinitis due to detergent enzymes in healthcare. Occup Med. 2011;61:364–369. doi: 10.1093/occmed/kqr107. [DOI] [PubMed] [Google Scholar]
- 36.Cullinan P, Harris JM, Taylor AJN, Hole AM, Jones M, Barnes F, Jolliffe G. An outbreak of asthma in a modern detergent factory. Lancet. 2000;356:1899–1900. doi: 10.1016/s0140-6736(00)03264-5. [DOI] [PubMed] [Google Scholar]
- 37.Loomis D. Towards population-wide exposure assessment. Occup Env Med. 2012;69:455–456. doi: 10.1136/oemed-2012-100928. [DOI] [PubMed] [Google Scholar]
- 38.Delclos GL, Gimeno D, Arif AA, Benavides FG, Zock JP. Occupational exposures and asthma in health-care workers: comparison of self-reports with a workplace-specific job exposure matrix. Am J Epidemiol. 2009;169:581–587. doi: 10.1093/aje/kwn387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Henn SA, Boiano JM, Steege AL. Precautionary practices of healthcare workers who disinfect medical and dental devices using high-level disinfectants. Infect Control Hosp Epidemiol. 2015;36:180–185. doi: 10.1017/ice.2014.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Garza JL, Cavallari JM, Wakai S, Schenck P, Simcox N, Morse T, Meyer JD, Cherniack M. Traditional and environmentally preferable cleaning product exposure and health symptoms in custodians. Am J Ind Med. 2015;58:988–995. doi: 10.1002/ajim.22484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.BLS. [Last accessed: January 31st, 2017];US Bureau of Labor Statistics. 2015 http://www.bls.gov/news.release/ocwage.nr0.htm.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.